Asthenia means weakness that occurs in the absence of exertion, lasts for a long time and does not go away even after a long rest. The main difference between asthenia and physiological fatigue is the ineffectiveness of sleep and its chronic course. In foreign literature, the term “chronic fatigue syndrome” is sometimes used to refer to asthenia.
Every fifth (10-25%) patient seeking medical help complains of asthenia [1]. In many cases, it is possible to establish a connection between asthenia and the effects of pathogenic biological or psychological factors. In particular, asthenia is a characteristic complaint of patients with organic diseases of the brain (chronic cerebrovascular insufficiency, post-traumatic encephalopathy, etc.) [1-3]. Such patients are especially susceptible to rapid mental exhaustion. Prescribing nootropic drugs, normalizing metabolic processes in the central nervous system, improves the well-being of such patients.
In many cases, asthenia is accompanied by mild to moderate cognitive impairment, autonomic dysfunction, emotional disturbances, including severe depression and anxiety. Thus, it was shown that 28% of patients with long-term (more than 6 months) current asthenia develop severe anxiety-depressive syndrome [3]. According to one of the multicenter placebo-controlled randomized studies [4], cytoflavin not only reduced the severity of asthenia in patients with asthenoneurotic syndrome against the background of chronic cerebral ischemia, but also improved cognitive functions and quality of life.
According to research by D.I. Laseeva and O.V. Dikova [5], cytoflavin had a positive effect on the emotional state in patients with eczema. In our previous study [6], we also observed more pronounced positive dynamics in women with depression due to organic brain disease who received cytoflavin as an additional therapy, compared with the control group (the study is being prepared for publication). In addition, in the same group of patients, we observed a normalization of autonomic disorders under the influence of cytoflavin.
Cytoflavin produced by NTFF POLYSAN LLC includes succinic acid, riboxin, nicotinamide and riboflavin, which are important components of normal metabolic processes in the brain. The drug is well tolerated and is used for encephalopathies of various origins (toxic, posthypoxic), for acute and chronic cerebrovascular accidents [7, 8]. In acute conditions, cytoflavin is used intravenously, and in chronic diseases it is prescribed in tablet form, 2 tablets 2 times a day for a course of at least 25 days [3].
The purpose of the study was to study the effect of cytoflavin as an additional therapy in patients with organic emotionally labile (asthenic) disorder.
Material and methods
The present study was observational.
The study included 100 patients, 49 men and 51 women, with organic emotionally labile (asthenic) disorder (F06.6 according to ICD-10), who underwent inpatient treatment at the Scientific and Practical Center for Psychoneurology of the Moscow Department of Health in 2012-2013.
The criteria for inclusion in the study were: severe asthenic disorders (75 or more points on the asthenic state scale) lasting at least 3 months as the main reason for seeking medical help; development of an asthenic state against the background of an organic brain disease due to severe perinatal pathology with developmental delay, chronic cerebral circulatory failure or traumatic brain injury; age over 25 years and under 60 years; complete secondary or higher education; absence of neurometabolic therapy for 3 months before the study. Exclusion criteria were: psychotic disorders or suicidal intentions; uncorrectable visual or hearing impairment; serious neurological or somatic diseases; alcoholism or drug addiction; pregnancy; history of allergic reactions or hypersensitivity to cytoflavin.
All patients were divided into two groups - the main and control groups of 50 people in each. Patients in the main group received cytoflavin in addition to basic therapy.
Cytoflavin was prescribed twice a day, 2 tablets. The duration of therapy was 3-4 weeks. Patients in the control group received only basic therapy. Basic therapy included antidepressants, vascular drugs, and in some cases drugs with sedative and/or antipsychotic effects. All patients were consulted by psychologists and psychotherapists, took courses in hydro- and electrophysiotherapy, received massage of the collar area, and did physical therapy.
Tolerability of cytoflavin was assessed based on side effects in two groups of patients.
All patients underwent an EEG to monitor high-amplitude paroxysmal τ-activity in the central leads or the presence of epileptic brain activity.
