Throughout life, a person repeatedly experiences abdominal pain. Under the age of 50, most often the cause of pain is not organic, but functional in nature, when drug therapy is most likely to be effective. The cause may be intestinal colic (in children in the first months of life), irritable bowel syndrome, biliary dyskinesia, dysfunction of the sphincter of Oddi, etc. About a third of cases of functional pain are accompanied by spasm of the smooth muscles of the gastrointestinal tract. This is why antispasmodics are so widely used without a doctor’s prescription. Providing a pronounced analgesic effect and normalizing the functioning of the organ, they, unlike non-narcotic and opioid analgesics, do not interfere with the mechanisms of pain, that is, they do not “erase” the picture of the disease, which is critically important in diagnosis.
Nota bene!
When a client asks for a remedy for abdominal pain, it is necessary to exclude urgent situations in order to send the sufferer to a doctor in time. These include:
- Severe pain that prevents you from sleeping or doing anything, lasts longer than 1-2 hours.
- Severe abdominal pain is accompanied by vomiting.
- Severe pain is accompanied by elevated body temperature - 38.5°C and above.
- Severe pain is accompanied by loss of consciousness.
- Severe abdominal pain in a pregnant woman.
- The abdominal muscles are tense and the stomach is as hard as a board.
- Diarrhea mixed with bright red blood.
- The stool is dark and tarry.
- Vomiting blood.
- Abdominal pain is accompanied by vomiting, diarrhea and severe dehydration.
Cellular mechanism of pain
Smooth muscle cells are mainly found in the large intestine. There are significantly fewer of them in the small intestine. The mechanism of cell contraction depends on the concentration of calcium ions in the cytoplasm. The sources of calcium are the extracellular space, connected to the cytoplasm through calcium (slow) membrane channels, as well as the intracellular depot. The release of calcium causes the muscle cell to contract. The contraction of muscle cells forms a spasm and the person feels pain.
The process of muscle contraction is most often triggered by the mediator acetylcholine, binding to muscarinic cholinergic receptors (M-cholinergic receptors). Thus, blockade of M-cholinergic receptors leads to a decrease in tone and relaxation of smooth muscles (and therefore helps relieve abdominal pain). This, in particular, is the basis for the mechanism of action of a group of drugs called M-anticholinergics.
The interaction of calcium with calmodulin leads to the interaction of actin with myosin and cell contraction. CAMP (cyclic adenosine monophosphate) and cGMP (cyclic guanosine monophosphate) weaken the interaction of calcium with calmodulin and also impede the entry of calcium ions into the cell. The level of cAMP and cGMP is controlled by phosphodiesterase (PDE), which destroys excess of these nucleotides. Thus, if you reduce the activity of PDE, the concentration of calcium ions in the cytoplasm will decrease and the tone of the muscle cell will decrease.
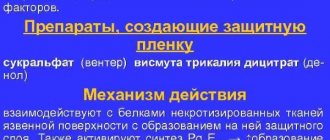
Based on the described mechanisms for regulating the calcium concentration inside the muscle cell, which are disrupted under pathological conditions and lead to spasm, the main groups of antispasmodics have been created:
- M-anticholinergics (atropine, hyoscine butyl bromide).
- PDE IV inhibitors (drotaverine).
- Blockers of calcium release from intracellular stores or sodium channel blockers (mebeverine).
- Calcium channel blockers.
M-anticholinergics
M-anticholinergics are one of the oldest groups of drugs.
Atropine has been used in medicinal herbs since the 4th century BC. e. Thus, the ancient Greek naturalist Theophrastus described mandrake as a remedy for treating wounds, gout and insomnia, and also as a “love potion.” The ancient Greek military physician Dioscorides (1st century AD) described mandrake wine as an anesthetic to treat pain or insomnia, to be given before surgery or cauterization. M-anticholinergics most effectively affect the upper gastrointestinal tract. The use of non-selective M-anticholinergics (atropine, platyphylline, metacin) is limited by their prescription, as well as by the fact that they have a systemic effect and have a number of side effects, such as intestinal atony and obstruction.
One of the relatively oldest selective M-anticholinergics is hyoscine butyl bromide (first registered in Germany in 1951). It acts on the M1 and M3 subtypes of receptors, localized mainly in the walls of the upper gastrointestinal tract, gallbladder and biliary ducts. Hyoscine butyl bromide does not penetrate the blood-brain barrier and has a weak systemic effect, unlike atropine. However, it is contraindicated in people with glaucoma, benign prostatic hyperplasia, as well as organic stenosis of the gastrointestinal tract and tachyarrhythmias. Hyoscine butyl bromide accumulates in the smooth muscles of the gastrointestinal tract and is excreted unchanged by the kidneys. The drug is successfully used for sphincter of Oddi dysfunction, biliary dyskinesia and pyloric spasm.
