Emla cream for local/external use 30g
Active substance
prilocaine
ATX code
N01BB20 (Combination drugs)
Release form, packaging and composition of the drug
◊ Cream for local and external use
white, uniform.
| 1 g | |
| lidocaine | 25 mg |
| prilocaine | 25 mg |
[PRING] macrogol glyceryl hydroxystearate (Arlaton 289) - 19 mg, carbomer 974P (carboxypolymethylene) - 10 mg, sodium hydroxide - 5.2 mg (to bring the pH to 8.7-9.7), purified water - up to 1 g.
5 g - aluminum tubes (5) - cardboard packs with first opening control. 30 g - aluminum tubes (1) - cardboard packs.
Clinical and pharmacological group
Local anesthetic for superficial anesthesia
Pharmacotherapeutic group
Local anesthetic
pharmachologic effect
Systemic absorption of Emla cream depends on the dose, duration of application and thickness of the skin (depending on the area of the body), as well as other skin characteristics, such as skin diseases and shaving. When applied to the ulcerative surface of the lower extremities, the absorption of the drug may be influenced by the characteristics of the ulcers, for example, the size (with an increase in the area of the ulcer, absorption increases).
Intact skin
In adults, after applying 60 g of cream to an area of 400 cm2 of intact thigh skin (1.5 g per 10 cm2) for 3 hours, systemic absorption for lidocaine was approximately 3% and for prilocaine 5%. Absorption is slow. Cmax of lidocaine (average value 0.12 μg/ml) and prilocaine (average value 0.07 μg/ml) in blood plasma was achieved approximately 4 hours after application of the cream. The risk of toxic symptoms exists only when the concentration of active substances in the blood plasma is 5-10 mcg/ml. When Emla cream is applied to intact skin 8-12 hours after shaving, the plasma Cmax of lidocaine and prilocaine in both young and elderly patients is very low and well below possible toxic levels.
Trophic ulcers of the lower extremities
The time to reach Cmax of lidocaine (0.05-0.84 mcg/ml) and prilocaine (0.02-0.08 mcg/ml) in blood plasma is 1-2.5 hours from the moment the drug is applied to the ulcer surface (5-10 g of cream for 30 minutes).
With repeated application of the cream to the ulcerative surface, there was no accumulation of prilocaine, lidocaine or their metabolites in the blood plasma. 2-10 g of Emla cream was applied to the ulcer surface with an area of up to 62 cm2 for 30-60 minutes from 3 to 7 times a week (15 times within a month).
Mucous membrane of the genital organs
The time to reach Cmax of lidocaine and prilocaine in the blood plasma (on average 0.18 mcg/ml and 0.15 mcg/ml, respectively) is approximately 35 minutes from the moment the drug is applied to the vaginal mucosa (10 g of cream for 10 minutes).
Indications for use
In adults:
- superficial anesthesia of the skin during injections (including vaccinations), punctures and catheterization of blood vessels and superficial surgical interventions, including minor cosmetic procedures and hair removal;
- superficial anesthesia of trophic ulcers of the lower extremities during surgical treatment (mechanical cleaning), for example, to remove fibrin, pus and necrotic tissue;
- superficial anesthesia of the mucous membrane of the genital organs before painful manipulations and for pain relief before injections of local anesthetics.
In children:
- superficial anesthesia of the skin during injections (including vaccination), punctures and catheterization of blood vessels and superficial surgical interventions (including removal of molluscum contagiosum).
Dosage
Externally on the skin, locally on the mucous membrane.