The effect of cytoflavin on the symptoms of the disease was assessed by the dynamics of asthenia indicators, the results of cognitive tests, changes in the level of depression, anxiety, autonomic disorders and quality of life after the course of treatment in comparison with the condition of patients in the first days of hospital stay, depending on taking cytoflavin.
The severity of asthenia symptoms was assessed using the asthenic state questionnaire. The technique was developed by L.D. Malkova and adapted by T.G. Chertovaya on the basis of clinical and psychological observations and the MMPI questionnaire. The questionnaire contains 30 questions, the answers to which are ranged from 1 point (no, incorrect) to 4 points (absolutely true). An indicator of 51-74 points is interpreted as mild asthenia, 75-100 points - moderate asthenia, 101-120 points - severe asthenia.
The severity of depression and anxiety was assessed using the Hospital Depression and Anxiety Scale and the Beck Depression Inventory [9]. The Hospital Scale consists of 14 items, 7 of which assess symptoms of depression and 7 of which assess symptoms of anxiety. The Beck Inventory consists of 21 items assessing symptoms of depression.
Autonomic disorders were assessed using the Autonomic Disorders Scale [10]. The scale consists of 2 parts. The Objective Autonomic Disorders subscale consists of 13 items and is completed by the clinician. The subjective autonomic disorders subscale consists of 11 items and is completed by the patient.
Cognitive function was examined using the Montreal Cognitive Assessment Scale (MoCa) [11]. The scale consists of 12 tasks assessing attention and concentration, memory, visual-constructive skills, abstract thinking, and speech functions. The maximum number of points is 30.
Quality of life was assessed using the SF-36 questionnaire (36-item short form Health Survey) [1, 12]. The questionnaire contains 36 items, on the basis of which 8 subscales are formed: physical functioning, role limitations due to physical problems, physical pain, general health, energy, social functioning, role limitations due to emotional problems, mental health.
Statistical analysis of the obtained data was carried out using the SPSS17 software package. The dynamics of psychological and other indicators were assessed using the Repeated measures ANOVA test, in which the grouping factor was the presence or absence of cytoflavin therapy. Since in a previous study we found differences in the severity of the effect of cytoflavin in men and women [6], in this work we included gender in the analysis as a second grouping factor. If there were between-group differences in testing, baseline test performance was also included in the analysis as a covariate.
results
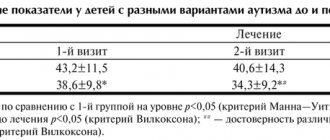
In the table
The characteristics of the patients are presented, including group average indicators on the scales studied.
The distribution of men and women, mean age and level of education did not differ between the groups of patients receiving cytoflavin and the control group.
The average group indicators of asthenia were: 80.3±2.6 and 82.3±3.8 points in the main and control groups, respectively. However, despite the small differences between the group average indicators, they were significant with less severity of asthenia in the main group. At the same time, the level of depression according to Beck and the severity of autonomic disorders according to a questionnaire filled out by a doctor were greater in the group of patients receiving cytoflavin. Indicators of depression and anxiety, identified using the Hospital Depression and Anxiety Scale, as well as the severity of subjective autonomic disorders did not differ in the study and control groups. The frequency of paroxysmal activity according to EEG examination was low in the examined population of patients with asthenia of organic nature. Thus, paroxysmal τ-activity upon admission was detected in 3 patients receiving cytoflavin and in 5 patients in the control group. During re-examination before discharge, paroxysmal τ-activity was detected in the same 8 patients. Epileptic activity was not detected in any case, either during the initial or re-examination.
Cytoflavin was well tolerated; 16 patients receiving cytoflavin and 15 patients in the control group noted moderate sedative effects of standard antidepressant therapy (drowsiness, mild lethargy, slight dizziness). No other complaints were identified in the group of patients receiving Cytoflavin. There were also no new cases of epileptic activity or paroxysmal high-amplitude activity on the EEG recorded after the course of treatment.