The severity of the effect of hyoscine butylbromide also depends on the patient’s individual sensitivity to this drug. Unfortunately, the antispasmodic effect of hyoscine butyl bromide on the small intestine (except the duodenum) and large intestine can be realized when taking a dose 2–10 times higher than the therapeutic dose, so its use is useless for spasms in the lower abdomen. A large number of restrictions and risks when taking this drug require medical supervision, which is why the M-anticholinergics known to us are currently used less and less abroad. However, hyoscine butyl bromide is still available without a prescription.
Phosphodiesterase inhibitors (PDE) type IV
These are traditionally widely used antispasmodics: drotaverine hydrochloride and papaverine. Their injectable forms are sold with a prescription, while their tablet forms are available without a prescription. PDE IV is widely present in smooth muscle along the entire length of the intestine, as well as in the biliary and urinary tracts. Thus, blocking PDE IV has a universal antispasmodic effect regardless of the severity of the spasm or its cause. In addition, drotaverine has anti-edematous and anti-inflammatory effects. Drotaverine can be used for acute abdominal pain - both to relieve acute spasms and for long-term treatment of biliary dyskinesia, cholelithiasis, chronic intestinal diseases with spastic syndrome, which are accompanied by colicky or bursting pain. Unlike M-anticholinergics, drotaverine can be used in elderly men with prostate pathology, as well as with concomitant pathology and combined use with other drugs. The therapeutic concentration of drotaverine in plasma when taken orally is achieved after 45 minutes.
Research results and discussion
Initially, on days 3–5 (removal of the urethral catheter), the indicators in the groups were not statistically significantly different. According to the questionnaires, all patients had irritative symptoms that reduced the quality of life. Comparative dynamics of the study results in the observation groups are presented in Table 1.
After 1 month. therapy, positive dynamics were noted in both groups. Statistically significant (p<0.05) in comparison with the initial results, the frequency of urination and nocturia decreased, Qmax increased, and the average score on the IPSS and QOL scales increased. However, the values of these indicators in group 2, in turn, differed significantly (p<0.05) from those obtained in group 1 and were closer to normal.
In group 1, no adverse events were noted. The proportion of patients with side effects in group 2 was 16.7%, but there were no cases of refusal to further participate in the study. Adverse events were identified as dry mouth (13.3%) and constipation (3.3%).
By the end of the 3rd month. observation in group 1, no statistically significant dynamics of parameters were revealed (p>0.05) (Table 1). In group 2, while taking fesoterodine, there was a further significant (p<0.05) decrease in the number of urgent urges, a decrease in the number of daytime and night urination, as well as an increase in Qmax, a decrease in the average score on the IPSS scale and an improvement in the quality of life of patients according to the scale QOL. In this group, these indicators reached normal values.
It should also be noted that there were no new cases of adverse events and episodes of acute urinary retention in both the 1st and 2nd groups.
At the end of 6 months. therapy in both groups, no significant changes were recorded compared to the results of the previous visit, and no new cases of adverse events and acute urinary retention were identified.
As evidenced by the results obtained during the study, all patients with BPH who underwent TUR of the prostate had symptoms of filling after removal of the urethral catheter. This may be explained by both inflammation in the lower urinary tract that persists in the postoperative period and detrusor overactivity. Both groups received anti-inflammatory therapy to eliminate the inflammatory component.
Taking fesoterodine in the 2nd group of patients made it possible to achieve significantly (p<0.05) more significant positive results by the 30th day, which manifested itself in more effective relief of dysuria, an increase in Qmax due to an increase in the effective capacity of the bladder and contributed to improved quality patients’ lives, according to the QOL scale, as evidenced by the preliminary results of the study [12].
Further administration of fesoterodine for 3 months. allowed us to completely normalize the studied parameters in group 2 (against the background of the absence of significant dynamics in group 1), which corresponds to the results of previously published large studies [13–16].
With regard to the safety of therapy with m-anticholinergics in this category of patients, it should be noted that, despite the relatively larger number of adverse events in the group of patients receiving fesoterodine, they were mild or moderate in nature (dry mouth, constipation), none of them led to to patient dropout from the study. However, no serious adverse events or cases of acute urinary retention were recorded. Thus, fesoterodine has a relatively high safety profile among drugs in this group, which is also consistent with the results of studies conducted in European countries [17, 18].
Sodium channel blockers
These drugs block intracellular calcium stores through a cascade of reactions. The most famous drug is a derivative of veratric acid - mebeverine. Unlike anticholinergics, it does not cause hypotension of the colon. Most often, this drug is prescribed for functional disorders of the gastrointestinal tract or as an adjuvant for organic diseases of the gastrointestinal tract. Mebeverine is used only for course treatment. Mebeverine is most effective in combination with other pathogenetic drugs. Mebeverine is mainly available by prescription, but there is a dosage form in tablets that does not require a doctor's prescription.
We will not dwell on calcium channel blockers in more detail, since these drugs do not have any over-the-counter forms.
The over-the-counter myotropic antispasmodic trimebutine stands apart. Trimebutine acts on the enkephalinergic system of the intestine and peripheral opiate receptors - µ, κ and δ. Having an affinity for receptors that enhance and suppress peristalsis, it stimulates the contraction of intestinal smooth muscles in hypokinetic conditions and is an antispasmodic in hyperkinetic conditions. Trimebutine reduces the tone of the esophageal sphincter, promotes gastric emptying and increased intestinal motility, as well as the response of the smooth muscles of the colon to food irritants. It is used for various functional disorders of the gastrointestinal tract.
