Diuretics remove excess fluid from the body. Stimulate urine excretion by inhibiting the reabsorption of sodium ions in the renal canals. They have many useful properties. They are widely used in medicine for the treatment of disorders and diseases. The drugs are used for: peripheral edema, for the normal functioning of the kidneys, removal of toxins, removal of excess fluid from cavities, diseases of the heart and blood vessels.
There are several different types of diuretics, differing in chemical structure and mechanism of action. They are divided into: short-acting saline, potassium-containing, taizide. Diuretics are used for weight loss. Removes large amounts of fluid and reduces weight. They have a cleansing effect and remove decay products. They have a positive effect on the condition of the skin and the health of the body. During the period of use, you must adhere to a certain diet and exercise regularly.
History of the origin of diuretics
Over the years, scientists have tried to discover organic and inorganic substances to treat edema. In the early 16th century, weak diuretics were used. Such as sea onion and calomel. In the 20s of the last century, people began to use mercury-containing substances to reduce swelling.
In 1950, the first taizide diuretics, chlorothiazide and hydrochlorothiazide, were synthesized. They are close in chemical structure to sulfonamides. In 1960, the structure of substances was modified. More effective loop diuretics, furosemide and ethacrynic acid, have been created. Diuretics with antikaliuretic activity have been synthesized. The drugs began to be widely used in medicine to treat diseases.
What are diuretics and how do they work?
Source:Me and Medicines (analogues, effects, combinations)
Diuretics, or diuretics, are substances that increase the excretion of urine from the body and reduce the fluid content in the tissues and serous cavities of the body. The increase in urination caused by diuretics is associated with their specific effect on the kidneys, which consists primarily of inhibiting the reabsorption of sodium ions in the renal tubules, which is accompanied by a decrease in water reabsorption. Increased filtration in the glomeruli plays a much smaller role.
Diuretics are mainly represented by the following groups:
a) “loop” diuretics and acting on the cortical segment of the loop of Henle;
b) potassium-sparing diuretics;
c) osmodiuretics.
Diuretics have varying strengths and durations of influence on urine formation, which depends on their physicochemical properties, mechanism of action and its localization (different parts of the nephron).
The most powerful existing diuretics are loop diuretics. According to their chemical structure, they are derivatives of sulfamoylanthranilic and dichlorophenoxyacetic acids (furosemide, bumetanide, ethacrynic acid, etc.). Loop diuretics act throughout the ascending limb of the nephron loop (loop of Henle) and sharply inhibit the reabsorption of chlorine and sodium ions; The release of potassium ions also increases.
Very effective diuretics include thiazides - benzothiadiazine derivatives (hydrochlorothiazide, cyclopenthiazide, etc.). Their effect develops mainly in the cortical segment of the nephron loop, where the reabsorption of cations (sodium and potassium) is blocked. They are characterized by hypokalemia, sometimes very dangerous.
Both loop diuretics and benzothiadiazines are used in the treatment of hypertension and chronic heart failure. By increasing diuresis, they reduce blood volume, respectively, its venous return to the heart and the load on the myocardium, and reduce congestion in the lungs.
Thiazides, in addition, directly relax the vascular wall: metabolic processes in the cell membranes of arterioles change, in particular, the concentration of sodium ions decreases, which leads to a decrease in swelling and a decrease in peripheral vascular resistance. Under the influence of thiazides, the reactivity of the vascular system changes, pressor reactions to vasoconstrictor substances (adrenaline, etc.) decrease and the depressor reaction to ganglion blocking agents increases.
Potassium-sparing diuretics also increase the excretion of sodium ions, but at the same time reduce the excretion of potassium ions. They act in the area of the distal tubules in places where sodium and potassium ions are exchanged. In terms of the strength and duration of the effect, they are significantly inferior to “loop” ones, but do not cause hypokalemia.
The main representatives of this group of drugs - spironolactone, triamterene - differ in their mechanism of action. Spironolactone is an aldosterone antagonist, and its therapeutic activity is higher, the higher the level and production of aldosterone in the body. Triamterene is not an aldosterone antagonist; under the influence of this drug, the permeability of the membranes of the epithelial cells of the distal tubules is selectively reduced for sodium ions; the latter remains in the lumen of the tubule and retains water, which leads to an increase in diuresis.
Drugs from the osmodiuretic group are the only ones that do not “block” urine formation. When filtered, they increase the osmotic pressure of “primary urine” (glomerular filtrate), thereby preventing the reabsorption of water in the proximal tubules.
The most active osmotic diuretics (mannitol, etc.) are used to cause forced diuresis in acute poisoning (barbiturates, salicylates, etc.), acute renal failure, as well as in acute heart failure in patients with reduced renal filtration. They are prescribed as dehydrating agents for cerebral edema.
The use of carbonic anhydrase inhibitors as diuretics is due to the inhibition of the activity of this enzyme in the kidneys (mainly in the proximal renal tubules).
As a result, the formation and subsequent dissociation of carbonic acid is reduced, the reabsorption of bicarbonate ions and Na+ ions by the tubular epithelium is reduced, and therefore the excretion of water significantly increases (diuresis increases). At the same time, the urine pH increases and compensatory, in response to the retention of H+ ions, the metabolic secretion of K+ ions increases. In addition, the excretion of ammonium and chlorine decreases, hyperchloremic acidosis develops, against which the drug ceases to act.
Mechanism of action of diuretics
The main mechanism of action of diuretics is their effect on the kidneys. First of all, on the structural and functional unit or nephron, where the processes of glomerular filtration, tubular reabsorption and secretion occur. To better understand the action of diuretics, it is necessary to consider the process of kidney functioning and the mechanism of urine formation.
Each kidney contains approximately 1 million nephron formations that do not communicate with each other. They consist of a vascular glomerulus (glomerulus), a glomerular capsule and tubules. In the renal glomerulus, plasma is filtered from the capillaries into the capsule cavity. The endothelium of the capillaries does not allow the penetration of blood elements and proteins.
The resulting filtrate is called primary urine. Subsequently, it penetrates the kidney tubules. The filtration process in the kidneys occurs due to the difference between the arterial and oncotic pressure of the blood plasma. A decrease in blood pressure leads to a decrease in the filtration rate in the kidneys. Increasing blood pressure increases the filtration rate.
The glomerular filtration rate depends not only on the blood supply to the kidneys, but also on the number of functioning nephrons. On average, glomerular filtration in an adult is 100 ml per minute. Every day, the human body filters about 200 liters of liquid. Urine is released on average about 2 liters. About 99% of primary urine is reabsorbed in the tubules.
The reabsorption process occurs throughout the nephron. To increase the amount of urine excreted, the glomerular filtration rate must be increased. The process of urine formation ends in the distal nephron and collecting ducts. Transport processes are regulated by hormonal influences. Taking diuretics helps increase the rate of urine formation. Reduce the amount of primary urine that is affected by the reabsorption process.
The clinical use of diuretics almost universally preceded the localization of their site of action. The consequence of diuretic specificity predicts clinical use and side effects, and the proximity of sodium transporters, one to another, often dictates the potency or effectiveness of the diuretic. All diuretics act by inhibiting the normal transport of sodium from the filtrate into the renal tubular cells. This movement of sodium into renal epithelial cells from the apical side is facilitated by a number of transporters, the function of which in turn depends on adenosine triphosphate (ATP), a Na-K dependent cotransporter on the basolateral side of the cell. Growing understanding of the physiology of sodium transport has generated new opportunities for the development of diuretics.
Blood Pressure Tablets: Part I
High blood pressure is one of the most common health problems in Russia. This disease is especially common in older people who have to “take pills” to feel good and relieve stress on the heart. What is blood pressure, why does it rise too much, how diuretic medications help normalize it and how to take them correctly - read about all this in our article.
What is blood pressure
When the heart muscle contracts, it forcefully pushes out a large volume of blood, putting pressure on the walls of the blood vessels. Depending on the location, this pressure is called arterial (BP), venous and capillary. Pushing a fluid as thick as blood through 100 billion capillaries is no easy task. Due to the natural resistance of this complex network of microscopic vessels, the blood pressure “at the entrance” to the heart is much lower than “at the exit” from it.
The blood pressure “at the exit” of blood from the heart (that is, at the moment of its contraction) is called systolic, and the blood pressure “at the entrance” to the heart at the moment of its relaxation is called diastolic.
