How does Herceptin work?
It has been established that Herceptin causes immune-mediated cytotoxicity, blocks proliferation and apoptosis of target cells, and has antiangiogenic activity. The principles of using Herceptin in the treatment of breast cancer, both as monotherapy and in combination with cytostatic drugs, are discussed in detail. Treatment with Herceptin may be effective for other types of tumors. Herceptin, unlike traditional chemotherapy drugs, affects only cancer cells with an increased content of HER2 receptors and therefore causes fewer side effects.
Operating principle
In some patients with breast cancer, the receptor for epidermal growth factor type 2 (HER-2/neu) is present in excess quantities on the membranes of tumor cells. This receptor interacts with this factor, present in the blood of patients, and causes accelerated tumor growth. The presence of such a receptor on cell membranes occurs in 30% of cases of breast cancer and in 6 - 40% of cases of advanced gastric cancer. It is associated with a lower rate of successful treatment of patients.
The drug Herceptin selectively binds to this receptor, preventing it from contacting the growth factor. As a result, a cytotoxic effect of the drug is observed, that is, tumor cells stop dividing and die.
Indications for use of Herceptin:
Metastatic breast cancer with tumor overexpression of HER2:
- as monotherapy, after one or more chemotherapy regimens;
- in combination with paclitaxel or docetaxel, in the absence of previous chemotherapy (first line of therapy);
- in combination with aromatase inhibitors for positive hormonal receptors (estrogen and/or progesterone) in postmenopausal women.
Early stages of breast cancer with tumor overexpression of HER2:
- in the form of adjuvant therapy after surgery, completion of chemotherapy (neoadjuvant or adjuvant) and radiation therapy;
- in combination with paclitaxel or docetaxel after adjuvant chemotherapy with doxorubicin and cyclophosphamide;
- in combination with adjuvant chemotherapy consisting of docetaxel and carboplatin;
- in combination with neoadjuvant chemotherapy and subsequent adjuvant monotherapy with Herceptin for locally advanced (including inflammatory form) disease or in cases where the tumor size exceeds 2 cm in diameter.
Pharmacokinetics
The administration of Herceptin in the form of short intravenous infusions once a week with a dosage of 10–500 mg is characterized by nonlinear pharmacokinetics. As the dose increases, a decrease in clearance is observed.
The half-life of the drug is 28–38 days. If Herceptin is discontinued, the withdrawal period lasts 27 weeks.
Mode of application
Testing for HER2 expression by the tumor is performed before starting therapy. The drug Herceptin is administered exclusively intravenously; Under no circumstances should the drug be administered intravenously. The medicine is compatible with infusion bags made of PVC, polyethylene, polypropylene.
According to the instructions for the Herceptin drug, the solution is prepared under strict aseptic conditions. Draw the solvent into a syringe and use it to dissolve the contents of the bottle with lyophilisate. Rock the bottle to dissolve the powder as quickly as possible. The prepared solution is stable for 28 days at a temperature of 2–8 °C. Cannot be frozen.
Due to the risk of protein aggregation, Herceptin is incompatible with dextrose solution (5%). According to the instructions, the drug should also not be mixed or diluted with other medications. A special solvent (bacteriostatic water for injection) is supplied with the medication.
Sterile water for injection that does not contain preservatives can also be used as a solvent. In this case, the solution remains stable only for 24 hours!
Side effects
Chills, nausea, fever, pain, vomiting, cough, tremor, shortness of breath, dizziness, skin rash, hypertension, weakness, arterial hypotension, bronchospasm, wheezing in the lungs, tachycardia, respiratory distress syndrome.
