Noliprel A Forte tablets 5 mg + 1.25 mg 30 pcs. in Moscow
Oblong, film-coated tablets, white.
The combination of perindopril and indapamide does not change their pharmacokinetic characteristics compared to taking these drugs separately.
Perindopril
When taken orally, perindopril is rapidly absorbed. Bioavailability is 65–70%.
Approximately 20% of the total amount of absorbed perindopril is converted to perindoprilat, the active metabolite. Taking the drug with food is accompanied by a decrease in the metabolism of perindopril to perindoprilat (this effect does not have significant clinical significance).
Cmax of perindoprilate in blood plasma is achieved 3–4 hours after oral administration of perindopril.
The binding to plasma proteins is less than 30% and depends on the concentration of perindopril in the blood.
The dissociation of perindoprilate associated with ACE is slowed down. As a result, the effective T1/2 is 25 hours. Repeated administration of perindopril does not lead to its cumulation, and T1/2 of perindoprilat upon repeated administration corresponds to the period of its activity, thus an equilibrium state is achieved after 4 days.
Perindoprilat is excreted from the body by the kidneys. T1/2 of the metabolite is 3–5 hours.
The elimination of perindoprilate is slowed down in old age, as well as in patients with heart and renal failure.
The dialysis clearance of perindoprilate is 70 ml/min.
The pharmacokinetics of perindopril is changed in patients with liver cirrhosis: its hepatic clearance is reduced by 2 times. However, the amount of perindoprilate formed does not decrease, so no change in the dose of the drug is required.
Perindopril crosses the placenta.
Indapamide
Indapamide is quickly and completely absorbed from the gastrointestinal tract.
Cmax of the drug in blood plasma is observed 1 hour after oral administration.
Connection with blood plasma proteins - 79%.
T1/2 is 14–24 hours (average 19 hours). Repeated administration of the drug does not lead to its accumulation in the body. It is excreted mainly by the kidneys (70% of the administered dose) and through the intestines (22%) in the form of inactive metabolites.
The pharmacokinetics of the drug does not change in patients with renal failure.
Noliprel® A forte is a combination drug containing perindopril arginine and indapamide. The pharmacological properties of the drug Noliprel® A forte combine the individual properties of each of the components.
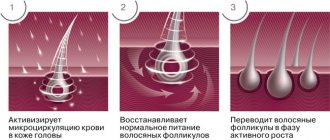
1. Mechanism of action
Noliprel® A forte
The combination of perindopril and indapamide enhances the antihypertensive effect of each of them.
Perindopril
Perindopril is an inhibitor of the enzyme that converts angiotensin I to angiotensin II (ACE inhibitor). ACE, or kininase II, is an exopeptidase that carries out both the conversion of angiotensin I into the vasoconstrictor substance angiotensin II, and the destruction of bradykinin, which has a vasodilatory effect, into an inactive heptapeptide. As a result, perindopril:
- reduces the secretion of aldosterone;
- according to the principle of negative feedback, it increases the activity of renin in the blood plasma;
- with long-term use, it reduces the peripheral vascular resistance, which is mainly due to the effect on the vessels in the muscles and kidneys. These effects are not accompanied by sodium and fluid retention or the development of reflex tachycardia.
Perindopril normalizes myocardial function, reducing preload and afterload.
When studying hemodynamic parameters in patients with chronic heart failure (CHF), it was revealed:
- decrease in filling pressure in the left and right ventricles of the heart;
— decrease in OPSS;
- increased cardiac output;
- increased muscle peripheral blood flow.
Indapamide
Indapamide belongs to the group of sulfonamides; its pharmacological properties are similar to thiazide diuretics. Indapamide inhibits the reabsorption of sodium ions in the cortical segment of the loop of Henle, which leads to an increase in the excretion of sodium, chlorine and, to a lesser extent, potassium and magnesium ions by the kidneys, thereby increasing diuresis and reducing blood pressure.
2. Antihypertensive effect
Noliprel® A forte
Noliprel® A forte has a dose-dependent antihypertensive effect on both DBP and SBP in both standing and lying positions. The antihypertensive effect persists for 24 hours. A stable therapeutic effect develops in less than 1 month from the start of therapy and is not accompanied by tachycardia. Stopping treatment does not cause withdrawal syndrome.