The average norm for an adult is considered to be 120/80 mm. rt. Art.; The first number in this case means systolic blood pressure, and the second number means diastolic. Thus, normally, the resistance of the capillary network “eats” 34% of the initial “power” of the blood flow.
In practice, the ratio of the two blood pressure readings varies greatly among different people and even within the same person at different points in time. It depends on a number of factors: heart rate, condition of blood vessels, elasticity of their walls (this parameter is skillfully regulated by the brain), etc.
Why is blood pressure rising?
Arterial hypertension (AH), also known as hypertension, is one of the most common diseases in the world. According to the latest WHO data, about 1.13 billion people worldwide suffer from high blood pressure. Blood pressure readings of 140/90 mm are considered elevated. rt. Art. and higher at rest.
The most common symptoms of a hypertensive crisis (a sharp increase in blood pressure in patients with hypertension) are headache, shortness of breath, chest pain and fatigue. Some patients experience dizziness, hear ringing in the ears, or notice redness on the face and chest.
The main cause of hypertension is excessive activity of the renin-angiotensin system (RAS). It is a cascade of chemical reactions that occur in the body in response to a decrease in blood pressure: the enzyme renin contained in the kidneys is converted into the enzyme angiotensin I, and then into angiotensin II. The latter is a powerful vasoconstrictor. The narrower the vessels, the higher the pressure. Angiotensin II also reduces the excretion of sodium and water by the kidneys. The more water in the tissues of the vessels, the smaller their diameter, which means the higher the pressure.
Arterial hypertension is also associated with an excess of calcium in the cells of blood vessels, as well as with an increased concentration of sodium in the vessels and in the blood. Many people know that calcium is good for bones and teeth, but not everyone realizes how important it is for the body as a whole. In fact, calcium is necessary for the transmission of nerve impulses, muscle contraction, blood clotting, the immune response, and so on. Without this metal we would not be able to think, move, or even live.
But in the body, as in life, everything is good in moderation. Calcium overload in vascular cells leads to hypertrophy of their muscle tissue. And this, in turn, means a thickening of the vessel wall and a decrease in its lumen. The “tube” becomes narrower, and, as a result, the pressure on its walls increases.
Why does calcium overload occur? Calcium metabolism in the body is regulated by hormones, and their level, in turn, depends on the concentration of other important substances. Thus, risk factors for hypertension are: obesity, sedentary lifestyle and hyperlipidemia (fat concentration), diabetes, smoking and alcoholism. In addition, old age is a key risk factor.
In the case of sodium, the risk factor is the abuse of salty foods and hormonal disorders that slow down the removal of this element from tissues. Sodium can accumulate in the blood, increasing its volume by binding water molecules. The more blood passes through the vessels per unit time, the greater the pressure on the walls of the vessels. In addition, the accumulation of sodium in the endothelium (a thin layer of cells lining the inside of blood vessels) leads to its swelling (essentially, edema) and, as a consequence, to a narrowing of the lumen of the vessel.
How do diuretics work?
In this article, we will look at only one class of drugs that are used to treat hypertension - diuretics. These medications are designed to “correct the situation” with sodium, while calcium metabolism and the functioning of the RAS are corrected by other drugs, which we will talk about in the following materials.
Diuretics improve the excretion of urine from the body, and along with it, water. Excess sodium and water leave the blood, its volume decreases and blood pressure decreases.
Diuretics act on the nephron, a structural unit of the kidney that performs filtration, reabsorption (reabsorption) and secretion of various substances. They reduce the return of previously “filtered” sodium and potassium ions into the blood. The lower the sodium reabsorption, the lower the water reabsorption. Instead of entering the blood, the water leaves in the urine.
Three types of diuretics are used to treat arterial hypertension: loop, thiazide and potassium-sparing. Loop diuretics are so called because they act on a special part of the nephron - the loop of Henle. Potassium-sparing ones differ from others in their ability to influence only sodium ions. And all thiazide diuretics are derivatives of the substance benzothiadiazine.
The latter are also capable of acting directly on the walls of blood vessels. They reduce the concentration of sodium ions in the endothelium, which reduces its swelling.
Examples of loop diuretics are torasemide and furosemide. Thiazide diuretics include indapamide. Potassium-sparing diuretics include spironolactone and triamterene.
How to take diuretics?
When taking a number of diuretics, especially loop diuretics as the most “powerful” ones, you should remember the risk of hypokalemia (potassium deficiency). It leads to serious problems with various muscle tissues - myalgia, paralysis, breathing problems and intestinal obstruction.
This is a relatively rare condition because potassium is a very common element in food. However, such risks can be caused by a combination of the action of diuretics, which “expel” potassium into the urine and, say, the consequences of prolonged diarrhea or laxative abuse. Also, medications called beta-agonists (salbutamol, fenoterol, etc.) can affect potassium concentration.
In this regard, we recommend that you begin treatment with diuretics only under the supervision of a doctor who will not prescribe incompatible drugs. Obviously, this problem does not apply to potassium-sparing diuretics.
Diuretics do not have strict guidelines for when to take oral forms, however, as is the case with many other drugs, it is better to take them before meals or a couple of hours after. Any medicine is unlikely to benefit from unnecessary interactions with food.
We wish you health, eternal 120/80 and a rational approach to treatment, including professional help from doctors!
Mark Volkov, editor of the online magazine for pharmacists and medical workers “Katren-Style”
Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors
Natural Diuretics
A natural diuretic diet is prescribed when there are contraindications to taking medications. People suffering from problems of the gastrointestinal tract, heart, and respiratory system. Experts include diuretic fruits, vegetables and herbs in weight loss diets.
Products with a diuretic effect:
- Watermelon.
- Cherry.
- Cranberry.
- Blueberry.
- Lemon.
- Melon.
- A pineapple.
- Pomegranate.
- Quince.
- Cabbage.
- Tomatoes.
- Beet.
- Onion.
- Carrot.
- Celery.
- Cucumber.
- Parsley dill.
- Ginger.
- Green tea.
- Nettle.
The products have a mild diuretic effect. Rich in vitamins, minerals and antioxidants. It must be consumed raw, prepared in juices and smoothies. During heat treatment, cooking and long-term storage, the energy value decreases.
Types of diuretics
The main purpose of diuretics is to speed up urine excretion by the kidneys and slow down reabsorption. Different types of diuretics differ from each other in their mechanisms of action. Diuretics remove not only excess fluid from the body, but also important electrolytes. Such as: calcium, magnesium, sodium, potassium, chlorine. It is important to maintain a balance and not increase the established dosages on your own without consulting a specialist.
There are several groups of diuretic drugs:
1. Potassium-sparing.
They have a mild diuretic effect. They act by blocking sodium channels in the epithelium. Reduces potassium excretion by the kidneys. Used in combination with other drugs to stimulate the diuretic and hypotensive effects of thiazide and loop diuretics. Minimize potassium loss. Increase the excretion of sodium, water, salts.
2.Loop
They have a strong diuretic effect. Fast-acting diuretics come in the form of chemically different compounds. They contain a sulfonamide group in their structure. They act in the thick segment of the ascending loop of Henle, located in the kidney. They have a relaxing effect on the smooth muscles of blood vessels. Increases renal blood flow. Reduce the amount of intercellular fluid. Increases the excretion of sodium, chlorine, potassium, magnesium, and calcium from the body.
3. Taizidnye.
Contains sulfonamide derivatives of benzothiadiazine and non-thiazide sulfonamides. They block the transport of calcium and sodium in the distal convoluted tubules. Stimulates the synthesis of prostacyclin.
4. Osmodiuretics.
They have a specific mechanism of action. They delay the reabsorption of water. Does not affect potassium excretion.
Problems of prescribing modern diuretics in patients with CHF
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
— We will ask Professor Grigory Pavlovich Arutyunov to tell us about adequate diuretic therapy for chronic heart failure. Please, Grigory Pavlovich.
00:13
Arutyunov Grigory Pavlovich , Doctor of Medical Sciences, Professor:
— Thank you very much, Vladimir Trofimovich.
Dear Colleagues. Chronic heart failure syndrome is a very well known syndrome since ancient times. Times change, but there is always a big problem in describing this syndrome, in describing the symptoms characteristic of this syndrome.
(Slide show).