Read also[edit | edit code]
- Anatomy and physiology of the nervous system
- Parasympathetic nervous system
- Sympathetic nervous system
- Synaptic transmission
- Acetylcholine
- Cholinergic receptors and synapses
- Cholinomimetics
- Nicotine
- M-cholinergic receptor stimulants
- M-cholinergic receptor blockers
- Acetylcholinesterase inhibitors (AChE)
- Poisoning with acetylcholinesterase blockers
- Nerve transmission at neuromuscular synapses and autonomic ganglia N-cholinergic receptors
- Muscle relaxants
- Agents acting on the autonomic ganglia
- Ganglion stimulators
- Ganglioblockers
Ask and choose
How can a pharmacy client choose an over-the-counter antispasmodic from the extensive list of drugs for abdominal pain? Guiding questions will help:
- Does a person have a chronic organic gastrointestinal disease - peptic ulcer of the stomach or duodenum, chronic cholecystitis, chronic pancreatitis, biliary colic, biliary dyskinesia? As a rule, the patient already knows what helps him or what drug the doctor recommended for him during an exacerbation.
- Patient's age? Selective M-anticholinergics are not suitable for the elderly due to the risk of developing intestinal obstruction. Also, antispasmodics have age restrictions for children: mebeverine can be used from twelve years of age, hyoscine butylbromide and drotaverine - from six, trimebutine - from three.
- For women - pregnancy, lactation? The use of antispasmodics during pregnancy is possible only as prescribed by a doctor. PDE inhibitors and trimebutine are contraindicated during lactation. Anticholinergics and sodium channel blockers can be used during lactation.
- Pain in the upper abdomen, possibly accompanied by nausea or vomiting? A selective M-anticholinergic drug is suitable for adults, in the absence of contraindications described in the instructions for a particular drug.
- Pain in the lower abdomen? Type IV PDE inhibitors and sodium channel blockers are suitable.
Sources
- Abdominal pain syndrome in the practice of general practitioner T. M. Benz “News of medicine and pharmacy.” Gastroenterology (239), 2008.
- Pchelintsev M. V. “Anspasmodics: from clinical pharmacology to pharmacotherapy.” Attending Physician 7 (2008): 74–77.
- Mikhailov I. B. Clinical pharmacology (textbook for students of medical universities) - 5th ed., revised. and additional - St. Petersburg: publishing house "Sotis-Med", 2013. - 588 p.
- Yakovenko E. P., et al. "Opiate receptor agonist trimebutine in the treatment of functional disorders of the gallbladder and sphincter of Oddi." Journal "Attending Physician" 2–2014 (2017): 56.
- Tytgat GN. Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain. Drugs 2007; 67:1343–57.
Bronchodilators in the treatment of respiratory diseases
In the structure of respiratory diseases, chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) are the leading causes of morbidity and mortality.
The pathophysiological basis of both nosological forms is bronchial obstruction, the relief or correction of which requires bronchodilator therapy. This provision is enshrined in international and national guidelines for the diagnosis and treatment of BA and COPD [1–6].
It should be noted that asthma and COPD are two independent diseases that have different etiologies, pathogenesis, prognosis, and also require different approaches to treatment. Thus, in particular, ventilation disorders in asthma are characterized by reversible bronchial obstruction and bronchial hyperreactivity, which makes it advisable to use bronchodilators used in this disease. On the contrary, bronchial obstruction in COPD steadily progresses and is only partially reversible. The latter circumstance argues for the feasibility of the clinical use of bronchodilators in this disease.
Naturally, these differences between asthma and COPD require a differentiated approach to both the selection of specific bronchodilators and the tactics of their administration. Thus, if patients with COPD are prescribed bronchodilators mainly on an ongoing basis, then patients with asthma are prescribed more often “on demand” and/or in combination with basic anti-inflammatory therapy (glucocorticosteroids or cromones).
Modern bronchodilators can be divided into three groups, listed below in the order in which they were introduced into clinical practice.
- Anticholinergic (cholinolytic) drugs. By duration of action: short-acting (ipratropium bromide, oxitropium bromide) and long-acting (tiotropium bromide); by route of administration: inhalation only.
- Methylxanthines. By duration of action: short-acting (aminophylline, diaphylline, aminophylline) and long-acting (teopek, theotard, etc.); by route of administration: mainly injection forms - intravenously, intramuscularly (aminophylline, diaphylline) and tablet forms, prolonged theophyllines (micronized forms).
- β2-agonists. By duration of action: short-acting (fenoterol, salbutamol, terbutaline) and long-acting (salbutamol, formoterol); by route of administration: inhalation (short-acting and long-acting β2-agonists), parenteral injection forms, oral tablet forms.