Side effects
The medicine is usually quite well tolerated. The most common side effects of Herceptin are:
- an infusion reaction (chills, shortness of breath, fever, etc.) occurs in 40% of patients upon first use, but is mild or moderate, and with further administration practically disappears;
- febrile neutropenia - a decrease in the number of neutrophilic leukocytes in the blood, accompanied by fever; infections such as pneumonia, cystitis, erysipelas of the skin may occur;
- headache, dizziness, muscle tremors;
- conjunctivitis and lacrimation;
- heart rhythm disturbances and heart failure;
- shortness of breath, wheezing, runny nose, cough, nosebleeds;
- nausea, vomiting, abdominal pain, loose stools;
- redness and swelling of the face;
- pain in muscles and joints.
The use of the drug Herceptin can also cause severe complications from the heart, nervous system, lungs, as well as allergic reactions. Therefore, its use is permissible only in well-equipped clinics under the supervision of experienced doctors.
Such conditions have been created in all oncology departments in Israel.
The place of Herceptin in oncological practice
IN
Recently, several highly effective drugs for targeted therapy have entered into oncology practice. One such drug is Herceptin. It, like other members of the group, blocks certain proteins inside tumor cells associated with tumor growth, progression and metastasis.
Trastuzumab (Herceptin)
is a recombinant monoclonal antibody that binds to the HER2/neu receptor on the surface of tumor cells in many solid tumors.
The high effectiveness of Herceptin is associated with the mechanisms of action of antibodies to HER2/neu. They not only cause immune-mediated (antibody- and complement-dependent) cytotoxicity, but directly block proliferation and induce apoptosis in HER2/neu positive cells. Herceptin has also shown antiangiogenic activity [14]. It inhibits the synthesis of TGF-β, angiopoietin-1, plasminogen activator inhibitor-1 (PAI-1) and possibly VEGF. In addition, it induces the synthesis of thrombospondin-1 (angiogenesis inhibitor).
Significance of HER2/neu overexpression for breast cancer patients
The HER-2/neu protein is a member of the epidermal growth factor receptor family. Overexpression of HER-2/neu in breast cancer tissue was found in 20–30% of patients.
Overexpression of HER-2/neu in a tumor (HER-2/neu+ tumor) is accompanied by a sharp decrease in apoptosis, increased proliferation, a decrease in estrogen receptors in the tumor, a decrease in the effectiveness of chemotherapy and endocrine therapy, etc. As a result, tumors with HER–2/neu+ status have a more aggressive course and higher resistance to therapy. HER2/neu has been shown to potentiate the activity of other receptors of the family: HER1 (EGFR), HER3 and HER4.
To date, sufficient clinical evidence has accumulated that overexpression of HER2/neu is associated with resistance to hormone therapy with tamoxifen in estradiol- and progesterone-positive patients. However, modern antiaromatase drugs are equally effective in both ER+HER2/neu– tumors and ER+HER2/neu+ tumors. A study was conducted comparing the effectiveness of aromatase inhibitors and tamoxifen in the neojuvant setting in patients with overexpression of HER2/neu+ER+. Remission rates were 88% for aromatase inhibitors and 21% for patients treated with tamoxifen. This means that aromatase inhibitors are able to overcome drug resistance in patients with HER-2/neu positive status.
Clinical use of Herceptin for the treatment of breast cancer
Currently, Herceptin has taken a strong position in the treatment of breast cancer. Herceptin is approved for clinical use in monotherapy in patients with HER-2/neu+ metastatic breast cancer in the II-III line alone, as well as in combination with cytostatic agents in patients who have not previously received chemotherapy for metastatic cancer.
Herceptin is effective when used independently in the first line of metastatic breast cancer. Among 114 patients with HER2+++ or HER2++, (FISH– or FISH+), significant tumor regression was achieved with HER2+++ – in 35% of patients, with HER2++ FISH+ – in 34% of patients. At the same time, with HER2++ FISH– the therapeutic effect was not achieved in any case. 57% of patients with complete or partial remission and 51% of patients with long-term stabilization (more than 6 months) did not have progression for more than 12 months when treated with Herceptin. In the treatment of 336 patients, complete or partial remission was obtained in the first and second line of breast cancer therapy in 26% and 22% of patients, respectively. The frequency of treatment effect also depended on the degree of HER2 overexpression. With overexpression of HER23+ or FISH+, the effect rate was 41%, although in the overall group (HER23+ or HER22+) it was only 26%.
