Instructions for use PRESTANCE
All instructions related to each of the components separately, as listed below, apply to the fixed Prestance combination.
Perindopril
Hypersensitivity/angioedema
There have been rare reports of angioedema of the face, extremities, lips, mucous membranes, tongue, glottis and/or larynx in patients treated with ACE inhibitors, including perindopril. These reactions may occur at any time during therapy. In such cases, Prestance should be stopped immediately and the necessary monitoring should be carried out until the symptoms disappear completely. If the swelling affects only the face and lips, it usually goes away on its own, although antihistamines can be used to treat symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, vocal cords, or larynx can lead to airway obstruction. If such symptoms occur, epinephrine (adrenaline) should be immediately administered subcutaneously and/or the airway should be secured. The patient should be under medical supervision until symptoms disappear completely and completely.
An increased risk of developing angioedema when taking an ACE inhibitor exists in patients who have had angioedema not associated with taking an ACE inhibitor.
In rare cases, angioedema of the intestine develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain (with or without nausea and vomiting), in some cases, without previous angioedema of the face and with normal C1-esterase levels. The diagnosis is made using computed tomography of the abdominal region, ultrasound, or at the time of surgery. Symptoms disappear after stopping ACE inhibitors. Therefore, in patients with abdominal pain receiving ACE inhibitors, when carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine.
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure.
Anaphylactoid reactions during desensitization
Some patients receiving ACE inhibitors during desensitization therapy (eg, hymenoptera venom) have developed anaphylactoid reactions. In a number of cases, these reactions were avoided by temporarily withdrawing the ACE inhibitor, and if the drug was accidentally taken, the anaphylactoid reaction occurred again.
Neutropenia, agranulocytosis, thrombocytopenia, anemia
Neutropenia/agranulocytosis, thrombocytopenia and anemia were observed while taking ACE inhibitors. In patients with normal liver function and in the absence of other complicating factors, neutropenia rarely develops. Perindopril should be used with extreme caution in patients with diffuse connective tissue diseases, while taking immunosuppressants, allopurinol or procainamide, especially in patients with pre-existing liver dysfunction. Some of these patients developed severe infections, in some cases resistant to intensive antibiotic therapy. When prescribing perindopril to such patients, it is recommended to periodically monitor the number of leukocytes in the blood. Patients should report any signs of infectious diseases (eg, sore throat, fever) to their doctor.
Double blockade of the RAAS
There is evidence that the combined use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren increases the risk of hypotension, hyperkalemia and renal impairment (including acute renal failure) compared with monotherapy. In this regard, double blockade of the RAAS by combined administration of an ACE inhibitor and an angiotensin II receptor antagonist or aliskiren is not recommended, especially in patients with diabetic nephropathy.
In some cases, when the combined use of ACE inhibitors and angiotensin II receptor antagonists is absolutely indicated, careful supervision by a specialist and mandatory monitoring of renal function, water-electrolyte balance and blood pressure are necessary. This applies to the use of candesartan or valsartan as adjunctive therapy to ACE inhibitors in patients with chronic heart failure. Carrying out double blockade of the RAAS under the careful supervision of a specialist and mandatory monitoring of renal function, water-electrolyte balance and blood pressure is possible in patients with chronic heart failure with intolerance to aldosterone antagonists (spironolactone), who have persistence of symptoms of chronic heart failure, despite other adequate therapy .
Arterial hypotension
ACE inhibitors can cause a sharp decrease in blood pressure. Arterial hypotension with clinical manifestations rarely develops in patients without concomitant diseases. The risk of an excessive decrease in blood pressure is increased in patients with reduced blood volume, which can be observed during diuretic therapy, following a strict salt-free diet, hemodialysis, diarrhea and vomiting, as well as in patients with severe arterial hypertension with high renin activity. In patients at increased risk of developing symptomatic hypotension, blood pressure, renal function and serum potassium levels should be carefully monitored during therapy with Prestance.
The same precautions apply to patients with coronary artery disease or cerebrovascular disease with an excessive fall in blood pressure due to myocardial infarction or a cerebrovascular event.
If arterial hypotension develops, the patient should be placed in a supine position with legs elevated. If necessary, the bcc should be replenished with the intravenous administration of 0.9% sodium chloride solution. Transient arterial hypotension is not an obstacle to further taking the drug. After restoration of blood volume and blood pressure, treatment can be continued.
Mitral stenosis, aortic stenosis, hypertrophic cardiomyopathy
Prestance, like other ACE inhibitors, should be prescribed with extreme caution to patients with mitral stenosis, left ventricular outflow tract obstruction (aortic stenosis, hypertrophic cardiomyopathy).
Kidney failure
In patients with renal failure (creatinine clearance <60 ml/min), individual selection of doses of perindopril and amlodipine is recommended. Such patients require regular monitoring of potassium and creatinine levels in the blood serum.
In patients with bilateral renal artery stenosis or stenosis of the artery of a single kidney during therapy with ACE inhibitors, cases of increased urea and creatinine in the blood serum were observed, usually reversible when therapy was discontinued. This is most likely to occur in patients with renal failure. Renovascular hypertension also has an increased risk of severe hypotension and renal failure. In some patients with arterial hypertension without signs of renal vascular damage, there may be an increase in the concentration of urea and creatinine in the blood serum (especially with a combination of perindopril and a diuretic), usually slight and transient. This is most likely in patients with pre-existing kidney failure.
Liver failure
In rare cases, taking ACE inhibitors has been accompanied by the development of a syndrome that begins with cholestatic jaundice and progresses to fulminant liver necrosis, sometimes with death. The mechanism of development of this syndrome is unclear. If jaundice or a significant increase in liver enzyme activity occurs while taking ACE inhibitors, patients should stop taking the drug and consult a doctor for a thorough medical examination.
Ethnic differences
In patients of the Negroid race, angioedema develops more often than in representatives of other races while taking ACE inhibitors.
Perindopril, like other ACE inhibitors, may have a less pronounced hypotensive effect in patients of the Black race compared to representatives of other races. Perhaps this difference is due to the fact that arterial hypertension in patients of the Negroid race very often occurs against the background of low renin activity.
Cough
Cases of cough have been reported during ACE inhibitor therapy. The cough is non-productive, incessant and goes away when therapy is stopped. Cough caused by ACE inhibitor use should be considered as part of the differential diagnosis of cough.