Modern clinical portrait of a patient suffering from circulatory failure. Green bars indicate doctors' opinions. Red bars – this is what happens in real clinical practice. Like many centuries ago, for many decades, the first positions are still the feeling of lack of air and clearly pronounced swelling that occurs in these patients.
Whatever new symptoms have appeared in recent years (for example, fatigue - a superbly described syndrome in the last decades of the 20th century), the special significance of old symptoms remains, the fight against which, in fact, is clinically significant in preserving the lives of our patients.
But the word “edema” in the minds of an internist or therapist is primarily associated with the word “diuretic drugs.”
As modern recommendations say, when diuretics should appear in the treatment regimen for circulatory failure. Let's take the simplest patients, the mildest. Circulatory failure, functional class I-II, also sinus rhythm.
Start-up therapy always begins with an ACE inhibitor; in case of intolerance, it is an ARA. Only then, when ACE inhibitors are titrated, in the presence of edema, the therapist has the right to raise the question of diuretic therapy.
If patients have atrial fibrillation, even in this situation, diuretics are not the first line. These are still drugs that correct the patient’s neurohormonal profile. These are glycosides for atrial fibrillation. Only when the rhythm is controlled with titrated drugs does the issue of diuretics come on the agenda.
In more severe patients, functional class III-IV, but still maintaining sinus rhythm, the therapist has the right to administer diuretics for the first time, the first line of drugs.
In patients with atrial fibrillation of functional class III-IV, three drugs are used in treatment. These are ACE inhibitors, diuretics (please note, first-line diuretics) and glycosides.
02:47
We have talked about the first conditional place for diuretics. Let's start with the first law of prescribing diuretics for a therapist. Without edema, there is no diuretic therapy. If there is no material substrate (no edema), the therapist should not think about diuretic therapy in the treatment of CHF.
However, edema itself requires the therapist to understand what kind of edema it is. Let us describe the swelling that requires diuretics. Let us remember Botkin, his description of edema. Patients with circulatory failure must obey the law of symmetry. Symmetrical swelling. Feel the swelling - it should be dense and cold. Check their color - they should be blue.
So, dense, cold, symmetrical swelling is swelling caused by hydrostatic problems and circulatory failure. Then diuretics come on the agenda.
When the law of symmetry is violated, edema becomes one-sided, and there is no place for diuretics. This is a surgical problem that requires a solution, always urgently.
The therapist meaningfully looked at the swelling, felt it, assessed its color, temperature and made a decision on prescribing diuretics.
What do we achieve by prescribing diuretics? First of all, we will influence the removal of sodium and sodium-related chlorine from the body. Since the volume of extracellular fluid is regulated mainly by the content of sodium and chlorine in the body, we will influence the exit of fluid from the body with primary, then secondary urine.
04:41
The law of the power of diuretics. The closer to the nephron, the stronger the effect of the diuretic drug. There are exceptions to this rule. Diacarb does not obey this rule. It acts next to the nephron. But this is not a powerful diuretic drug.
Closest to the level of the loop, loop diuretics will act (hence their name). Thiazide diuretics will continue to work. Potassium-sparing diuretics will act even further. So, we remember the first basic rule. The closer to the nephron, the more powerful the effect of the diuretic drug, with the only exception for the drug Diacarb.
Let's look at the second and third laws. They should always be in the therapist's working memory. Diuretics should not be prescribed discretely. Prescribing diuretics 1-2 times a week, on even or odd days, does not benefit the patient. On the contrary, they begin to shake up the patient’s neurohormonal profile.
What will happen to the patient when he takes diuretics irregularly. For a certain amount of time, the volume of urine produced will increase sharply. The neurohormonal profile will change. In response to the excreted fluid, oversynthesis of angiotensin II and norepinephrine will begin. You will begin to improve your neurohormonal profile.
Diuretics are prescribed daily in small doses, but in no case discretely, which today should not be considered at all in treatment regimens for circulatory failure.
The question of the history of the development of diuretics is very interesting. At the dawn of medicine, herbal remedies were diuretics. Then, quite by accident, during the period of treatment for syphilis, it was discovered that mercury (mercury ointment was used in the treatment of syphilis) has a diuretic effect. Of course, the diuretic drug turned out to be surprisingly toxic.
The era of diuretics is the post-war era. After World War II, when the first effective diuretics were synthesized, which were not so toxic and were clinically highly effective.
The process of synthesizing new drugs has not been completed. Today in the 20th century we are talking about three new classes of diuretics. This is a process that will probably evolve all the time.
But we remembered the history of the synthesis of diuretics only in order to approach the fourth law of prescribing diuretics. Diuretics are prescribed by the therapist according to the principle: from weakest to strongest. This is justified, because the stronger the diuretic effect, the stronger the diuretic drug, the greater its side effects, the greater its toxic effect.
07:40
So, let's look at a diuretic drug that is much weaker than loop diuretics.
This is a thiazide diuretic. It will, first of all, reduce the reabsorption of chlorine. This is his most important thing. Together with chlorine, it will have a passive effect on the excretion of sodium and sodium-bound water.
It is very important to see that the group of thiazide diuretics that we so easily talk about is a very large group. It includes the well-known drug Indapamide, Hydrochlorothiazide, Chlorthalidone, which is better known in other countries than here. However, these are completely different drugs.
This difference in diuretics means that the physician must be aware of the half-life. These half-lives are too different to be consistent across this group. The half-life of a diuretic drug is the most important indicator of a diuretic drug. The longer the half-life, the greater the toxic effect of the diuretic, the less its effect on the neurohormonal profile of our patient.
(Slide show).
Let's look at thiazide diuretics.
Well defined white line. One of the most important side effects of the thiazide diuretic drug (two arrows below the potassium level) is high potassium output. Consequently, high doses of thiazide diuretics will always be fraught with the development of severe arrhythmias. Sodium is excreted significantly less than potassium. This is a very important point.
Finally, thiazide diuretics have a rather toxic effect on the glomerular filtration rate.
09:20
Side effects. The discussion about the dose of thiazide diuretics ended today. 12.5 mg taken with ACE inhibitors is considered safe. Doses lower than 12.5 mg are safe. This is a very important find for us. But we remember that thiazide diuretics will interfere with the lipid spectrum, affect cholesterol levels, and, unfortunately, have a negative effect on blood glucose levels in high doses.
Application. Here the therapist must remember a simple rule. The worse the kidney function, the lower the glomerular filtration rate, the less effective thiazide diuretics. At a figure of 40 ml/min. (glomerular filtration rate calculated by Cockcroft-Gault or MDRD formula) thiazide diuretics are practically ineffective. This is a very important point when we build a daily treatment regimen for patients.
Loop diuretics are much more effective than thiazide diuretics. The point of action of a loop diuretic is the thick segment of the ascending limb of the loop of Henle. This site will reabsorb 25% of the filtered sodium. If we block the entry of sodium back, then water will leave along with the sodium.
Why are loop diuretics so effective? Along with sodium, other electrolytes will also leave. We are talking about calcium and magnesium. High doses will still interfere with the electrolyte balance and may cause rhythm disturbances in the patient.
A loop diuretic removes sodium much more than a thiazide diuretic, but at the same time it also affects the level of potassium excretion. Any diuretic drug, interfering with the electrolyte balance, will be fraught with rhythm disturbances.
Let's not forget that a large volume of water leaves along with the excreted sodium. Therefore, there will be a direct effect on hematocrit. If you are treating a bedridden patient, then ideal conditions will be created for deep vein thrombosis of the leg. Loop diuretics in high doses will always produce high levels of water excreted from the body. The therapist should always keep in mind the high probability of not only rhythm disturbances, but also thrombosis of the deep veins of the leg with possible embolic syndrome in the pulmonary artery.
Toxic effect. The most important indicator on which the patient’s life expectancy largely depends is the glomerular filtration rate. There are no negative effects here with moderate doses. However, there will be a sharp decrease in glomerular filtration rate with high doses of loop diuretics.
12:32
Let's come to the class of loop diuretics.
They are also very different from each other. These are ethacrynic acid, Furosemide and Torasemide. The main indicator by which they differ is the half-life. The second indicator is the metabolism of the diuretic drug. The more a diuretic drug is excreted through the kidney, the more toxic and negative its effect, especially in patients with initially altered kidney function (as in our patients with circulatory failure).