Two regimens for the use of Herceptin have been developed [21]:
1. Weekly intravenous administration at a dose of 2 mg/kg, 30-minute infusion (first dose 4 mg/kg, 90-minute infusion).
2. Administration once every 3 weeks intravenously at a dose of 6 mg/kg, 90-minute infusion (first dose 8 mg/kg, 90-minute infusion).
Important: Herceptin should only be administered in saline sodium chloride solution!
Herceptin is usually well tolerated by patients. Chills, increased body temperature, and asthenia are usually observed after the first injection; subsequently, their frequency decreases and does not exceed 5%. After the first administration, acute infusion reactions (shortness of breath, anaphylaxis) may also occur with a frequency of 3:1000; extremely rarely they can be life-threatening. Therapeutic measures give a quick effect. In the future, treatment with Herceptin can be continued with additional medication, which ensures the safety of treatment.
7% of patients receiving second-line Herceptin develop cardiotoxicity after anthracycline-containing regimens. When Herceptin was combined with anthracyclines, the incidence of cardiotoxicity increased to 28% of cases. Cardiotoxicity is characterized by the development of symptoms of cardiovascular failure. In most cases (79%), standard treatment for cardiovascular failure is effective. Of course, Herceptin administration should be discontinued in such cases. Echocardiography every 3 months is recommended for early detection of cardiotoxicity. Given the lack of significant improvement in treatment effect and the increased risk of cardiotoxicity, the Herceptin + doxorubicin combination is not recommended.
The most impressive results are the clinical use of Herceptin in combination with various chemotherapy regimens. Patients (HER23+ or HER22+) who did not receive adjuvant anthracyclines were randomized to doxorubicin 60 mg/m2 + cyclophosphamide 600 mg/m2 in combination with Herceptin or alone. Patients receiving anthracycline-containing regimens postoperatively were randomized to receive paclitaxel in combination with Herceptin or alone [1]. The results of the study are shown in Table 1. This study shows that the addition of Herceptin to standard chemotherapy regimens is associated with an increase in overall response rate and prolongation of time to progression
.
The combination regimen of vinorelbine (30 mg/m2 weekly) and Herceptin (4 mg/kg day 1, then 2 mg/kg weekly) in the first line of MBC turned out to be highly effective.
When treating patients, the effect rate was 78%, with 82% in HER23+ and 58% in HER22+ [2]. Preclinical trials have shown synergistic effects between platinum agents, taxanes, and Herceptin. The BCIRG group conducted a randomized, multicenter, two-arm trial of the combination of cisplatin or carboplatin with docetaxel and Herceptin. Group 1: docetaxel 75 mg/m2 in combination with cisplatin 75 mg/m2 - every 3 weeks and Herceptin weekly. Group 2: docetaxel 75 mg/m2 in combination with carboplatin AUC 6 - every 3 weeks and Herceptin weekly [3]. The results of the study are shown in Table 2.
It should be noted that in group 1 (FISH+ subgroup) the median time to progression was 12.7 months, and in group 2 (FISH+ subgroup) – 17 months.
Combinations of Herceptin with other cytotoxic agents are being studied.
The high activity of the combination of paclitaxel and docetaxel with Herceptin in metastatic breast cancer became the basis for its study in neoadjuvant treatment. Paclitaxel (175 mg/m2 every 3 weeks) in combination with weekly Herceptin was used in neoadjuvant chemotherapy of patients with stage II–III breast cancer. The number of courses performed was 4. Among 40 operated patients, complete disappearance of the tumor was achieved according to morphological examination in 25% of cases, complete + partial clinical remission was achieved in 64% of cases.
Van Pelt AE et al. published preliminary results of the combination of weekly trastuzumab with docetaxel 100 mg/m2 every 3 weeks in patients with locally advanced breast cancer. Preliminary data showed that 81% (of 16 patients included) had a clinical effect (Table 3).
