Isoptin CP 240 extended-release tablets 240 mg 30 pcs.
In vitro studies indicate that verapamil hydrochloride is metabolized by the cytochrome P450 isoenzymes CYP3A4, CYP1A2, CYP2C8, CYP2C9 and CYP2C18. A clinically significant interaction was observed with concomitant use of CYP3A4 inhibitors, which caused an increase in plasma levels of verapamil, while CYP3A4 inducers decreased its plasma concentration. Accordingly, when using such agents simultaneously, the possibility of interaction should be taken into account. The table provides a list of possible drug interactions due to changes in their pharmacokinetic parameters. Possible drug interactions when taking Verapamil: Alpha blockers. Prazosin. An increase in prazosin Cmax (~40%) does not affect the half-life of prazosin. Terazosin. Increased terazosin AUC (~24%) and Cmax (~25%). Antiarrhythmic drugs. Flecainide. Minimal effect on flecainide plasma clearance (<~10%); does not affect the clearance of verapamil in plasma. Quinidine. Decreased oral clearance of quinidine (~35%). Medicines for the treatment of asthma. Theophylline. Decreased oral and systemic clearance of quinidine (~20%). For smokers there is a decrease of ~11%. Anticonvulsants. Carbamazepine. Increased AUC of carbamazepine (~46%) in patients with resistant partial epilepsy. Antidepressants. Imipramine. Increase in AUC of imipramine (~15%) Does not affect the level of the active metabolite, desipramine. Antidiabetic agents. Glyburide. Smachglyburide increases (~28%), AUC (~26%). Antimicrobial agents. Erythromycin. Verapamil levels may increase. Rifampicin. The AUC of verapamil (~97%), Cmax (~94%), and oral bioavailability (~92%) decreases. Telithromycin. Verapamil levels may increase. Antitumor drugs. Doxorubicin. The half-life of doxorubicin decreases (~27%) and Cmax (~38%)*. Barbiturates. Phenobarbital. The oral clearance of verapamil increases by 5 times. Benzodiazepines and other tranquilizers. Buspirone. The AUC of buspirone, Cmax, increases by 3.4 times. Midazolam. The AUC of midazolam increases (~ 3 times) and Cmax (~ 2 times). Beta blockers. Metoprolol. The AUC of metoprolol (~32.5%) and Cmax (~41%) increases in patients with angina pectoris. Propranolol. Propranolol AUC (~65%) and Cmax (~94%) increase in patients with angina pectoris. Cardiac glycosides. Digitoxin. The total clearance (~27%) and extrarenal clearance (~29%) of digitoxin decreases. Digoxin. In healthy volunteers, Cmax increases by ~45-53%, Css by ~42% and AUC by ~52%. H2 receptor antagonists. Cimetidine. The AUC of R- (~25%) and S-(~40%) verapamil increases with a corresponding decrease in the clearance of R- and S-verapamil. Immunological agents. Cyclosporine. AUC, Css, Cmax increases by ~45%. Sirolimus. There may be an increase in sirolimus levels. Tacrolimus. Tacrolimus levels may increase. Lipid lowering agents. Atorvastatin. Possible increase in atorvastatin levels. Lovastatin. Possible increase in lovastatin levels. Simvastatin. The AUC (~2.6 times) and Cmax (~4.6 times) of simvastatin increases. Serotonin receptor antagonists. Almotriptan. The AUC (~20%) and Cmax (~24%) of almotriptan are increased. Uricosuric drugs. Sulfinpyrazone. Increased oral clearance of verapamil (~ 3 times), decreased bioavailability (~ 60%). Other. Grapefruit juice. Increased AUC of R- (~49%) and S-(~37%) verapamil and Cmax of R-(~75%) and S-(~51%) verapamil. Elimination half-time and renal clearance were unchanged. St. John's wort. The AUC of R- (~78%) and S-(~80%) verapamil decreases with a corresponding decrease in Cmax. * in patients with advanced neoplasms, verapamil does not affect the level or clearance of doxirubicin. In patients with small cell lung cancer, verapamil reduced the half-life and Cmax of doxirubicin. Antiarrhythmic drugs, beta blockers. Mutual enhancement of effects on the cardiovascular system is possible (more pronounced atrioventricular block, more significant decrease in heart rate, development of heart failure and increased hypotension). Antihypertensives, diuretics, vasodilators. Strengthening the