Noliprel® A forte reduces the degree of left ventricular hypertrophy (LVH), improves arterial elasticity, reduces peripheral vascular resistance, and does not affect lipid metabolism (total cholesterol, HDL and LDL cholesterol, triglycerides).
The effect of using a combination of perindopril and indapamide on LVG in comparison with enalapril has been proven. In patients with arterial hypertension and LVH who received therapy with perindopril erbumine 2 mg (equivalent to 2.5 mg of perindopril arginine)/indapamide 0.625 mg or enalapril at a dose of 10 mg once daily, and with an increase in the dose of perindopril erbumine to 8 mg (equivalent to 10 mg perindopril arginine) and indapamide up to 2.5 mg, or enalapril up to 40 mg once daily, a more significant decrease in left ventricular mass index (LVMI) was noted in the perindopril/indapamide group compared with the enalapril group. In this case, the most significant effect on LVMI was observed with the use of perindopril erbumine 8 mg/indapamide 2.5 mg.
A more pronounced antihypertensive effect was also noted during combination therapy with perindopril and indapamide compared to enalapril.
In patients with type 2 diabetes (mean age 66 years, body mass index 28 kg/m2, glycosylated hemoglobin (HbA1c) 7.5%, blood pressure 145/81 mm Hg), the effect of a fixed combination was studied perindopril/indapamide on major micro- and macrovascular complications in addition to both standard glycemic control therapy and intensive glycemic control (IGC) strategies (target HbA1c <6.5%).
83% of patients had arterial hypertension, 32% and 10% had macro- and microvascular complications, and 27% had microalbuminuria. The majority of patients were receiving hypoglycemic therapy at the time of inclusion in the study, 90% of patients were receiving oral hypoglycemic agents (47% of patients in monotherapy, 46% in two-drug therapy, 7% in three-drug therapy). 1% of patients received insulin therapy, 9% received only diet therapy. Sulfonylurea derivatives were taken by 72% of patients, metformin by 61%. As concomitant therapy, 75% of patients received antihypertensive drugs, 35% of patients received lipid-lowering drugs (mainly HMG-CoA reductase inhibitors (statins) - 28%), acetylsalicylic acid as an antiplatelet agent and other antiplatelet drugs (47%).
After a 6-week run-in period, during which patients received perindopril/indapamide therapy, they were allocated to the standard glycemic control group or the IGC group (Diabeton® MB with the possibility of increasing the dose to a maximum of 120 mg/day or adding another hypoglycemic agent).
The IGC group (average follow-up duration - 4.8 years, average HbA1c - 6.5%) compared with the standard control group (average HbA1c - 7.3%) showed a significant reduction of 10% in the relative risk of the combined incidence of macro- and microvascular complications.
The benefit was achieved due to a significant reduction in the relative risk of: major microvascular complications by 14%, the occurrence and progression of nephropathy by 21%, microalbuminuria by 9%, macroalbuminuria by 30% and the development of renal complications by 11%.
The benefits of antihypertensive therapy were independent of the benefits achieved with IGCs.
Perindopril
Perindopril is effective in the treatment of arterial hypertension of any severity.
The antihypertensive effect of the drug reaches its maximum 4–6 hours after a single oral dose and persists for 24 hours. 24 hours after taking the drug, a pronounced (about 80%) residual ACE inhibition is observed.
Perindopril has an antihypertensive effect in patients with both low and normal plasma renin activity.
The simultaneous administration of thiazide diuretics increases the severity of the antihypertensive effect. In addition, the combination of an ACE inhibitor and a thiazide diuretic also reduces the risk of hypokalemia while taking diuretics.
Indapamide
The antihypertensive effect occurs when the drug is used in doses that have a minimal diuretic effect.
The antihypertensive effect of indapamide is associated with an improvement in the elastic properties of large arteries and a decrease in peripheral vascular resistance.
Indapamide reduces LVG, does not affect the concentration of lipids in the blood plasma: triglycerides, total cholesterol, LDL, HDL; carbohydrate metabolism (including in patients with concomitant diabetes mellitus).
