The structure of the eye has a complex structure, but it is not necessary to study it all in detail to understand what intraocular pressure is and why it suddenly deviates from the norm. It is enough to imagine the eye as a liquid surrounded by multiple membranes. The outer one is the sclera, behind it is a network of blood vessels, and even deeper is the ciliary body. When the muscles contract, the shape of the lens changes and the person can see something up close. But this is not the only function of the ciliary body.
Another important task assigned to it is the secretion of intraocular fluid. By circulating between the various chambers of the eye, it ensures normal metabolism and maintains a certain level of intraocular pressure (IOP). In other words, the fluid secreted by the ciliary body constantly puts pressure on the eye, setting the parameters of its normal size and shape. As soon as the amount of this fluid increases excessively or there are problems with its outflow, the pressure will jump. This will entail distortion of the shape, and, consequently, of the entire optical system of the eye.
Important! Intraocular pressure directly affects the quality and acuity of vision. When it deviates from the norm, the shape of the eyeball changes and the mechanisms of accommodation that allow close vision are disrupted.
Normal blood pressure and pathology
Intraocular pressure may fluctuate slightly depending on what time of day the test is performed, but in general it is a constant value. In the morning, intraocular pressure may jump by 2-3 marks. Most likely, the reason lies in the horizontal position of the body, slowing of the pulse and breathing, as well as the predominance of the parasympathetic nervous system during sleep. By evening the pressure gradually drops.
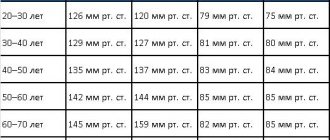
Normal intraocular pressure ranges between 10 and 21 mm. Hg column, although much depends on how the measurement is carried out. These numbers are the limit of true pressure, but if you try to determine it using a tonometric method, the norm will be different - from 12 to 25 mm. Hg Art. That is, it is simply not correct to compare indicators obtained by different methods.
Important! In domestic ophthalmological clinics, the method of the Russian researcher Maklakov is used to measure intraocular pressure. According to it, normal intraocular pressure is that which is below 26 mm Hg, from 27 to 32 mm Hg. Art. – moderately elevated, more than 33 mm Hg. - a reason to take action.
Indications for use
Tonometry is usually prescribed:
- patients after 40-45 years;
- potential owners of glaucoma, as well as those patients whose parents had this disease;
- pain or stinging in the organ of visual perception, migraine;
- the presence of retinal detachment or prerequisites for its development;
- diagnostics of the visual organ after surgery;
- anatomical defects in the structure of the eye;
- neurological and endocrine diseases;
- disruptions in the functioning of the heart muscle and blood vessels.
In general, the study is recommended to be carried out 1-2 times a year, especially if patients have any suspicion of the disease. This is the only way to identify pathologies at those stages when the chances of their cure are highest. But the norms of the results obtained can vary significantly, which will depend on the age, gender of the patient, or even on the type of study itself; this is also important to take into account.
Measurement according to Maklakov
- The patient lies down on the couch, and the doctor administers anesthesia by instilling several drops of dicaine into each eye in turn.
- Then the head is fixed and asked to look at one point.
- A small weight treated with special marking paint is carefully lowered onto the open eye, under the pressure of which the eyeball should be slightly deformed.
- Now the weight is lowered onto a sheet of paper to see how much paint is left on it. Intraocular pressure is determined by the intensity of the imprint.
- The procedure is repeated again in both eyes to avoid the possibility of misinterpretation.
Naturally, some amount of paint from the load will remain on the surface of the eyeball, but it will quickly be washed away with tears. Instead of weights, ophthalmologists sometimes use a portable device that looks like a ballpoint pen. They also apply pressure on the eye, having previously treated the eyeball with an anesthetic.
This method also has an alternative – non-contact tonometry. No weights are placed on the eye, but instead a controlled air flow is used. Many patients find this method more acceptable, but in reality it is rarely used - it is not as accurate.
Important! In patients with glaucoma, eye pressure fluctuates much more noticeably throughout the day than in healthy people. Having such suspicions, the doctor may ask the patient to come to the clinic several times throughout the day. To ensure the accuracy of the diagnosis, you need to measure your blood pressure at least three times before lunch, and the same number in the evening.
How to measure the pressure inside the eye yourself?