The effect of cytoflavin on the level of asthenia and cognitive functions
After an inpatient course of treatment, the level of asthenia decreased to 57.3±6.8 points in the main group and 58.4±6.8 points in the control group, while the positive dynamics of this indicator was highly reliable ( p
<0.001). At the same time, the magnitude of changes in the severity of asthenia symptoms in accordance with the indicators of the asthenic state questionnaire did not differ in the two groups, either with or without using the baseline level of asthenia as a covariate.
The results of the Montreal Cognitive Impairment Scale tests also significantly improved in both examined groups of patients ( p
<0.001).
However, no effect of the drug was detected in the general group of subjects ( p
= 0.224).
It is important to note that in 53 subjects the total score on the Montreal scale already during the initial examination reached the “ceiling” value of 27 to 30 points, i.e. any dynamics of this indicator during repeated examination was impossible. Accordingly, we re-analyzed the dynamics of the results of the cognitive tests of the Montreal scale depending on the drug intake in a group of 35 patients who completed these tests with a score of 21 to 26 points. A significant improvement in the results of performing cognitive tests before discharge compared to the first days of hospitalization was also found in this group of patients ( p
<0.001). It is important that patients receiving cytoflavin (11 patients) demonstrated a more pronounced improvement in the results of cognitive tests upon re-examination compared to the group of patients (24 people) receiving standard therapy (Fig. 1).
Figure 1. Dynamics of the total score on the Montreal Cognitive Impairment Scale depending on cytoflavin intake. Here and in Fig. 2-4: solid line – main group of patients, dotted line – control group. When excluding from the analysis patients who performed Montreal scale tests at a level of 26 points, this trend reached significance ( p
= 0.009).
Effect of cytoflavin on emotional disorders
In both groups of patients, a decrease in the level of depression on the Beck depression scale was recorded before discharge ( p
<0.001).
A more pronounced decrease in depression was found in the group of patients receiving cytoflavin compared to the control group ( p
= 0.004).
However, patients receiving the drug were significantly different from the control group in higher levels of depression during hospitalization ( p
= 0.011).
Thus, in 8 patients from the main group, depression exceeded 35 points on the Beck scale, while in the control group not a single patient had such a high score. In addition, in 4 patients characterized by very low depression scores on admission (3-6 points), dynamics was impossible. Accordingly, we re-analyzed the effect of cytoflavin on the severity of depression after excluding 8 patients with Beck scale scores of 40-47 (Fig. 2)
.
Figure 2. Dynamics of depression according to the Beck scale depending on cytoflavin intake. The trend toward a more pronounced decrease in depression in patients receiving Cytoflavin compared with the control group remained significant in repeated analysis ( p
= 0.045). It should be noted that the positive effect of cytoflavin on the dynamics of depression was more pronounced in men, but gender differences in this indicator did not reach statistical significance.
Depression and anxiety, as measured by the Hospital Depression and Anxiety Scale, also decreased significantly before discharge in both groups of patients ( p
<0.001), however, the decrease in anxiety level was significantly greater in the group that did not receive cytoflavin (
p
= 0.008) compared with patients treated with cytoflavin
(Fig. 3)
.
Figure 3. Dynamics of depression and anxiety according to the Hospital Depression and Anxiety Scale depending on cytoflavin intake. The dynamics of anxiety depending on the intake of cytoflavin did not differ between men and women; in other words, a more pronounced decrease in anxiety in patients who did not receive cytoflavin was observed both in the group of men ( p
= 0.043) and in the group of women (
p
= 0.079).
Effect of cytoflavin on autonomic disorders
The severity of objective and subjective autonomic disorders significantly decreased in the examined group of patients with emotionally labile disorder after an inpatient course of treatment compared to the period before treatment ( p
<0.001).
Patients treated with cytoflavin showed a tendency towards a more pronounced normalization of autonomic functions according to the corresponding questionnaire compared to patients not treated with cytoflavin ( p
= 0.076). This trend was expressed to the same extent in both the subgroup of men and the subgroup of women.