hypotensive effect. Prazosin, terazosin. Additive hypotensive effect. Antiviral and drugs for the treatment of HIV infection. Ritonavir and antiviral drugs may inhibit the metabolism of verapamil, resulting in increased plasma concentrations. In this regard, the dose of verapamil should be reduced. Quinindine. Hypotension. Patients with hypertrophic obstructive cardiomyopathy may develop pulmonary edema. Carbamazepine. Increased plasma levels of carbamazepine and increased neurotoxicity. Adverse reactions characteristic of carbamazepine, such as diplopia, headache, ataxia or dizziness, may occur. Lithium. Increased lithium neurotoxicity. Rifampicin. May reduce the hypotensive effect of verapamil. Sulfinpyrazone. May reduce the hypotensive effect of verapamil. Muscle relaxants. The effect of muscle relaxants may be enhanced. Aspirin (acetylsalicylic acid). Increased bleeding. Ethanol (alcohol). Increased plasma ethanol levels. HMG-Co A reductase inhibitors (statins). Simvastatin/lovastatin. Concomitant use with verapamil may result in increased serum levels of simvastatin or lovastatin. In patients receiving verapamil, treatment with HMG-CoA reductase inhibitors (i.e. simvastatin/lovastatin) should be started at the lowest possible doses and increased thereafter. If it is necessary to prescribe verapamil to patients already receiving HMG-CoA reductase inhibitors, it is necessary to review and reduce their doses according to the concentration of cholesterol in the blood serum. Similar tactics should be followed when concomitantly prescribing verapamil with atorvastatin (although there is no clinical data confirming the interaction of verapamil and atorvastatin), since pharmacokinetic studies are clearly known to confirm that verapamil had a similar effect on the level of atorvastatin. Fluvastatin, pravastatin and rosuvastatin are not metabolized by CYP3A4 isoenzymes, so their interaction with verapamil is least likely.
Composition and release form
| Film-coated tablets, extended release | 1 table |
| verapamil hydrochloride | 240 mg |
| (the active substance is embedded in a hydrocolloid matrix of alginate, a natural polysaccharide; the rate of release is determined by diffusion and surface erosion; upon contact with the liquid contents of the intestine, the surface of the tablet swells to form a gel-like diffusion layer; specially included surface defects cause uniform erosion of the gel, and therefore provide almost constant diffusion characteristics; the combination of these two mechanisms allows controlled release of the active substance with almost zero-order kinetics of about 7 h) | |
| excipients: MCC; sodium alginate; povidone (constant K = 30); magnesium stearate; purified water; hypromellose; macrogol 400; macrogol 6000; talc; titanium dioxide; quinoline yellow; indigotine; mountain glycol wax |
in a blister 10, 15 or 20 pcs.; There are 1, 2, 3, 5 or 10 blisters in a cardboard box.
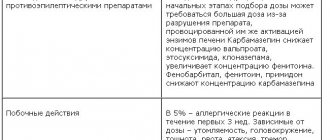
Side effects
Sometimes, when taking verapamil in high doses or in the presence of any cardiovascular disorders, the following may be observed: arrhythmia due to bradycardia (sinus bradycardia, sinoatrial block, AV block I, II or III degree or bradyarrhythmia with atrial fibrillation), arterial hypotension, palpitations , tachycardia, development or worsening of symptoms of heart failure.
Constipation has been reported to occur quite frequently when taking the drug orally; in rare cases, nausea, vomiting, intestinal obstruction, abdominal pain or discomfort, dizziness or drowsiness, increased fatigue, increased nervousness/tremor, swelling of the lower leg, erythromelalgia or paresthesia may develop.
In rare cases, dizziness, headache and hot flashes may occur. In very rare cases, myalgia and arthralgia may occur.
Allergic reactions (exanthema, urticaria, urticaria, angioedema, Stevens-Johnson syndrome) have been rarely reported. A reversible increase in the levels of liver transaminases and/or alkaline phosphatase and an increase in prolactin levels have also been described.