Without the help of a doctor and special equipment, it is impossible to determine with what force the fluid secreted by the ciliary body presses on the eye. Nevertheless, it is possible to understand that blood pressure is greatly increased, and ophthalmologists recommend that everyone master this simple technique.
Close your eyes and relax. Now gently press your index finger on the eyeball. You should feel an elastic ball that gives in to your pressure - this is normal. If the eye is very hard and practically does not deform, the IOP level is most likely elevated and it is better to consult a specialist to make sure that its value is not critical
Symptoms of ocular hypertension
signs indicate high ophthalmotonus :
- pain above the eyebrows and in the temple area. Pain also appears when the eyes move up;
- persistent headaches that do not disappear even after taking the medicine;
- cracked blood vessels on the whites of the eyes;
- feeling very tired in the evening;
- blurred vision after waking up, when it takes time for vision to normalize;
- when working visually, the eyes get tired quickly;
- When moving from a light room to a dark one, visibility decreases.
Eye pressure should be measured frequently . Symptoms of so-called ocular hypertension may sometimes not appear. Therefore, it is better to play it safe.
Why does intraocular pressure increase?
Two parts are responsible for the regulation of intraocular pressure - the nervous system and some hormones. That is why most often a temporary increase in IOP is associated with increased mental work, stress and the experience of violent emotions. In women, the risk of glaucoma can develop during menopause, when large-scale hormonal changes occur in the body.
So, the true cause of IOP most often needs to be looked for in one of the following directions.
- Chronic stressful situations, prolonged mental or physical stress.
- Problems with the cardiovascular system that provoke surges in blood pressure.
- Some kidney diseases, due to which a lot of fluid is retained in the body.
- Endocrine pathologies, in particular increased levels of adrenal hormones in the blood, hypothyroidism.
- Anatomical pathology in the structure of the eyeball. People suffering from atherosclerosis should be especially careful in this regard.
In any case, it is important to understand that intraocular pressure does not suddenly increase on its own, it is always a consequence. Sometimes - hidden pathological processes occurring in the body, and sometimes - diseases associated directly with the eyes. So, a jump in IOP can be provoked by:
- an eye tumor that puts pressure on the inner membranes and chambers of the eye, thereby interfering with the normal outflow of fluid;
- inflammatory disease of the iris (iritis), ciliary body (cyclitis), choroid (uveitis);
- severe eye injury, after which inflammation, swelling and stagnation of blood in the vessels inevitably appears.
Important! Under any of the above circumstances, IOP cannot be critically high all the time. It increases periodically, in jumps, which depend on the characteristics of the course of the disease that provokes it. But if the pathology is not found and treated, then with age, increased IOP can transform into glaucoma. Gradually, due to strong pressure, the retinal cells will be destroyed, the optic nerve will atrophy, and eventually the person will completely lose vision.
What is low ophthalmotonus
In addition to increased IOP, low blood pressure also occurs, although much less frequently. This condition may be caused by the following reasons:
- retinal detachment;
- inflammatory processes in the eyes;
- eye injuries;
- low blood pressure;
- dehydration and some others.
With reduced ophthalmotonus, the following symptoms are observed: dry eyes, painful sensations when blinking, pop-up dots, burning, blurred vision. Low IOP is no less dangerous than high IOP. Clinical examination of this condition reveals papilledema, venous congestion, maculopathy, papillar atrophy, vitreous opacities, and keratopathy. Visual functions deteriorate significantly.
How to relieve intraocular pressure?
Trying to deal with the consequences without eliminating the cause is useless. That is why, if you notice that your eyes are constantly tired, red and very tense, you need to look for a reason that provokes periodic jumps in intraocular pressure. Further, the method of eye restoration will depend on how neglected everything is.
If we are talking about the initial stages and barely noticeable symptoms, then, most likely, preventive measures alone will be sufficient:
- master a set of eye exercises and devote a few minutes a day to it;
- choose safety glasses for reading and standing in front of a monitor;
- As far as possible, limit any eye strain - TV, computer, working with small parts;
- give up contact and strength sports;
- Spend free time outdoors, giving your eyes a chance to rest and look into the distance.
Treatment of intraocular pressure with drops
When high IOP ceases to be episodic and develops into ocular hypertension or hypotension, preventive measures alone are not enough - timely local treatment is needed. With such diagnoses, the easiest way to regulate the pressure in the eye is with eye drops. They come in several types.