Noliprel® A forte
The use of Noliprel® A forte 5 mg + 1.25 mg is not accompanied by a significant reduction in the frequency of side effects, with the exception of hypokalemia, compared with perindopril and indapamide at the lowest approved doses (see “Side effects”). When starting therapy with two antihypertensive drugs that the patient has not previously received, an increased risk of developing idiosyncrasies cannot be excluded. Careful monitoring of the patient can minimize this risk.
Renal dysfunction
Therapy is contraindicated in patients with severe renal failure (creatinine Cl less than 30 ml/min). In some patients with arterial hypertension without previous obvious renal impairment, laboratory signs of functional renal failure may appear during therapy. In this case, treatment should be stopped. In the future, you can resume combination therapy using low doses of drugs, or use drugs in monotherapy.
Such patients require regular monitoring of potassium and creatinine levels in the blood serum - 2 weeks after the start of therapy and every 2 months thereafter. Renal failure occurs more often in patients with severe chronic heart failure or underlying renal impairment, incl. with renal artery stenosis.
Arterial hypotension and water-electrolyte imbalance
Hyponatremia is associated with a risk of sudden development of arterial hypotension (especially in patients with arterial stenosis of a solitary kidney and bilateral renal artery stenosis). Therefore, during dynamic monitoring of patients, attention should be paid to possible symptoms of dehydration and decreased levels of electrolytes in the blood plasma, for example after diarrhea or vomiting. Such patients require regular monitoring of plasma electrolyte levels.
In case of severe arterial hypotension, intravenous administration of 0.9% sodium chloride solution may be required.
Transient arterial hypotension is not a contraindication for continued therapy. After restoration of blood volume and blood pressure, therapy can be resumed using low doses of drugs, or drugs can be used as monotherapy.
Potassium level
The combined use of perindopril and indapamide does not prevent the development of hypokalemia, especially in patients with diabetes mellitus or renal failure. As in the case of the combined use of an antihypertensive drug and a diuretic, regular monitoring of the level of potassium in the blood plasma is necessary.
Excipients
It should be taken into account that the excipients of the drug include lactose monohydrate. Noliprel® A forte should not be prescribed to patients with hereditary galactose intolerance, lactase deficiency and glucose-galactose malabsorption.
Lithium preparations
The simultaneous use of a combination of perindopril and indapamide with lithium preparations is not recommended (see “Contraindications”, “Interaction”).
Perindopril
Neutropenia/agranulocytosis
The risk of developing neutropenia while taking ACE inhibitors is dose-dependent and depends on the drug taken and the presence of concomitant diseases. Neutropenia rarely occurs in patients without concomitant diseases, but the risk increases in patients with impaired renal function, especially against the background of systemic connective tissue diseases (including systemic lupus erythematosus, scleroderma). After discontinuation of ACE inhibitors, signs of neutropenia disappear on their own.
To prevent the development of such reactions, it is recommended to strictly follow the recommended dose. When prescribing ACE inhibitors to this group of patients, the benefit/risk factor should be carefully assessed.
Angioedema (Quincke's edema)
When taking ACE inhibitors, incl. and perindopril, in rare cases, the development of angioedema of the face, extremities, lips, tongue, glottis and/or larynx may occur. If symptoms appear, perindopril should be discontinued immediately and the patient should be observed until signs of edema completely disappear. If the swelling affects only the face and lips, it usually resolves on its own, although antihistamines may be used to treat symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, glottis, or larynx can lead to airway obstruction. If such symptoms appear, you should immediately administer subcutaneous epinephrine (adrenaline) at a dilution of 1:1000 (0.3 or 0.5 ml) and/or ensure airway patency.
Patients with a history of angioedema, not associated with taking ACE inhibitors, may have an increased risk of developing it when taking drugs of this group (see “Contraindications”).
In rare cases, angioedema of the intestine develops during therapy with ACE inhibitors.
Anaphylactoid reactions during desensitization
There are isolated reports of the development of long-term life-threatening anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy with the venom of hymenoptera insects (bees, wasps). ACE inhibitors should be used with caution in patients prone to allergic reactions undergoing desensitization procedures. Prescription of an ACE inhibitor should be avoided in patients receiving immunotherapy with hymenoptera venom. However, an anaphylactoid reaction can be avoided by temporarily discontinuing the ACE inhibitor at least 24 hours before the procedure.