In rare cases, gynecomastia developed in elderly patients during long-term therapy, which in all cases was completely reversible after discontinuation of the drug. Cases of galactorrhea and impotence have been reported.
In extremely rare cases, during long-term treatment, gum hyperplasia may develop, which is completely reversible after discontinuation of the drug.
Overdose
Symptoms of poisoning resulting from an overdose of the drug Isoptin depend on the amount of the drug taken, the time of detoxification measures and the contractility of the myocardium (depending on age). Fatal cases resulting from overdose have been reported.
The following symptoms predominate: a drop in blood pressure (in some cases to levels that cannot be measured); shock, loss of consciousness; AV block of the 1st and 2nd degree, often with Wenckebach periods with or without escape rhythm; complete AV block with complete AV dissociation, escape rhythm, cardiac arrest; sinus bradycardia, sinus node arrest.
Treatment. Therapeutic measures should be carried out depending on the duration and method of taking the drug Isoptin and on the nature and severity of the symptoms of poisoning.
In case of overdose with a large number of long-acting film-coated tablets (i.e. Isoptin CP 240), it must be borne in mind that the active substance is released and absorbed in the intestine within 48 hours after taking the drug orally. Depending on the timing of oral administration of the drug, individual conglomerates of swollen tablet residues, acting as active depots, are likely to be located throughout the gastrointestinal tract.
General events.
If there is no motility of the stomach and intestines (signs of peristalsis during auscultation), then it is advisable to perform gastric lavage even 12 hours after taking the drug orally. If there is a suspicion of an overdose of the drug Isoptin CP 240, then appropriate measures aimed at eliminating the drug are indicated, for example, inducing vomiting, washing the stomach and intestines in combination with an endoscopic examination, taking laxatives and emetics.
Common emergency resuscitation measures include chest compressions, artificial respiration, and electrical stimulation of the heart.
Special events.
Elimination of effects associated with depression of cardiac function, arterial hypotension and bradycardia.
Calcium is a specific antidote: 10–30 ml of a 10% calcium gluconate solution is administered as an intravenous injection (2.25–4.5 mmol), if necessary, re-injected or as a slow drip infusion (for example, 5 mmol/h).
The following activities may be required.
In case of 2nd or 3rd degree AV block, sinus bradycardia, cardiac arrest: atropine, isoprenaline, orciprenaline or cardiac stimulation.
In case of arterial hypotension: dopamine, dobutamine, norepinephrine.
In case of persistent signs of myocardial failure: dopamine, dobutamine, additional calcium injections as necessary.
Pharmacokinetics
Verapamil, the active substance of the drug Isoptin CP 240, is quickly and almost completely absorbed in the small intestine. The degree of absorption is 90–92%. T1/2 - from 3 to 7 hours after a single dose of the drug orally. With repeated doses, T1/2 of verapamil can almost double compared to a single dose.
Verapamil is almost completely metabolized. The main metabolite is norverapamil, which has pharmacological activity; other metabolites are largely inactive.
Verapamil and its metabolites are excreted mainly through the kidneys; only 3–4% is unchanged. Within 24 hours, 50% of the administered dose of the drug is excreted in the urine, within 48 hours - 55–60% and within 5 days - 70%. Up to 16% is excreted in feces. Recent results indicate that there are no differences in the pharmacokinetics of verapamil between subjects with normal renal function and those with end-stage renal disease.
In case of coronary artery disease and arterial hypertension, no correlation was found between the therapeutic effect and the concentration of the drug in the blood plasma; there is only a definite relationship between plasma drug levels and the effect on the PR interval. After taking extended-release dosage forms, the plasma concentration curve of verapamil stretches and becomes flatter than with the administration of normal-release dosage forms.
About 90% of the drug binds to blood plasma proteins.
Bioavailability
Following oral administration, verapamil undergoes significant first-pass metabolism, which occurs almost exclusively in the liver.
The average absolute bioavailability in healthy volunteers after a single dose of the drug is 22%. Recent studies in patients with atrial fibrillation or angina showed mean bioavailability levels of 35 and 24% after a single oral and IV dose, respectively.