Anticholinergic drugs. For many millennia, traditional medicine has been used to treat respiratory diseases. References to the use of plants of the nightshade family were found in ancient Egyptian papyri. Hippocrates recommended that people with lung diseases use incense and smoke powders prepared from the dried roots and leaves of belladonna (Atropa belladonna), datura (Datura stramonium), and henbane (Hyoscyamus niger). Recent studies have found that the effect of smoking anti-asthmatic cigarettes containing Datura stramonium leaves is comparable to that of modern bronchodilators [7].
By the beginning of the 19th century. The anticholinergic effect of belladonna alkaloids was already known; a little later, scientists established the role of the parasympathetic nervous system in the development of bronchospasm, and since the mid-19th century, cholinergic blockers - atropine and platyphylline, soon synthesized - have become the “gold standard” in the treatment of asthma. The widespread use of anticholinergics for this indication continued until the 70s. XX century Only with the advent of powerful selective β2-agonists, as well as methylxanthines, atropine lost its importance in the treatment of patients with asthma. This was greatly facilitated by the presence of a large number of adverse events accompanying the administration of the drug: dry mouth, impaired mucociliary clearance, mydriasis, etc. [8].
In the 70s XX century Muscarinic receptors in the human respiratory tract were isolated and classified (M1-, M2-, M3 receptors). The establishment of the important role of the parasympathetic nervous system in the control of bronchial patency in asthma gave impetus to further development of anticholinergic drugs, which led to the creation of a fundamentally new drug - ipratropium bromide [8, 9]. However, during clinical trials in patients with asthma, its effectiveness turned out to be low. On the contrary, the drug demonstrated a clear clinical and, in some cases, bronchodilator effect in patients with COPD. Thus, it was possible to prove the partial reversibility of bronchial obstruction in COPD and subsequently establish its two pathophysiological components - reversible and irreversible.
The reversible (“bronchodilator”) component of bronchial obstruction is represented by inflammatory swelling of the mucous membrane of the respiratory tract, accumulation of inflammatory cells, mucus and plasma in the bronchial lumen, spasm of smooth muscles, which are mainly controlled by the parasympathetic part of the autonomic nervous system, the tone of which is naturally increased in COPD [10] .
The irreversible (“emphysematous”) component of bronchial obstruction is caused by the development and progression of pulmonary emphysema and the so-called disease of the small bronchi (decreased elastic traction of the lung tissue due to uneven, predominantly centriacinar emphysema, early expiratory collapse, deformation and narrowing of the small bronchi). It was assumed that these structural changes cannot serve as a point of application for bronchodilators and/or anti-inflammatory drugs. However, later it was possible to establish that it is these changes in the lung parenchyma that cause the formation of hyperinflation of the lungs with the development of an “air trap”, leading to impaired emptying of the alveoli during exhalation (this pathophysiological phenomenon can be most clearly demonstrated when performing physical activity). It is this mechanism that explains the development of such cardiac symptoms of COPD as severe shortness of breath and decreased exercise tolerance, which significantly worsen the quality of life of this category of patients [11].
The most well-known and widely used inhaled anticholinergic drug is currently ipratropium bromide. The drug is well tolerated, effective and safe with long-term use, does not cause the development of tachyphylaxis, and has no cardiotoxic effects. It is important to note that the sensitivity of M-cholinergic receptors does not decrease with age. That is why, in recommendations for the management of patients with COPD, approaches to prescribing this drug are defined as follows: treat “as long as the symptoms of the disease continue to cause inconvenience to the patient” [2].
The duration of action of ipratropium bromide is 4–6 hours, resulting in the need for repeated inhalations (4 times a day), so it is sometimes problematic to control possible deterioration of bronchial obstruction at night or in the early morning hours. Like atropine, ipratropium bromide is not a selective anticholinergic blocker and equally quickly blocks all three types of muscarinic receptors, so the patient should be closely monitored, since blockade of M2 receptors can sometimes lead to paradoxical bronchoconstriction [9].
A representative of the new generation of anticholinergic drugs is tiotropium bromide, registered in Russia in 2003. The peculiarities of the chemical structure of the drug explain the uniqueness of its interaction with muscarinic receptors, namely the unique kinetic selectivity, i.e., differences in the rate of blocking of the corresponding subtypes of muscarinic receptors, as well as increasing the duration of action [12, 13].
In the course of the studies, in particular, it was shown that long-term bronchodilation (~ 24 hours), recorded after a single inhalation of tiotropium bromide, persists even with long-term use (for 12 months) [14, 15]. Already 30 minutes after the first inhalation, the values of forced expiratory volume in the first second (FEV1) and forced vital capacity (FVC) increased, and did not subsequently decrease over the next 24 hours. The greatest bronchodilator effect was observed by the second week of treatment with tiotropium bromide.