Surgery/general anesthesia
During surgery or during anesthesia with drugs that cause arterial hypotension, Prestance can block the formation of angiotensin II, as a consequence of compensatory release of renin. It is recommended to stop treatment the day before surgery. When hypotension occurs, which is presumably associated with this mechanism of action, the volume of blood volume should be increased.
Hyperkalemia
During treatment with ACE inhibitors, incl. and perindopril, cases of hyperkalemia have been reported. Risk factors for hyperkalemia are renal failure, impaired renal function, old age (over 70 years), diabetes mellitus, some concomitant conditions (dehydration, acute decompensation in heart failure, metabolic acidosis), concomitant use of potassium-sparing diuretics (spironolactone, eplerenone, triamterene, amiloride ), as well as potassium preparations or potassium-containing substitutes for table salt, as well as the use of other drugs that help increase the content of potassium in the blood plasma (for example, heparin). The use of potassium supplements, potassium-sparing diuretics, and potassium-containing table salt substitutes can lead to a significant increase in potassium levels in the blood, especially in patients with reduced renal function. Hyperkalemia can lead to serious, sometimes fatal arrhythmias. If simultaneous use of perindopril and the above drugs is necessary, treatment should be carried out with caution against the background of regular monitoring of potassium levels in the blood serum.
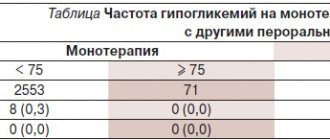
Patients with diabetes mellitus
Patients with diabetes mellitus receiving oral hypoglycemic agents or insulin should carefully monitor blood glucose concentrations during the first month of ACE inhibitor therapy.
Amlodipine
The safety and effectiveness of amlodipine in hypertensive crisis has not been established.
In elderly patients, the dose of the drug should be increased with caution.
Liver failure
T1/2 and AUC values are higher in patients with impaired liver function. Recommended doses for this category of patients have not been established, so treatment should begin with the minimum effective dose and increase it with caution. Patients with severe hepatic impairment require slow dose titration and close monitoring.
Kidney failure
In patients with renal failure, amlodipine can be used in normal doses. Changes in plasma amlodipine concentrations do not correlate with the degree of renal failure. Amlodipine is not eliminated by dialysis.
Heart failure
Caution is required when prescribing amlodipine to patients with heart failure.
In a long-term placebo-controlled study in patients with severe heart failure (NYHA classes III and IV), the incidence of pulmonary edema was higher in the amlodipine-treated group than in the placebo group. Calcium channel blockers, including amlodipine, should be used with caution in patients with congestive heart failure. they may have an increased risk of cardiovascular complications and mortality in the future.
Prestance
The combination of Prestance with lithium, potassium-sparing diuretics, potassium supplements or dantrolene is not recommended.
Due to the presence of lactose in the drug, the drug should not be prescribed to patients with hereditary lactose intolerance, glucose/galactose malabsorption syndrome, or lapp lactase deficiency.
Impact on the ability to drive vehicles and machinery
There have been no studies of the effect of the drug Prestance on the ability to drive vehicles and operate machinery. Amlodipine may have a slight or moderate effect on the ability to drive vehicles and operate machinery. If the patient suffers from dizziness, headache, tiredness, fatigue or nausea, the response may be impaired. Patients should exercise caution during these types of activities, especially at the beginning of therapy.
Preclinical safety data
Perindopril
In chronic oral toxicity studies (in rats and monkeys), the receptor organ is the kidney, and the damage is reversible.
No mutagenicity was observed in in vitro or in vivo studies.
Reproductive toxicity studies (in rats, mice, rabbits and monkeys) showed no evidence of embryotoxicity or teratogenicity. However, ACE inhibitors as a class have been shown to have adverse effects on late fetal development, leading to fetal death and congenital defects in rodents and rabbits:
- kidney damage and an increase in perinatal and postnatal mortality were observed.
No carcinogenicity was observed in studies with long-term administration in rats and mice.
Amlodipine
Reproductive toxicity studies in rats and mice have shown delayed delivery, increased duration of labor, and decreased offspring survival at doses approximately 50 times the maximum mg/kg recommended for humans.
There was no effect on fertility in rats treated with amlodipine (for males for 64 days and females for 14 days before mating) at doses up to 10 mg/kg/day (eight* times the recommended human dose, based on 10 mg/m2) . Other studies in which male rats were administered amlodipine besylate for 30 days at mg/kg doses comparable to human doses found a decrease in plasma FSH and testosterone, as well as a decrease in sperm density and the number of maternal spermatids and Sertolli cells.
In rats and mice that were administered amlodipine for 2 years at doses of 0.5, 1.25 and 2.5 mg/kg/day, no signs of carcinogenicity were detected. The highest doses (for mice, the same as for rats, exceeding the maximum recommended by 2 times, at the rate of 10 mg/kg/day) were close to the maximum tolerated doses for mice, but not for rats. Mutagenicity studies did not reveal drug-related effects at the gene or chromosomal level.
*calculated for patient body weight 50 kg
Prestance tablet 10 mg+10 mg fl pl/pack cards x30
Prestance tablet 10 mg+10 mg x30, ATX code: C09BB04 (Perindopril in combination with amlodipine)
Active substances
amlodipine Rec.INN registered by WHO perindopril arginine Rec.INN Mod. WHO registered, modified name
Dosage forms
PRESTANCE
tab. 5 mg+10 mg: 29, 30 or 90 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 5 mg+5 mg: 29, 30 or 90 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 5 mg+10 mg: 30 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 5 mg+5 mg: 30 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 10 mg+5 mg: 29, 30 or 90 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 10 mg+10 mg: 29, 30 or 90 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 10 mg+10 mg: 30 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
tab. 10 mg+5 mg: 30 pcs.reg. No.: LSR-000836/10 dated 02/09/10 - Indefinitely
Release form, composition and packaging
The tablets are white, oblong, biconvex, with “5/5” engraved on one side and the company logo on the other.
1 tab.
perindopril arginine 5 mg,
which corresponds to the content of perindopril 3.395 mg
amlodipine besilate 6.935 mg,
which corresponds to the content of amlodipine 5 mg
Excipients: microcrystalline cellulose - 26 mg, lactose monohydrate - 65.233 mg, magnesium stearate - 0.52 mg, colloidal anhydrous silicon dioxide - 0.312 mg.
The tablets are white, square, biconvex, with “5/10” engraved on one side and the company logo on the other.