In case of ineffective treatment with Herceptin in the first line, it is possible to use a combination of Herceptin with another type of chemotherapy in the second line. It has been shown that the use of Herceptin ± Taxanes/vinorelbine regimens in the 2nd line of therapy after progression while taking Herceptin ± Taxanes is also highly effective.
A series of studies are currently underway on the adjuvant use of Herceptin after completion of standard chemotherapy regimens (NSAPB B-31, BCIRG 006, PACS 004, HERA) [6].
It is planned to conduct a series of studies on the combination of Herceptin with other targeted drugs, as well as, if possible, a combination with anthracyclines, which have lower cardiotoxicity (Fig. 1).
Rice.
1. The most promising combinations of Herceptin (G) with other targeted drugs Possibilities of using Herceptin for the treatment of other malignant tumors
The high effectiveness of Herceptin in patients with breast cancer opens up prospects for its use in other neoplasms. A big problem is the lack of standards for determining HER2/neu overexpression in patients with other neoplasms.
The high effectiveness of Herceptin in patients with breast cancer opens up prospects for its use in other neoplasms. A big problem is the lack of standards for determining HER2/neu overexpression in patients with other neoplasms.
Overexpression of HER2 has been found in various malignant tumors (non-small cell lung cancer, colorectal cancer, pancreatic cancer, head and neck cancer, prostate cancer, thyroid cancer, etc.). The effectiveness of Herceptin is being studied for the treatment of patients with prostate cancer, non-small cell lung cancer, ovarian cancer, bladder cancer and other tumors with overexpression of HER2/neu.
23 patients with metastatic pancreatic cancer with overexpression of HER-2/neu (2–3+) received gemcitabine 1000 mg/m2/week for 7–8 cycles, then every 3 weeks, Herceptin (4–2 mg/kg/week). 24% of patients had a partial effect according to computed tomography, 47% of patients had a decrease in the level of CA19-9 in the blood serum by more than 2 times [9].
A study was conducted comparing the effectiveness of a combination of gemcitabine (1250 mg/m2, days 1.8) and cisplatin (75 mg/m2, day 1) - 6 cycles, alone and in combination with Herceptin in NSCLC with overexpression of HER-2/neu (2- 3+). Of the 103 patients, the remission rate was 41% and 32%, respectively. The median time to progression was 7.2 and 6.3 months. respectively.
The combination of Herceptin in a standard weekly regimen and irinotecan 125 mg/m2 weekly, 4 weeks, 2 weeks interval for colorectal cancer in the second line was studied. 5 out of 7 patients had partial remission [12].
For disseminated bladder cancer, a combination of weekly Herceptin, paclitaxel 200 mg/m2, carboplatin AUC 5 and gemcitabine 800 mg/m2 was used. Of the 13 patients, 9 had partial remission [13].
Most studies have shown that Herceptin has high efficacy in patients with different types of tumors with overexpression of HER2/neu and low toxicity
. Further randomized studies of the effectiveness of Herceptin in combination with chemotherapy are required.
There is an urgent need to more carefully evaluate overexpression and determine the indications for Herceptin. The degree of HER2/neu overexpression determines the therapeutic effect of Herceptin and its combinations with chemotherapeutic drugs.
Prospects for further clinical use of Herceptin are associated with a more detailed analysis of HER-2/neu overexpression (IHC or FISH), elucidation of correlations of HER-2/neu with the clinical course of the disease and the effectiveness of treatment in various types of tumors.
Methods for determining HER-2/neu overexpression in tumors
Today, immunohistochemistry is the main method for determining overexpression of the HER-2/neu protein. For an accurate determination, a number of conditions must be met when fixing the material and performing an immunohistochemical reaction.