Long-term therapy with tiotropium bromide (for 12 months) is accompanied by optimization of bronchial obstruction, regression of respiratory symptoms, and improvement in the quality of life of patients [16]. At the same time, the severity of shortness of breath clearly decreased. The famous pulmonologist P. Jones highly appreciated the possibilities of symptomatic control using inhaled tiotropium bromide, noting its sanogenetic effect: patients who took the drug for a long time no longer experienced shortness of breath during exercise and moved at a pace characteristic of their age [17]. Regression of shortness of breath is explained by a decrease in lung hyperinflation and the size of the “air trap”. Moreover, in the long-term treatment of patients with COPD, it was possible to demonstrate the therapeutic superiority of tiotropium bromide over ipratropium bromide [18].
An important advantage of inhaled anticholinergic drugs is the minimal frequency and severity of adverse events. The most common of these is dry mouth, which, as a rule, does not lead to discontinuation of medications [16, 18].
Methylxanthines. For many decades, methylxanthines (theophylline, etc.) have been used in the treatment of patients with asthma, although the mechanism of their action remained unclear for a long time. In 1859, Dr. Hyde Salter reported that a cup of strong coffee could stop an attack of asthma. In 1888, theophylline was isolated from tea leaves. For a long time, the approach to the use of theophylline was purely empirical and only after the mechanism of its action was clarified in the late 1930s. the drug became widespread. The bronchodilator effect of theophylline occurs through inhibition of phosphodiesterase isoforms with a subsequent increase in intracellular cAMP content and relaxation of smooth muscles of the respiratory tract. In addition, the immunomodulatory and anti-inflammatory effects of theophylline have been established, which allows this drug to be prescribed as monotherapy when it is impossible to use inhaled anti-inflammatory and/or bronchodilator drugs. Short-term use of long-acting theophyllines for 6–12 weeks is accompanied by improved indicators of symptomatic control of the disease and an increase in FEV1 [19, 20].
When discussing the possibilities of using theophylline in patients with broncho-obstructive diseases, it is important to take into account its extrapulmonary effects: improvement of peripheral ventilation, reduction of the development of “air traps”, improvement of diaphragm function, especially with hyperinflation of the lung, improvement (restoration) of mucociliary clearance, dilatation of the arteries of the pulmonary circulation, decreased pressure in the pulmonary artery and hemodynamic “unloading” of the right heart, increased physical performance.
At the same time, it is known that the metabolism of theophylline is subject to significant changes. Thus, in smokers, people suffering from chronic alcoholism, patients taking rifampicin or anticonvulsants, theophylline clearance is accelerated, which means that when using a standard dosage regimen, the plasma concentration of the drug may not reach therapeutic levels. On the contrary, with age, in the presence of arterial hypoxemia (PaO2 < 45 mm Hg), respiratory acidosis, in patients with congestive heart failure, liver cirrhosis, carrying a viral infection, taking macrolides (primarily clarithromycin and erythromycin), fluoroquinolones, cimetidine (but not ranitidine), there is a slowdown in the clearance of theophylline, which means that even with a standard dosage regimen there is a risk of creating toxic concentrations of the drug in the blood plasma.
However, the predictability of effects on the plasma concentration of theophylline makes it possible to either avoid them or change the dose (while monitoring the concentration of the drug in the blood). It has also been shown that when theophylline and salmeterol are used together, the “sum” of adverse events is comparable to the frequency of adverse events with monotherapy with each of these drugs [20].
The second no less serious circumstance limiting the widespread use of theophylline is its small therapeutic breadth, which requires determining the concentration of the drug in the blood plasma. It has been established that the optimal concentration of theophylline in blood plasma is 8–15 mg/l. An increase in concentration to 16–20 mg/l is accompanied by a more pronounced bronchodilator effect, but at the same time it is fraught with the development of a large number of adverse events, especially in patients of older age groups [21]. Meanwhile, recent studies have shown that the anti-inflammatory effect of theophylline is more pronounced when low concentrations of the drug are reached (5–10 mg/l) [22].
Currently, theophylline is usually classified as a second-line drug (in relation to anticholinergic blockers and β2-agonists). They represent a kind of reserve for those patients in whom other areas of bronchodilator therapy do not adequately control the symptoms of the disease. It is also possible to prescribe theophylline to those patients who cannot use inhaled delivery devices.
β2-agonists. Currently, it is difficult to imagine therapy for BA and COPD without β2-agonists. However, the history of the use of β-adrenergic receptor stimulants goes back a little over 100 years.
The basis for the first injection of adrenaline (epinephrine) to a patient with asthma was its vasoconstrictor effect, since it was assumed that bronchial obstruction was based on swelling of the mucous membrane of the respiratory tract. Subsequently, adrenaline was widely used to relieve attacks of bronchial obstruction, both parenterally and inhaled. The short duration of action (up to 1–1.5 hours), a large number of undesirable effects of adrenaline, as a non-selective stimulator of α- and β-adrenergic receptors, prompted scientists to search for new drugs [24].
One of them was isoproterenol, synthesized in 1940, a non-selective β-agonist. It was successfully used in inhalation form, allowing patients suffering from asthma to move freely - first with a glass nebulizer, and then (since 1956) with a metered dose aerosol inhaler. Unfortunately, the duration of action of isoproterenol also did not exceed 1.5–2 hours, and frequent inhalations of the drug contributed to the development of adverse events, in particular life-threatening cardiac arrhythmias.