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors, during LDL apheresis using dextran sulfate, or in patients receiving hemodialysis using high-flow membranes. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued at least 24 hours before the apheresis procedure.
Hemodialysis
Anaphylactoid reactions have been reported in patients receiving ACE inhibitors during hemodialysis using high-flux membranes (eg AN69®). Therefore, it is advisable to use a different type of membrane or use an antihypertensive agent of a different pharmacotherapeutic group.
Cough
During therapy with an ACE inhibitor, a dry cough may occur. The cough persists for a long time while taking drugs of this group and disappears after their discontinuation. If a patient develops a dry cough, one should be aware of the possible iatrogenic nature of this symptom. If the attending physician believes that ACE inhibitor therapy is necessary for the patient, the drug may be continued.
Children and teenagers
The drug should not be prescribed to children and adolescents under the age of 18 years due to the lack of data on the effectiveness and safety of the use of perindopril as monotherapy or as part of combination therapy in patients in this age group.
Risk of arterial hypotension and/or renal failure (in patients with heart failure, fluid and electrolyte imbalance, etc.)
In some pathological conditions, significant activation of the RAAS system may be observed, especially with severe hypovolemia and a decrease in the level of plasma electrolytes (due to a salt-free diet or long-term use of diuretics), in patients with initially low blood pressure, with bilateral renal artery stenosis or with stenosis of the artery of a single kidney , chronic heart failure or cirrhosis of the liver with edema and ascites.
The use of an ACE inhibitor causes a blockade of this system and therefore may be accompanied by a sharp decrease in blood pressure and/or an increase in plasma creatinine levels, indicating the development of functional renal failure. These phenomena are more often observed when taking the first dose of the drug or during the first two weeks of therapy. Sometimes these conditions develop acutely and during other periods of therapy. In such cases, when resuming therapy, it is recommended to use the drug at a lower dose and then gradually increase the dose.
Elderly patients
Before starting to take the drug, it is necessary to assess the functional activity of the kidneys and the concentration of potassium in the blood plasma. At the beginning of therapy, the dose of the drug is selected taking into account the degree of reduction in blood pressure, especially in the case of dehydration and loss of electrolytes. Such measures help to avoid a sharp decrease in blood pressure.
Atherosclerosis
The risk of arterial hypotension exists in all patients, however, special care should be taken when using the drug in patients with coronary artery disease and cerebrovascular insufficiency. In such patients, treatment should be started with low doses.
Patients with renovascular hypertension
The treatment method for renovascular hypertension is revascularization. However, the use of ACE inhibitors has a beneficial effect in this category of patients, both awaiting surgery and in cases where surgery is not possible.
Treatment with Noliprel® A in patients with diagnosed or suspected bilateral renal artery stenosis or stenosis of the artery of a single kidney should begin with a low dose of the drug in a hospital setting, monitoring renal function and potassium concentration in the blood plasma. Some patients may develop functional renal failure, which disappears when the drug is discontinued.
Other risk groups
In persons with severe heart failure (stage IV) and patients with insulin-dependent diabetes mellitus (risk of a spontaneous increase in potassium concentration), treatment should begin with a low dose of the drug and under constant medical supervision.
Patients with arterial hypertension and coronary artery disease should not stop taking beta-blockers: ACE inhibitors should be used together with beta-blockers.
Anemia
Anemia can develop in patients after kidney transplantation or in people on hemodialysis. In this case, the decrease in hemoglobin concentration is greater, the higher its initial value. This effect does not appear to be dose-dependent, but may be related to the mechanism of action of ACE inhibitors.
A slight decrease in hemoglobin concentration occurs during the first 6 months, then it remains stable and is completely restored after discontinuation of the drug. In such patients, treatment can be continued, but hematological tests should be performed regularly.
Surgery/general anesthesia
The use of ACE inhibitors in patients undergoing surgery under general anesthesia can lead to a significant decrease in blood pressure, especially when using general anesthesia agents that have a hypotensive effect.
It is recommended to stop taking long-acting ACE inhibitors, incl. perindopril, the day before surgery. It is necessary to warn the anesthesiologist that the patient is taking ACE inhibitors.
Aortic stenosis/hypertrophic cardiomyopathy
ACE inhibitors should be prescribed with caution to patients with left ventricular outflow tract obstruction.