- Those that act directly on the ciliary body and reduce fluid production are carbonic anhydrase inhibitors. The most popular of this group are Azopt and Trusopt. By reducing the amount of intraocular fluid, the pressure also decreases, but this process can be accompanied by burning, severe redness of the eyes and even a bitter taste in the mouth.
- The second category is prostaglandins. They operate on a different principle: they affect not the amount of fluid, but its intensive outflow.
- Beta blockers. They also reduce the amount of fluid formed in the eye, but have one significant nuance - together with eye pressure, they reduce the heart rate, which is strictly contraindicated for heart patients.
There are also combination drugs that act in two directions: on the one hand, they inhibit the process of fluid production, and on the other, they increase its outflow.
Important! On average, drops are used twice a day, but the exact dosage and frequency of instillation can only be determined by a doctor, having an accurate description of the clinical picture. By self-medicating, you can not only further damage your vision, but also damage your cardiovascular system, lungs and kidneys.
Relieving intraocular pressure at home
If you feel pressure in your eyes, but cannot immediately get an appointment with an ophthalmologist, then instead of drops you can try to relieve painful symptoms using traditional methods. Helps normalize eye pressure:
- meadow clover decoction (brew with boiling water, leave for 2 hours and drink 100 g before bedtime);
- tincture of golden mustache (pour about 20 purple inflorescences with 500 grams of vodka and leave in a dark place for 12 days, then take one teaspoon before breakfast);
- a glass of kefir with cinnamon.
No matter how tempting such treatment may seem, ophthalmologists do not recommend relying too much on it. Such recipes can be used only if the pressure jumps rarely and not greatly. Trying to get rid of serious symptoms that indicate progressive blindness in this way is simply dangerous.
Most of these arrogant patients, when they finally get to the ophthalmologist’s office, hear one thing: “an operation is necessary.” A laser is used to relieve high intraocular pressure. Depending on where the problem is located, they can either excise the iris or stretch the trabecula to increase the flow of fluid.
If you don't want to end up in the operating room, take the advice of ophthalmologists seriously and constantly engage in prevention. A five-minute break every hour of working near the computer, a simple set of gymnastic exercises for the eyes, a dinner of sea fish and blueberry-carrot snacks - and you will maintain sharp vision for many years!
Cost of services for glaucoma
| № | Service name | Price in rubles | Make an appointment |
| 2010025 | Set of disposable consumables for antiglaucomatous surgery | 36000 | Sign up |
| 2010024 | Molteno valve implantation | 54000 | Sign up |
| 2010023 | Implantation of the EX-Pres shunt valve | 54000 | Sign up |
| 2010022 | Ahmed valve implantation | 54000 | Sign up |
| 2010021 | Summing collagen or silicone drainage | 9000 | Sign up |
| 2010020 | Pupilloplasty | 30000 | Sign up |
| 2010019 | Iridoplasty | 22200 | Sign up |
| 2010018 | Basal iridotomy | 10800 | Sign up |
| 2010001 | Sinutrabeculectomy (STE) | 42000 | Sign up |
| 2010002 | Non-penetrating deep sclerectomy (NPDS) | 46200 | Sign up |
| 2010004 | Antiglaucomatous surgery for primary glaucoma of the first category of complexity | 23400 | Sign up |
| 2010005 | Antiglaucomatous surgery for primary glaucoma of the second category of complexity | 30600 | Sign up |
| 2010006 | Antiglaucomatous surgery for primary glaucoma of the third category of complexity | 37200 | Sign up |
| 2010007 | Antiglaucomatous surgery for secondary or refractory glaucoma of the first category of complexity | 29500 | Sign up |
| 2010008 | Antiglaucomatous surgery for secondary or refractory glaucoma of the second category of complexity | 42000 | Sign up |
| 2010009 | Antiglaucomatous surgery for secondary or refractory glaucoma of the third category of complexity | 48000 | Sign up |
| 2010010 | Antiglaucomatous surgery with drainage of the anterior chamber angle for primary glaucoma of the first category of complexity | 28200 | Sign up |
| 2010011 | Antiglaucomatous surgery with drainage of the anterior chamber angle for primary glaucoma of the second category of complexity | 39300 | Sign up |
| 2010012 | Antiglaucomatous surgery with drainage of the anterior chamber angle for primary glaucoma of the third category of complexity | 45600 | Sign up |
| 2010013 | Antiglaucomatous surgery with drainage of the anterior chamber angle for secondary or refractory glaucoma of the first category of complexity | 33360 | Sign up |
| 2010014 | Antiglaucomatous surgery with drainage of the anterior chamber angle for secondary or refractory glaucoma of the second category of complexity | 43800 | Sign up |
| 2010015 | Antiglaucomatous surgery with drainage of the anterior chamber angle for secondary or refractory glaucoma of the third category of complexity | 54000 | Sign up |
| 2010017 | Reconstruction of the anterior chamber angle in secondary glaucoma | 27000 | Sign up |
Making an appointment Today: 13 registered
Preparing for the examination
If you wear contact lenses, regardless of the type of examination, you must remove them before the procedure and do not use them for at least two hours after completion. You can get to the clinic wearing glasses. Also, after the examination, it is highly recommended not to touch your eyes with your hands.