I would like to draw your attention to the doses that are recommended by World Guidelines for administration, for example, Furosemide. Oral, of course, taking 40 mg, 160 mg is not an everyday practice dose, but such practice exists in the world. We must be prepared that doses of loop diuretics will not pass without a trace.
Where will the negative effect of high doses be if taken daily or discretely? If we block the absorption of sodium, then we must clearly remember that after stopping the circulation of the drug in the blood, unfortunately, rebound syndrome will occur. This will be post-diuretic reabsorption. The amount of sodium that will be absorbed from primary urine will increase sharply.
The half-life of the diuretic drug becomes dominant. We should aim for a long half-life to reduce the syndrome of increased post-diuretic reabsorption. This is the first one. But if more sodium is absorbed and the cells are not ready for it, they will die.
Second point. We blocked sodium absorption by 25%. This means that sodium has moved further along the tubules. Unfortunately, cells in distant sections are not ready for such an amount of sodium. This will lead to direct toxic damage.
The third point that the therapist should always remember is the glomerular filtration rate. The lower it is, the higher the concentration at usual doses of the drug, the greater the direct toxic effect of the diuretic drug. We must keep this direct toxic effect of a diuretic drug in our working memory, because it worsens the patient’s condition and shakes his neurohormonal profile.
Finally, remember that Furosemide is the main drug in this group. 65% of it is excreted by the kidneys. Let's remember this number. This is a very important number. It is very high, because Torasemide will be excreted significantly less through the kidney. This becomes important for the therapist when choosing long-term, lifelong therapy with diuretics.
15:21
The main side effects of diuretics. The first and constant effect is the effect on the activity of the renin-angiotensin-aldosterone system. Diuretic therapy will always cause angiotensin II activity to increase and a cascade will follow that will cause high angiotensin II levels. General peripheral vascular resistance will increase, sodium reabsorption will increase, leading to myocardial hypertrophy and hypertrophy of smooth muscle elements.
The second point is the nephrotoxic effect. Any diuretic drug does not remain indifferent to the kidney. It affects the kidney. Finally, we must remember that we are reducing the patient’s quality of life. After the prescription of a diuretic drug, the number of urinations increases. This is significant.
Imagine a real working class 2 patient to whom you have prescribed a diuretic. After taking a diuretic in the morning, the number of urination increases for several hours. At this time he must go to work. We are creating parameters that will worsen his quality of life.
For a very long time we knew that diuretics do not increase life expectancy. According to meta-analyses, they led to an even greater likelihood of deaths, unfortunately.
This was the case until a key study was carried out with the drug Torasemide. For the first time, diuretics have been shown to reduce the risk of death in patients with circulatory failure.
17:05
So, the patient received a loop diuretic. However, you see that a certain pattern occurs: the therapist is unable to achieve adequate urine output. What should a therapist do for a patient with circulatory failure. First of all, think about the pH of your urine. We need to acidify the urine.
It is well known that for this purpose there is a diuretic drug from the “reserve group”. We are talking about the drug Diacarb. Prescribing Diacarb for a short course of 5-7 days changes the pH of urine and increases the effectiveness of diuretic therapy with loop diuretics.
This is also a very interesting story about the appearance of Acetozolamide. It was a drug that actually came out of antibiotics. No one will remember it now as an antibiotic. But this is a very interesting diuretic drug, which primarily affects the pH of urine, helping loop diuretics to act.
We are approaching the drugs with the weakest diuretic effect. These are mineralcorticoids. There are two drugs. Spironolactone is justified. Eplerenone is a bit arbitrary. Eplerenone is an aldosterone receptor antagonist with a diuretic effect.
They differ in only one thing. Eplerenone differs from Spironolactone in that it has two radicals that have a sexual effect cut off. Every tenth man on Spironolactone developed gynecomastia. Eplerenone does not have this effect. This is a very interesting connection.
This is a drug that is not considered as an independent diuretic drug, but as a drug added to an already existing diuretic regimen. In normal doses there is no toxic effect. You need to remember the prescription regimen for this drug.
When large doses are used. When the therapist consciously uses large doses. Then, when there is circulatory decompensation and conventional therapy with loop diuretics does not allow “wetting” the patient and achieving a lasting diuretic effect (then large doses are justified).
There are more commonly prescribed smaller doses (25 – 50 mg). These are doses that are prescribed continuously, for life. For a patient with functional class III-IV, since there we achieve not so much a diuretic effect (I beg you to pay attention to this), there we achieve the effect of blocking the D-position of collagens.
This is the first time we are talking about the additional effect of a diuretic drug that does not relate to the kidney at all. We are talking about blocking the D-position of collagen in the body of a person suffering from circulatory failure.
19:50
Let's return to the class of diuretics. They all vary. First of all, we pay attention to half-lives. It was shown in volunteers, young people, that Torasemide has the highest half-life. The higher the half-life, the safer the diuretic.
What we should remember from the pharmacokinetics of Torasemide. The most important drug. Where the use of, for example, Furosemide is ineffective, Torasemide will be more effective.
The long half-life helps you remember two things. It can be used in patients with initially altered kidney function. In an elderly patient, there is no need to modify the dosage.
Let's remember the most important thing. 80% of administered Torasemide is metabolized in the liver. This means that only 20% is excreted through the kidney. This means that this drug can be used in patients with inherently altered kidney function. This sets Torasemide apart from the entire class of loop diuretics, making it safe and widely used.
What does Torasemide do? Look at the word "aldosterone". It's a hormone. Locally in the kidney, due to the fact that the patient has circulatory failure, the renin-angiotensin-aldosterone system turned on. Aldosterone, in addition to affecting sodium levels, will affect local synthesis and D-position of collagen. How serious is this? Let's ask this question and see the answer a little later.
The concentration of potassium and magnesium does not show a peak-like decrease. This means there is no need to expect, or at least the probability of severe rhythm disturbances will not be very high.
21:41
One more thing. The most important thing for the patient. He knows about the level of potassium and sodium, but he does not clearly see the amount of urination that occurs after taking a diuretic drug. Torasemide has a smooth line. It is very important. There will be no sharp deterioration in the patient's quality of life after taking this diuretic drug.
The left ventricular myocardial mass index decreases. Let's ask the question: why? We asked the second question. Why does the mass of the left ventricular myocardium decrease and why is it necessary to influence the level of collagen? Easy enough to explain. Transmitral blood flow actually improves because you change the volume of circulating blood. It's easy to explain. But how to explain the left ventricular myocardial mass index?
Let's look at one more thing - hormones. The circulating blood volume changed, and brain natriuretic peptide decreased. It's clear. But what happened to aldosterone. The diuretic drug Torasemide, in addition to its diuretic effect, has a direct effect on the level of aldosterone activity.
What does this lead to? First of all, to reduce fibrosis. When you and I were born, for each of us the distance between the capillaries and muscle bundles of the myocardium was determined genetically. This distance, which ensured an even supply of nutrients and oxygen, was guaranteed by the amount of collagen between the muscle bundles.
At a young age, thin and delicate threads are collagen. A patient with circulatory failure has an intravital biopsy sample. Collagen cables that are deposited in the myocardium push the bundles apart, making the myocardium thick and electrically unstable. This is, of course, extremely bad.
A diuretic that can not only reduce circulating blood volume but also affect this D-position of collagen will be very important for us.
(Slide show).
Powerful pink fields at the top are on Furosemide. The absence of pink fields at the bottom is on Thorasemid. There is no collagen not only in the kidney, but also in the myocardium. What gives such an effect of using Torasemide. We chose Torasemide from a whole class of loop diuretics. Reliably reduces hospitalization. The total number of hospitalizations is decreasing. The most important thing is that the average patient stay in bed is reduced.
Why are these numbers important to us? This is not just a mechanical reduction in the patient's stay in the hospital. These include fewer deep vein thromboses, less impact on nosocomial infections, and fewer pulmonary embolisms.
24:29
The patient was treated with Furosemide and then switched to Torasemide. Will we succeed? Yes. The use of torasemide after long-term therapy led to a sharp decrease in the number of hospitalizations. This is an essential thing.
For the first time, it was shown that therapy with a diuretic drug led to a decrease not only in overall death, but, more importantly, in a decrease in sudden death. By reducing the D-position of collagen, which led to electrical homogenization of the myocardium. There is no disconnection, no electrical instability (at least much less of it). Naturally, reducing the load and volume. This is very important data for everyday practice.
