The danger of candidiasis
Thrush is not a dangerous condition, since it does not relate to any particular disease and cannot affect the condition of the cervix and vaginal walls in women. The occurrence of a condition such as candidiasis indicates a disruption in the functioning of the body. Therefore, recurring thrush requires an examination to find out the cause of its occurrence. If you get rid of the cause, you can forget about the further appearance of candidiasis.
Etiology of VK
Candida spp., the causative agents of vaginal candidiasis, are opportunistic fungi that are the most common cause of fungal infections in humans. The genus Candida has about twenty species. As a rule, BK is associated with one species of Candida, but there is a probability (2-5%) of simultaneous infection with two or more species.
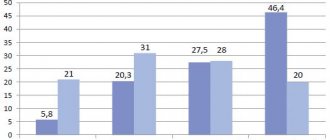
In Russia, the USA, Australia and Europe, Candida albicans is most often detected in women with VK (76-89%). It is followed by C. glabrata (7-16%). The percentage of non-albicans Candida ranges from 11 to 24%. Some studies have shown a trend toward an increase in the incidence of non-albicans candidiasis, but recent work by scientists in the United States involving ninety thousand samples refuted this assertion: the proportion of Candida species causing BK remained virtually unchanged from 2003 to 2007.
Etiologically, various candidiasis are clinically very similar, however, atypical pathogens are characterized by resistance to azole antimycotics. C. glabrata and C. krusei are more resistant to azole antifungal drugs than others.
CC dossier
Marina Pozdeeva
pharmacist of the first category and head of the pharmacy. Author of numerous works on pharmacology and pharmacotherapy, Dnepropetrovsk.
These data highlight the importance of identifying Candida spp. in women with a high risk of developing non-Candida albicans-associated VK in order to select effective therapy for the disease.
Causes
Reasons why thrush may occur in women:
- pregnancy;
- microflora disturbance;
- weakened immunity;
- endocrine diseases;
- use of contraceptives;
- failure to comply with hygiene standards.
Causes of thrush in men:
- failure to comply with hygiene standards;
- the result of unprotected sexual intercourse, transmission of the candida pathogen from a partner with thrush;
- sudden change in climatic conditions;
- use of aggressive detergents;
- weakened immunity;
- long-term use of antibiotics.
Risk factors
In many healthy women, VC develops sporadically. However, there are risk factors for candidiasis. Behavioral factors include frequent sexual intercourse and oral sex, as well as the use of spermicides.
Tight clothing and underwear usually do not cause illness. However, among women with recurrent VC (RVC), wearing tight tights and panty liners is positively associated with recurrence.
Biological risk factors for VC include:
- use of antibiotics;
- uncontrolled diabetes mellitus;
- genetic predisposition;
- high levels of sex hormones;
- taking oral contraceptives containing high doses of estrogen;
- pregnancy.
Antibacterial drugs help reduce the number of lacto- and bifidobacteria, a shift in pH in the vagina and the growth of Candida spp.
Tetracyclines, cephalosporins and ampicillin are more likely than other broad-spectrum antibiotics to provoke the development of candidiasis.
Pregnancy is one of the most common predisposing factors. According to studies, a third of pregnant women develop VK. High levels of sex hormones increase the glycogen content in the vagina, which in turn provides a constant source of carbon necessary for the growth of fungi.
Additionally, the increased acidity of the vaginal flora during pregnancy may inhibit the growth of other microorganisms that naturally inhibit Candida. Although the initial attachment of fungal cells occurs at higher pH values (6–7), an acidic environment favors mycelial development.
In the pathogenesis of vaginal candidiasis (VC), two main phases are distinguished: the adhesion phase, that is, the attachment of fungal cells to epithelial cells, and the mycelial phase. The mycelial phase begins with the entry of Candida spp. into epithelial cells. The growing pseudomycelium of fungi penetrates into the deep layers of the cervical and vaginal epithelium.
Candida are able to penetrate cells without violating the integrity of their mannoprotein membrane (this is the fibrillar coating of the cell wall of the fungus involved in adhesion processes). As a result, Candida resists defense factors and survives in the macroorganism.