Subsequent studies of the pharmacological properties of isoproterenol revealed the presence of two subtypes of β-adrenergic receptors: β1- and β2-adrenergic receptors, which made it possible to synthesize the first selective β2-agonist salbutamol soon (1970), and a little later - fenoterol and terbutaline [24] .
β2-agonists cause bronchodilation, this occurs primarily as a result of direct stimulation of β2-adrenergic receptors on airway smooth muscle. They are considered as functional antagonists, causing the reverse development of bronchospasm, regardless of the constrictor effect that has taken place. This property of the drugs is especially important since many proinflammatory mediators have a bronchoconstrictor effect.
β2-agonists are characterized by a rapid onset of bronchodilation (within 5 minutes) and a sufficient duration of action (up to 5–6 hours). However, they continue to be short-acting drugs and require repeated inhalations (usually 4 times a day). The drugs are used primarily by inhalation, although there are other dosage forms - injectable, intended to relieve severe exacerbation of asthma, and oral, to prevent/relieve nocturnal attacks of asthma.
In 1990, the first long-acting, highly selective β2-agonist salmeterol was synthesized, and a little later, formoterol. The duration of action of the drugs reached 12 hours, which made it possible to use them 2 times a day and reliably prevent night/pre-dawn attacks of asthma. Despite the same duration of action, there is a difference between these drugs in the timing of the onset of the bronchodilator effect. If salmeterol begins to act within 30–40 minutes, then formoterol is able to stop an attack of bronchial obstruction within 5 minutes after inhalation, similar to short-acting β2-agonists. Numerous studies evaluating the effectiveness of long-acting β2-agonists have shown that these drugs help reduce the frequency of asthma exacerbations, the number of hospitalizations, and also reduce the need for inhaled glucocorticosteroids (ICS) [3].
The long duration of action of salmeterol and formoterol makes it possible to prevent nocturnal attacks of bronchial obstruction. At the same time, monotherapy with long-acting β2-agonists is recommended only for the treatment of COPD [1, 2, 4]. Recent studies have shown that salmeterol and formoterol, like tiotropium bromide, can influence the size of the “air trap”, thereby increasing the exercise tolerance of COPD patients [25].
A study comparing the effectiveness of tiotropium bromide and formoterol [26] showed that tiotropium bromide is more effective on daytime symptoms of COPD, while formoterol improves pulmonary function parameters at night. This fact also indicates that in some cases it is advisable to combine long-acting anticholinergics and β2-agonists.
In the treatment of asthma, long-acting β2-agonists can only be used in combination with ICS [3]. This is also facilitated by the fact that the addition of long-acting β2-agonists is equivalent to doubling the dose of ICS. As a result of the use of a combination of ICS and long-acting β2-agonists, it was possible to reduce the incidence of adverse events that often develop during anti-inflammatory therapy with ICS. This fact gave rise to the creation of such combination drugs as seretide (a combination of salmeterol and fluticasone) and Symbicort turbuhaler (a combination of formoterol and budesonide). These drugs should be used in the treatment of asthma, but their short-term use in the treatment of COPD is also possible [1–5].
It should be noted that β2-agonists, both short-acting and long-acting, are not free from the development of adverse events. Frequent use of short-acting β2-agonists during the day (more than 4-5 times) and/or monotherapy with long-acting β2-agonists in asthma can mask progressive inflammation of the airways, which in the absence of ICS can cause the development of severe exacerbation of asthma.
Particular attention should be paid when prescribing β2-agonists to elderly patients suffering from concomitant diseases of the cardiovascular system. Firstly, with age, the number and sensitivity of β2-adrenergic receptors in the respiratory tract decrease, which causes a decrease in the therapeutic effectiveness of drugs. Secondly, the prescription of even therapeutic doses can aggravate hypokalemia, which naturally develops in the majority of elderly and old people, which, in turn, can lead to the development of severe, often life-threatening cardiac arrhythmias.
Combined bronchodilator therapy. The combination of an inhaled β2-agonist (short-acting or long-acting) and an anticholinergic blocker is accompanied by an improvement in bronchial obstruction to a greater extent than when prescribing either of these drugs as monotherapy [27]. It is possible to optimize the ventilation function of the lungs to an even greater extent with the simultaneous use of β2-agonists, anticholinergic blockers and theophylline [28]. However, according to popular belief, combination therapy should be used only if it is impossible to achieve an optimal therapeutic effect with any one class of bronchodilators.
In accordance with modern recommendations for the management of patients with COPD, in cases of inadequate control of the disease, combination therapy should be used, for example, Berodual (ipratropium bromide + fenoterol). The use of combination drugs promotes better compliance and significantly reduces the cost of treatment compared to the use of each drug separately.
BA is a disease based on inflammation of the airways, accompanied by reversible bronchial obstruction and changes in the sensitivity of the bronchi and manifested by an attack of suffocation, status asthmaticus, or in the absence of such symptoms of respiratory discomfort (paroxysmal cough, distant wheezing and shortness of breath) against the background of a hereditary predisposition to allergic diseases , extrapulmonary signs of allergy, blood and/or sputum eosinophilia.