Adults
Superficial anesthesia of intact skin
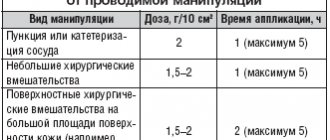
| Indication | Dose and method of application | Application time |
| When inserting a needle, for example when catheterizing blood vessels and taking blood samples | Apply half a 5 g tube (approximately 2 g) per 10 cm2 in a thick layer to the skin and cover with an occlusive dressing. | 1 hour, maximum 5 hours |
| For minor surgical procedures, such as curettage of molluscum contagiosum, removal of warts, minor cosmetic procedures and hair removal | Apply 1.5-2 g/10 cm2 in a thick layer to the skin and cover with an occlusive dressing | 1 hour, maximum 5 hours |
| On large areas of freshly shaved skin (on an outpatient basis), incl. before epilation | maximum recommended dose 60 g, maximum recommended application area 600 cm2; apply a thick layer to the skin and cover with an occlusive dressing | 1 hour, maximum 5 hours |
| For superficial procedures over large areas (in hospital settings), for example, skin harvesting using the split flap method | Apply 1.5-2 g/10 cm2 in a thick layer to the skin and cover with an occlusive dressing | 2 hours, maximum 5 hours |
Superficial anesthesia of trophic ulcers of the lower extremities
For surgical treatment (mechanical cleaning) of trophic ulcers of the lower extremities: a single dose of about 1-2 g/10 cm2; Apply the cream in a thick layer to the ulcer surface, no more than 10 g of cream per procedure. Apply an occlusive dressing. Application time: minimum 30 min.
An opened tube of cream is intended for single use; the tube with any remaining cream should be discarded after use on one patient.
In the case of treating ulcers, into the tissues of which penetration of the drug is difficult, the duration of application can be increased to 60 minutes. Mechanical cleaning must begin no later than 10 minutes after removing the cream.
When manipulating ulcers of the lower extremities, Emla cream was used up to 15 times over 1-2 months without reducing effectiveness and increasing the incidence of local reactions.
Superficial anesthesia of the genital organs
Genital skin
Anesthesia before injections of local anesthetics.
Men -
1 g/10 cm2;
apply the cream in a thick layer to the skin; application time - 15 minutes. Women
- 1-2 g/10 cm2; apply the cream in a thick layer to the skin; application time - 60 min.
Superficial anesthesia of the genital mucosa
When removing condylomas and for pain relief before injections of local anesthetics.
Approximately 5-10 g of cream, depending on the area of the treated surface. The cream should be applied to the entire surface of the mucous membrane, including the folds of the mucous membrane. No occlusive dressing is required. Application time: 5-10 min. Carry out the procedure immediately after removing the cream.
Children
Anesthesia during needle insertion (including vaccination), curettage of molluscum contagiosum and other minor superficial surgical procedures.
Apply the cream in a thick layer to the skin and cover with an occlusive dressing. The dose should correspond to the surface being treated and should not exceed 1 g of cream per 10 cm2
| Age | Application area | Duration of application |
| 0-3 months | maximum 10 cm2 (total 1 g of cream) (maximum daily dose) | 1 hour (important: no more than 1 hour) |
| 3-12 months | maximum 20 cm2 (total 2 g cream) | 1 hour |
| 1-6 years | maximum 100 cm2 (total 10 g of cream) | 1 hour (maximum 4 hours) |
| 6-12 years | maximum 200 cm2 (total 20 g of cream) | 1 hour (maximum 4 hours) |
A strip of Emla cream 3.5 cm long approximately corresponds to a dose of 1 g.
Increasing the application time reduces anesthesia. In children with atopic dermatitis
Application time should be reduced to 30 minutes.
Apply the cream in a thick layer to the skin and cover with an occlusive dressing.
Recommendations for applying the drug
1. Pierce the protective membrane of the aluminum tube using the screw cap, squeeze out a sufficient amount of cream from the tube and apply to the site of the intended procedure. When anesthetizing the skin, it is possible to use occlusive stickers (attached to the 5x5 g package).
2. a. Take one of the occlusion stickers and remove the center portion.
b. Separate the paper lining from the paper edging on the back of the headband
When anesthetizing trophic ulcers of the lower extremities, use an occlusive PVC dressing.
3. Cover the applied cream with a bandage so that the layer of cream underneath is thick and does not squeeze out from under the bandage. Gently smooth the edges of the bandage to avoid cream leakage.