As noted above, autonomic disorders, as examined by a physician, were significantly more pronounced in the group of patients receiving Cytoflavin. However, as can be seen in Fig. 4
, there were no intergroup differences in the dynamics of objective symptoms of autonomic dysfunction depending on the intake of cytoflavin (
p
= 0.24).
Figure 4. Dynamics of autonomic disorders according to the questionnaire by A.M. Vein depending on the intake of cytoflavin.
Effect of cytoflavin on quality of life
Group mean scores on all 8 SF-36 subscales improved at re-examination compared with examination at admission ( p
<0.001), but these changes did not depend on cytoflavin intake.
Cytoflavin
Metabolic drug. Pharmacological effects are due to the complex action of the components that make up the drug Cytoflavin®.
Succinic acid is an endogenous intracellular metabolite of the Krebs cycle, which performs a universal energy-synthesizing function in the cells of the body. With the participation of the coenzyme flavin adenine dinucleotide (FAD), succinic acid is quickly transformed by the mitochondrial enzyme succinate dehydrogenase into fumaric acid and then into other metabolites of the tricarboxylic acid cycle. Stimulates aerobic glycolysis and ATP synthesis in cells. The end product of succinic acid metabolism in the Krebs cycle is carbon dioxide and water. Succinic acid improves tissue respiration by activating electron transport in mitochondria.
Inosine is a purine derivative, a precursor to ATP. It has the ability to activate a number of Krebs cycle enzymes, stimulating the synthesis of key nucleotide enzymes - FAD and NAD.
Nicotinamide (vitamin PP), nicotinic acid amide. Nicotinamide in cells, through a cascade of biochemical reactions, is transformed into the form of nicotinamide adenine nucleotide (NAD) and its phosphate (NADP), activating nicotinamide-dependent enzymes of the Krebs cycle, necessary for cellular respiration and stimulation of ATP synthesis.
Riboflavin (vitamin B2) is a flavin coenzyme (FAD) that activates succinate dehydrogenase and other redox reactions of the Krebs cycle.
Thus, all components of the drug Cytoflavin® are natural metabolites of the body and stimulate tissue respiration. Metabolic energy correction, antihypoxic and antioxidant activity of the drug, which determine the pharmacological properties and therapeutic effectiveness of the components, is due to the complementary action of succinic acid, inosine, nicotinamide and riboflavin.
Pharmacokinetics
Cytoflavin® has high bioavailability.
When taken orally, succinic acid is absorbed from the gastrointestinal tract, enters the blood and tissues, participating in energy metabolism reactions, and completely decomposes to the final metabolic products (carbon dioxide and water) after 30 minutes.
Inosine is well absorbed from the gastrointestinal tract. Tmax in the blood is 5 hours, the average retention time in the blood is 5.5 hours, Vd at steady state is about 20 l. Inosine is metabolized in the liver to form inosine monophosphate, followed by its oxidation to uric acid. A small amount is excreted by the kidneys.
Nicotinamide is quickly distributed in all tissues (Vd at steady state is about 500 l). Tmax in the blood is 2 hours, the average retention time in the blood is 4.5 hours. Metabolized in the liver to form N-methylnicotinamide. Excreted by the kidneys. Nicotinamide penetrates the placental barrier. Passes into breast milk.
Riboflavin is quickly absorbed from the gastrointestinal tract, distributed unevenly (the largest amount in the myocardium, liver, kidneys), and is transformed into flavin adenine mononucleotide (FMN) and FAD in mitochondria. Penetrates through the placental barrier. Excreted in breast milk. It is excreted by the kidneys, mainly in the form of metabolites.