For the study, paraffin blocks of patients are used, fixed in neutral formalin for 18–36 hours. To study HER2/neu overexpression, antibodies CB11 (Novocastra, Ventana), A0485 (Dako) or 4D5 are used. It is necessary to heat treat the sections in 0.01 mM citrate buffer (pH 6.0) in a water bath at 95–99°C. There is a standardized immunohistochemical test system for assessing HER2/neu protein expression, used by the FDA, HercepTest (Dako Corp, Carpinteria, CA) [16]. The HerceptTest is recommended by the FDA for selecting patients for Herceptin treatment.
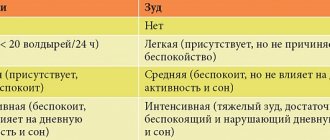
Of fundamental importance is the calculation of the results of determining HER2/neu overexpression, since it is the degree of HER2/neu overexpression that determines the therapeutic effect of Herceptin (Table 4) [18].
The recently developed fluorescence in situ hybridization (FISH) method is a rapid, sensitive and highly reliable method for detecting HER-2/neu gene amplification. It can be easily performed on archival blocks stored for a long period, on material obtained from trypanobiopsies. 2 test systems for determining HER2/neu gene amplification by FISH method are recommended by the FDA along with HercepTest. These are PathVysion HER–2 [Vysis, Inc, Downers Grove, Ill] and Oncor/Ventana INFORM HER–2/neu Gene Detection System.
To determine “true” gene amplification, it is important to determine the ratio: the number of HER2/neu genes / the number of 17 chromosomes per cell nucleus. In some cases (especially in neoplasms other than breast cancer), polysomy of chromosome 17 (an increase in the number of copies of chromosome 17) often occurs while maintaining a normal gene/chromosome ratio. The significance of polysomy for the prescription of Herceptin has hardly been studied [19].
The effectiveness of Herceptin among FISH+ tumors coincides with the effectiveness in HER2/neu+++ patients.
Today, it should be recommended to prescribe Herceptin to patients with breast cancer alone or in combination with chemotherapy only with a strictly positive test (3+) both when using HercepTest and other immunohistochemical studies. For 2+, a FISH study is recommended, and only if the result is positive, patients should be prescribed Herceptin. For other malignant tumors, it is recommended to use the same criteria.
conclusions
Herceptin is a highly effective targeted drug for the treatment of breast cancer patients with HER2/neu overexpression. A large number of clinical studies are studying the effectiveness of Herceptin in other malignant tumors that have overexpression of HER2/neu according to IHC or FISH.
The successful clinical use of the epidermal growth factor receptor type II blocker - HER2/neu and its low toxicity opens up new opportunities for the creation of drugs that block other growth factor receptors, which can actually increase the effectiveness of treatment and the survival of patients without compromising the quality of life.
References:
1. Bangemann N., Burstein H., Harvey V., et al Trastuzumab A Review of its Use in the Treatment of Metastatic Breast Cancer Overexpressing HER2. Drugs 2002; 62(1), 209–243.
2. Jahanzeb M., Mortimer JE, Yunus F., et al. Phase II Trial of Weekly Vinorelbine and Trastuzumab as First–Line Therapy in Patients with HER2+ Metastatic Breast Cancer. The Oncologist, Vol. 7, No. 5, 410–417, October 2002.
3. Slamon DJ 2001 Update on Taxoter/Platinum/Herceptin combinations. Satellite meeting of the 24th San Antonio Breast Cancer Symposium. San Antonio, TX, USA.
4. Bangemann N., Kuhle A., Ebert A., et al. Capecitabine combined with Trastuzumab in the therapy of intensively pretreated HER2–overexpressing metastatic breast cancer [abstract]. Ann Oncol 2000; 11 Suppl. 4:143.
5. Miller KD, Sisk J, Ansari R, et al. Gemcitabine, paclitaxel, and trastuzumab in metastatic breast cancer. Oncology 2001 Feb; 15(2) Suppl. 3:38–40.
6. Harries M., Smith I. The development and clinical use of trastuzumab (Herceptin). Endocrine-Related Cancer 2002, 9 75–85.