1 tab.
perindopril arginine 5 mg,
which corresponds to the content of perindopril 3.395 mg
amlodipine besilate 13.87 mg,
which corresponds to the content of amlodipine 10 mg
Excipients: microcrystalline cellulose - 52 mg, lactose monohydrate - 135.466 mg, magnesium stearate - 1.04 mg, colloidal anhydrous silicon dioxide - 0.624 mg.
The tablets are white, triangular, biconvex, with “10/5” engraved on one side and the company logo on the other.
1 tab.
perindopril arginine 10 mg,
which corresponds to the content of perindopril 6.79 mg
amlodipine besilate 6.935 mg,
which corresponds to the content of amlodipine 5 mg
Excipients: microcrystalline cellulose - 52 mg, lactose monohydrate - 137.401 mg, magnesium stearate - 1.04 mg, colloidal silicon dioxide Tablets are white, round, biconvex, with an engraving “10/10” on one side and the company logo on the other.
1 tab.
perindopril arginine 10 mg,
which corresponds to the content of perindopril 6.79 mg
amlodipine besilate 13.87 mg,
which corresponds to the content of amlodipine 10 mg
Excipients: microcrystalline cellulose - 52 mg, lactose monohydrate - 130.466 mg, magnesium stearate - 1.04 mg, colloidal anhydrous silicon dioxide - 0.624 mg.
Clinical-pharmacological group: Combined antihypertensive and antianginal drug Pharmaco-therapeutic group: Antihypertensive combined drug (ACE inhibitor + BMCC)
pharmachologic effect
Perindopril
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II (ACE inhibitor). ACE, or kininase II, is an exopeptidase that carries out both the conversion of angiotensin I into the vasoconstrictor substance angiotensin II, and the breakdown of bradykinin, which has a vasodilatory effect, into an inactive heptapeptide.
Since ACE inactivates bradykinin, suppression of ACE is accompanied by an increase in the activity of both the circulating and tissue kallikrein-kinin system, while the prostaglandin system is also activated.
Perindopril has a therapeutic effect due to its active metabolite, perindoprilat. Other metabolites do not have an inhibitory effect on ACE in vitro.
Arterial hypertension
Perindopril is a drug for the treatment of arterial hypertension of any severity. With its use, there is a decrease in both systolic and diastolic blood pressure in the supine and standing positions. Perindopril reduces peripheral vascular resistance, which leads to a decrease in blood pressure and improvement of peripheral blood flow without changing heart rate.
As a rule, taking perindopril increases renal blood flow, but the glomerular filtration rate does not change.
The antihypertensive effect of the drug reaches its maximum 4-6 hours after a single oral dose and persists for 24 hours.
The antihypertensive effect 24 hours after a single oral dose is about 87-100% of the maximum antihypertensive effect. A decrease in blood pressure is achieved quite quickly.
The therapeutic effect occurs in less than 1 month from the start of therapy and is not accompanied by tachyphylaxis. Stopping treatment does not cause a rebound effect. Perindopril has a vasodilating effect, helps restore the elasticity of large arteries and the structure of the vascular wall of small arteries, and also reduces left ventricular hypertrophy.
Stable ischemic heart disease
The effectiveness of perindopril in patients (12,218 patients over 18 years of age) with stable coronary artery disease without clinical symptoms of chronic heart failure was studied during a 4-year study. 90% of study participants had previously suffered an acute myocardial infarction and/or a revascularization procedure.
In addition to the study drug, most patients received standard therapy, including antiplatelet agents, lipid-lowering agents, and beta-blockers. The primary outcome measure was a composite endpoint of cardiovascular mortality, nonfatal myocardial infarction, and/or cardiac arrest with successful resuscitation.
Therapy with perindopril tertbutylamine at a dose of 8 mg 1 time / day (equivalent to 10 mg perindopril arginine) led to a significant reduction in the absolute risk of complications by 1.9%; in patients who had previously suffered a myocardial infarction and/or a revascularization procedure, the absolute risk reduction was 2.2% compared with the placebo group.
Double blockade of the RAAS
There are data from clinical studies of combination therapy using an ACE inhibitor and angiotensin II receptor blocker (ARB II).
A clinical study was conducted in patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes mellitus accompanied by confirmed target organ damage, as well as studies in patients with type 2 diabetes and diabetic nephropathy.
Study data did not reveal a significant positive effect of combination therapy on the occurrence of renal and/or cardiovascular events and on mortality rates, while the risk of hyperkalemia, acute renal failure and/or arterial hypotension increased compared with monotherapy.
Taking into account the similar intragroup pharmacodynamic properties of ACE inhibitors and ARB II, these results can be expected for the interaction of any other drugs, representatives of the classes of ACE inhibitors and ARA II. Therefore, ACE inhibitors and ARB II should not be used simultaneously in patients with diabetic nephropathy.
There is clinical trial data examining the beneficial effects of adding aliskiren to standard therapy with an ACE inhibitor or angiotensin-converting enzyme II inhibitor in patients with type 2 diabetes mellitus and chronic kidney disease or cardiovascular disease, or a combination of these diseases. The study was stopped early due to an increased risk of adverse outcomes. Cardiovascular death and stroke were observed more often in the aliskiren group compared with the placebo group, and adverse events and serious adverse events of special interest (hyperkalemia, hypotension and renal dysfunction) were reported more often in the aliskiren group than in the placebo group.
Amlodipine
Amlodipine is a slow calcium channel blocker, a dihydropyridine derivative. Amlodipine inhibits the transmembrane transition of calcium ions into cardiomyocytes and smooth muscle cells of the vascular wall.
The antihypertensive effect of amlodipine is due to a direct relaxing effect on the smooth muscle cells of the vascular wall. The detailed mechanism by which amlodipine exerts its antianginal effect is not well established, but amlodipine is known to reduce overall ischemic burden through a dual action:
- causes dilation of peripheral arterioles, reducing peripheral vascular resistance (afterload). Since the heart rate does not change, the myocardial oxygen demand decreases,
- causes expansion of the coronary arteries and arterioles in both ischemic and intact zones. Their dilatation increases the supply of oxygen to the myocardium in patients with vasospastic angina (Prinzmetal's angina, or variant angina).
In patients with arterial hypertension, taking amlodipine 1 time per day provides a clinically significant decrease in blood pressure in the standing and lying position for 24 hours. The antihypertensive effect develops slowly, and therefore the development of acute arterial hypotension is uncharacteristic.
In patients with angina, taking amlodipine 1 time per day increases the total time of physical activity, increases the time before the development of an attack of angina, and before the appearance of depression in the ST segment by 1 mm, and also reduces the frequency of attacks angina pectoris and consumption of nitroglycerin under the tongue.