I specifically show, by way of contrast, studies that were performed long before our understanding of the half-life of loop diuretics. Before the advent of Diuver, a meta-analysis performed on Furosemide, the placebo line was higher than the Furosemide line. This means that the number of deaths was lower on therapy without diuretics.
How then can we help a patient with circulatory failure? We still faced the problem of choosing a diuretic drug. When we took into account the half-life, when we took into account the fact that Diuver interferes with the D-position of collagen, it led to a reduction in mortality and a reduction in hospitalization of patients.
The TORIC study is also important to us because we firmly stated that a diuretic always leads to increased potassium excretion from the body. This means that severe rhythm disturbances are expected. The effect of Torasemide is milder compared to Furosemide in its effect on potassium levels. There is no peak decrease in potassium.
26:36
One more thing. We will now allow ourselves to say that Diuver has a long-lasting effect. It is very important. There is no peak-like fluctuation in the level of neurohormones. Question two: There is no spike in potassium levels, which suggests that severe arrhythmias are unlikely to occur.
A very important fact for a therapist is that sudden death is reduced by almost 70%. This is the first time we are saying that a diuretic drug can have such a powerful antiarrhythmic effect. But still, in the daily practice of a therapist, there are very frequent situations when he has a refractory kidney, when he cannot achieve an adequate amount of urine. How to be.
Let's start with the most common cause of refractoriness. This is incompliance. Patients forget to take diuretics or do not take them regularly. There is concomitant therapy that requires taking non-steroidal anti-inflammatory drugs.
There is one more point. This, unfortunately, is a catastrophic decrease in glomerular filtration rate. If the rate is below 40, then the first thing the physician should do is to stop prescribing Hydrochlorothiazide and consider switching the patient to a daily loop diuretic.
One more issue to pay attention to. Diuretics will never be effective unless you control the renin-angiotensin-aldosterone system. ACE inhibitors are mandatory in any patient receiving diuretic therapy.
Then begins the aerobatics of the therapist - this is combined diuretic therapy. If you don't get results with simple therapy, consider a combination.
Combination stages. There is no effect on a simple loop diuretic - increase the dose. No effect - think about the method of administration. Perhaps the edema syndrome is such that intramuscular or oral administration will not be effective. Then you need to switch to intravenous administration. If administered intravenously, the physician should be aware that different rates will have different diuretic effects.
Let's remember them. Bolus administration will be less effective than drip administration over a long time interval. If you have not achieved an effect on a loop diuretic, combine it with either a thiazide (this is terribly toxic to the kidney, but will be effective in terms of the volume of water excreted) or combine it with Spironolactone. When you add or subtract a diuretic, always remember that Torsemide has the fewest side effects.
29:21
But the most important effect for us will be the law, which sounds like this: having achieved the effect, titrate the diuretic drug to smaller doses. Patients with CHF who receive minimal doses of diuretics live the longest. This is extremely important. This is a snapshot of the modern use of diuretics in the modern treatment of CHF.
What does the future hold for us? Several new classes of drugs. Adenosine receptor blockers. They have now entered the stage of clinical trials. This is Rolofilin. These are necessarily vasopressin receptor antagonists (selective or non-selective). They have already entered everyday practice. These are peptides with a natriuretic effect.
Therapy with diuretics has been and remains a difficult chapter in the daily practice of a therapist, requiring deep knowledge and high aerobatics of the therapist in prescribing diuretics.
Thank you for your attention and the honor you have shown me.
Vladimir Ivashkin : Thank you very much. If you analyze or remember the names of all those who contributed to the creation of this ladder of diuretic effectiveness, do you think the scientist who discovered the diuretic effect of digitalis, and generally found digitalis, would he have received the Nobel Prize? Or was it pushed aside by other more modern manufacturers or creators of diuretics?
Grigory Arutyunov : No, I think they would definitely give it to him, because he turned the vector of clinical thinking. After all, he is an internist, and his understanding of the patient was turned once and for all. There was a completely different perception of the patient, a completely different vision of the future of this patient. I think the contribution he made to history cannot be overstated.
Vladimir Ivashkin: He did not have a chemical laboratory with a large number of employees. He was just thinking.
Grigory Arutyunov: He was a doctor who looked at the patient, touched, listened, and understood.
Vladimir Ivashkin : Thank you very much.
Admission rules
Before taking diuretics, you should consult a specialist. The daily dosage of the drug for the treatment of diseases is prescribed by the doctor. When using diuretics for weight loss, you must follow a drinking regime. To avoid dehydration, you need to drink at least 2 liters of water daily. Maintain a proper and balanced diet. Avoid junk and fried foods, sugar, salt, and alcoholic beverages. Every 2-3 days, weigh yourself in the morning and control your weight. If you feel unwell and side effects occur, you should stop taking it.
The history of the study and practical use of synthetic diuretics goes back just over 50 years. The first thiazide diuretic, hydrochlorothiazide, was synthesized in 1952 and after a relatively short period of time, in 1956, it was introduced into clinical practice. After intensive laboratory research, the loop diuretic furosemide was first used in 1963. The following years were characterized by the active use of diuretics, the accumulation of clinical experience, and the development of new classes of diuretics (osmotic, potassium-sparing). Recent decades in the history of diuretics have been marked by the emergence of drugs with new pharmacological properties (indapamide). Diuretics occupy an important place, first of all, in the treatment of chronic heart failure (CHF), due to their unique pharmacological properties. This circumstance allows us to consider some practical aspects of their use using the example of this nosological form, which represents the final stage of the development of many cardiovascular diseases.
The modern classification of diuretics can be presented as follows [1]:
acting on the glomerulus: - Euphyllin
· acting on the proximal tubule: - osmotic diuretics - Mannitol, Urea, Isosorbitol, Potassium acetate
;
- carbonic anhydrase inhibitors - Acetazolamide
.
· loop: - Furosemide, Ethacrynic acid, Bumetanide, Piretanide, Torsemide
;
· acting on the initial part of the distal tubule: - thiazide sulfonamides - Hydrochlorothiazide, Polythiazide, Cyclopenthiazide, Metolazone
- non-thiazide sulfonamides -
Clopamide, Chlorthalidone, Indapamide, Xipamide
.
· acting on the final part of the distal tubule: - competitive aldosterone antagonists - Spironolactone, Potassium Canreonate
;
- Na transport blockers - Triamterene, Amiloride
.
· herbal diuretics: Bearberry leaf, Birch buds, Lingonberry leaf, Horsetail herb, Juniper fruit, Blue cornflower herb.
· combined diuretics: Triampur, Moduretic.
Diuretics reduce preload and afterload on the heart, eliminate congestion in the internal organs and peripheral edema. The effectiveness of their action depends on which part of the nephron they affect. The most powerful diuretics are furosemide and uregit, as they act throughout the loop of Henle, where the main reabsorption of sodium occurs. The effect of thiazide diuretics, which exert their effect only in the cortical segment of the loop of Henle, is less pronounced. Aldosterone antagonists have weak diuretic activity, but unlike other diuretics, they retain potassium in the body, their effectiveness increases in secondary hyperaldosteronism, and in primary hyperaldosteronism they are the drugs of choice [2].
Diuretics actually used in the treatment of CHF have a number of features. Thiazide and thiazide-like diuretics have a more moderate diuretic and natriuretic effect than loop diuretics; they are ineffective in renal failure; an increase in the diuretic effect with increasing their dose occurs in a very limited range (for hydrochlorothiazide - 25-100 mg).
Loops have a powerful diuretic effect, high efficiency in renal failure, a pronounced dependence of the effect on the dose (furosemide in chronic renal failure is administered up to 2000 mg/day);
Potassium-sparing (relatively weak) drugs are effective for primary and secondary aldosteronism. They can cause hyperkalemia and are often used in combination with other drugs.
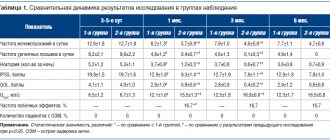
The main diuretics used to treat CHF [5] and their proprietary names are presented in Table 1.