Liver failure
In rare cases, cholestatic jaundice occurs while taking ACE inhibitors. As this syndrome progresses, liver necrosis may rapidly develop, sometimes with death. The mechanism of development of this syndrome is unclear. If jaundice appears or a significant increase in the activity of liver enzymes while taking ACE inhibitors, you should stop taking the drug and consult a doctor (see “Side effects”).
Indapamide
In the presence of liver dysfunction, taking thiazide and thiazide-like diuretics can lead to the development of hepatic encephalopathy. In this case, you should immediately stop taking the drug.
Water and electrolyte balance
Content of sodium ions in blood plasma.
Before starting treatment, it is necessary to determine the content of sodium ions in the blood plasma. While taking the drug, this indicator should be regularly monitored. All diuretics can cause hyponatremia, which sometimes leads to serious complications. Hyponatremia at the initial stage may not be accompanied by clinical symptoms, so regular laboratory monitoring is necessary. More frequent monitoring of sodium ion levels is indicated for patients with liver cirrhosis and the elderly (see “Side effects” and “Overdose”).
Content of potassium ions in blood plasma.
Therapy with thiazide and thiazide-like diuretics is associated with a risk of hypokalemia. Hypokalemia (less than 3.4 mmol/l) should be avoided in the following categories of high-risk patients: elderly people, debilitated patients or those receiving concomitant drug therapy, patients with liver cirrhosis, peripheral edema or ascites, coronary artery disease, heart failure. Hypokalemia enhances the toxic effect of cardiac glycosides and increases the risk of developing arrhythmias.
The high-risk group also includes patients with an increased QT interval, and it does not matter whether this increase is caused by congenital causes or the effect of drugs.
Hypokalemia, like bradycardia, contributes to the development of severe cardiac arrhythmias, especially arrhythmias, which can be fatal. In all the cases described above, more regular monitoring of the content of potassium ions in the blood plasma is necessary. The first measurement of potassium ion concentration should be carried out within the first week from the start of therapy.
If hypokalemia is detected, appropriate treatment should be prescribed.
Content of calcium ions in blood plasma.
Thiazide and thiazide-like diuretics reduce the excretion of calcium ions by the kidneys, leading to a slight and temporary increase in the concentration of calcium in the blood plasma. Severe hypercalcemia may be a consequence of previously undiagnosed hyperparathyroidism. Before studying the function of the parathyroid gland, you should stop taking diuretics.
Glucose content in blood plasma.
It is necessary to monitor blood glucose levels in patients with diabetes mellitus, especially in the presence of hypokalemia.
Uric acid.
In patients with elevated levels of uric acid in the blood plasma during therapy, the frequency of gout attacks may increase.
Diuretics and kidney function.
Thiazide and thiazide-like diuretics are fully effective only in patients with normal or slightly impaired renal function (plasma creatinine in adults below 25 mg/l or 220 µmol/l).
At the beginning of diuretic treatment in patients, due to hypovolemia and hyponatremia, a temporary decrease in glomerular filtration rate and an increase in the concentration of urea and creatinine in the blood plasma may be observed. This transient functional renal failure is not dangerous for patients with unchanged renal function, but its severity may increase in patients with renal failure.
Photosensitivity
Cases of photosensitivity reactions have been reported while taking thiazide and thiazide-like diuretics. If photosensitivity reactions develop while taking the drug, treatment should be discontinued. If it is necessary to continue diuretic therapy, it is recommended to protect the skin from exposure to sunlight or artificial UV rays.
Athletes
Indapamide may give a positive reaction during doping control.
Impact on the ability to drive a car or perform work that requires increased speed of physical and mental reactions.
The effect of the substances included in the drug Noliprel® A forte does not lead to disturbances in psychomotor reactions. However, some people may develop different individual reactions in response to lowering blood pressure, especially at the beginning of therapy or when other antihypertensive drugs are added to therapy. In this case, the ability to drive a car or perform work that requires increased speed of physical and mental reactions may be reduced.
Compound
The drug Noliprel is offered in several different forms. All variations of the drug include perindopril and indapamide . Combined Noliprel contain 2 mg of perindopril and 0.625 mg of indapamide. The composition of Noliprel Forte includes 4 mg of perindopril and 1.25 mg of indapamide. Noliprel A contains 2.5 mg of perindopril and 0.625 mg of indapamide.
