Chemical properties
Drospirenone - what is it? This substance belongs to the group of oral contraceptives. Most often it is used in combination with other hormones. The drug can have a therapeutic effect on androgen-dependent diseases .
Drospirenone - what kind of hormone is it? Drospirenone is a synthetic hormone, its properties are close to natural progesterone , a derivative of spironolactone . Molecular mass of chemical compound = 366.5 grams per mole. Density of the substance = 1.26 grams per cm3, melting point is approximately 200 degrees Celsius.
Drospirenone is mentioned on Wikipedia in articles about hormonal contraception and the effect of drugs on human sexual function.
Pharmacodynamics and pharmacokinetics
Due to the fact that this substance has pronounced antiandrogenic properties, it has a beneficial effect on the course of androgen-dependent diseases such as acne , alopecia and seborrhea . Drospirenone stimulates the excretion of sodium ions and other fluids from the body, as a result of which blood pressure normalizes, swelling and tenderness in the mammary glands subsides, and body weight decreases.
Clinical studies have shown that after 4 months of using the drug, systolic pressure decreases by an average of 2-4 mm Hg, and diastolic pressure by 1-3 mm Hg. Art., weight decreases by 1-2 kg. During menopause, women are significantly less likely to develop colon cancer , hyperplasia , and endometrial cancer .
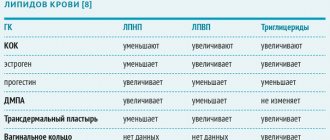
The synthetic hormone does not have estrogenic , androgenic and glucocorticosteroid activity , does not change insulin resistance and the body's response to glucose . During treatment with the drug, the patient's blood cholesterol LDL , and the concentration of triglycerides .
After taking tablets containing Drospirenone, the active substance is quickly and almost completely absorbed by the body. The biological availability of the substance is about 75-85%. Concurrent food intake does not affect the pharmacokinetics of the drug . The concentration of the drug in the blood plasma decreases in two phases, the half-life is 35-40 hours. With systematic, daily use, the equilibrium concentration of the drug is observed after 10 days.
The product has a high degree of binding to plasma proteins (serum albumin ) - about 95-97%. The main metabolites of the hormone are formed without affecting the cytochrome P450 system . The drug is excreted in the form of metabolites in feces and urine, a small part is excreted unchanged.
What will drospirenone change in contraception and hormone replacement therapy?
About the article
19083
0
Regular issues of "RMZh" No. 17 dated September 16, 2005 p. 1139
Category: General articles
Authors: Tarasova M.A. , Lekareva T.M.
For quotation:
Tarasova M.A., Lekareva T.M. What will drospirenone change in contraception and hormone replacement therapy? RMJ. 2005;17:1139.
One of the most important extragenital effects of endogenous progesterone is its antimineralcorticoid effect as a natural aldosterone antagonist. Aldosterone, supporting active sodium absorption and excretion of potassium and hydrogen ions in the urine in the distal renal tubules, performs the biological function of a regulator of extracellular metabolism and water metabolism. In the luteal phase of the menstrual cycle, against the background of increased secretion of progesterone, natriuresis increases [4].
Estradiol and synthetic estrogens have a sodium-sparing effect opposite to progesterone, which is mainly due to an increase in the synthesis of angiotensinogen in the liver and, accordingly, an increase in the level of angiotensin, the main stimulator of aldosterone production. Synthetic progestogens, derivatives of 17a-hydroxyprogesterone and 19-nortestosterone, do not have an antimineralkorticoid effect and do not counteract the stimulating effect of estrogen on the renin-angiotensin-aldosterone system (RAAS). The result of sodium and fluid retention in women taking estrogen-containing drugs for contraception and hormone replacement therapy (HRT) may be weight gain due to fluid retention, swelling and increased blood pressure in predisposed women. Drospirenone is a new progestogen - a derivative of 17a-spironolactone, the spectrum of effects of which is progestogenic, antimineralocorticoid and antiandrogenic, characteristic of natural progesterone. The antimineralocorticoid activity of drospirenone is 8 times higher than that of spironolactone (a diuretic with antimineralocorticoid activity) [5,6]. The results of this property of the drug are a decrease in body weight and a decrease in systolic and diastolic blood pressure. The loss of sodium in the body caused by drospirenone does not lead to a clinically significant increase in potassium concentration, which allows its use even in women with impaired renal function [1]. In a study by Oelkers et al. a significant increase in cumulative sodium excretion was established in a group of healthy women receiving 2 mg of drospirenone compared to the placebo group [7]. It should also be noted that there is an increase in the level of aldosterone in plasma and its excretion in the urine, which, according to the authors, characterizes compensatory activation of the RAAS in response to changes in the electrolyte composition of the blood. The same study showed that drospirenone significantly increases plasma renin activity, and this effect is independent of the dose of the drug. In addition, a slight decrease in body weight was detected in patients taking a drug containing 30 mcg ethinyl estradiol and 3 mg drospirenone (Yarina) [8,9], in contrast to women taking a contraceptive containing 30 mcg ethinyl estradiol in combination with 150 mcg desogestrel, in whom, on the contrary, there was a slight increase in body weight [10,11]. These data indicate that drospirenone in COCs can effectively counteract estrogen-dependent sodium and fluid retention. Drospirenone is also an androgen receptor antagonist. The antiandrogenic activity of drospirenone is 5–10 times stronger than that of progesterone, but lower than that of cyproterone acetate [12–14]. Combined oral contraceptives (COCs), by inhibiting the secretion of androgens by the ovaries, have a positive effect on acne and seborrhea. In addition, ethinyl estradiol (EE) causes an increase in the concentration of sex steroid binding globulin (SHBG), which reduces the free fraction of androgens in the blood plasma. The severity of the androgenic effect of the progestogen included in the combination drugs significantly affects the effects of EE, such as an increase in GSPC and antiatherogenic changes in the spectrum of lipoproteins. Drospirenone does not reduce SHB levels [15] and has an antiatherogenic effect on lipid metabolism [16]. The use of combined estrogen-progestogen preparations containing drospirenone for contraception and hormone replacement therapy allows for additional benefits associated with the pharmacological and