Table 1
The main diuretics used to treat CHF and their proprietary names
| A drug | Proprietary names |
| A) Thiazide and thiazide-like diuretics | |
| Hydrochlorothiazide | Hypothiazide, esidrex |
| Indapamide | Indapamide, indap, natrilix, arifon |
| Xipamide | Aquaphor |
| Chlorthalidone | Hygroton, oxodoline |
| Metolazone | Zaroxoline |
| Cyclopenthiazide | Cyclomethiazide |
| B) Loop diuretics | |
| Bumetanide | Bumex, Bufenox |
| Torasemide | Demadex |
| Furosemide | Lasix, furosemide, furesis |
| Ethacrynic acid | Uregit |
| B) Potassium-sparing diuretics | |
| Amiloride | Midamor, modamide |
| Spironolactone | Veroshpiron, spironol |
| Triamterene/div> | Pterofen, daitek |
Diuretics vary significantly in their pharmacological properties and doses used [2, 4]. Summary data for this section is presented in Table 2.
Table 2
Main pharmacological properties of diuretics most often used in the treatment of CHF
| A drug | Bioavailability (%) | T 1/2, (hours) | Main route of elimination | Initial dose per day (mg) | Duration of action (hours) | Therapeutic doses (mg/day) | Frequency of intake per day |
| Thiazide and thiazide-like diuretics | |||||||
| Hydrochlorothiazide | 60 — 80 | 10 — 12 | kidneys | 25 | 12 — 18 | 25-200 | 1 |
| Indapamide | 90 — 100 | 15 — 25 | kidneys + liver(30%) | 1,25 | 12 — 24 | 1,25 — 2,5 | 1-2 |
| Chlorthalidone | 60 — 65 | 24 — 50 | kidneys + liver | 25 | 24 — 72 | 25-100 | 1 |
| Metolazone | 50 — 60 | 8 — 14 | kidneys + liver | 2,5 | 12-36 | 10 | 1 |
| Loop diuretics | |||||||
| Furosemide | 10 — 90 | 0,3 — 3,4 | kidneys + liver(40%) | 10 — 40 | 6 — 8 | 20 — 200 | 2-1 |
| Bumetanide | 60 — 90 | 60 — 90 0,3 — 1,5 | kidneys + liver | 0,5 — 1,0 | 4 — 6 | 10 | 1 |
| Torasemide | 80 — 90 | 0,8 — 6.0 | kidneys + liver | 5-10 | 24 | 10-100 | 1 |
| Potassium-sparing diuretics | |||||||
| Spironolactone | 60 — 90 | 14 | kidneys + liver(20%) | 25 | 8 — 12 | 25-200 | 2 |
| Triamterene | 50 | 3 — 5 | kidneys + liver | 50 | 12 | 150-300 | 2 |
| Amiloride | 50 | 6 — 9 | kidneys + liver(50%) | 5 | 24 | 5-20 | 1 |
The use of diuretics for CHF is usually associated with loop diuretics. Indeed, furosemide is used most often for heart failure.
Furosemide (Lasix)
causes a fast, powerful, but not long-lasting diuretic effect. Has a fairly pronounced withdrawal syndrome. Enhances the excretion of potassium, phosphates, calcium and magnesium without affecting the glomerular filtration rate, increases the excretion of bicarbonates and increases the pH of urine. Can be used for renal failure. Usually the drug is prescribed orally at a dose of 20-240 mg/day. When taken orally, its effect begins after 1 hour and lasts 4-6 hours. When administered intravenously, the effect occurs after 10-15 minutes and lasts 2-3 hours. Standard regimen The use of furosemide for CHF involves taking the drug orally 1-2 times a week. In case of development of renal failure and in the absence of adequate diuresis from therapeutic doses, the last maximum dose is doubled and continues to be doubled every 30-60 minutes until the effect is achieved (sometimes up to 2-3 g per day).
Ethacrynic acid (uregitis)
somewhat less active than furosemide, otherwise the drugs are similar. Prescribed 50-200 mg/day. The onset of action is after 30 minutes, the maximum effect when taken orally occurs after 2 hours and lasts about 4-6 hours. With intravenous administration, the diuretic effect occurs after 15 minutes and lasts 2-3 hours.
Furosemide and ethacrynic acid, administered intravenously, reduce pressure in the pulmonary artery and filling pressure of the left ventricle, cause veno- and arteriodilatation, which is associated with an improvement in myocardial contractility. The drugs affect different parts of sodium reabsorption (furosemide has an additional effect on the proximal tubule), so they can be prescribed simultaneously or replaced with one another when the diuretic effect decreases. The biotransformation of both drugs is impaired in liver cirrhosis.
Side effects of loop diuretics:
hyperchloremic alkalosis, hypokalemia, hyperuricemia, hyperglycemia, potentiation of toxic effects when used together with antibiotics (cephalosporins, aminoglycosides).
Thiazide and thiazide-like diuretics are somewhat less important in the treatment of CHF.
Hydrochlorothiazide
(hypothiazide, dichlothiazide, Nephrix, Ezidrex) are used orally at 25-200 mg/day, maintenance dose 6.25-12.5-50 mg once a day in the morning, 1-3 times a week. The onset of action is after 2 hours, its peak is after 4 hours, the duration of the diuretic effect is about 10-12 hours. It is most advisable to take hydrochlorothiazide for arterial hypertension associated with CHF, since the long-term and moderate hypotensive effect of this drug largely corresponds to the goals of treating hypertensive diseases.
Klopamide
(brinaldix), unlike other thiazide and other thiazide-like diuretics, increases venous tone (indicated for patients with orthostatic reactions). Used in doses of 10-40 mg in the morning, maintenance dose 10-20 mg once a day or every other day. The onset of action is 1-3 hours, its duration is 8-20 hours. The main feature of the drug is a long-term diuretic effect without forced diuresis.
CHF is quite often a consequence of arterial hypertension, which makes combined treatment of patients with ACE inhibitors and diuretics preferable. Indapamide can be considered one of the drugs of choice among diuretics, which reduces the level of intracellular calcium, preserves magnesium content, reduces the rigidity of the vascular wall and promotes more effective relaxation of the cardiomyocyte in diastole. In this case, there is an increase in the synthesis of prostacyclins, a decrease in platelet aggregation and the release of thromboxane A2, which ultimately has a positive hemodynamic effect by reducing the afterload for the left ventricle. Indapamide is expected to have a cardioprotective effect comparable to ACE inhibitors. The effect of the drug on blood pressure without a significant effect on diuresis is manifested in a daily dose of up to 2.5 mg, with an increase in which the diuretic effect becomes dominant. Take indapamide in the morning, the duration of action is up to 24 hours.
Side effects of thiazide diuretics
: atherogenic and diabetogenic effects, hypokalemia, hyperuricemia. It should be noted that these side effects were noted when studying maximum doses of diuretics and with their long-term use, however, clinical observations show that hypokalemia and hyperuricemia can develop with small doses of thiazides, especially in patients with “compromised” metabolism of electrolytes and purines. The great advantage of indapamide is the absence of rebound syndrome and adverse metabolic disorders (negative effects on carbohydrate and lipid metabolism) when using it.
In recent years, potassium-sparing diuretics have occupied a special place in the treatment of CHF.
Triamterene
(pterophen) as a potassium-sparing agent is used at 25-100 mg/day, with further individual dose selection (no more than 300 mg/day in 2 doses). For CHF, drugs combined with hydrochlorothiazide are often used (Triampur, 1-2 tablets per dose, 1-2 times a day). The onset of action is after 2-4 hours, its peak is 6-8 hours, duration is 7-9 hours. Taking triamterene in the elderly is associated with an increased risk of hyperkalemia and hyponatremia.
Spironolactone
(veroshpiron) has a diuretic effect dependent on the level of aldosterone in the blood plasma. The main feature of the drug’s action is considered to be neuro-hormonal modulation of the activated RAAS. For CHF, it is prescribed together with hydrochlorothiazide or furosemide. Spironolactone is prescribed after the diuretic effect of more active thiazide or loop diuretics wanes after 1-2 weeks of therapy. The onset of action is after 24-48 hours, its peak is 2-3 days of administration, duration is 4-6 days. The drug is prescribed at a dose of 50-100 mg/day in 1-2 doses, but not more than 400 mg/day.