Amlodipine does not have adverse metabolic effects and does not affect the concentration of plasma lipids. The drug can be used in patients with concomitant bronchial asthma, diabetes mellitus and gout.
IHD
The results of the efficacy assessment indicate that amlodipine is characterized by fewer hospitalizations for angina pectoris and revascularization procedures in patients with coronary artery disease.
Heart failure
The results of hemodynamic studies, as well as the results of clinical studies involving patients with chronic heart failure of NYHA class II-IV, demonstrated that amlodipine does not lead to clinical deterioration, based on data on exercise tolerance, left ventricular ejection fraction and clinical symptoms.
In patients with NYHA class III-IV chronic heart failure while taking digoxin, diuretics and ACE inhibitors, it has been shown that taking amlodipine does not lead to an increased risk of mortality or mortality and morbidity associated with heart failure.
The results of long-term studies in patients with chronic heart failure class III and IV according to the NYHA classification without clinical symptoms of ischemic heart disease or objective data indicating the presence of ischemic heart disease while taking stable doses of ACE inhibitors, cardiac glycosides and diuretics showed that taking amlodipine has no effect on mortality rate from cardiovascular diseases. In this patient population, amlodipine was associated with an increase in reports of pulmonary edema.
Prevention of myocardial infarction
The effectiveness and safety of the use of amlodipine at a dose of 2.5-10 mg/day, the ACE inhibitor lisinopril at a dose of 10-40 mg/day and the thiazide diuretic chlorthalidone at a dose of 12.5-25 mg/day as a first-line drug was studied in patients with mild or moderate Hypertension and at least one of the additional risk factors for coronary complications, such as myocardial infarction or stroke suffered more than 6 months before inclusion in the study, or other confirmed cardiovascular disease of atherosclerotic origin, diabetes mellitus, HDL cholesterol concentration less than 35 mg/dL, left ventricular hypertrophy according to ECG or echocardiography, smoking.
The main criterion for assessing effectiveness is a combined indicator of the incidence of deaths from coronary artery disease and the incidence of non-fatal myocardial infarction. There were no significant differences between the amlodipine and chlorthalidone groups in the main evaluation criterion. The incidence of heart failure in the amlodipine group was significantly higher than in the chlorthalidone group - 10.2% and 7.7%, respectively, the overall incidence of deaths in the amlodipine and chlorthalidone groups did not differ significantly.
Perindopril and amlodipine
Efficacy of long-term use of amlodipine in combination with perindopril and atenolol in combination with bendroflumethiazide in patients aged 40 to 79 years with hypertension and at least 3 additional risk factors, such as left ventricular hypertrophy according to ECG or echocardiography, diabetes type 2 diabetes, peripheral arterial atherosclerosis, previous stroke or transient ischemic attack, male gender, age 55 years or older, microalbuminuria or proteinuria, smoking, total cholesterol/HDL cholesterol ≥ 6, early onset of coronary artery disease in first-degree relatives, studied in the ASCOT study -BPLA.
The main criterion for assessing effectiveness is a combined indicator of the frequency of non-fatal myocardial infarction (including painless) and fatal outcomes of coronary artery disease.
The rate of end-point complications in the amlodipine/perindopril group was 10% lower than in the atenolol/bendroflumethiazide group, but this difference was not statistically significant. In the amlodipine/perindopril group, there was a significant reduction in the incidence of complications provided for by additional efficacy criteria (except for fatal and non-fatal heart failure).
Pharmacokinetics
The amount of absorption of perindopril and amlodipine when using the drug Prestance does not differ significantly from that when using single drugs.
Perindopril
Suction
When taken orally, perindopril is rapidly absorbed, Cmax in blood plasma is achieved within 1 hour. T1/2 of perindopril from blood plasma is 1 hour.
Perindopril has no pharmacological activity. Approximately 27% of the total amount of perindopril ingested enters the bloodstream in the form of the active metabolite perindoprilate. In addition to perindoprilate, 5 more metabolites are formed that do not have pharmacological activity. Cmax of perindoprilate in blood plasma is achieved 3-4 hours after oral administration. Eating slows down the conversion of perindopril to perindoprilat, thereby affecting bioavailability. Therefore, the drug should be taken 1 time/day, in the morning, before meals.
Distribution
There is a linear relationship between the concentration of perindopril in the blood plasma and its dose. The Vd of free perindoprilate is approximately 0.2 l/kg. The binding of perindoprilate to plasma proteins, mainly to ACE, is about 20% and is dose-dependent.
Removal
Perindoprilat is excreted from the body by the kidneys. The final T1/2 of the free fraction is about 17 hours, so the equilibrium state is achieved within 4 days.
Pharmacokinetics in special clinical situations
The elimination of perindoprilate is slowed down in old age, as well as in patients with heart and renal failure (see section “Dosing regimen”). Therefore, in these groups of patients it is necessary to regularly monitor the concentration of creatinine and potassium in the blood plasma.
The dialysis clearance of perindoprilate is 70 ml/min.
The pharmacokinetics of perindopril is impaired in patients with liver cirrhosis: its hepatic clearance is reduced by 2 times. However, the amount of perindoprilate formed does not decrease, which does not require dose adjustment (see section “Dosing regimen” and “Special instructions”).
Amlodipine
Suction
After oral administration, amlodipine is slowly absorbed from the gastrointestinal tract. Food intake does not affect the bioavailability of amlodipine. Cmax of amlodipine in blood plasma is achieved 6-12 hours after taking the drug orally. Absolute bioavailability is about 64-80%.
Distribution
Vd - approximately 21 l/kg. In vitro studies have shown that about 97.5% of circulating amlodipine is bound to plasma proteins.
Metabolism and excretion
The final half-life of amlodipine from blood plasma is 35-50 hours, which allows taking the drug 1 time per day. Amlodipine is metabolized in the liver to form inactive metabolites, with 10% of the dose taken unchanged and 60% excreted by the kidneys in the form of metabolites.
Pharmacokinetics in special clinical situations
The time from taking the drug to reaching Cmax of amlodipine does not differ between elderly and younger patients. In elderly patients, the clearance of amlodipine is slowed, which leads to an increase in AUC.
The increase in AUC and T1/2 in patients with CHF corresponds to the expected value for this age group.
In patients with impaired renal function, changes in plasma concentrations of amlodipine do not correlate with the degree of renal failure. A slight increase in T1/2 is possible.