clinical characteristics of this progestogen. Contraception with drospirenone Modern hormonal contraceptives provide a real opportunity to regulate the timing of pregnancy and thus reduce the risk of maternal mortality associated with abortion. However, their impact on reproductive health is not limited to this. Estrogen-gestagen contraceptives have numerous non-contraceptive preventive and therapeutic effects: they reduce the abundance, duration and pain of menstrual blood loss, have a positive effect on the condition of the skin, reduce the risk of anemia, ectopic pregnancy, pelvic inflammatory diseases, benign and malignant ovarian tumors, endometrial cancer. Currently, according to WHO (2001), about 100 million women use hormonal methods of contraception. There is no doubt that the relevance of hormonal contraception will continue to increase in the future. The new progestogen drospirenone is part of the combined low-dose monophasic contraceptive Yarin (Schering AG, Germany), containing 30 μg of EE and 3 mg of drospirenone. As is known, the effectiveness of contraceptive methods is determined by the number of pregnancies occurring in 100 women in the first 12 months of using a contraceptive (Pearl index). For Yarina, this figure is 0.07, which meets the criteria for a highly effective contraceptive [17]. Studies of the duration of COC use have shown that about 30% of women stop using the drugs within the first year [18]. The main reason for discontinuation of COCs is side effects [19]. Side effects such as weight gain, breast engorgement and tenderness, and increased blood pressure are associated with the effect of EE on the RAAS. Due to its antimineralkorticoid activity, drospirenone prevents sodium and fluid retention in the body, which maintains stability of body weight and blood pressure levels and prevents engorgement of the mammary glands when taking Yarina. During the first month of use, headache, tension in the mammary glands, decreased libido, and depression occur in 3.1–4.6%; nausea – in 4.6–6.2% of cases. By the sixth month of treatment, all of the above symptoms are mostly relieved [2]. Therapeutic properties of COCs with drospirenone Drospirenone, which has an effect on the RAAS similar to spironolactone, opens up new therapeutic possibilities for the use of COCs. This primarily applies to the treatment of premenstrual syndrome (PMS). At least 95% of women of reproductive age, to one degree or another, a few days before menstruation, experience symptoms such as irritability (93.8%), engorgement and tenderness of the mammary glands (87.5%), flatulence (75%), headache (56.3%), mood changes with a tendency towards depression (56.3%), swelling (50%) [3]. The use of COCs is the most common therapeutic strategy for PMS. However, the severity of PMS symptoms does not always decrease, and may even worsen, which is associated with a deficiency of natural progesterone. Numerous clinical studies have shown the positive effect of the drug Yarina on the somatic and psycho-emotional symptoms of PMS. In an open, uncontrolled study conducted by Apter D. et al. [20]. The effectiveness of the drug was assessed in 336 women aged 18 to 42 years using the health questionnaire The Psychological General Well-Being Index (PGWBI), which includes indicators such as anxiety, low mood, general well-being, ability to control one’s emotions, and overall health , activity. After three cycles of treatment, there was a trend toward improvement, and after six cycles, a statistically significant increase in overall well-being was detected. In addition, the severity of somatic symptoms was assessed. A decrease in the symptoms of bloating and engorgement of the mammary glands occurred by the 6th cycle of taking the drug in 77.3 and 69% of women, respectively. In addition, in 52% of cases, patients noted a decrease in swelling of the extremities. Body weight remained stable or even decreased slightly. Although this study did not include a placebo group, this shortcoming was compensated for by the duration of treatment (12 months), because It is known that after 3–6 months the placebo effect is leveled out [21]. In another study conducted in the USA in 2002, Borenstein J. et al. assessed the effect of the drug on premenstrual symptoms and quality of life in more than a thousand women suffering from PMS. Premenstrual symptoms and quality of life were assessed before treatment and after two cycles of treatment. The use of Yarina led to an improvement in the physical and psycho-emotional symptoms of PMS, as well as overall well-being and quality of life [22]. Boschitsch E. et al. studied the effectiveness of using Yarina and a drug containing 30 mcg of EE and 150 mcg of desogestrel in the treatment of PMS. In the group of women receiving Yarina, a significant decrease in body weight was noted. In addition, there was a statistically significant decrease in the severity of premenstrual symptoms, such as depressed mood, fluid retention, and increased appetite. The drug had a positive effect on skin manifestations. The number of acne elements decreased by 62.5%, seborrhea decreased by 25.1%. After the end of the study, 75.6% of women expressed a desire to continue taking the drug [23]. In a study by Brown C. et al. 326 women aged 18 to 35 years filled out the 23-component Women's Health Assessment Questionnaire at the beginning of observation and after completing the 6th cycle of taking Yarina. At the end of cycle 6, there was an improvement in scores on scales characterizing fluid retention and emotional status. It should be especially noted that the results were similar in groups of patients who had not previously used oral contraceptives and used OCs that did not contain drospirenone [24]. In a randomized placebo-controlled study, Freeman EW et al. The effectiveness of the drug Yarina was studied during 3 menstrual cycles in 82 women with severe PMS, the so-called premenstrual dysphoric syndrome. Patients treated with a drug containing EE and drospirenone showed significantly greater improvement in all 22 items on the Calendar of Premenstrual Experiences (COPE) questionnaire. A significant difference between the groups was obtained for factor 3 – constant increased appetite, acne [25,26]. In all of the studies described above, a standard dosage regimen was used: taking 21 tablets followed by a seven-day break. It is known that it is during this period of time that PMS symptoms more often recur in women taking oral contraceptives [27]. The use of an extended COC regimen, when the patient receives the drug daily for 9–12 weeks and only then takes a break, increases the effectiveness of PMS therapy. A decrease in symptoms in this case is noted by 74% of women [28]. When using this regimen, breakthrough bleeding is quite rare; a menstrual-like reaction occurs when the pills are discontinued [29]. Taking these data into account, a study was conducted on the use of Yarina in an extended regimen [30]. It involved 1,433 women, 175 of whom received the drug continuously for 42–126 days. It was shown that swelling of the extremities decreased by 49% in patients taking the drug in an extended regimen compared to 34% in patients using the standard 21-day regimen. Soreness of the mammary glands decreased by 50 and 40%, respectively, and the feeling of bloating by 37 and 29%. An extended regimen is also more effective in women with acne. The incidence of breakthrough bleeding was 15% at the beginning of therapy and tended to decrease as the drug was continued. There was no increase in the incidence of other side effects. Thus, an extended regimen can be used to increase the therapeutic effectiveness of Yarina. The antiandrogenic properties of COCs with drospirenone are due to several mechanisms: suppression of ovulation, the ability of drospirenone to block androgen receptors and the absence of a decrease in the concentration of sex steroid binding globulin [31]. The use of the drug Yarina is pathogenetically justified in women with excess body weight or increased blood pressure when taking combined contraceptives, as well as those requiring therapy due to premenstrual syndrome, acne, mild arterial hypertension or “idiopathic edema”. Hormone replacement therapy with drospirenone Termination of the estrogen-producing function of the ovaries, leading to the development of vasomotor symptoms, sleep disturbances, decreased resistance to psychological and emotional stress, urogenital and sexual disorders, changes in appearance, osteoporosis, back pain and fractures, significantly reduces the quality of life older women. Correction of all these manifestations is the goal of hormone replacement therapy in peri- and postmenopausal women. Drospirenone is part of a combination drug for continuous HRT in postmenopause Angelique (Schering AG, Germany), containing 17b-estradiol and 2 mg of drospirenone. The use of drospirenone in a combination drug for HRT, similar to Yarina, reduces the incidence of side effects (such as mastodynia, swelling, weight gain due to fluid retention) and improves tolerability of therapy. Increasing the acceptability of therapy (“compliance”) is the most important condition for its maximum effectiveness, since preventive effects are achieved only with a sufficient duration of estrogen therapy. In addition, the antialdosterone effect of drospirenone is especially important for women in older age groups, who have a higher incidence of hypertension and coronary heart disease. It is known that the renin–angiotensin–aldosterone system has a multicomponent effect on the function of the cardiovascular system. Angiotensin II has a strong direct vasoconstrictor effect on the arteries and a less strong vasoconstrictor effect on the veins. In addition, angiotensin II serves as the main stimulator of the production of aldosterone, the main regulator of water and electrolyte balance, acting through mineralocorticoid receptors in the distal tubules of the kidneys. At the same time, it was recently discovered that aldosterone receptors are also located in other organs, including the brain, blood vessels and heart [32]. This indicates the role of aldosterone in the physiology and pathology of the cardiovascular system. Excessive synthesis of aldosterone, which always accompanies the course of heart failure, leads to stimulation of fibroblasts, which, in turn, causes an increase in collagen synthesis, the development of interstitial fibrosis, and disruption of the functional activity of the myocardium with the development of left ventricular diastolic dysfunction. In addition, excessive synthesis of aldosterone promotes increased sodium reabsorption, loss of potassium, retention of water in the renal tubules, which, in turn, leads to an increase in the volume of circulating blood and, as a consequence, to overload of the left ventricle of the heart with volume and pressure, which also leads to progression heart failure. The influence of aldosterone on the development of cardiovascular pathology includes effects on cardiac and vascular fibrosis, hypertension, endothelial dysfunction, suppression of fibrinolysis, and cardiac arrhythmia. It has been shown that the use of the aldosterone receptor blocker spironolactone reduces blood pressure, improves endothelial function, reduces left ventricular hypertrophy, reduces the incidence of fatal arrhythmia and, as a result, leads to a 30% reduction in mortality among patients with severe cardiac pathology [32]. Large cohorts of patients have shown that circulatory levels of norepinephrine, renin, angiotensin II, aldosterone, endothelin-1 and adrenomedulin correlate with both the severity and prognosis of chronic heart failure. In particular, there is a complex relationship between the activity of the renin–angiotensin–aldosterone system and the overproduction of endothelin-1. As the Framingham Offspring Study (Framingham, Massachusetts) showed, even in normotensive individuals, a single measurement of aldosterone in the morning predicted the likelihood of increased blood pressure several years later. A multicenter study examined serum potassium levels and blood pressure levels in postmenopausal women 45–70 years old with and without diabetes mellitus receiving Angeliq and angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers [33]. The women examined showed a hypotensive effect of HRT. In addition, hyperkalemia was not detected in any of the observed groups. The hypotensive effect was also confirmed by the results of a 12-week multicenter, randomized, double-blind, placebo-controlled study of the effect of Angeliq on blood pressure in 212 postmenopausal women with moderate hypertension (BP in the range of 140/90–159/99 mmHg). Compared with the placebo group, women who used Angeliq showed a significant decrease in blood pressure and no significant changes in the potassium content in the blood serum [34]. The presented research results indicate the new capabilities of combined estrogen -gestagenic preparations containing drospirenon as a progestogen component. Due to the anti -mineral of the corticoid and anti -anti -anti -thorough effect of Drospyrenon, the contraceptive drug has good tolerance associated with the preservation of stable weight, the lack of increase in blood pressure, improving the condition of the skin, and efficiency with respect to the relief of premenstrual symptoms. In addition, data were obtained indicating the potential capabilities of the ZGT with Drospirenone to reduce the risk of cardiovascular pathology in women in postmenopausa. Literature 1. Andreeva E.N. and others. New Gestagen opportunities: Drospirenon - progestogen with anti -mineralcorticoid properties. Russian messenger of the obstetrician - gynecologist. 2004; 6. 2. Pasman N.M. Yarina is the first experience of applying an oral contraceptive with the healing properties in Novosibirsk. Russian messenger of the obstetrician - gynecologist. 