In this drug, perindopril is associated with the amino acid arginine, which has a beneficial effect on the condition of the cardiovascular system. Noliprel A Forte tablets contain 5 mg of perindopril and 1.25 mg of indapamide. Noliprel A Bi-forte contains 10 mg of perindopril and 2.5 mg of indapamide.
As additional substances in the composition of the drug Noliprel there is magnesium stearate, lactose monohydrate, colloidal hydrophobic silicon dioxide, microcrystalline cellulose.
Contraindications
Contraindications to the use of all types of the drug Noliprel are the following diseases and conditions:
- high sensitivity to the components of the drug or the presence of allergic reactions to its components;
- renal failure , in which creatinine clearance is less than 30 ml/min;
- liver failure , in which there is a tendency to encephalopathy ;
- combination with drugs that prolong the QT interval, as well as antiarrhythmic drugs;
- hypokalemia;
- renal artery stenosis;
- lactase deficiency, glucose-galactose malabsorption syndrome, galactosemia;
- history of angioedema;
- pregnancy , lactation ;
- age up to eighteen years.
Also, you should not take the drug at the same time as potassium supplements or potassium-sparing diuretics if the patient has hyperkalemia.
Due to the lack of sufficient information, it is not recommended to use the tablets for treatment in people who are on hemodialysis , as well as in patients with decompensated heart failure.
It is prescribed with caution to people with systemic connective tissue diseases, those taking antidepressants, and suppression of bone marrow hematopoiesis. angina pectoris are also treated with caution .
Pharmacokinetics and pharmacodynamics
The pharmacokinetics of perindopril and indapamide when used in combination is the same as when used separately. After oral administration, perindopril is rapidly absorbed. Bioavailability level - 65-70%. About 20% of total absorbed perindopril is later converted to perindoprilat (the active metabolite). The maximum concentration of perindoprilate in plasma is observed after 3-4 hours. Less than 30% binds to blood proteins, depending on the concentration in the blood plasma. The half-life is 25 hours. The substance penetrates the placental barrier. Perindoprilat is excreted from the body through the kidneys. Its half-life is 3-5 hours. There is a slower administration of perindoprilate in older people, as well as in patients with heart failure and renal failure.
Indapamide is completely and relatively quickly absorbed from the gastrointestinal tract. The maximum concentration of the substance in plasma is observed one hour after oral administration.
The substance binds to plasma proteins by 79%. Half-life is 19 hours. The substance is excreted in the form of inactive metabolites by the kidneys (approximately 70%) and intestines (approximately 22%). In people with renal failure, no changes in the pharmacokinetics of the substance are observed.
Overdose
In case of an overdose of the drug, there is a severe decrease in blood pressure, nausea, vomiting, dizziness , mood instability, symptoms of renal failure, and electrolyte imbalance. In this case, you need to immediately bring the water-electrolyte balance back to normal, rinse the stomach, and take enterosorbents. Noliprel metabolites can be removed using dialysis. If necessary, intravenous saline is administered.
pharmachologic effect
Noliprel is a combination drug that contains perindopril (an angiotensin-converting factor inhibitor) and indapamide (a diuretic that is part of the sulfonamide group).
The pharmacological effect of a drug is determined by a combination of some of the effects of these components. In this combination, both components mutually increase the effect. Noliprel is an antihypertensive drug that effectively lowers both diastolic and systolic blood pressure. The severity of the effect depends on the dose. After taking the drug, there is no rapid heartbeat. The clinical effect is observed 1 month after treatment was started. The antihypertensive effect lasts for one day. After therapy is suspended, the patient does not experience withdrawal symptoms. During treatment, the severity of left ventricular hypertrophy decreases, and the degree of total precardiac and postcardiac load decreases. Large vessels become more elastic, the walls of small vessels are restored. The medicine has no effect on the metabolic processes that occur in the body.
Perindopril reduces the level of aldosterone secretion, resulting in increased renin activity in the blood. Blood pressure decreases in people with different levels of renin . Under the influence of this component, blood vessels dilate.
When taking the drug, the likelihood of hypokalemia . The mechanism of action of indapamide is similar to thiazide diuretics: urination and excretion of sodium and chloride ions in the urine will increase.