Discussion
The results of the study indicate that cytoflavin at a dose of 4 tablets per day (in 2 doses) has a positive effect on cognitive functions in patients with organic brain damage. Data from a previous study [6] regarding the positive effect of cytoflavin on depressive symptoms in patients with severe asthenia were confirmed. At the same time, in contrast to a multicenter study that included patients with cerebrovascular disease [4], we did not detect an additional effect of cytoflavin on the overall positive dynamics of asthenic symptoms in patients with emotionally labile disorder. We observed a pronounced regression of asthenia symptoms regardless of cytoflavin intake. It should be noted that the average age of the examined patients was significantly lower compared to the specified multicenter study [6], which included patients with cerebrovascular disease and demonstrated a more pronounced reduction in asthenia during treatment with cytoflavin. It can be assumed that the effectiveness of cytoflavin manifests itself mainly in patients with reduced neurotrophic resources. Indirect confirmation of this hypothesis is a more pronounced improvement in cognitive status while taking cytoflavin in patients with cognitive impairment compared to the control group in our study.
In patients treated with cytoflavin, a significantly more pronounced decrease in the Beck depression score and normalization of autonomic regulation were found compared to the control group. Interestingly, in our previous study involving patients with organic depression, a similar effect of cytoflavin was observed only in a subgroup of women. In the present study, the effect of cytoflavin was more pronounced in the subgroup of men with emotional labile disorder compared to the subgroup of women. Our data are consistent with previous experimental and clinical studies demonstrating the antidepressant effect of nootropics [13–15]. Numerous neuroimaging and experimental studies have revealed a deficit in neurotrophic processes in patients with chronic depression, leading to hypotrophic changes in the frontal cortex and other brain structures in such patients [16-18]. Thus, the effectiveness of prescribing cytoflavin as an additional method of treating depression seems pathogenetically justified.
It is well known from clinical practice that most nootropic drugs have a stimulating effect on the functions of the central nervous system. It is likely that the stimulating effect of cytoflavin was the reason for less regression of anxiety symptoms in the group of patients receiving the drug compared to the control group. Accordingly, the possibilities and limitations of nootropic therapy in patients with anxiety disorders require further research.
Thus, the data from the present observational study indicate that cytoflavin is well tolerated by patients with organic emotionally labile (asthenic) disorder and helps to normalize cognitive functions, mood and autonomic regulation in such patients. The effectiveness of cytoflavin as a treatment for asthenia in young patients requires further research.
Increasing the efficiency of medical care for children of different ages, including the youngest, is one of the most pressing medical and social tasks. Hypoxic-ischemic and infectious lesions of the central nervous system require special attention in the field of neonatal and pediatric pathology. Problems of perinatal pathology are relevant both due to their high frequency among diseases of newborns and children of the first year of life (according to a number of authors, from 60% to 80% with a tendency to further increase), and due to the presence of unresolved issues of diagnosis and therapy. To this it should be added that perinatal lesions of the central nervous system contribute to the development of early psychoneurological disability (early disability among children occurs in 60-70% of cases) [1-4].
Hypoxic-ischemic lesions of the central nervous system
One of the most significant pathogenetic factors of perinatal damage to the central nervous system of newborns is hypoxia. Fetal hypoxia, which often develops as a result of pathological pregnancy, contributes to the birth of a premature baby with impaired respiratory function. Premature, and especially very premature, children are characterized by pronounced physiological abnormalities. These include hypercatecholaminemia, carnitine deficiency, loose type of coronary arteries, which in turn leads to significant inhibition of the synthesis of macroergs in the mitochondria of cardiomyocytes and the predominance of the carbohydrate component of metabolism, resulting in a cascade of pathobiochemical and pathobiological disorders. All this leads to the formation of respiratory acidosis with the secondary development of tissue hypoxia and metabolic acidosis. Hypercatecholaminemia promotes stimulation of the vasomotor center and cardiac activity, increased arteriolar tone and hypertension, further leading to arrhythmia, decreased sensitivity of adrenal receptors and ultimately to severe heart failure. As a result, extremely premature babies lose the ability to adequately respond to postpartum changes in blood circulation, which in turn leads to pronounced functional stress in the cardiovascular system.