The use of bronchodilators in patients with asthma due to the presence of transient bronchial obstruction is certainly justified. However, at present, when the leading role of inflammation in the pathogenesis of asthma is recognized, it is advisable to use anti-inflammatory drugs, and primarily ICS, as a basic therapy for the disease. Monotherapy with β2-agonists, as already noted, can mask progressive inflammation and contribute to the development of severe exacerbations of asthma.
According to the modern concept of stepwise therapy for BA, short-acting β2-agonists should be used as monotherapy only in patients with rare attacks (mild intermittent BA that does not require anti-inflammatory therapy) (see Fig. 1, under the heading “Under glass”). It is necessary to pay attention to the fact that if a β2-agonist is taken more than 4 times a day, both to relieve an attack and to prevent it, it is necessary to prescribe anti-inflammatory therapy corresponding to the next stage of treatment.
At stages II, III and IV, the use of short-acting β2-agonists should also not exceed 4 times a day. Thus, the frequency of administration
Short-acting β2-agonists are a marker of control over the symptoms of the disease, i.e., the adequacy of anti-inflammatory therapy.
Long-acting β2-agonists can be used already at the second stage of treatment, especially in patients with nocturnal or early morning asthma attacks/episodes of respiratory discomfort. It is natural to prescribe long-acting drugs at stages III and IV - in order to potentiate the effect of ICS and possibly reduce the dose of the latter.
As for anticholinergics, the role of tiotropium bromide in the treatment of asthma has not yet been determined. Ipratropium bromide, being inferior in the severity of the bronchodilator effect to β2-agonists, can be added to the complex therapy of severe asthma (IV stage) and/or used to relieve a severe asthmatic attack.
COPD is a disease characterized by chronic bronchial obstruction, which is only partially reversible and slowly progresses over the years. Bronchial obstruction naturally leads to the development of shortness of breath during physical activity, an increasing decrease in tolerance to physical activity - all this limits the activity of patients and leads to a sharp decrease in their quality of life [1, 2, 3].
The cornerstone in the treatment of patients with COPD is therapy aimed at reducing bronchial obstruction. For this purpose, short- and long-acting β2-agonists, anticholinergic drugs, and methylxanthines are used [1–6].
When prescribing bronchodilators to patients with COPD, every doctor must answer two key questions: which bronchodilator to choose and how to use the bronchodilator - “on demand” or on a regular basis?
It should be noted that the issues of choosing bronchodilators are not fully defined and are controversial. This is primarily due to the fact that both β2-agonists and anticholinergic drugs are almost equally effective in COPD: they reduce shortness of breath and improve quality of life. Thus, experts from the European Respiratory Society (ERS) recommend either β2-agonists or anticholinergic drugs, without providing clear criteria for choosing between them [6]. On the contrary, the recommendations of the American Thoracic Society (ATS) [6] and the French Pulmonary Society give preference to anticholinergic drugs (as the drugs of choice in patients with persistent symptoms), while β2-agonists are proposed to be used “on demand” in patients with paroxysmal shortness of breath [3 , 4]. Finally, according to experts from the British Thoracic Society (BTS), β2-agonists should be prescribed initially, and anticholinergic drugs should only be used if sympathomimetics are insufficiently effective or if there is a need to “intensify” bronchodilator therapy [5].
It should be noted that anticholinergics are still preferable for the regular treatment of COPD than β2-agonists. This is explained primarily by the fact that the reversible component of bronchial obstruction is controlled by the parasympathetic division of the autonomic nervous system.
In addition, patients with COPD are, as a rule, elderly and senile people, in whom β2-agonists can naturally cause undesirable effects, and the sensitivity of muscarinic receptors remains until old age.
At the same time, short-acting β2-agonists, characterized by an unsurpassed speed of onset of bronchodilator effect, are most suitable for on-demand therapy. If β2-agonists are poorly tolerated or in order to increase the power of the bronchodilator effect to relieve attacks, it is possible to use combination drugs (Berodual). The dose of β2-agonist in this drug is half that of standard inhalers; in this case, the combination of two drugs potentiates the effect of each other.
As for methylxanthines, as already mentioned, they are “second-line” drugs and are prescribed either for intolerance to inhaled drugs for one reason or another, or as an additive drug when β2-agonists, anticholinergics, or their combination are ineffective.
The preference for prescribing one or another bronchodilator is determined after an inhalation test, and the final decision remains with the patient.
In accordance with modern recommendations, the tactics of bronchodilator therapy for patients with COPD can be presented as follows (see Fig. 2, under the heading “Under glass”).
Stage I (mild) COPD involves the prescription of short-acting bronchodilators on demand. At stage II (moderate course), long-acting bronchodilators—tiotropium bromide or β2-agonists—are added to therapy, with the former being preferable (left side of the regimen), while the prescription of long-acting β2-agonists (right side of the regimen) is alternative. At stage III (severe course), it is advisable to combine one of the long-acting β2-agonists and tiotropium bromide. Stage IV is characterized as extremely severe: the course of the disease with frequent exacerbations - and involves, in addition to bronchodilator therapy, the administration of glucocorticosteroids (inhaled and/or oral).