The standard recommended dose, which has the effect of maximum neurohormonal modulation, is 25 mg/day. If it is necessary to increase the potassium concentration in patients with CHF against the background of aggressive diuretic therapy, the dose of spirolactone can be increased to 200-400 mg, but only for a short period of time, since increased doses of veroshpiron help reduce antitumor protection.
Eplerenone
(inspra) is a new potassium-sparing diuretic that is being actively studied at the stage of practical use in the clinic.
Side effects of potassium-sparing diuretics:
hyperkalemia, menstrual irregularities, deepening of voice, hirsutism, gynecomastia.
Potassium-sparing diuretics are contraindicated for hyperkalemia (chronic renal failure or a combination of potassium supplements and ACE inhibitors). The latter circumstance in clinical practice seems to be very relative, since in case of persistent and severe hypokalemia associated with repolarization disorders, arrhythmogenesis, the entire available arsenal is used to increase potassium concentration, including, as a rule, potassium-sparing diuretics, ACE inhibitors and potassium preparations directly.
Diuretic therapy tactics
Diuretics are prescribed when the first signs of edema syndrome appear, and the activity of therapy should directly depend on the degree of its severity [3, 4].
Begin treatment with small doses of thiazide or thiazide-like drugs (25 mg hydrochlorothiazide or equivalent doses of others) to avoid large and rapid losses of water and electrolytes. This is due to the rapid emergence of tolerance to diuretics and activation of the renin-angiotensin-aldosterone and sympathoadrenal systems, antidiuretic hormone, which in CHF plays a leading role in maintaining disturbances of central and peripheral hemodynamics.
As necessary, increase the dosage of drugs; instead of thiazide diuretics, loop diuretics are prescribed or 2-3 diuretics with different mechanisms of action are combined. This allows, with an increase in diuresis, to correct unfavorable electrolyte-metabolic changes and reduce the risk of developing resistance to therapy. To avoid excessive loss of potassium during treatment with thiazide or loop diuretics, it is necessary to limit the intake of table salt (up to 5 g/day) and water (up to 1.5 l/day). It is better to combine thiazide or loop diuretics with one of the potassium-sparing drugs - veroshpiron, triamterene. In patients with CHF outside of emergency situations, taking diuretics should cause fluid loss in a volume of no more than 1.0 l/day (decrease in body weight by 1 kg), so as not to cause a sharp decrease in the volume of circulating blood, which, in turn, adversely affects the systemic hemodynamics and neurohumoral regulation.
For stage II CHF, hydrochlorothiazide is prescribed 50 mg 1-2 times a week, if necessary increasing the dose to 100-150 mg. The effectiveness of treatment is assessed by diuresis, which should increase by 1.5-2 times (1.5-2 liters of urine). For severe edematous syndrome, powerful “loop” diuretics are used. Furosemide is administered 40 mg parenterally or orally 2-3 times a week or more often. If the effect is insufficient, the dose can be increased to 160 mg/day or more. The accumulation of fluid in the abdominal or other cavities indicates the presence of secondary hyperaldosteronism; in such cases, it is advisable to combine furosemide with spironolactone (150-200 mg/day).
It should be borne in mind that active diuretic therapy may be complicated by dehydration, hypokalemia (muscle weakness, anorexia, ST segment depression, decreased T wave amplitude), and hyponatremia. Therefore, as the patient's condition improves, diuretics should be used less frequently and in lower doses.
The causes of resistance to the action of diuretics are: dilution hyponatremia, hyperaldosteronism, active inflammatory process, hypoproteinemia, plethora (polycythemia), arterial hypotension, hypoxia. Patients may become refractory to high doses of diuretics if they consume large amounts of dietary sodium, are taking medications that may block the effects of diuretics (eg, NSAIDs, including COX-2 inhibitors), or have a significant deterioration in renal function or perfusion.
Resistance can be avoided (depending on its cause) by administering sodium chloride solutions, using veroshpiron, anti-inflammatory and antibacterial agents, administering albumin and plasma, bloodletting, using cardiac glycosides and glucocorticoids. Resistance to diuretics can often be overcome by intravenous administration (including the use of continuous infusions), use of two or more diuretics in combination (eg, furosemide and metolazone), or use of diuretics with drugs that increase renal blood flow (eg, positive inotropic agents).
To overcome refractoriness to treatment with diuretics, a more expanded set of methods can be used [5]:
1. Strict restriction of salt intake (not liquid!). 2. Prescribing diuretics only intravenously. 3. Use of high doses of diuretics. There are reports of overcoming refractoriness to therapy when prescribing up to 2000 mg of Lasix. In particularly difficult cases, a bolus injection of Lasix intravenously at a dose of 40-80 mg is recommended, followed by drip administration at a rate of 10-40 mg over 48 hours. 4. Creating conditions for normalizing blood pressure:
- refusal to take vasodilators, most often nitrates prescribed without indications, only due to a diagnosis of coronary artery disease;
- if necessary, use of steroid hormones (prednisolone intravenously up to 180-240 mg and orally up to 30 mg), cordiamine;
- in critical situations, intravenous drip infusion of dopamine is used at a “renal” rate of 0.5-2.0 mg/kg/min, lasting up to 24 hours. In this case, the drug, due to its effect on dopaminergic receptors, in isolation increases the renal fraction of blood flow, glomerular filtration and slightly reduces proximal reabsorption. With an increase in the duration of dopamine administration, as well as with an increase in the infusion rate, other effects of the drug begin to predominate (stimulation of beta-1 and then alpha-1 receptors), accompanied by an increase in blood pressure and inotropic effects, which allow maintaining an acceptable level of glomerular filtration.
5. Normalization of the neurohormonal profile (prescription of ACE inhibitors and aldosterone antagonists). Aldactone (veroshpiron) is best prescribed in the morning, during the maximum circadian rise in aldosterone levels at a dose of 200-300 mg/day. It must be remembered that the drug prescribed orally begins to act only on the 3rd day, so in the first 2-3 days it is better to administer the drug intravenously. 6. Normalization of the protein profile - the use of albumin (200-400 ml/day), together with diuretics, which increases the rate of their filtration. 7. At a sufficient level of blood pressure, it is possible to additionally prescribe drugs that increase the glomerular filtration rate (positive inotropic drugs, aminophylline). 8. Combination of several diuretics. We have already talked about the advisability of combining active diuretics with carbonic anhydrase inhibitors, which avoids the development of alkalosis, under which the effect of thiazide and loop diuretics is weakened. Diacarb, firstly, acidifies the urine, and secondly, due to the disruption of sodium reabsorption in the proximal tubules, it maintains a higher concentration of this ion in primary urine. Because of this, the ascending part of the loop of Henle is more “loaded” with sodium ions and the substrate for the action of loop and thiazide diuretics increases.
Similarly, the combined use of loop and thiazide diuretics increases the flow of sodium ions into the distal tubules, where aldosterone antagonists act, and thereby increases the effectiveness of veroshpiron.
This is an important rule: the prescription of any diuretic drug leads to the fact that due to impaired sodium reabsorption, the “loading” of more distal parts of the nephron with this ion increases. As a result, the effect of diuretics aimed at the underlying tubules is potentiated.
The methods of use and dosage regimens of spironolactone can be presented in the form of the following sequence of actions: 1) assess the severity of CHF (spironolactone should be prescribed only for severe CHF); 2) make sure that the potassium content in the blood serum is below 5.0 mmol/l, and creatinine is below 250 mmol/l; 3) first prescribe spironolactone at a dose of 25 mg/day; 4) assess potassium levels after 4-6 days; 5) if the potassium concentration is from 5 to 5.5 mmol/l, the dose should be reduced by 2 times; if potassium levels are above 5.5 mmol/L, spironolactone should be discontinued; 6) if after 1 month of therapy symptoms of HF persist and there is no hypokalemia, it is advisable to increase the dose of spironolactone to 50 mg/day, followed by assessment of the level of potassium in the blood after 1 week.
Controlled studies have demonstrated the ability of diuretics to increase urinary sodium excretion and reduce symptoms of fluid retention in patients with CHF. In these short-term studies, diuretic therapy led to reductions in central venous pressure, pulmonary congestion, peripheral edema, and body weight, all of which were observed in the first days of therapy. In studies with medium follow-up, diuretics improved cardiac function and exercise capacity, and reduced symptoms in patients with CHF. There have been no long-term studies of diuretic therapy in CHF, and thus the effect on morbidity and mortality is unknown.