Data on the use of amlodipine in patients with hepatic impairment are limited. In patients with liver failure, a decrease in the clearance of amlodipine is observed, which leads to an increase in T1/2 and AUC by approximately 40-60%.
Amlodipine is not excreted from the body by dialysis.
Indications
- arterial hypertension and/or coronary artery disease (stable angina pectoris) in patients who require therapy with perindopril and amlodipine.
ICD-10 codes
Dosage regimen
The drug is prescribed orally, 1 tablet. 1 time/day, preferably in the morning before meals. The dose of Prestance is selected after previously titrated doses of individual components of the drug: perindopril and amlodipine in patients with arterial hypertension and/or coronary artery disease.
If therapeutically necessary, the dose of Prestance can be changed or an individual selection of doses of individual components can be carried out in advance:
5 mg perindopril + 5 mg amlodipine or 5 mg perindopril + 10 mg amlodipine or 10 mg perindopril + 5 mg amlodipine or 10 mg perindopril + 10 mg amlodipine.
Special, groups, patients,
Elderly patients and patients with renal insufficiency (see sections “Pharmacokinetics” and “Special Instructions”)
The elimination of perindoprilate in elderly patients and patients with renal failure is slower. Therefore, in such patients it is necessary to regularly monitor the concentration of creatinine and potassium in the blood plasma. Prestance can be prescribed to patients with CC ≥ 60 ml/min. Prestance is contraindicated in patients with CC <60 ml/min (see section “Contraindications”). In such patients, individual selection of doses of perindopril and amlodipine is recommended. Amlodipine, used in equivalent doses, is equally well tolerated by both elderly and younger patients. There is no need to change the dosage regimen in elderly patients, however, increasing the dose should be done with caution due to age-related changes and an increase in T1/2. Changes in the concentration of amlodipine in blood plasma do not correlate with the severity of renal failure. Amlodipine is not excreted from the body by dialysis.
Patients with hepatic insufficiency (see sections “Dosage regimen” and “Special instructions”).
For patients with mild or moderate hepatic impairment, dose selection should be done with caution. It is recommended to start taking the drug with low doses (see sections, “Dosage regimen” and “Special instructions”). The search for the optimal initial and maintenance dose for patients with liver failure should be carried out individually, using amlodipine and perindopril in monotherapy. The pharmacokinetics of amlodipine in patients with severe hepatic impairment has not been studied. For such patients, amlodipine should be started with the lowest dose and increased gradually.
Prestance should not be prescribed to children and adolescents under 18 years of age due to the lack of data on the effectiveness and safety of the use of perindopril and amlodipine in these groups of patients, both as monotherapy and in combination therapy.
Side effect
Frequency of adverse reactions that were noted during monotherapy with perindopril and amlodipine: very often (≥1/10), often (≥1/100, <.1/10), uncommon (≥1/1000, <.1/100) , rare (≥1/10,000, <.1/1000), very rare (<.1/10,000), including isolated reports, unspecified frequency (frequency cannot be calculated from available data).
From the hematopoietic and lymphatic system: very rarely - leukopenia, neutropenia, agranulocytosis, pancytopenia, thrombocytopenia, hemolytic anemia in patients with congenital deficiency of glucose-6-phosphate dehydrogenase, decreased hemoglobin concentration and hematocrit.
From the immune system: infrequently - allergic reactions.
From the side of metabolism: very rarely - hyperglycemia, unspecified frequency - hypoglycemia.
From the side of the central nervous system: often - drowsiness (especially at the beginning of treatment), dizziness (especially at the beginning of treatment), headache, paresthesia, vertigo, infrequently - insomnia, mood lability (including anxiety), sleep disturbance, tremor, hypoesthesia, depression, fainting , rarely - confusion, very rarely - peripheral neuropathy, hypertonicity.
From the senses: often - visual impairment (including diplopia), tinnitus.
From the cardiovascular system: often - a feeling of palpitations, a rush of blood to the skin of the face, a pronounced decrease in blood pressure, very rarely - angina pectoris, myocardial infarction, possibly due to an excessive decrease in blood pressure in patients at high risk (see section, "Special , instructions"), arrhythmias (including bradycardia, ventricular tachycardia and atrial fibrillation), stroke, possibly due to an excessive decrease in blood pressure in high-risk patients (see section, "Special instructions"), vasculitis.
From the respiratory system: often - shortness of breath, cough, infrequently - rhinitis, bronchospasm, very rarely - eosinophilic pneumonia.
From the digestive system: often - abdominal pain, nausea, vomiting, dyspepsia, diarrhea, constipation, infrequently - changes in the rhythm of bowel movements, dryness of the oral mucosa, very rarely - pancreatitis, gingival hyperplasia, gastritis.
From the liver and biliary tract: very rarely - hepatitis, jaundice, increased activity of liver enzymes (most often in combination with cholestasis), cytolytic or cholestatic hepatitis (see section "Special instructions").
On the part of the skin and subcutaneous fat: often - skin itching, rash, exanthema; infrequently - angioedema of the face, extremities, lips, mucous membranes, tongue, vocal folds and/or larynx (see section, "Special instructions "), alopecia, hemorrhagic rash, skin discoloration, increased sweating, urticaria, very rarely - Quincke's edema, erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, photosensitivity.
From the musculoskeletal system: often - muscle spasms, swelling of the legs, infrequently - arthralgia, myalgia, back pain.
From the urinary system: infrequently - urinary disturbances, nocturia, frequent urination, impaired renal function, very rarely - acute renal failure.
From the reproductive system and mammary glands: infrequently - impotence, gynecomastia.
General reactions: often - swelling, asthenia
Prestance®
Special instructions regarding perindopril and amlodipine also apply to the drug Prestance®.
Perindopril
Hypersensitivity/angioedema
When taking ACE inhibitors, including perindopril, in rare cases, the development of angioedema of the face, extremities, lips, mucous membranes, tongue, vocal folds and/or larynx may occur (see section “Side effects”). This can happen at any time during therapy. If symptoms appear, the drug should be stopped immediately and the patient should be observed until then. until signs of swelling disappear completely. If the swelling affects only the face and lips, it usually resolves on its own, although antihistamines may be used to treat symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, vocal folds, or larynx can lead to airway obstruction. If such symptoms occur, epinephrine (adrenaline) should be immediately administered subcutaneously and/or the airway should be secured. The patient should be under medical supervision until symptoms disappear completely and permanently.
Patients with a history of angioedema not associated with taking ACE inhibitors may have an increased risk of developing it when taking drugs of this group (see section "Contraindications").