4. If using the occlusion sticker included in the package, remove the paper frame. The time of application of the drug can be recorded directly on the bandage.
5. After the recommended time has passed, remove the bandage and any remaining cream from the surface.
Contraindications
- hypersensitivity to amide-type local anesthetics or any other component of the drug;
- premature newborns born at less than 37 weeks of gestation;
- newborns weighing less than 3 kg.
Carefully:
glucose-6-phosphate dehydrogenase deficiency, hereditary or idiopathic methemoglobinemia, common neurodermatitis (atopic dermatitis), patients taking class III antiarrhythmic drugs (eg, amiodarone).
Overdose
If the recommended dosage regimen is followed, the development of signs of systemic toxicity is unlikely.
Symptoms
intoxications are probably the same as with the use of other local anesthetics, for example, stimulation of the central nervous system, and in severe cases, depression of the central nervous system and cardiac activity.
In rare cases, the development of clinically significant methemoglobinemia has been observed. Prilocaine in high doses can cause an increase in methemoglobin levels.
Superficial application of 125 mg of prilocaine for 5 hours caused the development of moderate methemoglobinemia in a child aged 3 months. Superficial application of lidocaine at a dose of 8.6-17.2 mg/kg caused serious intoxication in newborns.
Treatment:
severe neurological symptoms (convulsions, central nervous system depression) require symptomatic treatment, incl. prescribing anticonvulsants and, if necessary, mechanical ventilation. In case of development of methemoglobinemia, the antidote is methylthioninium chloride (methylene blue).
Due to the slow systemic absorption of the drug, patients should be monitored for several hours after starting treatment for intoxication.
Side effects
When applied to intact skin
| Common (≥1%, 10%) | Skin: transient local reactions in the area where the drug is applied, such as pallor, redness and swelling. |
| Uncommon (≥0.1%, 1%) | Skin: at the first moment after application there is a slight burning sensation, itching and a feeling of warmth (in the area where the drug is applied). |
| Rare (<0.1%) | General: allergic reactions, in the most severe cases – anaphylactic shock. Methemoglobinemia and/or cyanosis. Reactions in the area of application of the drug, such as hemorrhagic rash or pinpoint hemorrhages, especially after prolonged application in children with atopic dermatitis or molluscum contagiosum. Irritation of the cornea due to accidental contact of the cream with the eyes. |
When applied to trophic ulcers of the lower extremities
| Common (≥1%, <10%) | Skin: transient local reactions in the area of application of the drug, such as pallor, redness and swelling; at the first moment after application there is a slight burning sensation, itching and a feeling of warmth (in the area where the drug is applied). |
| Uncommon(≥0.1%, 1%) | Skin: skin irritation (in the area where the drug is applied). |
| Rare(<0.1%) | General: allergic reactions, in the most severe cases – anaphylactic shock. |
Overdose
In patients receiving drugs that induce the development of methemoglobinemia (for example, drugs containing a sulfo group), Emla cream may help increase the concentration of methemoglobin in the blood.
When treating with other local anesthetics and drugs structurally similar to them (including tocainide), the risk of increased systemic effects when using high doses of Emla cream should be taken into account.
No specific studies have been conducted to evaluate the interaction of lidocaine/prilocaine with class III antiarrhythmic drugs; caution should be exercised when using drugs together.
Drugs that reduce the clearance of lidocaine (eg, cimetidine or beta-blockers) may cause potentially toxic plasma concentrations when repeated high doses of lidocaine are administered over an extended period of time. This interaction is not clinically significant during short-term therapy with lidocaine (eg, Emla cream) at recommended doses.
Pharmaceutical interactions
not detected.
Storage conditions
The drug should be stored out of the reach of children at a temperature below 30°C. Do not freeze. Shelf life: 3 years. Do not use after the expiration date stated on the package.
Conditions for dispensing from pharmacies
The drug is available without a prescription.
Special Instructions
Patients with glucose-6-phosphate dehydrogenase deficiency or hereditary or idiopathic methemoglobinemia are more susceptible to drug-dependent methemoglobinemia.