7. Baselga J. Combined anti – EGF receptor and anti – HER2 receptor therapy in breast cancer: a promising strategy ready for clinical testing. Annals of Oncology 2002, 13:8–9.
8. Crone SA, Zhao YY, Fan L, et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. J. Nature Medicine, Vol. 8, No. 5, May 2002.
9. Safran H., Ramanathan R., Schwartz J., et al. Herceptin and gemcitabine for metastatic pancreatic cancers that overexpress HER–2/neu. [abstract] ECCO 2001/
10. Heinmoeller P., Gross C., Schmidtgen C., et al. HER2 status in non–small cell lung cancer: results from the patient screening for enrolment to a phase 2 study of herceptin. [abstract] European Journal of Cancer, Vol. 37, Suppl. 6, October 2001.
11. Tran HT, Herbst RS, Glisson BS, et al. Herceptin in combination with Cisplatin and Gemcitabine in patients with HER2 overexpressing, untreated, advanced. Non-small-cell Lung Cancer: Final report of a phase II trial. [abstract] Proc ASCO 2002.
12. Hwang JJ, Sinicrope F, Safran H, et al. A phase II Trial of Irinotecan and Trastuzumab in patients overexpressing HER–2/neu in metastatic colorectal cancer. [abstract] Proc ASCO 2001.
13. Hussain M., Smith DC, Al-Sukhum S., et al. Preliminary results of HER–2/neu screening and treatment with Trastuzumab (Herceptin), Paclitaxel, Carboplatin and Gemcitabine in patients with advanced urothelial cancer. [abstract] Proc ASCO 2002.
14. Izumi, Y., Xu, L., di Tomaso, E., Fukumura, D., Jain, RK Tumor biology: Herceptin acts as an anti–angiogenic cocktail. Nature – 2002. – Vol. 416. – P. 279 – 280.
15. Jacobs TW., Gown AM., Yaziji H. et al. Comparison of Fluorescence in situ hybridization and immunohistochemistry for the evaluation of HER–2/neu in breast cancer. J.Clin.Oncol. 1999; 17(7): 1974–1982.
16. Graziano C. HER–2 breast assay, linked to Herceptin, wins FDA's okay. CAP Today 1998; 12:13–16.
17. Jacobs TW., Gown AM., Yaziji H. et al. Specificity of HercepTest in determining HER–2/neu status of breast cancers using United States food and Drug administration–approved scoring system. J Clin Oncol 1999b; 17(7): 1983–1987.
18. Herceptin (Trastuzumab) full prescribing information. Genentech, Inc. South San Francisco, CA, USA, September 1998.
19. Bose S., Mohammed M., Shintaku P., Rao PN Her–2/neu gene amplification in low to moderately expressing breast cancers: possible role of chromosome 17/Her–2/neu polysomy. Breast 2002, 7(5): 337–44.
20. Yamauchi H., Stearns V., Hayes DF. When is a tumor marker ready for prime time? A case study of c–erbB–2 as a predictive factor in breast cancer. J Clin Oncol 2001, 19(8): 2334–2356.
21. Carbonell Castellon X., et al. Efficacy and safety of 3–weekly Herceptin monotherapy in women with HER–positive metastatic breast cancer. [abstract] Proc ASCO 2002; 19.
22. Normanno N et al. Cooperative inhibitory effect of ZD 1839 (Iressa) in combination with trastuzumab (Herceptin) on human breast cell growth. Annals of Oncology. 2002; 13, 65–72.
Contraindications
In some cases, the use of Herceptin is prohibited. These are the following situations:
- metastases to the lungs, causing severe shortness of breath, which requires additional oxygen therapy;
- pregnant and lactating women, as well as children under 18 years of age;
- individual intolerance.
With great caution, Herceptin can be used:
- with ischemic heart disease, hypertension and/or heart failure;
- for any lung diseases;
- after previous treatment with cardiotoxic chemotherapy drugs, including cyclophosphamide.