In rare cases, angioedema of the intestine develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea or vomiting, in some cases, without previous angioedema of the face and with normal C1-esterase levels. The diagnosis is made using computed tomography of the abdominal region, ultrasound, or at the time of surgery. Symptoms disappear after stopping ACE inhibitors. Therefore, in patients with abdominal pain receiving ACE inhibitors. when carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine (see section “Side effects”).
Combined use with combination drugs containing valsartan + sacubitril
The combined use of perindopril with combination drugs containing valsartan + sacubitril is contraindicated, as the risk of developing angioedema is increased (see section "Contraindications"). The use of a combination drug containing valsartan + sacubitril is possible no earlier than 36 hours after the last dose of perindopril. The use of perindopril is possible no earlier than 36 hours after stopping the combination drug containing valsartan + sacubitril (see sections “Contraindications” and “Interaction with other drugs”). When ACE inhibitors are used together with other neprilysin inhibitors (for example, racecadotril), the risk of developing angioedema may be increased (see section "Interaction with other drugs"). In patients receiving perindopril, a careful risk/benefit assessment should be performed before initiating treatment with enkephalinase inhibitors (eg, racecadotril).
Concomitant use with mTOR inhibitors (for example, sirolimus, everolimus, temsirolimus)
When used together with mTOR inhibitors (for example, sirolimus, everolimus, temsirolimus), the risk of developing angioedema (for example, swelling of the airways or tongue with or without impairment of respiratory function) may increase (see section "Interactions with other drugs").
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during low-density lipoprotein (LDL) apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure.
Anaphylactoid reactions during desensitization
There are isolated reports of the development of anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy (for example, hymenoptera venom). In these same patients, an anaphylactoid reaction was avoided by temporarily discontinuing ACE inhibitors, and if the drug was accidentally taken, the anaphylactoid reaction occurred again.
Neutropenia/agaranulocytosis/thrombocytopenia/anemia
There are reports of the development of neutropenia/agranulocytosis. thrombocytopenia and anemia while taking ACE inhibitors. In patients with normal renal function and in the absence of other concomitant factors, neutropenia rarely develops. Perindopril should be used with extreme caution against the background of systemic connective tissue diseases, as well as while taking immunosuppressants, allopurinol or procainamide, especially in patients with impaired renal function.
Some patients developed severe infectious diseases, in some cases resistant to intensive antibiotic therapy. When using perindopril in such patients, it is recommended to periodically monitor leukocytes in the blood. Patients should report any signs of infectious diseases (eg, sore throat, fever) to their doctor.
Renovascular hypertension
In patients with bilateral renal artery stenosis or arterial stenosis of a single functioning kidney, the risk of developing arterial hypotension and renal failure increases during therapy with ACE inhibitors. Taking diuretics may be an additional risk factor (see section "Contraindications"). Deterioration of renal function can be observed with even a slight change in serum creatinine concentration, even in patients with unilateral renal artery stenosis.
Double blockade of the RAAS
There is evidence of an increased risk of arterial hypotension, hyperkalemia and renal dysfunction (including acute renal failure) when ACE inhibitors are used together with ARB II or aliskiren. Therefore, double blockade of the RAAS through the combined use of ACE inhibitors with angiotensin II receptor antagonists or aliskiren is not recommended (see sections “Pharmacodynamics” and “Interaction with other drugs”). If a double blockade is absolutely necessary, it should be performed under the strict supervision of a specialist with regular monitoring of kidney function, blood electrolyte concentrations and blood pressure.
The use of ACE inhibitors in combination with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients (see sections “Contraindications” and “Interaction with other drugs”).
Primary hyperaldosteronism
Patients with primary hyperaldosteronism are usually not susceptible to antihypertensive drugs that act by inhibiting the RAAS. Therefore, the use of the drug in such patients is not recommended.
Arterial hypotension
ACE inhibitors can cause a sharp decrease in blood pressure. Symptomatic hypotension rarely develops in patients without concomitant diseases. The risk of excessive reduction in blood pressure is increased in patients with reduced circulating blood volume, which can be observed during diuretic therapy, while following a strict salt-free diet, hemodialysis, diarrhea and vomiting, as well as in patients with severe arterial hypertension with high renin activity (see sections “Side effects” and “Interaction with other drugs”). In patients at increased risk of developing symptomatic arterial hypotension, blood pressure, renal function and serum potassium levels should be carefully monitored during therapy with Prestance.
A similar approach is also used in patients with angina pectoris and cerebrovascular diseases, in whom severe arterial hypotension can lead to myocardial infarction or cerebrovascular accident.
If arterial hypotension develops, the patient should be transferred to the supine position with legs elevated. If necessary, the volume of circulating blood should be replenished with intravenous administration of 0.9% sodium chloride solution. Transient arterial hypotension is not an obstacle to further taking the drug. After restoration of circulating blood volume and blood pressure, treatment can be continued.
Mitral stenosis/aortic stenosis/hypertrophic cardiomyopathy
Perindopril, like other ACE inhibitors, should be administered with caution to patients with left ventricular outflow tract obstruction (aortic stenosis, hypertrophic obstructive cardiomyopathy), as well as to patients with mitral stenosis.
Renal dysfunction
For patients with renal failure (creatinine clearance < 60 ml/min), individual selection of doses of perindopril and amlodipine is recommended (see section “Dosage and Administration”). Such patients require regular monitoring of potassium and creatinine levels in the blood serum (see section “Side Effects”).
In patients with bilateral renal artery stenosis or stenosis of the artery of a single kidney during therapy with ACE inhibitors, an increase in the concentration of urea and creatinine in the blood serum is possible, which usually resolves when therapy is discontinued. This effect is most often observed in patients with renal failure. The additional presence of renovascular hypertension causes an increased risk of severe hypotension and renal failure in such patients.
In some patients with arterial hypertension without signs of renal vascular damage, an increase in the concentration of urea and creatinine in the blood serum is possible, especially when perindopril is co-administered with a diuretic, usually slight and transient. This effect is more often observed in patients with pre-existing renal impairment.
Liver failure
In rare cases, cholestatic jaundice occurs while taking ACE inhibitors. As this syndrome progresses, fulminant liver necrosis may develop, sometimes with death. The mechanism of development of this syndrome is unclear. If jaundice or a significant increase in the activity of liver enzymes occurs while taking ACE inhibitors, you should stop taking the drug (see section “Side Effects”) and be under appropriate medical supervision.
Ethnic differences
In patients of the Negroid race, angioedema develops more often than in representatives of other races while taking ACE inhibitors.