As is known, the blood circulation of the fetus has features, which consist primarily in the fact that the lungs do not carry out the respiratory function, and therefore the pulmonary circulation does not function, while oxygen comes from the placenta through the umbilical vein and passes through the inferior vena cava into the right atrium. In order for oxygenated blood to enter the systemic circulation, the fetus has major fetal ducts: the duct of Arantius between the umbilical vein and the inferior vena cava, connecting the right and left atria, and the ductus arteriosus between the aorta and the pulmonary trunk. After birth, they should normally close, which often does not happen in very premature babies.
The consequence of metabolic acidosis is the worsening of circulatory disorders in all tissues of the body, including circulatory disorders of brain tissue. The emerging instability of autoregulation of cerebral blood flow due to the morphofunctional immaturity of its main components is accompanied by a high frequency of ischemic and hemorrhagic brain lesions in newborns, which in turn lead to various deviations in neuropsychic development and early childhood disability of varying severity.
According to a number of authors [4–7], 85% of all perinatal lesions of the central nervous system in premature infants appear during the first week of their life.
Analysis of the pathophysiological mechanisms of post-hypoxic brain damage in premature infants led to an understanding of the need for early pharmacological correction. Such correction is intended to prevent or at least significantly reduce the severity of brain damage, increase therapeutic and rehabilitation potential, and improve the prognosis of the disease [4, 8–10].
When considering the problem of early pharmacological correction, it should be borne in mind that there are divergent views on the duration of the so-called “therapeutic window”, within which pharmacological neurocytoprotective correction for hypoxic and ischemic disorders can be considered effective. In the literature [7, 10], one can find the following range of this “therapeutic window”: from 2 to 48 hours after the development of hypoxic-ischemic disorders. This “therapeutic window” framework is associated with the postulate that the most significant cellular losses of nervous tissue develop 2, 6 and 48 hours after birth due to the oxidative stress that accompanies brain reperfusion, when the phase of perfusion deficiency passes into the phase of reperfusion with highly oxygenated blood, which in turn, is accompanied by excess production of highly reactive free radicals or products that generate them [11]. In such a situation, in the first hours and days of life of children who have suffered ante- and intranatal hypoxia and ischemia, a pronounced imbalance in the regulation and distribution of cerebral circulation occurs, which contributes, especially in premature infants, to the frequent development of ischemic and hemorrhagic disorders of brain tissue in the early neonatal period [4, 12].
The most promising areas for drug correction of hypoxic and ischemic lesions of brain structures in both adults and children are currently considered [7, 13] the use of antihypoxants that regulate intracellular metabolism, which include natural metabolites, which at the same time activate the production of macroergs under conditions of oxygen deficiency and have antioxidant activity [14].
One can confidently include the drug Cytoflavin (NTFF POLYSAN LLC, St. Petersburg) among the medicinal products that meet these requirements. This drug is one of the few neurocytoprotectors whose effectiveness and safety have been assessed from the standpoint of evidence-based medicine.
Cytoflavin has a neurocytoprotective, antihypoxic, antioxidant effect, positively influencing the processes of energy formation in the cell, reducing the production of free radicals and restoring the activity of antioxidant enzymes [15]. Thus, in biopharmaceutical studies [16, 17], it was found that cytoflavin improves oxidative metabolism under ischemic conditions, preventing a sharp decrease in ATP levels, stimulates the activity of adenylate cyclase, which allows anaerobic metabolism of glucose without the formation of lactate. This drug also stimulates reparative processes and limits the area of ischemic damage [18]. In addition, cytoflavin improves blood oxygenation and activates cellular respiration, as well as ion transport and protein synthesis. The drug, preserving the ribosome apparatus, activates the intracellular synthesis of nucleic acids, enzymatic processes of the Krebs cycle, promotes the utilization of glucose and the synthesis and intracellular accumulation of ATP and other macroergs [19]. It is also important that when treating patients with hypoxia and cerebral ischemia, cytoflavin promotes the resynthesis of γ-aminobutyric acid in neurons [20, 21].