The effectiveness of using the cream in newborns during the procedure of taking blood samples from the heel has not been established.
Care should be taken when applying Emla cream to the skin around the eyes, as the drug causes eye irritation. Elimination of protective reflexes can cause irritation or damage to the cornea. If the cream gets into your eyes, immediately rinse your eyes with water or 0.9% sodium chloride solution and protect your eyes until protective reflexes are restored.
Caution must be exercised when applying the drug to the skin with atopic dermatitis; Application time should be reduced (15-30 min).
Patients taking class III antiarrhythmic drugs (for example, amiodarone) should be under constant monitoring and ECG control, because Possible effect on cardiac activity.
Emla cream should not be applied to a damaged eardrum or in other cases of possible penetration of the cream into the middle ear.
The cream should not be applied to open wounds.
Lidocaine and prilocaine in concentrations above 0.5-2% have bactericidal and antiviral properties. In this regard, it is recommended to take special care when applying the cream before subcutaneous administration of a live vaccine (for example, BCG).
Use in pediatrics
Due to the lack of data on the absorption of the drug, it is not recommended to apply the cream to the genital mucosa in children.
In children under 3 months of age
The safety and effectiveness of Emla cream was determined after applying a single dose. In such children, after applying the cream, a temporary increase in the level of methemoglobin in the blood was often observed, lasting up to 13 hours. However, the observed increase in the level of methemoglobin in the blood is probably not clinically significant.
Due to the lack of data, the combined use of Emla cream and drugs that cause methemoglobinemia is not recommended in children aged 0 to 12 months.
.
Impact on the ability to drive vehicles and machinery
Does not affect the ability to drive vehicles or operate equipment.
Emla cream for local and external use, tubes of 5 g, 5 pcs.
EMLA cream contains lidocaine and prilocaine, which are amide-type local anesthetics, as active ingredients. Skin anesthesia is caused by the penetration of lidocaine and prilocaine into the layers of the epidermis and dermis. The degree of anesthesia depends on the dose of the drug and the duration of application. Intact skin. After applying EMLA cream to intact skin for 1-2 hours, the duration of anesthesia after removing the occlusive dressing is 2 hours. There were no differences in efficacy (including time to achieve analgesic effect) and safety when applying the cream to intact skin between elderly (65-96 years) and younger patients. Due to the effect of EMLA cream on superficial vessels, temporary paleness or redness of the skin is possible. Similar reactions in patients with widespread neurodermatitis (atopic dermatitis) may occur faster, within 30-60 minutes after applying the cream, which indicates faster penetration of the cream through the skin. For puncture biopsy (4 mm in diameter), the use of EMLA cream provides adequate anesthesia of intact skin in 90% of patients 60 minutes after application of the cream when the needle is inserted to a depth of 2 mm and after 120 minutes when the needle is inserted to a depth of 3 mm. The effectiveness of EMLA cream does not depend on skin color or pigmentation (skin types I-IV). When using combination vaccines against infections such as measles, rubella, mumps, or intramuscular combined vaccines against diphtheria, whooping cough, tetanus, polio and infection caused by Haemophilius influenzae type b, as well as vaccination against hepatitis B, the use of EMLA cream did not affect on the average antibody titer, the rate of appearance or disappearance of specific antibodies in the blood serum, or the number of patients who achieved a protective or positive antibody titer after immunization. Mucous membrane of the genital organs. Anesthesia of the genital mucosa is achieved faster compared to anesthesia of intact skin due to faster absorption of the drug. In women, 5-10 minutes after applying EMLA cream to the mucous membrane of the genital organs, anesthesia sufficient to relieve pain caused by the use of an argon laser is achieved; The duration of anesthesia is 15-20 minutes (taking into account individual characteristics from 5 to 45 minutes). Trophic ulcers of the lower extremities. After applying the cream when treating trophic ulcers of the lower extremities, the duration of pain relief is up to 4 hours. There was no negative effect of the drug on the healing process of ulcers or on bacterial flora.