Clothes with tight collars, ties and other accessories that put pressure on the neck should be avoided. This may well inflate the indicators, affecting the accuracy of the study.
4 hours before the medical procedure, reduce the amount of fluid you consume; you should also not abuse alcohol or use drugs at least 12 hours before the appointed time.
Women should not overdo it with cosmetics and use eye shadow and mascara. Be prepared that all methods, except non-contact, use anesthesia. Make sure you are not allergic to the anesthetic used in the clinic.
Apart from the above, additional preparation of the eyes for any type of examination is not required.
Non-contact examination method
This approach does not require direct interaction with the organ of vision. During the study, the level of changes in corneal indentation under the influence of air shocks is monitored. The patient's head is fixed in front of a special device - a non-contact tonometer; the gaze must be focused at one point. Deformations of the cornea are recorded by certain tonometer sensors, which convert the data into a digital signal.
Advantages:
- no contraindications;
- no anesthetics required;
- no discomfort;
- low probability of infection;
- high accuracy of the results obtained.
Flaws:
- in some cases there is an underestimation of indicators;
- unreliability of data for prescribing treatment for glaucoma.
The method has proven itself to be fast and painless, ideal for screening groups of patients, people with hypersensitive eyes and, of course, children.
Contraindications
The main contraindications include:
- progressive corneal defects;
- state of alcohol or drug intoxication;
- external influence, injuries resulting in destruction of the membrane of the organ of vision;
- allergy to anesthetics;
- diseases of a bacterial or viral nature (it is possible to perform a tonometry procedure after completion of the course of treatment);
- severe migraine, pain in the eyes;
- diseases of the endocrine system, neurological.
It should be noted that the described contraindications apply only to contact research methods. Non-contact tonometry can be used even in the presence of relevant diseases. Next, we will consider in detail the main methods of tonometry.
What other consequences can occur with high blood pressure?
In most cases, an increase in IOP leads specifically to glaucoma, but there are cases when it also provokes the following disorders:
- Retinal detachment is the process of separation of the retina from the choroid. In a healthy eye they are in close contact. As a result of retinal detachment, a noticeable decrease in the quality of vision occurs;
- Optic neuropathy is the partial or complete destruction of the nerve fibers that are responsible for transmitting images to the brain. This can lead to distorted color vision.
These two eye disorders, along with glaucoma, if untimely intervention lead to blindness in almost 100% of cases. This is why it is so important to monitor the pressure inside the eyes, especially after the age of 40.
Applanation tonometry
The first study in our review related to the group of contact methods. The method is recognized as the most accurate, which has given it widespread use in medicine. All techniques in this group are quite painful due to direct contact with the cornea, so local anesthesia is required.
Internal pressure is measured by applying a certain amount of force (applanate) required to create a flat surface area. When the colored base of the tonometer comes into contact with the cornea, the coloring enzyme is distributed along its boundaries. The resulting prints are transferred to paper and measured. A smaller imprint will indicate greater internal pressure.
There are two types of applanation tonometry:
- tonometry according to Maklakov - a weight is used, the flat bottom of which is painted with a special substance;
- Goldman tonometry - fluorescein-stained plates are used, and pressure readings are read by a probe exposed to bright lighting.