2005; 1. 3. Mezhreevitinova E.A., Prilepskaya V.N. Premenstrual syndrome. Gynecology 2002; Appendix: 3-8. 4. Oelkers W. Drospirenone, A Progestogen with Antiminaralocorticoid Properties: A Short Review. Mol Cell Endocrinol. 2004 Mar 31; 217 (1–2): 255–61. 5. Losert W, Casals - Stenzel J, Buse M. Progestogenes with Antimineralcorticoid Activity. Arzneimittelforschung 1985; 35: 459–71. 6. Muhn P, Fuhrmann U, Fritzemeier Kh, et al. Drospirenone: A Novel Progestogen with AntimineralCorticoid and Antiandrogenic Activity. Ann Ny Acad Sci 1995; 761: 311–35. 7. Oelkers W, Berger V, Bolik a, et al. Dihydrospirorenone, a New Progestogen with Antimineralcorticoid Activity: Effects on Ovolution, Electrolyte Excretion, and the Rennin -Aldosterone System in Normal Women. J Clin Endocrinol Metab 1991; 73: 837–42. 8. Oelkers W, Helmerhorst FM, Wuttke W, et al. Effect of an Oral Contraceptive Containing Drospirenone on the Rennin - Angiotensin - AldoSterane System in Healthy Female Volunteers. Gynecol Endocrinol 2000; 14: 204–13. 9. Oelkers W, Foidart JM, Dombrovicz, et al. Effects of a New Oral Contraacepting Containing Antimineralcorticoid Progestogen, Drospirenone, On the Rennin - Aldosterone System, Body Weight, Blood Pressure, Glucose Tolener E, and lipid metabolism. J Clin Endorinol Metab 1995; 80: 1816–21. 10. Huber J, Foidart JM, Wuttke W, Efficacy and Tolerance of a Monophasic Oral Contraacepting Containing Ethynilestradiol and Drospirenone. EUR J Contraacept Reprod Health Care 2000; 5: 25–34. 11. Foidart JM, Wuttke W, Bouw Gm, et al. A Comparative Investigation of Contraception ReliaBility, Cycle Control and Tolerance of Two Monophasic Oral Contraception Containing Eithernone Or Desigestral. EUR J Contraacept Reprod Health Care 2000; 5: 124–34. 12. Huber J, Foidart JM, Wuttke W, Efficacy and Tolerance of a Monophasic Oral Contraacepting Ethynilestradiol and Drospirenone. EUR J Contraacept Reprod Health Care 2000; 5: 25–34. 13. Oelkers W, Berger V, Bolik a, et al. Dihydrospirorenone, a New Progestogen with Antimineralcorticoid Activity: Effects on Ovolution, Electrolyte Excretion, and the Rennin -Aldosterone System in Normal Women. J Clin Endocrinol Metab 1991; 73: 837–42. 14. Fuhrmann U, Kratenmacher R, Slateer Ep, et al. The Novel Progestin Drospirenone and Its Natural Counterpart Progesterone: Biochemical Profile and Antiandrogenic Potential. Contraception 1996; 54: 243–51. 15. Van Vloten Wa, Van Haselen CW, Van Zuuren Ej, Gerlinger C, Heithhecker R. The Effect of 2 Combined Oral Contraceptives Containing Either Drosporenone Or Cyprolterone Acetate ON ACTATE ONA Eborrhea. Cutis 2002 APR; 69 (4 SUPPL): 2–15. 16. Gaspard U, Endrikat J, Design Jp, Buicu C, Gerlinger C, Heithecker R. a Randomized Study On the Influence of Oral ContaracepTiving Ethinesystrandiol Combined with malespi Renone or Desogestrel on Lipid and Lipoprotein Metabolism Over a Period of 13 Cycles. Contraception. 2004 APR; 69 (4): 271–8. 17. Huber J, Foidart JM, Wuttke W, Efficacy and Tolerance of a Monophasic Oral Contraacepting Ethynilestradiol and Drospirenone. EUR J Contracept Reprod Health Care 2000; 5: 25–34 18. Pinter B. Continuation and Compliance of Contraceptive Use. Eur J Contracept Reprod Health Care. 2002 SEP; 7 (3): 178–83. Review. PMID: 12428939. 19. Aubeny E. et al. Oral Contraception: Patterns of non - compliance. The Coraliance Study. Eur J Contracept Reprod Health Care. 2002 SEP; 7 (3): 155–61. 20. Apter D, Borsos a, Baumgartner W, Melis Gb, Vexiau - Robert D, Colligs - Hakert a, Palmer M, Kelly S. Effect of ano Contaracepting Containing Drospirenone and Ethinylestraadraadraadraadiol -U ENERAL WELL - Being and FLUID - RELEETED SYMPTOMS. Eur J Contracept Reprod Health Care. 2003 mar; 8 (1): 37–51. 21. Wiklund I, Dimenas E, Wahl M. Factors of Importance When Evaluating of Life in Clinical Trials. CONTROL CLIN TRIALS 1990; 11: 169–79. 22. Borenstein J, Yu Ht, Wade S, Chiou CF, Rapkin A. Effect of an Oral Contraacepting Containing Ethinyl Estraadiol and Drosporenone on Premenstrual Symptomato and Health Ulyity of Life. J Reprod Med. 2003 FEB; 48 (2): 79–85. 23. Boschitch E, Skarabis H, Wuttke W Et Al. The Acceptability of A Novel Oral Contraacepting Containing Drospirenone and Its Effect on Well - Being. The EUR J of Contracept and Reprod Health Care 2000; 5 (SUPPL 3): 34–40. 24. Brown C, Ling F, Wan J. A New Monophasic Oral Contraacepting Containing Drospirenene. Effect on premenstrual symptoms. J Reprod Med. 2002 Jan; 47 (1): 14–22. 25. Freeman Ew, Kroll R, Rapkin A, Pearlstein T, Brown C, Parsey K, Zhang P, Patel H, Foegh M; PMS/PMDD Research Group. Evaluation of a Unique Oral Contraceptive in the Treatment of Premenstrual Dysphoric Disorder. J Womens Health Gend Based Med. 2001 Jul - Aug; 10 (6): 561–9. 26. Freeman EW. Evaluation of a Unique Oral Contraceptive (Yasmin) in the Management of Premenstrual Dysphoric Disorder. Eur J Contracept Reprod Health Care. 2002 Dec; 7 SUPPL 3: 27–34; Discussion 42–3. 27. Sulak P, Scow RD, Preece C, et al. Hormone Withdrawal Symptoms in Oral Contraceptive Users. Obstet Gynecol 2000; 95: 261–6. 28. Sulak Pj, Cressman Be, Waldrop E, et al. Extending the Duration of Active Oral ContraacPontive Pills to Manage Hormone Withdrawal Symptoms. Obstet Gynecol 1997; 89: 179–83 29. Clarke AK, Miller SJ. The Debate Regarding Continous Use of Oral Contraceptives. Ann Pharmacother 2001; 35: 1480–4. 30. Sillem M, Schneidereit R, Heithecker R, et al. Use of an Oral Contraceptive Containing Drospirenone in An Extended Regimen. EUR J Contraacept Reprod Health Care 2003; 8: 162–169. 31. Mansour d Experiences with Yasmin: The Acceptability of aral Contraceptive and Its Effect on Well - Being. EUR J Contraacept Reprod Health Care. 2002 Dec; 7 SUPPL 3: 35–41. 32. Stier TC, Koenig S, Lee Dy, Chawla M, Frishman W. Aldosterone and Aldosterone Antagonism in Cardiovascular Disease: Focus on Eplenone (Inspra) Heart Dis 2003; 5: 10: 102–118. 33. Preston Ra, White WB, Pitt B, Norris PM, Foegh M, Hanes V. Drospirenone/Estradiol Effect on Serum Potassium of PostMenopausal Women at Risk for Hyperkalemia. Obstet Gynecol 2004; 103: 4; 26S - 27S. 34. White WB, Pitt B, Foegh M, Hanes V. Drospirenone with Estradiol Lowers Blood Pressure in PostMenopausal With Systolic Hypertension. Obstet Gynecol 2004; 4, SUPPL., 26S.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Indications for use
The drug is prescribed:
- as part of complex therapy for the prevention of postmenopausal osteoporosis ;
- if it is necessary to carry out hormonal contraception in women with folate or fluid retention in the body;
- as a hormonal replacement treatment for menopausal disorders to eliminate hot flashes , sweating and other vasomotor symptoms;
- with involutional changes in the genitourinary tract in women with an unremoved uterus;
- in combination with other synthetic hormones for contraception;
- for contraception in severe PMS ;
- for severe and moderate forms of acne for contraception.