With repeated doses of the drug, bioavailability increases almost 2 times compared to a single dose. This effect is likely due to partial saturation of liver enzyme systems and/or a transient increase in hepatic blood flow after a single dose of verapamil. In patients with liver failure, compared with those with normal liver function, the bioavailability of verapamil was much higher and a delay in drug elimination was observed.
Penetration through the placenta
Verapamil penetrates the placental barrier; the concentration found in umbilical vein plasma was 20–92% of that in maternal plasma.
Excretion in breast milk
Verapamil is excreted in breast milk, but at therapeutic doses its concentration is so low that clinical effect in newborns is unlikely.
Contraindications
Absolute:
cardiogenic shock;
complicated acute myocardial infarction (bradycardia, severe arterial hypotension, left ventricular failure);
AV block II–III degree;
sick sinus syndrome (bradycardia-tachycardia syndrome);
sinoatrial block.
Relative:
AV block of the first degree;
bradycardia (<50 beats per minute);
arterial hypotension (sBP <90 mm Hg);
atrial fibrillation/flutter with WPW syndrome (risk of ventricular tachycardia);
heart failure (if necessary, cardiac glycosides are prescribed before starting treatment with Isoptin CP 240);
children's age (currently there is no convincing data on the safety of the drug in children under 18 years of age).
Pharmacodynamics
Verapamil inhibits the transmembrane current of calcium ions into smooth muscle cells. The antianginal effect is associated with a direct effect on the myocardium and an effect on peripheral hemodynamics (reduces the tone of peripheral arteries, peripheral arterial resistance). Blockade of the entry of calcium ions into the cell leads to a decrease in the transformation of energy contained in high-energy bonds of ATP into mechanical work and a decrease in myocardial contractility.
The antihypertensive effectiveness of Isoptin SR 240 is due to a decrease in peripheral vascular resistance without an increase in heart rate as a reflex response. Blood pressure begins to decrease immediately on the first day of treatment; this effect persists with long-term therapy. The drug Isoptin CP 240 is used for the treatment of all types of arterial hypertension: for monotherapy of mild or moderate arterial hypertension in combination with other antihypertensive drugs, especially diuretics and, according to recent observations, ACE inhibitors for more severe arterial hypertension. It has a vasodilating, hypotensive, negative ino- and chronotropic effect. The drug Isoptin CP 240 has a pronounced antiarrhythmic effect, especially in cases of supraventricular arrhythmia. It delays the conduction of impulses in the AV node. As a result, sinus rhythm is restored and/or the ventricular rate is normalized, depending on the type of arrhythmia. Normal heart rate does not change or decreases slightly.
Directions for use and doses
Orally, swallow whole, with water, preferably during a meal or immediately after a meal.
Doses of verapamil should be used depending on the clinical picture of the disease; Many years of clinical experience have shown that the average dose for all indications is 240–360 mg/day.
For long-term treatment, the daily dose should not exceed 480 mg; a temporary dose increase above this level is possible.
In patients with impaired liver function, the effect of verapamil is enhanced and becomes longer lasting as a result of slow metabolism of the drug, which depends on the severity of liver dysfunction. In such cases, the dose should be set with extreme caution and treatment should begin with lower doses (i.e., patients with liver cirrhosis are initially prescribed 1 film-coated tablet of Isoptin 40 mg 2-3 times a day).
| Indications for use | Recommended dose for adults |
| IHD: chronic stable angina; angina caused by vasospasm (Prinzmetal's angina, variant) | 240–480 mg/day Isoptin SR 240 — ½–1 tablet, film-coated, prolonged action, 2 times a day with an interval of 12 hours |
| Arterial hypertension (mild to moderate) | Isoptin SR 240 - 1 tablet, coated, prolonged action, in the morning. In cases where patients are especially indicated for a slow decrease in blood pressure, treatment should begin with ½ tablet, film-coated, prolonged release, in the morning. If necessary, additionally ½–1 tablet, film-coated, prolonged action, in the evening with an interval between doses of about 12 hours. If necessary, the dose should be increased every 2 weeks of treatment |
| Paroxysmal supraventricular tachycardia; atrial fibrillation/flutter accompanied by tachyarrhythmia | Isoptin SR 240 - ½–1 tablet, film-coated, prolonged action, 2 times a day with an interval of 12 hours |
The duration of use is not limited.