Perindopril, like other ACE inhibitors, may have a less pronounced antihypertensive effect in patients of the Black race compared to representatives of other races. This difference may be due to the fact that black patients with arterial hypertension are more likely to have low renin activity.
Cough
During therapy with an ACE inhibitor, a dry cough may occur. The cough persists for a long time while taking drugs of this group and disappears after their discontinuation. This should be taken into account when carrying out the differential diagnosis of cough.
Surgery/general anesthesia
In patients who are planning to undergo major surgery or use anesthetic agents that cause arterial hypotension, the use of perindopril may block the formation of angiotensin II against the background of compensatory release of renin. Treatment should be stopped one day before surgery. If arterial hypotension develops according to this mechanism, blood pressure should be maintained by replenishing blood volume.
Hyperkalemia
Hyperkalemia may develop during treatment with ACE inhibitors. including perindopril. Risk factors for hyperkalemia include renal failure, deterioration of renal function, age over 70 years, diabetes mellitus, certain concomitant conditions (dehydration, acute decompensation of chronic heart failure, metabolic acidosis), concomitant use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, or amiloride). ), as well as potassium preparations or potassium-containing salt substitutes, as well as the use of other drugs that increase the level of potassium in the blood plasma (for example, heparin, co-trimoxazole, also known as the combination of sulfamethoxazole + trimethoprim). The use of potassium supplements, potassium-sparing diuretics, and potassium-containing table salt substitutes can lead to a significant increase in potassium levels in the blood, especially in patients with reduced renal function. Hyperkalemia can cause serious, sometimes fatal, abnormal heart rhythms. If the combined use of perindopril and the above drugs is necessary, treatment should be carried out with caution against the background of regular monitoring of the content of potassium ions in the blood serum (see section “Interaction with other drugs”).
Patients with diabetes mellitus
When prescribing the drug to patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, during the first month of therapy it is necessary to carefully monitor the concentration of glucose in the blood (see section “Interaction with other drugs”).
Amlodipine
The effectiveness and safety of amlodipine in hypertensive crisis has not been established.
Heart failure
Patients with heart failure should be treated with caution.
When using amlodipine in patients with chronic heart failure of functional class III and IV according to the NYHA classification, pulmonary edema may develop. Slow calcium channel blockers, including amlodipine, should be used with caution in patients with congestive heart failure due to a possible increased risk of cardiovascular adverse events and mortality.
Liver failure
In patients with impaired liver function, T1/2 and AUC of amlodipine are increased. Recommendations for dosing of the drug have not been established. Taking amlodipine should be started with the lowest doses and precautions should be taken both at the beginning of treatment and when increasing the dose. In patients with severe hepatic impairment, the dose should be increased gradually, ensuring careful monitoring of the clinical condition.
Elderly patients
In elderly patients, increasing the dose should be done with caution (see sections “Pharmacokinetics” and “Dosage and Administration”).
Kidney failure
Patients with renal failure can take amlodipine in standard doses. Changes in plasma concentrations of amlodipine do not correlate with the degree of renal failure. Amlodipine is not excreted from the body by dialysis.
Prestance®
Special instructions regarding amlodipine and perindopril also apply to the drug Prestance®.
Excipients
Due to the presence of lactose in the drug, it is contraindicated to prescribe the drug to patients with hereditary galactose intolerance, complete lactase deficiency and glucose-galactose malabsorption.
Drug interactions
The combined use of the drug Prestance® with lithium preparations, potassium-sparing diuretics, potassium-containing substitutes or dantrolene is not recommended (see section “Interaction with other drugs”).
Prestance Tablets, box, 30 pcs., 10 + 5 mg + mg, for oral administration
special instructions
Special instructions regarding perindopril and amlodipine apply to Prestance. Perindopril Hypersensitivity/angioedema When taking ACE inhibitors, incl. and perindopril, in rare cases, the development of angioedema of the face, extremities, lips, mucous membranes, tongue, vocal folds and/or larynx may occur (see section Side effects). This can happen at any time during therapy. If symptoms appear, the drug should be stopped immediately and the patient should be observed until signs of edema completely disappear. If the swelling affects only the face and lips, it usually resolves on its own, although antihistamines may be used to treat symptoms. Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, vocal cords, or larynx can lead to airway obstruction. If such symptoms occur, epinephrine (adrenaline) should be immediately administered subcutaneously and/or the airway should be secured. The patient should be under medical supervision until symptoms disappear completely and permanently. Patients with a history of angioedema not associated with taking ACE inhibitors may have an increased risk of developing it when taking drugs of this group (see section Contraindications). In rare cases, angioedema of the intestine develops during therapy with ACE inhibitors. In this case, patients experience abdominal pain as an isolated symptom or in combination with nausea or vomiting, in some cases, without previous angioedema of the face and with normal C1-esterase levels. The diagnosis is made using computed tomography of the abdominal region, ultrasound, or at the time of surgery. Symptoms disappear after stopping ACE inhibitors. Therefore, in patients with abdominal pain receiving ACE inhibitors, when carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine (see section Side effects). Anaphylactoid reactions during LDL apheresis: In rare cases, life-threatening anaphylactoid reactions may develop in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure. Anaphylactoid reactions during desensitization There are isolated reports of the development of anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy (for example, hymenoptera venom). In these same patients, an anaphylactoid reaction was avoided by temporarily discontinuing ACE inhibitors, and if the drug was accidentally taken, the anaphylactoid reaction occurred again. Neutropenia, agranulocytosis, thrombocytopenia, anemia Neutropenia/agranulocytosis, thrombocytopenia and anemia may occur while taking ACE inhibitors. In patients with normal renal function and in the absence of other aggravating factors, neutropenia rarely develops. Perindopril should be used with extreme caution in patients with systemic connective tissue diseases, while taking immunosuppressants, allopurinol or procainamide, especially in patients with impaired renal function. Some patients developed severe infections, in some cases resistant to intensive antibiotic therapy. When prescribing perindopril to such patients, it is recommended to periodically monitor the number of leukocytes in the blood. Patients should report any signs of infectious diseases (eg, sore throat, fever) to their doctor. Dual RAACE blockade There is evidence that concomitant use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren increases the risk of hypotension, hyperkalemia and renal dysfunction (including acute renal failure). Thus, double blockade of the RAAS by combined use of ACE inhibitors, angiotensin II receptor antagonists or aliskiren is not recommended (see sections Drug interactions and Pharmacological effects). If dual block therapy is considered absolutely necessary, it