Contraindications
The medicine is contraindicated:
- patients with allergies to Drospirenone;
- with porphyria ;
- persons with a tendency to form blood clots ;
- with severe liver failure;
- during lactation;
- with thromboembolism or thrombophlebitis in severe form;
- if the patient experiences vaginal bleeding of unknown origin;
- for cancer of the breast or other genital organs;
- pregnant women.
Side effects
During treatment with the drug, the following may develop:
- allergic reactions of varying severity, dizziness;
- thromboembolism of the pulmonary artery or cerebral vessels;
- thrombophlebitis , blood clots in the retinal veins;
- arterial hypertension , swelling, headaches;
- calculous cholecystitis;
- drowsiness , apathy , depression ;
- decreased visual acuity, vomiting, height or weight loss;
- galactorrhea , nausea, hirsutism ;
- alopecia , pain and swelling of the mammary glands;
- bloody or unusual vaginal discharge;
- decreased sexual desire, chloasma ;
- insomnia , decreased seizure threshold, varicose veins .
Interaction
Long-term treatment with drugs that induce liver enzymes ( barbiturates , carbamazepine , oscarbazepine , derivatives , primidone , rifampicin , topiramate , griseofulvin , felbamate ) increases the clearance of this substance and reduces their effectiveness. As a rule, this effect manifests itself 2-3 weeks after the start of therapy and persists for a month after stopping the medication.
The medicine reduces the effectiveness of drugs that stimulate uterine smooth muscle and anabolic steroids .
Experience with the use of drospirenone-containing hormonal contraceptives
Gevorkyan M.A., Manukhin I.B., Tikhomirov A.L., Kuznetsova E.M.
Family planning has been an important medical and social problem for many decades. In Russia, this issue is most acute, since the number of abortions continues to remain high. Every second abortion (even without complications) subsequently leads to infertility, which significantly reduces the reproductive potential of the nation. This is especially true for adolescence, when the function of the reproductive system has not yet formed. It is known that the period of puberty is critical in a woman’s life and the influence of various factors (in particular, termination of pregnancy) contributes to disorders of ovarian function and endocrine infertility.
Of all the methods of preventing unwanted pregnancy, the most reliable is the use of oral contraceptives (OCs). The use of intrauterine contraceptives, especially in nulliparous young women, is undesirable due to the risk of developing inflammatory diseases of the pelvic organs and tubal infertility. In recent years, more and more women in Russia prefer OK. In large cities, the number of OK users is up to 15%. And this is undoubtedly due to the improvement of drugs that have minimal side effects. The main reason for both reluctance to take OCs and cessation of their further use is weight gain. In addition, reasons to stop taking OCs include pain in the mammary glands (mastalgia), mood changes, and headaches. All these side effects are mainly caused by estrogens and are aggravated by the progestogen component, so the search for a progestogen that would be as close as possible to endogenous progesterone in properties has continued for decades.
Drospirenone is a new progestogen included in the monophasic OK Midiana (). Drospirenone is a spirolactone analogue and has antimineralocorticoid effects, whereby it prevents estrogen symptoms associated with sodium retention, clinically manifested by weight gain, edema and mastalgia. This is a very important advantage of Midiana, which allows it to be used for PMS (premenstrual syndrome), the symptoms of which can be observed in more than 50% of women of reproductive age.
In addition, being a derivative of spirolactone (which has long been known as a peripheral androgen receptor blocker), drospirenone is effective in the treatment of dermatological manifestations of hyperandrogenism, especially acne. It is known that all estrogen-containing OCs have an antiandrogenic effect, which is based on an increase in the concentration of sex steroid binding globulins (SGBS) in the blood, resulting in a decrease in the free (biologically active) fraction of androgens. However, most progestogens of the previous generation neutralized these effects. Drospirenone does not affect the estrogen-induced increase in GSPC levels in the blood. These antiandrogenic effects of drospirenone provide women with additional non-contraceptive benefits.
To determine the effectiveness and side effects of the new OC Midiana, our study included 54 women aged 16–40 years (average age 26±1.6)), of which 34 were “switched” from other OCs and 20 were starting to use OCs for the first time . The drug was used for 6 cycles (total 324 cycles). Taking into account our extensive experience, to reduce the frequency of acyclic bleeding in those using OCs for the first time, it was recommended to use the drug from the 5th to the 25th day of the cycle with additional barrier contraception in the 1st cycle.
During the observation process, contraceptive reliability was assessed, which was 100%, which may be due to the short duration of observation (6 cycles). In addition, the nature of side effects was assessed, the frequency of which was higher in novice users.
Acyclic bleeding was not observed in 96% of cycles. In 3.7% of cycles, spotting was observed in cycles 1–2; the frequency of cycles with breakthrough bleeding was only 0.3%. Only one woman (from beginners) refused to continue taking OCs due to these side effects.
Weight gain (minor, 1–2 kg) was observed in 5 women (9.3%), mostly novice users of OCs, which can most likely be explained by the estrogenic component of OCs. However, this was not a reason to stop taking the drug. These women were satisfied with the additional benefits of Midiana, in particular the regression of acne. Of interest are 28% of women (all of whom “switched” from other OCs) who noted weight loss on the background of Midiana, which is associated with the antimineralocorticoid effect of drospirenone.