Groups at risk for infection with non-albicans Candida species include:
- women with recurrent VK;
- HIV-infected women;
- women over 50 years of age;
- women with uncontrolled diabetes.
In all of the above groups, the most common species is C. glabrata.
The percentage of cases of non-albicans Candida-associated infection increases with women's age.
Features of RVC
Most women with VK respond quickly to therapy, but some may develop a relapsing form, characterized by four or more episodes of infection per year. Predisposing factors:
- uncontrolled diabetes mellitus;
- taking immunosuppressants;
- deviations in the local vaginal immunity of the mucous membranes;
- genetic predisposition.
Studies have proven that patients with RVC have a higher frequency of specific gene polymorphisms compared to the control group. In addition, these patients have certain Lewis system antigens in their blood.
Intermittent VK may also be associated with decreased in vivo concentrations of mannose-binding lectin. The latter, by binding to sugars on the surface of the Candida cell, triggers the pathway of activation of the complement system and leads to the death of the fungus through complement-mediated phagocytosis.
With this disease, an increased concentration of interleukin-4 is also recorded, which inhibits local protective mechanisms.
The Lewis antigen system depends on a group of genes that are expressed in the glandular epithelium. Lewis antigens, unlike erythrocyte antigens, are components of exocrine epithelial secretions, including vaginal ones.
The role of sexual transmission remains unproven. However, most studies indicate the need for treatment of sexual partners. Thus, an experiment by Dr. Horowitz, UK, demonstrated the presence of Candida species in the ejaculate of men whose partners suffered from RVC.
However, the same Horowitz conducted another study, which studied the results of therapy in 54 women, divided into two groups. Partners from the first group were subjected to antifungal therapy, but those from the second were not. There were no significant differences in the rate of relapse among women in these groups.
Relapses can also be caused by other Candida species that are not equally sensitive to first-line therapy.
Symptoms
The most common symptoms of thrush in women are:
- Pain that occurs during sexual intercourse.
- Swelling and redness of the mucous membranes.
- Pain with cutting when urinating.
- Pain with the release of cheesy contents from the genital tract, without odor.
- There is itching and burning in the vagina, which can periodically or regularly intensify during sleep, after sexual intercourse, after swimming and during menstruation.
In men, there is a burning sensation and pain during emptying of the bladder, constant or periodic itching, and a white coating on the head of the genital organ.
Methods of treatment and prevention of vaginal candidiasis
Today, in order to treat women from vaginal candidiasis, our clinic uses low-toxic and quite effective medications. For local treatment, qualified doctors at our clinic use special suppositories and creams that contain antifungal components. All medications offered by our doctors are highly effective; they are distributed evenly and quickly throughout the vaginal walls. However, the most effective treatment is to take medications orally and vaginally at the same time. In addition to increased effectiveness, this method of treatment minimizes the possibility of relapses.
In some cases, treatment is supplemented with immunotherapy and physiotherapy, and preparations of competing microorganisms (colibacterin, lactobacterin, lactic acid bacteria). From a scientific point of view, the effectiveness of these drugs has not been fully studied, but in practice their use has a targeted positive effect.
In addition to direct treatment, the disease requires timely prevention - elimination of the causes of vaginal candidiasis:
- normalize the microflora of your genital organs by using medications containing live cultures of lactobacilli;
- normalize the acidity of the vagina by giving up junk food, unfiltered water, and also be less nervous;
- take care of your intestinal health and cure dysbiosis;
- stimulate the immune system with vitamins and wellness treatments, as well as sports or gymnastics in clothing specially designed for this;
- normalize your metabolism with a properly structured diet;
- If possible, minimize your use of antibiotics by talking to your doctor.
Do not forget to take vitamin complexes prescribed by your doctor to increase your overall immunity level. Due to the fact that thrush can affect the intestines, B vitamins are prescribed in the form of tablets or injections. Avoid using synthetic underwear and replace them with natural fabrics such as cotton.