Vascular hyperreactivity decreases under the influence of adrenaline. The amount of lipids in the blood does not change.
Side effects
- In the functions of the cardiovascular system : severe hypotension, orthostatic collapse, in rare cases: arrhythmia , stroke , myocardial infarction .
- In the functions of the genitourinary system : deterioration of kidney function, proteinuria in people with glomerular nephropathy, in rare cases - acute renal failure. There may be a decrease in potency.
- In the functions of the central and peripheral nervous system : severe fatigue, dizziness , headache , asthenia, unstable mood, impaired hearing, vision, decreased appetite, convulsions, and in some cases, stupor.
- In the functions of the respiratory system : cough, difficulty breathing, bronchospasm, nasal discharge.
- In the functions of the gastrointestinal tract : dyspepsia, abdominal pain, pancreatitis , cholestasis, increased transaminase activity, hyperbilirubinemia.
- In the functions of the blood system : against the background of hemodialysis or after a kidney transplant, patients may develop anemia, in rare cases - thrombocytopenia, pancytopenia, agranulocytosis, hemolytic anemia.
- Allergic manifestations : skin itching, rash, swelling, urticaria.
- Patients with liver failure may develop hepatic encephalopathy. People with impaired water-electrolyte balance may experience hyponatremia, hypovolemia, hypokalemia, and dehydration.
special instructions
People who have been prescribed treatment with Noliprel need adequate dehydration of the body to prevent a sharp decrease in blood pressure.
People with heart failure may be treated with beta blockers at the same time.
When treated with Noliprel, a positive reaction is observed during a doping test.
In the first weeks of treatment, it is important to drive vehicles or operate precision machinery carefully when treating with Noliprel.
If during treatment there is a significant decrease in pressure, it may be necessary to administer 0.9% sodium chloride intravenously.
Treatment of patients with cerebral circulatory insufficiency or coronary heart disease should begin with small doses of Noliprel.
In people who have very high levels of uric acid in the blood, when treated with varieties of the drug Noliprel, the risk of developing gout .
Interaction
Noliprel should not be taken at the same time as lithium medications. If it is impossible to discontinue one of the drugs, the lithium level in the blood should be closely monitored.
With simultaneous treatment with potassium-sparing diuretics or drugs with potassium, the concentration of potassium in the blood may increase. This combination is recommended only for hypokalemia.
When indapamide with vincamine, bepridil, sultopride, halofantrine, as well as with simultaneous intravenous administration of erythromycin , arrhythmia and bradycardia may occur.
Sometimes, with simultaneous treatment with Insulin and Noliprel, hypoglycemia may develop.
When taking non-steroidal anti-inflammatory drugs, the antihypertensive properties of Noliprel are inhibited. If you are dehydrated, this combination of medications can cause kidney problems or kidney failure.
When treated with Noliprel and antipsychotics or tricyclic antidepressants, orthostatic hypotension may develop.
Due to the retention of water and electrolytes in the body, with simultaneous treatment with Noliprel and mineralocorticoids, glucocorticosteroids, stimulant laxatives, tetracosactide, amphotericin B, the hypotensive effect is reduced and the likelihood of hypokalemia increases.
Due to the possibility of developing hypokalemia, the risk of toxic effects of cardiac glycosides increases.
When combined with Metformin, acidosis may develop .
Before using iodine-containing X-ray contrast agents with Noliprel, the body must be adequately hydrated.
The simultaneous use of calcium salts can provoke hypercalcemia.
Concomitant treatment with cyclosporine may increase blood creatinine levels.
Instructions for use of Noliprel (Method and dosage)
It is advisable to take Noliprel tablets in the morning. The medicine is prescribed one tablet per day. The instructions for Noliprel Forte provide for a similar treatment regimen. Noliprel A and Noliprel A Bi Forte are prescribed to patients 1 tablet per day. If patients have creatinine clearance equal to or greater than 30 ml/min, then there is no need to reduce the dose. If clearance equals or exceeds 60 ml per day, then during treatment it is necessary to carefully monitor the level of potassium and creatinine in the blood.
If necessary, after several months of treatment, the doctor may increase the dose by prescribing Noliprel A Forte or another type of this drug instead of Noliprel.