Soreness of the mammary glands (mastalgia) was noted by 3 women (5.6%) - all of them started taking OCs for the first time. These effects are also more related to the estrogen component and stopped on the 4th cycle, i.e. optimal time to get used to OK.
Headaches were noted by 11% of women in the first 2 cycles, of which mainly novice OC users. Symptomatic medications stopped these effects, and women continued to take OCs.
Mood changes and nausea were also noted in a small number of women (1.9 and 3.7%, respectively) in the novice user group. It should be noted that women who complained of nausea had a history of dysfunction of the gastrointestinal tract or intestinal dysbiosis after the use of antibacterial drugs. These side effects were observed within 1–3 cycles and were not a reason for refusing further use of OK Midiana.
It should be noted that there was a combination of several side effects in one woman, so the total number of women presenting various complaints is significantly less.
Thus, the low incidence of side effects (11%) while taking the new OC Midiana indicates its good tolerability and high contraceptive effectiveness, which is due to the progestogen (drospirenone), which is as close in structure as possible to endogenous progesterone. This conclusion is also confirmed by the fact that only one woman (1.9%) refused to use OCs due to ongoing breakthrough bleeding. Moreover, acyclic bleeding is observed against the background of any OC.
As noted, OCs of the 21st century have additional advantages, in particular, a positive effect on the condition of the skin and symptoms of PMS, which have a negative effect on the psycho-emotional sphere, reducing the quality of life. Therefore, based on the properties of drospirenone, the effect of OK Midiana on skin condition (acne) and PMS symptoms is of interest.
Effect of OK Midiana on skin condition. Of the 54 women included in the study, 29 took OCs not only for contraception, but also for the treatment of acne. These are mainly young girls aged 16–23 who have not given birth. The choice of OCs in this group of women requires special caution, since long-term use of OCs can lead to a syndrome of hyperinhibition of the gonadotropic function of the pituitary gland. Progestogens close to endogenous progesterone (drospirenone) in OCs have the least pronounced antigonadotropic effect, which is confirmed by our data from ultrasound monitoring of folliculogenesis, which revealed normal follicular growth in 25% of women. The contraceptive effect of the drug is based on the level of suppression of the ovulatory peak of gonadotropins, and to a greater extent - atrophic processes in the endometrium. For the treatment of acne, OK Diane-35 was successfully used for a long time. However, in overweight women it promoted weight gain. 9 women who switched to Midiana not only noted an improvement in their skin condition, but also a decrease in body weight by 2–3 kg.
Effectiveness of treating PMS symptoms. Of the 54 women examined, PMS symptoms were detected in 19. The age of these women was on average 34.5 years, i.e. more senior. At this age, the incidence of metabolic syndrome and other extragenital diseases increases, which requires choosing the safest OC, which includes Midiana. Moreover, in a heterogeneous PMS clinic, there are always symptoms associated with fluid retention (edema, mastodynia), which limited the use of previous generation OCs. The antimineralocorticoid effect of drospirenone opens up new possibilities in the treatment of PMS, observed in the majority of ovulating women of reproductive age. According to the results of this study, after only 3 cycles there was a positive trend in the regression of PMS symptoms, and after 6 cycles all women noted a significant improvement and agreed to continue taking Midiana.
Thus, based on the results of the study and the existing works of foreign authors, we can conclude that the new OK Midiana is a highly effective contraceptive; contains a new progestogen drospirenone, which is as close as possible to endogenous progesterone, and has antimineralocorticoid and antiandrogenic effects. It is drospirenone that promotes stable weight, good tolerability with minimal side effects. Additional benefits - reduction of symptoms of PMS and acne make OK Midiana the drug of first choice today.
Literature
1. Guide to contraception. Edited by V.N. Prilepskaya. M. 2006.
2. Manukhin I.B., Tumilovich L.G., Gevorkyan M.A. Clinical lectures on gynecological endocrinology. M. Geotarmedia. 2009.
3. J.Verchaeghe. Hormonal contraception in women with metabolic syndrome. Contraception Reproductive Health Care. 2010. 5 (5); 305–314.
4. A. Motivala, B. Pitt. Drospirenone fore Oral Contraception and Hormone Replacement Therapy. Drugs. 2007; 7 (5): 47–655.
5. U. Halbreich, T. Backstrom et all. Clinical diagnostic criteria for premenstrual syndrome and guidelines for research studies. Genecolodical Endocrinology. 2007; 23(3); 123–130.
6. G. Paul, C. Bell et al. The real deal: A feasibility study of peer–led sex education for early school leavers. Contraception Reproductive Health Care. 2010. 5 (5); 343–357.
special instructions
A number of uncontrolled randomized studies have revealed an increased risk of venous thromboembolism during treatment with the drug. It is necessary to prescribe the drug with special caution to women who have a predisposition to the occurrence of venous thromboembolism (heredity, obesity , age). It is necessary to carefully compare the risk-benefit indicators.
Rarely during treatment did benign, and even more rarely, malignant liver tumors . If the patient has any signs of this disease, pain in the area under the ribs, organ enlargement and intra-abdominal bleeding, then treatment must be interrupted.
In patients with moderate to mild renal failure, taking this synthetic hormone may affect the concentration of potassium ions in the blood serum. There is a small risk of developing hyperkalemia , especially if the patient is additionally taking potassium-sparing medications .
Before starting treatment with the drug, it is recommended to undergo a gynecological and general medical examination, it is recommended to pay special attention to the cytological examination of the ecclesiastical mucus and mammary glands, the blood coagulation system, and to exclude pregnancy. During therapy, these studies should be repeated periodically.
Drospirenone
Pharmacokinetics
After oral administration, drospirenone is absorbed quickly and almost completely. The Cmax of the active substance in the blood serum is 38 ng/ml and is achieved 1-2 hours after a single dose. Bioavailability is 76-85%. Concomitant food intake does not affect the bioavailability of drospirenone.
Drospirenone binds to serum albumin and does not bind to sex hormone binding globulin (SHBG) or corticoid binding globulin (CBG). Only 3-5% of total serum concentrations of drospirenone exist as free steroids. The ethinyl estradiol-induced increase in SHBG does not affect the binding of drospirenone to serum proteins. The average apparent Vd of drospirenone is 3.7±1.2 l/kg.
During one cycle of treatment, Cssmax of drospirenone in blood plasma is about 70 ng/ml, achieved after 8 days of treatment. Serum concentrations of drospirenone increase approximately 3-fold due to the ratio of final T1/2 and dosing interval.