Literature
- Chronic obstructive pulmonary disease: A practical guide for doctors. Federal program. M., 2004.
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. (Based on the April 1998 NHLBI/WHO Workshop). National Institutes of Healt, National Heart. Lung and Blood Institute. April 2001 (Updated 2003).
- Global Strategy for Asthma Management and Prevention. National Institutes of Health, National Heart, Lung, and Blood Institute REVISED 2002 Updated from: NHLBI/WHO Workshop Report: Global Strategy for Asthma Management and Prevention Issued January, 1995. NIH Publication. No. 2.
- Chronic Obstructive Pulmonary Disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax. 2004; 59; 1.
- British Guideline on the Management of Asthma. Thorax. 2003; 58; 1.
- Celli BR, McNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004; 23: 932-936.
- Trechsel K., Bachofen H., Scherre M. Die bronchodilatorische Wirkung der Asthmazigarette. Scweizerische Medizinische Wochenschrift 1973; 103:415-423.
- Gross NJ editor. Anticholinergic therapy in obstructive airway disease. London, Franklin Scientific Publications, 1993.
- Barnes PJ Muscarinic receptor subtypes in airways. Life Sci. 1993; 52:521-527.
- Barnes P. Tiotropium bromide: a new long-acting anticholinergic bronchodilator. In: Barnes P., Buist AS editors. The role of anticholinergics in chronic obstructive pulmonary disease and chronic asthma. Macclesfied Cheshire, UK: Gardiner-Caldwell Communications Limited; 1997; 126-136.
- Calverley HVA Breathlessness during exercise in COPD: how do the drugs work? Thorax. 2004; 59: 45-457.
- Barnes PJ The pharmacological properties of tiotropium. Chest. 2000; 117: 63-69.
- Disse B., Reichl R., Speck G. et al. DF 679 BR, a novel long acting anticholinergic bronchodilator. Life Sci 1993; 52(5-6): 537-544.
- van Noord JA, Bantje TA, Eland ME et al. A randomized controlled comparison of tiotropium and ipratropium in the treatment of chronic obstructive pulmonary disease. The Dutch Tiotropium Study Group. Thorax. 2000; 55: 289-294.
- O`Donnell DE, Fluge F., Gerken F. et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD/ Eur Respir J/ 2004; 23: 832-840.
- Casaburi R., Mahler DA, Jones PW et al. A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J. 2002; 19: 217-224.
- P. Personal communication. 10th European Respiratory Society Annual Conference (ERS), Florence, Italy, 30 August-3 September 2000. www.medscape.com/ConferenceSearchAll.ctm/.
- Wincken W., van Noord JA, Greefhorst APM et al. on behalf of the Dutch/Belgian Tiotropium Study Group. Improved health patients with COPD during 1-yr's treatment with tiotropium. Eur Respir J. 2002; 19: 209-216.
- Murciano D. et al. A randomized, controlled trial of theophylline in patients with severe chronic obstructive pulmonary disease. N Engl J Med. 1989; 320: 1521-1525.
- ZuWallak RL, Mahler DA, Reilly D. et al. Salmeterol Plus Theophilline Therapy in the Treatment of COPD. Chest. 2001; 119: 1661-1670.
- Shannon M. Life-threatening events after theophylline overdose: a 10-year-prospective analysis. Arch Intern Med. 1999; 159:989-994.
- Torphy TJ State of the art: Phosphodiesterase isozymes: Molecular targets for novel antiasthma agents. Am J Respir Crit Care Med. 1998; 157: 351-370.
- Tsukino M. et al. Effects of theophylline and ipratropium bromide on exercise performance pulmonary disease. Thorax. 1998; 53: 269-273.
- Lawrence D. R., Benitt P. N. Clinical pharmacology: In 2 vols. M.: Medicine, 1991.
- O`Donnell DE, Voduc N., Fizpatrick M., Webb KA Effect of salmeterol on tye ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J. 2004; 24: 86-94.
- Van Noord JA, Aumann J.-L., Jansens E. et al. Comparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPD. Eur Respir J. 2005; 26: 214-222.
- Van Noord JA et al. Long-term treatment of chronic obstructive pulmonary disease with salmeterol and the additive effect of ipratropium. Eur Respir J. 2000; 15: 878-885.
- Karpel JP et al. A comparison of inhaled ipratropium, oral theophylline plus inhaled beta-agonist, and the combination of all three in patients with COPD. 1994; 105: 1089-1094.
- Tashkin D, Cooper CB The role of long-acting bronchodilators in the management of stable COPD. Chest. 2004; 125: 249-259.
I. L. Klyachkina , Candidate of Medical Sciences, Associate Professor of the State Institute of Internal Medicine of the Ministry of Defense of the Russian Federation, Moscow