As for recurrent vaginal candidiasis, occurring more than 4 times a year, the following can be noted. It is necessary to undergo screening for endocrine diseases, as well as other chronic diseases, as early as possible. It is important to examine the organs adjacent to the urethra, primarily the intestines and bladder. Most likely, the doctor will order cultures (bacteriological studies), the purpose of which is to determine the body's response to certain antifungal drugs. Treatment of the chronic form is usually carried out with several drugs over a longer period of time than the treatment of the primary disease. Suppositories or vaginal tablets should be taken according to an individual dosage regimen, usually over several months. In some cases, periodic observations are necessary from a gynecologist, as well as from a doctor who monitors the treatment of the organ that is the source of infection.
Recurrence of thrush can also be caused by chronic intoxication with alcohol or drugs. Patients taking phenylbutazone, tranquilizers, and metronidazole are at increased risk. The cause of relapses may be untreated tuberculosis, colitis, anacid gastritis, pneumonia and other diseases.
The effectiveness of the completed course of treatment is usually determined using bacteriological testing. The average waiting time for results is 1 – 2 days.
Diagnostics
To determine the presence of candidiasis, you will need to take a scraping and send it for further research to a laboratory to identify pathogenic microflora.
The main goal of laboratory diagnostics is to determine the presence of candida fungus. If the diagnosis is carried out in women, then the diagnosis of thrush is established only when there is a large number of yeast-like fungi, as well as additional symptoms of vaginal dysbiosis.
Candidiasis in men is diagnosed when there is a small number of fungi, which indicates the presence of infection. Severe symptoms will allow the urologist to conduct a more detailed examination.
Which doctor should I contact?
If symptoms appear that indicate candidiasis, a woman should consult a gynecologist, and a man should consult a urologist.
Treatment of RVC caused by non-albicans Candida species
Non-albicans species respond very moderately to therapy with azole antimycotics. Therefore, the treatment regimen in such cases is selected individually, based on the severity of the disease and response to drugs.
Topical boric acid has been used to treat RVC for many decades. However, boric acid preparations can be absorbed through the vaginal mucosa into the blood and have a toxic effect. To avoid absorption, boric acid-based vaginal products are released in gelatin capsules. The recommended treatment regimen is one 600 mg capsule per day for two weeks.
There is no ready-made dosage form in Russia, but capsules can be prepared in pharmacies ex tempore. Studies have shown that treatment with vaginal boric acid capsules is effective in 70% of cases of C. glabrata-associated RVC.
An alternative to toxic boric acid is suppositories with amphotericin B. The antibiotic penetrates the cell membrane of the fungus and, by binding to ergosterol, destroys the cell wall. The course of treatment is 50 mg at night per os for two weeks. This treatment regimen is successful in 70% of patients suffering from disease caused by non-albicans species that are not amenable to azole therapy, especially C. glabrata.
Local preparations for vaginal use containing 17% flucytosine have also proven activity against non-albicans Candida species. Fungal cells absorb flucytosine, after which it is deaminated and converted into 5‑fluorouracil, which is incorporated into Candida DNA instead of uracil. As a result, protein synthesis is disrupted and the cell dies. A combination of 17% flucytosine cream and 3% amphotericin B cream is also possible. The average duration of treatment with flucytosine should be at least two weeks. The peculiarity of the drug is its high cost.
Treatment
All medical procedures related to candidiasis should be carried out only under the supervision of the attending physician. If you try to treat yourself, thrush may transform into an acute form, into a chronic form, and there is also a possibility of an exacerbation of the condition, which will lead to further difficult treatment.
Treatment for thrush includes:
- Antibiotic therapy, personal hygiene, support and protection of the immune system.
- Adhering to a diet that will require limiting carbohydrate intake.
- Complete cessation of bad habits.
- Use of prescribed medications to combat thrush.
Medicines
In the treatment of thrush, which occurs in a mild stage, it will be enough to use local remedies such as vaginal ointments, suppositories and tablets. The most popular drugs include:
- Natamycin;
- Nystatin;
- Miconazole;
- Clotrimazole;
- Isoconazole;
- Ketoconazole.
Doctors most often prescribe drugs with clotrimazole, and avoid the use of vaginal tablets, as they can suppress the normal microflora of the vagina.