Cytoflavin is a harmonious combination of succinic acid, riboxin, nicotinamide (vitamin PP) and riboflavin mononucleotide (vitamin B2). Succinic acid is a central substrate of the Krebs cycle and can be included in this cycle in ionized form, crossing cellular and mitochondrial membranes. Riboxin helps inhibit the enzyme xanthan oxidase and suppress free radical processes, thereby providing an antioxidant effect. Riboflavin, which is a profactor of the main coenzymes of the respiratory chain flavin mononucleotide and flavin adenine dinucleotide, has a direct antihypoxic effect, which is associated with the activation of flavin reductases and restoration of ATP levels, as well as antioxidant properties due to the reduction of glutathione. Nicotinamide activates the antioxidant systems of ubiquinone oxyreductases, which have a protective effect on cell membranes.
Thus, all components of cytoflavin are inducers of cellular metabolic pathways and activators of energy production processes, which in turn promotes the utilization of free oxygen and, accordingly, reduces the level of peroxide processes. An important advantage of this drug is the presence in its composition of methylglucamine, a transmembrane transporter that transfers compounds associated with it through cell membranes into the internal structures of the cell, where all the main pathochemical disorders occur during hypoxia and ischemia.
It should be noted that thyroid hormones play an important role in the development and maturation of child brain structures. Neonatal transient hypothyroidism has an adverse effect on the development of children (physical, speech, mental), as well as on the level of their social adaptation [22, 23]. In turn, the main pathogenetic mechanisms for the development of perinatal lesions of both the nervous system and the thyroid gland are hypoxia and, accordingly, insufficient tissue perfusion, which contributes to an increase in energy deficiency and disruption of intracellular homeostasis. Considering the disorders described above, it becomes clear the importance of using antihypoxants with membrane-stabilizing effects for perinatal lesions of the central nervous system and thyroid gland [7, 10], which may include cytoflavin. Its effectiveness has been established in a number of studies.
In the study by V.I. Strukova et al. [24] analyzed the effectiveness of basic therapy and therapy that included cytoflavin in the treatment regimen for children aged 7 days to 1 month, born at a gestational age of 37 to 42 weeks and suffering from cerebral ischemia and transient hypothyroidism. In the group of patients receiving Cytoflavin, on days 5-6 of therapy there was a statistically significant decrease in the severity of cerebral tissue ischemia compared to the group of patients who did not receive Cytoflavin. A statistically significant faster decrease in serum TSH levels was also found in patients treated with Cytoflavin. The results of the study also showed the effectiveness of cytoflavin in the treatment of children with extremely low and very low body weight with post-hypoxic myocardial damage and significant metabolic disorders. They showed normalization of acid-base balance within 24 hours from the start of treatment without increasing the risk of developing intraventricular hemorrhages. Analyzing the average duration of symptoms of perinatal central nervous system damage, the study authors came to the conclusion that their duration was significantly shorter (1.5-2 times) in the group of patients receiving cytoflavin. These symptoms included impaired motor activity, vegetative-visceral dysfunction, sleep disturbance, decreased appetite and impaired weight gain.
The results of the study conducted by S.O. were interesting and useful from a practical point of view. Rogatkin et al. [25], who studied the effectiveness of cytoflavin in post-hypoxic lesions of the central nervous system in premature newborns. The cerebroprotective effect of this drug was confirmed. Thus, among newborns who received cytoflavin, compared with those who did not receive this drug, a statistically significant level of reduction in the incidence and severity of ischemic and hemorrhagic lesions of the central nervous system was revealed. This corresponded to a lower level of concentration of neurospecific proteins in the blood, which is primarily associated with a more rapid normalization of acid-base balance, partial pressure of oxygen and carbon dioxide, as well as the elimination of lactic acidosis.
The beneficial effect of cytoflavin on cerebral ischemia in premature newborns was also established by A.G. Antonov et al. [26]. They found that with the use of cytoflavin, more rapid and complete psychomotor development of children occurred during the first year of life.
It is important to note that, according to the results of these studies, cytoflavin was well tolerated by children and they had no side effects.