Optimal use of diuretics is the cornerstone of any successful approach to the treatment of HF. When using diuretics in patients with CHF, physicians should remember the following points [6]:
1. Diuretics provide clinical improvement more quickly than any other drug for the treatment of CHF. They can reduce pulmonary and peripheral edema within hours or days, whereas the clinical effects of cardiac glycosides, ACEIs, or beta blockers may take weeks or months to become apparent.
2. Diuretics are the only drugs used to treat CHF that can adequately correct fluid retention. Although both cardiac glycosides and low-dose ACEIs can increase urinary sodium excretion, few patients with CHF can maintain sodium balance without the use of diuretics. Attempts to replace diuretics with ACE inhibitors can lead to fluid accumulation in the periphery and in the cavities.
3. Diuretics should not be used as monotherapy in the treatment of CHF. Even when diuretics are successful in controlling symptoms and fluid retention, they alone are not able to maintain clinical stability in patients with CHF over the long term. The risk of clinical decompensation may be reduced when diuretics are combined with digoxin, an ACE inhibitor, or a beta blocker.
4. The use of diuretics in adequate doses and appropriate regimens is a key element in the effectiveness of other drugs used to treat CHF. Inappropriate use and inappropriately low doses of diuretics can cause fluid retention, which may reduce response to ACEIs and increase the risk of complications with beta blockers. In contrast, the use of inappropriately high doses of diuretics will lead to a reduction in volume, which may increase the risk of hypotension with ACEIs and vasodilators and the risk of renal failure with ACEIs and angiotensin II receptor antagonists.
Practical use of diuretics
Patient selection.
Diuretics should be prescribed to all patients with symptoms (and most patients with a previous history) of fluid retention. Diuretics should be combined with an ACEI and a beta blocker (and usually digoxin) [7].
Initiation and implementation of therapy.
The most commonly used loop diuretic for the treatment of CHF is furosemide, but some patients respond favorably to newer agents in this category (eg, torsemide) due to their higher bioavailability. Studies have shown that torsemide may reduce the risk of progression of heart failure more effectively than furosemide, but this issue remains controversial.
In outpatients with CHF, therapy usually begins with low doses of diuretics, and the dose is increased until diuresis increases and body weight decreases, on average, by 0.5-1.0 kg daily. Further increases in the dose or frequency of diuretics may be necessary to maintain active diuresis and weight loss. The ultimate goal of treatment is to eliminate symptoms of fluid retention, either by restoring central venous pressure to normal, eliminating the presence of edema, or a combination of these mechanisms.
Diuretics are usually combined with moderate dietary sodium restriction (less than 3 g daily). If signs of electrolyte imbalance appear, they must be persistently combated and diuretic therapy must be continued. If hypotension or azotemia occurs before treatment goals are achieved, the clinician may elect to reduce diuretic doses, but diuresis should still be maintained until fluid retention is corrected, even if this strategy will result in a modest decrease in blood pressure or renal function as long as the patient remains asymptomatic. Excessive concern about hypotension and azotemia may lead to underprescription of diuretics and the development of resistant edema.
Chronic volume overload not only contributes to the persistence of symptoms, but may also limit the effectiveness and compromise the safety of other drugs used to treat HF.
Once fluid retention has resolved, diuretic treatment should be continued to prevent recurrence of volume overload. Patients are usually prescribed a fixed dose of a diuretic, but the dosage of these medications must be adjusted periodically. In many cases, this adjustment can be made by measuring the patient's body weight daily and providing recommendations for dosage adjustments as body weight increases or decreases beyond certain limits.
The response to a diuretic depends on the concentration of the drug and the time it is eliminated in the urine. Patients with moderate CHF respond favorably to low doses because absorption occurs quickly in the intestine and these drugs quickly reach the renal tubules. However, in advanced CHF, drug absorption may be reduced due to intestinal edema or insufficient intestinal perfusion, and drug delivery may be reduced due to chronically decreased renal perfusion. Consequently, clinical progression of CHF is characterized by the need to increase doses of diuretics.
Dangers of diuretic treatment.
The major adverse effects of diuretics include electrolyte imbalance, hypotension, and azotemia. Diuretics can also cause hearing impairment, but this is usually limited to individual intolerance or occurs when very high doses of the drug are prescribed. Diuretics can cause loss of important cations (potassium and magnesium), which may predispose patients to serious arrhythmias, especially when treated with cardiac glycosides [7, 8]. The risk of electrolyte depletion increases markedly when two diuretics are used in combination. The loss of electrolytes is associated with increased delivery of sodium to the distal renal tubules and the exchange of sodium for other cations, a process that is potentiated by activation of the renin-angiotensin-aldosterone system. Potassium deficiency can be corrected by short-term administration of potassium and, in severe cases, additional administration of magnesium. Concomitant administration of ACE inhibitors or their combination with potassium-sparing agents can prevent electrolyte depletion in most patients taking loop diuretics. When these drugs are prescribed, long-term oral potassium intake is unnecessary and may even be harmful.
Excessive use of diuretics can decrease blood pressure, impair kidney function and exercise capacity. Hypotension and azotemia may also occur as a result of progression of CHF, which may be exacerbated by attempts to reduce the dose of diuretics. If there are no signs of fluid retention, hypotension and azotemia are likely due to a decrease in blood volume and may resolve after reducing the diuretic dose. If symptoms of fluid retention are present, hypotension and azotemia appear to reflect progressive CHF and decreased effective peripheral perfusion. Such patients should be treated with maintenance doses of diuretics and improvement of end-organ perfusion.
The criteria for the positive effect of diuretics in CHF are:
: improvement in the clinical condition of patients (reduction of edema, loss of body weight, shortness of breath, increase in exercise tolerance, etc.), persistent decrease in ventricular filling pressure at rest and during exercise, reduction in the frequency of sudden death, development of acute vascular accidents, increase in duration life.
Thus, the presented analysis, based on the available literature data and practical experience in the use of diuretics, reflects the main clinical aspects of the use of diuretics in chronic heart failure. The authors of the material hope that the background, theoretical and practical information provided in the article will help doctors optimize the prescription of diuretics to patients with CHF.
Literature.
1. Bobrov L.L., Gaivoronskaya V.V., Shcherbak Yu.A., Kulikov A.N., Obrezan A.G., Filippov A.E. Clinical pharmacology and pharmacotherapy of internal diseases (methodological manual), - St. Petersburg. - 2000 - 365 p.
2. Kushakovsky M.S. Chronic congestive heart failure. Idiopathic cardiomyopathies. St. Petersburg: Foliot, 1998. - 320 p.
3. Mareev V.Yu. Diuretics in the treatment of heart failure // Heart failure. - 2001. - T.2, No. 1. — P.11-20.
4. Mareev V.Yu. Recommendations for the rational treatment of patients with heart failure // Consilium medicum. - 1999. - T.1, No. 3. — P.109-147.
5. Obrezan A.G., Vologdina I.V. Chronic heart failure. — St. Petersburg: “Vita Nova.” - 2002. - 320 p.
6. Recommendations for the diagnosis and treatment of chronic heart failure // Heart failure. - 2001. - T.2, No. 6. — P.251-276.
7. ACC/AHA/ Guidelines for the Management of Patients With Chronic Heart Failure //
8. Braunwald E.. Heart disease: a textbook of cardiovascular medicine / Ed. E.Braunwald. — 4th ed. - Philadelphia.: Sounders. - 1992. - 1874, Xl.IV p.
Start
Contraindications and indications for use
Indications:
- Urinary tract diseases.
- Arterial hypertension.
- Renal dysfunction.
- Edema.
- Moist rales in the lungs.
- Rapid weight gain.
- Ascites.
- Hydrothorax.
- Endocrine diseases.
- Increased liver size.
Contraindications:
- Elevated uric acid levels.
- Diabetes.
- Tuberculosis.
- Diseases of the liver, kidneys.
- Pregnancy.
- Lactation period.
- Individual intolerance to components.
- Hepatitis.
- Thrombosis.
- Cancer.
Side effects:
- Dizziness.
- Weakness.
- Fainting.
- Dehydration.
- Nausea.
- Disorders of the gastrointestinal tract.
- Diarrhea.
- Decreased libido.
- Skin rashes.
- Increased blood cholesterol levels.