should only be carried out under strict medical supervision and with regular monitoring of renal function, blood electrolytes and blood pressure. ACE inhibitors should not be used in combination with angiotensin II receptor antagonists in patients with diabetic nephropathy. Arterial hypotension ACE inhibitors can cause a sharp decrease in blood pressure. Symptomatic arterial hypotension rarely develops in patients without concomitant diseases. The risk of an excessive decrease in blood pressure is increased in patients with reduced blood volume, which can be observed during diuretic therapy, while following a strict salt-free diet, hemodialysis, diarrhea and vomiting, as well as in patients with severe arterial hypertension with high renin activity (see sections Drug interactions and Side effects). In patients at increased risk of developing symptomatic hypotension, blood pressure, renal function and serum potassium levels should be carefully monitored during therapy with Prestance. A similar approach is also used in patients with angina pectoris and cerebrovascular diseases, in whom severe arterial hypotension can lead to myocardial infarction or cerebrovascular accident. If arterial hypotension develops, the patient should be placed in a supine position with legs elevated. If necessary, the bcc should be replenished with the intravenous administration of 0.9% sodium chloride solution. Transient arterial hypotension is not an obstacle to further taking the drug. After restoration of blood volume and blood pressure, treatment can be continued. Mitral stenosis, aortic stenosis, hypertrophic obstructive cardiomyopathy Perindopril, like other ACE inhibitors, should be administered with caution to patients with left ventricular outflow tract obstruction (aortic stenosis, hypertrophic obstructive cardiomyopathy), as well as to patients with mitral stenosis. Amlodipine is contraindicated in patients with left ventricular outflow tract obstruction. Impaired renal function In patients with renal failure (creatinine clearance less than 60 ml/min), individual selection of doses of perindopril and amlodipine is recommended (see Dosage regimen). Such patients require regular monitoring of potassium and creatinine levels in the blood serum (see section Side effects). In patients with bilateral renal artery stenosis or stenosis of the artery of a single kidney during therapy with ACE inhibitors, an increase in serum urea and creatinine levels is possible, which usually resolves when therapy is discontinued. This effect is most often observed in patients with renal failure. The additional presence of renovascular hypertension causes an increased risk of severe hypotension and renal failure in such patients. In some patients with arterial hypertension without signs of renal vascular damage, an increase in the concentration of urea and creatinine in the blood serum is possible, especially when perindopril is co-administered with a diuretic, usually slight and transient. This effect is more often observed in patients with pre-existing renal impairment. Liver failure: In rare cases, cholestatic jaundice occurs while taking ACE inhibitors. As this syndrome progresses, fulminant liver necrosis develops, sometimes with death. The mechanism of development of this syndrome is unclear. If jaundice or a significant increase in the activity of liver enzymes occurs while taking ACE inhibitors, you should stop taking the drug (see section Side effects) and consult a doctor. Ethnic differences Patients of the Black race are more likely than representatives of other races to develop angioedema while taking ACE inhibitors. Perindopril, like other ACE inhibitors, may have a less pronounced antihypertensive effect in patients of the Black race compared to representatives of other races. This difference may be due to the fact that black patients with arterial hypertension are more likely to have low renin activity. Cough During therapy with an ACE inhibitor, a dry cough may occur. The cough persists for a long time while taking drugs of this group and disappears after their discontinuation. This should be taken into account when carrying out the differential diagnosis of cough. Surgery/general anesthesia In patients undergoing major surgery or using anesthetic agents that cause hypotension, the use of perindopril may block the formation of angiotensin II against the background of compensatory renin release. Treatment should be stopped one day before surgery. If arterial hypotension develops according to this mechanism, blood pressure should be maintained by replenishing blood volume. HyperkalemiaHyperkalemia may develop during treatment with ACE inhibitors, incl. and perindopril. Risk factors for hyperkalemia are renal failure, impaired renal function, age over 70 years, diabetes mellitus, some concomitant conditions (dehydration, acute decompensation of chronic heart failure, metabolic acidosis), concomitant use of potassium-sparing diuretics (such as spironolactone and its derivative eplerenone, triamterene, amiloride), as well as potassium preparations or potassium-containing salt substitutes, as well as the use of other drugs that increase the level of potassium in the blood plasma (for example, heparin). The use of potassium supplements, potassium-sparing diuretics, and potassium-containing table salt substitutes can lead to a significant increase in potassium levels in the blood, especially in patients with reduced renal function. Hyperkalemia can cause serious, sometimes fatal, abnormal heart rhythms. If simultaneous use of perindopril and the above drugs is necessary, treatment should be carried out with caution against the background of regular monitoring of potassium levels in the blood serum (see section Drug interactions). Patients with diabetes mellitus When prescribing the drug to patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, during the first month of therapy it is necessary to carefully monitor the concentration of glucose in the blood (see section Drug interactions). Amlodipine The effectiveness and safety of amlodipine in hypertensive crisis has not been established. Heart failure Patients with heart failure should be treated with caution. When using amlodipine in patients with chronic heart failure of functional class III and IV according to the NYHA classification, pulmonary edema may develop. Slow calcium channel blockers, including amlodipine, should be used with caution in patients with chronic heart failure due to a possible increased risk of cardiovascular adverse events and mortality. Liver failure: In patients with impaired liver function, T1/2 and AUC of amlodipine are increased. Recommendations for dosing of the drug have not been established. Taking amlodipine should be started with the lowest doses and precautions should be taken both at the beginning of treatment and when increasing the dose. In patients with severe hepatic impairment, the dose should be increased gradually, ensuring careful monitoring of the clinical condition. Elderly patients In elderly patients, dose increases should be carried out with caution (see sections Dosage regimen and Pharmacokinetics). Renal failure Patients with renal failure can take amlodipine in standard doses. Changes in plasma concentrations of amlodipine do not correlate with the degree of renal failure. Amlodipine is not excreted from the body by dialysis. PrestanceSpecial instructions regarding amlodipine and perindopril also apply to the drug Prestance. Excipients Due to the presence of lactose in the drug, Prestance should not be prescribed to patients with hereditary lactose intolerance, lactase deficiency and glucose/galactose malabsorption syndrome. Effect on the ability to drive vehicles and operate machinery Although no negative effects on the ability to drive vehicles or other complex mechanisms were observed while taking the drug Prestance, however, due to a possible excessive decrease in blood pressure, the development of dizziness, drowsiness and other adverse reactions, caution should be exercised in the listed situations, especially at the beginning of treatment and when increasing the dose.