After oral administration, drospirenone undergoes extensive metabolism. The main metabolites in the blood plasma are the acid form of drospirenone, formed during the opening of the lactone ring, and 4,5-dihydro-drospirenone-3-sulfate, both formed without the participation of the P450 system. Drospirenone is slightly metabolized by CYP3A4 and is capable of inhibiting this enzyme, as well as CYP1A1, CYP2C9 and CYP2C19 in vitro.
T1/2 of drospirenone with a corresponding decrease in its concentration in the blood serum after oral administration is 31 hours. The renal clearance of drospirenone metabolites in the blood serum is 1.5 ± 0.2 ml/min/kg. Drospirenone is excreted only in trace amounts unchanged. Drospirenone metabolites are excreted through the intestines and kidneys in a ratio of about 1.2:1.4. T1/2 of metabolites by the kidneys and through the intestines is about 40 hours.
Css of drospirenone in blood plasma in women with mild renal failure (creatinine clearance 50-80 ml/min) was comparable to the corresponding values in women with normal renal function. In women with moderate renal failure (creatinine clearance 30-50 ml/min), the plasma concentration of drospirenone was on average 37% higher than in women with normal renal function. Drospirenone therapy was well tolerated in women with mild to moderate renal impairment. Taking drospirenone did not have a clinically significant effect on serum potassium levels.
In a single-dose study, oral clearance in volunteers with moderate hepatic impairment was reduced by approximately 50% compared with subjects with normal hepatic function. The observed decrease in drospirenone clearance in volunteers with moderate hepatic impairment does not lead to any significant differences in serum potassium levels. Even with diabetes mellitus and concomitant use of spironolactone (two factors that can provoke hyperkalemia in the patient), there was no increase in serum potassium above the ULN. It can be concluded that drospirenone is well tolerated by patients with mild to moderate hepatic impairment (Child-Pugh class B).
Drugs containing (Analogs)
Level 4 ATX code matches:
Trisequence
Silhouette
Angelique
Divina
Claira
Hormone Drospirenone in contraceptives: Angelique , Angelique Micro (with estradiol ); Yarina , Dayla , Midiana , Dimia , Jess , Vidora , Modell Pro , Simitsia , Modell Trend (+ ethinyl estradiol ); Yarina Plus , Jess Plus (+ ethinyl estradiol + calcium levomefolinate ).
Gestodene or Drospirenone, which is better?
Both synthetic hormones belong to the latest generation of drugs. They are quite effective and have minimal side effects. Medicines containing Gestodene are more often prescribed for dysmenorrhea and to establish a regular menstrual cycle. Drospirenone is advisable to use for contraception to reduce the severity of PMS , get rid of acne , and remove excess fluid from the body. It is necessary to remember the increased risk of thromboembolism and hyperkalemia during treatment with Drospirenone.
Desogestrel or Drospirenone, which is better?
Desogestrel, like Drospirenone, belongs to the latest generation of hormonal contraceptives. By analogy with Gestodene, the substance is used to eliminate dysmenorrhea . It should also be noted that clinical studies have found that the risk of weight gain is higher during treatment with Drospirenone. In any case, the decision about which of the substances listed above should be chosen must be made by the attending physician.
Today, hormonal contraception is not only a means of preventing unplanned pregnancy, but also an effective method of treating gynecological diseases. This became possible due to the fact that in modern combination drugs the dose of hormonal components has been significantly reduced, progestogens have been synthesized with high selectivity for progesterone receptors, new routes of hormone administration have been developed, the duration and frequency of application regimens have been changed, etc., which provides a real opportunity for individualization of treatment. The use of modern contraceptives, especially hormonal ones, by women who do not need them is today not only a new chapter in the history of contraception, but also a new direction in gynecology (David Serfaty, 2011).
Intensive research and development in the field of hormonal contraception over recent years has seemingly made further improvements in hormonal contraceptives impossible. It should be emphasized that the contraceptive effect of hormonal drugs is mainly due to the action of progestogens; estrogens only potentiate the inhibitory effect of progestogens on ovulation at the level of the hypothalamic-pituitary-ovarian system.
Thus, focusing primarily on the additional non-contraceptive effects of progestogens, scientists in 1980 developed the progestogen dienogest, which does not contain an ethynyl group at position 17α, which combines the advantages of progesterone derivatives and 19-norsteroids, and in 2000 a completely new progestogen , which is a derivative of spironolactone, is drospirenone [1].
Currently, a wide variety of progestogens have been synthesized, which opens up wide opportunities for individual selection of hormonal drugs. Progestogens are steroid hormones. According to the chemical classification, they are divided into progesterone derivatives (chloramdinone acetate, medroxyprogesterone acetate, cyproterone acetate), 19-nortestosterone derivatives, subdivided into estranes (noretinodrel, norethinodrone, ethynodiol diacetate) and gonans (levonorgestrel, desogestrel, norgestimate, gestodene), as well as dienoge st , combining the advantages of progesterone derivatives and 19-norsteroids, and spironolactone derivatives (drospirenone) [2]. Progesterone derivatives do not have a contraceptive effect when taken orally.
The mechanism of action of progestogens is associated with the effect on steroid receptors. There are five types of steroid receptors: for glucocorticoids, mineralocorticoids, estrogens, progestins and androgens. Progesterone and progestogens specifically bind to gestagen receptors, but can, to one degree or another, bind to other types of steroid receptors, which determines the characteristics of their action. Thus, in addition to gestagen receptors, progesterone binds to mineralocorticoid receptors, which determines its antimineralocorticoid effect, medroxyprogesterone acetate binds to glucocorticoid receptors, so it has little glucocorticoid activity, a number of gestagens (cyproterone acetate, chloramdinone, dienogest) bind to androgen receptors [1].
Thus, the spectrum of pharmacological activity of any progestogen is determined by the severity of the gestagenic effect, the presence or absence of antiandrogenic, antiestrogenic, antimineralocorticoid activity, depending on its chemical structure.
Drospirenone is the first synthetic progestin used in combined hormonal drugs, which is not a derivative of sex steroids, but is synthesized on the basis of 17α-spironolactone and is chemically similar to the diuretic and antihypertensive drug spironolactone. Unlike other progestins, it has antimineralocorticoid and antiandrogenic activity. And its pharmacological profile is closer to endogenous progesterone than any other synthetic progestin used today. Drospirenone inhibits ovulation by suppressing the synthesis of luteinizing hormone. It also prevents fertilization by slowing the transport of sperm through changes in the cervix and cervical mucus, and prevents implantation because it causes endometrial atrophy.