Thus, data from a number of studies convincingly demonstrate the neuro-(cerebro-)protective effect of cytoflavin in the treatment of children with hypoxic and ischemic lesions of the central nervous system, as well as the cardio- and thyroid-protective effect of this drug in the category of patients under discussion, which certainly provides grounds for its use for the treatment of children in the first months of life with neurometabolic disorders as part of the complex treatment of perinatal CNS lesions.
Infectious lesions of the central nervous system
It is known that infectious lesions of the central nervous system occupy one of the leading places among all infectious diseases. They are characterized by a severe course and a high mortality rate (8-36%). The incidence of residual damage to the nervous system is 26–75% [27]. Signs and manifestations of persistent organic damage to the central nervous system in the residual period are observed in almost 50% of children who have suffered an infectious lesion of the nervous system [27], and therefore, increasing the effectiveness of treatment for children with infectious diseases, and primarily with bacterial purulent meningitis and viral encephalitis, is one of the most pressing medical and social problems.
One of the main manifestations of infectious processes in the central nervous system is damage to the vascular bed and disruption of the hemostatic system. Vascular lesions that develop against the background of infectious diseases include vascular occlusion and stenosis, the development of which, in turn, is associated with a violation of the rheological properties of the blood. In case of infectious lesions of the central nervous system, the most common is generalized vascular damage, involving the cerebral vessels in the pathological process. Their damage is characterized by damage to the endothelium, disruption of neurovascular regulation and coagulation, which dictates the need for timely use of various vasoactive and neurocytoprotective drugs.
In the treatment of infectious pathology in pediatrics, preference is given to complex drugs [27] that have a multimodal and multifactorial effect, which is the cytoflavin discussed in this article. It has been the subject of study in a number of works.
N.V. Skripchenko and E.S. Egorova [27] assessed the effectiveness of therapy in patients aged 1 month to 18 years who had suffered bacterial purulent meningitis and viral encephalitis. All patients received standard therapy (antibacterial or antiviral drugs and dehydration agents) and were divided into two groups - those who received and did not receive cytoflavin during basic therapy. The authors concluded that the use of cytoflavin during the acute period of bacterial purulent meningitis and viral encephalitis helps to reduce the duration of the main clinical symptoms of the disease. The authors associated these changes with the multimodal and multifactorial action of this drug, namely with the ability of cytoflavin to favorably influence both the improvement of blood circulation in the brain and the stimulation and activation of neurometabolic processes. In addition, the results of the study in question indicated normalization of clinical blood parameters under the influence of cytoflavin and the anti-inflammatory effect of this drug. It has been suggested [18, 28] that this is due to activation of metabolic processes and inhibition of the synthesis of proinflammatory cytokines. In addition, the use of cytoflavin contributed to the rapid normalization of circulating endothelial cells and D-dimer. A beneficial effect of cytoflavin on the rheological properties of blood was also noted.
Thus, the use of the drug cytoflavin in children as pathogenetic therapy in the acute stage of bacterial purulent meningitis and viral encephalitis is effective. In addition, good tolerability and safety of cytoflavin have been established. Cytoflavin not only has anti-inflammatory and neuroprotective effects, but also improves the rheological properties of blood. Thanks to the improvement of the treatment of pediatric patients who have suffered bacterial purulent meningitis and viral encephalitis, with the help of Cytoflavin, a decrease in the average hospital day was achieved, as well as a significant reduction in the risk of residual neurological deficit - from 35 to 15%.
The above increases the possibility of treating CNS lesions of hypoxic-ischemic and infectious etiology. It should be emphasized that the effectiveness of this therapy depends on a comprehensive combined and multifactorial approach to its implementation. From the presented review of the literature, it is clear that protection is currently possible with the help of timely administration of the energy-correcting antioxidant and antihypoxant cytoflavin, the use of which in the treatment of this category of patients is justified from the point of view of effectiveness and safety and can be recommended for use in practical neonatology and pediatrics.
The authors declare no conflict of interest.
*e-mail; https://orcid.org/0000-0002-1004-2162