Experts prescribe tablets for candidiasis in more advanced cases, as well as in chronic cases of thrush. Almost all medicines have fluconazole as their active ingredient; itraconazole may be an alternative.
Compared to women, thrush in men occurs more easily, and as a treatment, an experienced specialist will prescribe local treatment in the form of ointments, which will need to be applied to the affected areas. In more severe cases, oral medications such as Diflucan and Fluconazole may be prescribed.
Is thrush really a problem?
The content of the article
People of all ages suffer from candidiasis, with the peak incidence occurring between 20 and 40 years of age. According to statistics, 60% of women have been diagnosed with thrush at least once in their lives, and in 9%, candidiasis has a recurrent (repeating) course. In reality, this figure is higher, since in many patients the disease does not produce noticeable symptoms and the fungus is detected only when swabs are taken from the vagina.
The main problems of this pathology are self-medication, which leads to the disease becoming chronic, and negligent attitude towards one’s health. Gynecologists at the Diana Medical Center daily encounter cases of thrush, the severity of which is due to the patients’ late seeking of professional medical help.
Diet
For thrush in women, the diet plan should be based on consuming foods that have antibacterial and antifungal effects. These include:
- garlic;
- seafood;
- parsley;
- buckwheat;
- White rice;
- broccoli;
- natural yoghurts;
- oatmeal;
- cucumbers
For men, when diagnosing candidiasis, the diet should be followed for up to 12 months, the minimum is 4 months. During this time you should:
- Avoid consumption of spicy foods and various sauces.
- Completely abstain from alcohol for the entire period of treatment.
- There are only low-fat dishes, those that are steamed, boiled or stewed.
Myths and truth about treating thrush
Myth No. 1. Thrush is normal!
The causative agent of thrush is fungi of the genus Candida, which are classified as opportunistic microorganisms. This means that they are contained in small quantities in the microflora of the body of healthy women. This fact leads some patients to believe that periodic manifestations of thrush do not deserve attention.
This is a misconception, because normally fungal pathogens do not cause unpleasant symptoms and do not bring discomfort to their owner. But in large quantities, Candida becomes dangerous, so thrush needs to be treated.
Myth No. 2. If thrush is not treated, it will go away on its own
This misconception, propagated on many websites, has led to the spread of chronic thrush among young women.
The primary symptoms of the disease - severe itching and curdled discharge, characteristic of the acute phase of the disease, indeed, even without treatment, gradually fade away. But this is a false sense of recovery. After some time, the troubles will return again - at the moment when the body experiences severe physical or psychological stress. In addition, the recurrence of thrush is facilitated by changes in hormonal levels, which occurs during menstruation and during pregnancy.
Myth No. 3. One tablet is enough to treat thrush!
The advertisement claims that after taking one capsule of the miracle drug, a woman will forever forget about the symptoms of thrush. Yes, the thrush may go away, but it will be replaced by severe dysbiosis, vaginosis and other diseases associated with disturbances in the vaginal microflora.
All antifungal agents used in the treatment of candidiasis (thrush) are drugs that specifically suppress pathological flora. At the same time, a safe drug should have a gentle effect on the mucous membrane without causing dysbacteriosis. In other words, he should treat smoothly, leaving time for the body to adapt. Whereas the “killer dose” will destroy both the causative agent of thrush and all living things, freeing up a springboard for colonization by new fungi and bacteria.
In addition, thrush rarely comes alone. Analysis (smear) sometimes reveals a whole bunch of STDs. In this case, combination treatment is required.
Myth No. 4. Local remedies for thrush are useless
Topical antifungal drugs quickly suppress fungal growth and play an important role in the treatment of thrush. Candles, creams, gels and sprays do not cause side effects and have no restrictions on use. But local therapy is considered by gynecologists exclusively as an additional measure, since it is effective only in the early stages of the development of pathology.
At the same time, suppositories and ointments are the drugs of choice in the treatment of candidiasis in pregnant and lactating women.
Myth No. 5. The appearance of thrush does not depend on lifestyle
The development of thrush always has a specific cause. Frequent stress, poor diet and heavy physical activity, which weaken the immune system, activate the fungal flora. Failure to comply with personal hygiene rules also affects the state of the vaginal microflora; in addition, the disease can be acquired by changing partners and using traumatic sex toys.