Drospirenone inhibits ovulation in a dose-dependent manner. The results of a number of randomized studies conducted in healthy menstruating women indicate that the optimal oral dose of drospirenone is 3.0 mg. In these studies, the combination of drospirenone 3.0 mg and ethinyl estradiol 30 mcg completely suppressed ovulation. Like endogenous progesterone, drospirenone has an antimineralocorticoid effect on the renin-angiotensin-aldosterone system. The antimineralocorticoid activity of drospirenone 3.0 mg is comparable to that of spironolactone 25 mg, thus the antimineralocorticoid activity of drospirenone is 8 times higher than that of spironolactone.
Drospirenone and cyproterone acetate exhibit their antiandrogenic activity in therapeutic doses. Like 2.0 mg cyproterone acetate/35 mcg ethinyl estradiol, the drospirenone/ethinyl estradiol combination reduced ovarian androgen production and seborrhea in women with mild to moderate acne in a double-blind, randomized trial [3]. The antiandrogenic activity of drospirenone is about 30% of the activity of cyproterone acetate. Preclinical studies have shown that drospirenone has no estrogenic, androgenic, glucocorticoid or antiglucocorticoid activity. The special properties of the drospirenone molecule associated with the absence of an ethynyl radical, namely a more effective effect on progesterone receptors, the absence of an inhibitory effect on the liver enzymes of the cytochrome system (P450), determine its additional advantages.
A striking example is the use of drospirenone-containing drugs by patients with polycystic ovary syndrome (PCOS), a pathology of the structure and function of the ovaries, the main criteria of which are ovulatory dysfunction and hyperandrogenism. Polycystic ovary syndrome occurs in 4 to 8% of the female population of fertile age and is one of the most common endocrinopathies [4]. The syndrome is the leading cause of anovulatory infertility, skin manifestations of hyperandrogenism (hirsutism, acne), and is also associated with a high risk of developing type 2 diabetes mellitus and cardiovascular pathology [5]. However, its etiology is still unknown; therapy is symptomatic. Diagnosis of PCOS requires a differential approach and exclusion of similar nosologies. A detailed examination and identification of the main symptoms of PCOS, as well as the exclusion of clinically similar diseases are necessary to make a diagnosis.
Numerous metabolic disorders in PCOS can lead to a number of diseases, including endometrial cancer. The long-term effect of estrogen on the endometrium due to progesterone deficiency is a common cause of endometrial hyperplasia, which, if left untreated, can progress to endometrial carcinoma even in young women. Strategies to reduce the risk of cancer in PCOS include the use of combined oral contraceptives (COCs), adequate dietary counseling, weight loss, and exercise. Treatment of PCOS outside of pregnancy planning consists of correcting skin manifestations of hyperandrogenism (hirsutism, acne, alopecia), regulating the menstrual cycle, and preventing mortality from cardiovascular diseases (treatment of metabolic disorders). For PCOS in women who are not planning a pregnancy, microdosed COCs containing drospirenone are the first-line drug, since drospirenone is a metabolically neutral progestin that does not interfere with carbohydrate and fat metabolism.
Numerous studies have shown that drospirenone-containing contraceptives can be considered as well-tolerated and highly contraceptive effective (Pearl index 0.7) [6, 7]. One well-known large multicenter study involving 11 thousand women, conducted in 2004 in 15 European countries, showed a significant improvement in the overall well-being of women, which was manifested by a decrease in symptoms of fluid retention and cycle-related mood changes, as well as improvement in skin condition [8]. Another study showed a significant reduction in fluid retention and bulimia in the period preceding menstruation, as well as an improvement in mood in women by the 6th cycle of taking drospirenone-containing COCs [6].
Thus, summarizing the above data, we can highlight the following main advantages of drospirenone: • antimineralocorticoid effect (reduces sodium and water retention, as a result does not affect body weight, does not cause mastalgia and has a therapeutic effect in premenstrual syndrome); • gestagenic effect (reliable blockade of ovulation and cycle control); • antiandrogenic effect (treatment of acne and seborrhea) [9].
Today in Russia, only three drugs contain drospirenone as a progestin component: Yarina (drospirenone 3 mg, ethinyl estradiol 30 mcg), Jess (drospirenone 3 mg, ethinyl estradiol 20 mcg) and the recently registered Midiana (drospirenone 3 mg, ethinyl estradiol 30 mcg).
I would like to present the results of the use of Midiana, obtained by our colleagues and us at the Scientific Center for AGiP of the Ministry of Health of the Russian Federation. In the study by I.B. Manukhina et al. 54 women aged 16–40 years were included (mean age: 26.0 ± 1.6 years), of which 34 had previously taken other oral contraceptives (OCs) and 20 had started using OCs for the first time. The drug was used for 6 cycles (total 324 cycles). To reduce the frequency of acyclic bleeding in patients using OCs for the first time, the authors recommended using the drug from the 5th to the 25th day of the cycle with additional barrier contraception in the 1st cycle. Contraceptive reliability was 100%. In addition, the nature of side effects was assessed, the frequency of which was higher in patients who took hormonal contraception for the first time. Acyclic bleeding was noted in only 4% of cases. The rate of cycles with breakthrough bleeding was only 0.3%. An increase in body weight (by 1–2 kg) was noted in 5 (9.3%) women, mostly novice users of OCs. And in 28% of women (all of whom “switched” from other OCs), a decrease in body weight was noted while taking Midiana. The authors noted other side effects, such as mastalgia, headache, mood changes, and nausea, but these were extremely rare. All side effects resolved within the first few months of taking the drug, without having a significant impact on tolerability and adherence to treatment. Only 1 (1.9%) woman refused to use the drug due to continued breakthrough bleeding. Thus, the low incidence of side effects (11%) when taking the new drug Midiana indicates its good tolerability and high contraceptive effectiveness [10].
Our preliminary data, based on the use of Midiana by 32 women of reproductive age, indicate that the drug is well tolerated, reliable cycle control and no cases of refusal to use it. The duration of use of the drug was 6 months.
Thus, the increase in the arsenal of drospirenone-containing compounds with the introduction of the drug Midiana allows us to hope for a further expansion of the possibilities of their use in the practice of an obstetrician-gynecologist.