Another, perhaps significant reason is the uncontrolled use of antibiotics that affect the flora of the body. Broad-spectrum antibacterial drugs are not able to distinguish “bad” bacteria from “good” ones; they kill everything not only in the vagina, but also in the stomach and intestines. Therefore, lovers of self-medication are in for a surprise in the form of dysbiosis and accompanying candidiasis.
Myth No. 6. The most effective treatment for thrush is traditional medicine!
Traditional methods of treating candidiasis usually come down to the use of infusions and decoctions of herbs for washing and douching the vagina. For this purpose, herbs with antibacterial and antifungal effects are used.
These measures are good only as an aid to the main treatment, but thrush cannot be cured in this way. For quality treatment of vaginal candidiasis, you need to take antifungal drugs, immunostimulants and vitamins. Only this set of medications is guaranteed to reduce the likelihood of relapse of the disease.
Prevention
Prevention of thrush:
- It is important to wear underwear made exclusively from natural fabrics. It should be such that it does not rub anywhere;
- when playing sports, it is recommended to wash your sports uniform as often as possible;
- in order to maintain hygiene of the genital organs, they should be washed only with water, using a special mild soap;
- Hygiene products should not contain dyes or fragrances;
- for those who suffer from diabetes, blood sugar control should be constant;
- adhere to proper nutrition and actively walk in the fresh air to support your immune system.
Why thrush develops: causes of candidiasis
The main cause of the disease is fungi of the genus Candida. Normally, the fungus lives in the body of any person, but under certain circumstances, as a result of the influence of various predisposing factors, it begins to actively multiply. Therefore, such microorganisms are called opportunistic.
Normal vaginal microflora keeps the fungus from excessively multiplying. When it changes (dysbiosis), the growth of Candida increases, and thrush .
Stimulate the activation of infection:
- hormonal changes in the body: pregnancy, menopause, diseases of the endocrine system (diabetes, thyroid problems), incorrect selection of birth control pills;
- violation of personal hygiene rules and wearing synthetic underwear - the fungus loves dampness, warmth and does not like fresh air;
- douching, using aggressive cleaning agents;
- the presence of sexually transmitted infections, inflammation of the internal female organs, infection with thrush from a partner;
- diseases accompanied by changes in the concentration of sex hormones in the blood,
- pregnancy and chronic foci of infection in the body, weakening the immune system;
- uncontrolled use of antibiotics, which destroy, along with parasitic flora, beneficial lactobacilli - protectors of the mucous membrane.
It’s easy to provoke candidiasis: just walk around in tight synthetic panties in the heat. The fungus develops instantly in such conditions - it loves moisture, warmth, and does not need air.
Complications
Most complications of vaginal candidiasis are associated with the spread of the inflammatory process to nearby organs and tissues and the addition of bacterial inflammation. It occurs against the background of a sharp decrease in local immunity. Most often, patients encounter the following problems:
- salpingitis and salpingo-oophoritis (adnexitis): inflammation of the uterine appendages: tubes and ovaries; the process can be unilateral or bilateral, accompanied by pain in the lower abdomen, weakness, fever; without treatment, it can cause infertility due to the development of adhesions;
- urethritis: inflammation of the urethra; classic symptoms are a burning sensation when urinating, changes in the appearance and color of urine, redness and swelling in the area of the external urethral meatus;
- cystitis: inflammation of the bladder that develops as a result of the passage of the pathogen from the urethra; Symptoms of urethritis include frequent urination with a small amount of urine, pain and cramping at the end of the process, increased temperature and pain in the lower abdomen.
In addition to the spread of infection, vaginal candidiasis can threaten the development of stenosis (narrowing) of the vagina. This condition occurs due to chronic inflammation, which leads to the growth of scar tissue and narrowing of the lumen of the organ. This leads to significant difficulty in sexual life.
Vaginal candidiasis is very dangerous for pregnant women, since without treatment, infection of the fetus is possible, which can lead to its death.
In the postpartum period, women may develop candidal endometritis.