General information
Neutropenia or agranulocytosis is a condition characterized by a decrease in the number of neutrophil granulocytes in the blood. With severe neutropenia in a person, the likelihood of developing fungal and bacterial infections, as well as the severity of their course, increases. With agranulocytosis, the level of leukocytes decreases to less than 1•10 per 9/L due to a decrease in the number of granulocytes (less than 0.75•10 per 9/L) and monocytes .
There are several forms of the disease depending on the pathogenesis. Speaking about neutropenia - what it is, it should be noted that this condition was first described in 1922. Currently, due to the active use of cytostatic treatment and various medications, the frequency of manifestation of this syndrome has increased.
To diagnose this condition, it is necessary to determine the number of leukocytes in the blood and the leukocyte formula. However, during the diagnostic process, it is very important to find out the cause of this manifestation in order to provide adequate treatment.
Why this condition can occur, and what treatment methods are used depending on the cause of neutropenia, will be discussed in this article.
How to prevent infection
Below are some ways to prevent infection:
- Do not accept guests who have a cold or who have recently had an infection.
- Wear a mask when visiting public places, using public transport or being in crowded places. It will help protect you from a cold or respiratory infection.
- Do not treat your teeth unless absolutely necessary. Consult your healthcare provider before undergoing any procedure.
- Ask your healthcare provider when you can again: use tampons;
- use dental floss;
- use suppositories (solid soluble medications);
- give enemas;
- have sex.
to come back to the beginning
Pathogenesis
The pathogenesis of different forms of agranulocytosis is different, and for many it has not yet been studied well enough. In autoimmune forms of the disease, the death of granulocytes occurs due to the influence of autoantibodies. In hapten agranulocytosis, the mechanism of the individual reaction of the body has not been fully studied. When haptens are administered after the first occurrence of hapten agranulocytosis, this condition will recur again.
Neutrophils
Granulocytes (neutrophils) provide protection to the body from attacks by bacteria and fungal infections. With the development of neutropenia, the response to such infections is ineffective.
The limit of the lower norm of neutrophils is 1500/μl in representatives of the Caucasian race; in people of the Negroid race this figure is slightly lower - about 1200/μl. The number of these cells is unstable - depending on the influence of various factors, it can change over a short period of time.
When the number of neutrophils decreases to <500/μl, an infectious process can develop due to the influence of endogenous microflora (in the intestines, in the mouth). If the number of these cells is reduced to <200/μl, the inflammatory response may be suppressed and typical signs of such a process (leukocytes in the urine, in the area of infection, leukocytosis) may not be observed.
In acute neutropenia , especially when combined with other factors (oncological disease, etc.), the function of the immune system is significantly impaired, which can subsequently lead to fulminant fatal infections. The risk of developing infectious processes is also affected by the integrity of the skin, mucous membranes, blood supply and tissue nutrition. People with severe neutropenia most often develop the following infectious diseases: pneumonia , furunculosis , septicemia .
The presence of places where vascular catheters were placed and injections were performed additionally increases the risk of developing skin infections. The most common pathogens are Staphylococcus aureus, coagulase-negative staphylococci, but other bacteria can also provoke the pathological process. People with agranulocytosis often develop other diseases: colitis , paraproctitis , stomatitis , otitis , sinusitis , etc. Those patients who have prolonged neutropenia after chemotherapy , stem cell transplantation, high doses of corticosteroid drugs are prone to developing fungal infections.
Leukopenia (neutropenia)
Neutrophils are white blood cells that help fight infection. Neutropenia is a decrease in the level of neutrophils.
This complication, as a rule, occurs 7-14 days after the administration of chemotherapy and, in good cases, resolves itself by 21 days. When the neutrophil count falls below a certain level, bacterial complications can develop.
Why is neutropenia dangerous?
- development of bacterial complications;
- the need to postpone the next course of chemotherapy;
- the need to reduce the dose of chemotherapy drugs, which negatively affects the results of treatment;
- Febrile neutropenia without appropriate treatment can cause the development of life-threatening conditions, including death.
The lower limit of normal for blood neutrophil levels is approximately 2000/mm3. A neutrophil level below this is considered neutropenia, which is classified according to severity.
What are the severity levels of neutropenia?
- light (1000–1500/µl);
- moderate (500–1000 µl);
- severe (<500/µl).
Main symptoms of neutropenia
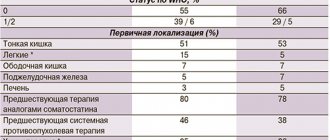
| DEGREE OF SEVERITY | MANIFESTATIONS |
| EASY | Usually asymptomatic, episodes of viral or bacterial infection are possible, which respond well to standard therapy. |
| AVERAGE | Frequent relapses of purulent infection. The weakening of the body's defenses leads to frequent acute respiratory viral infections, sore throats and other acute diseases of a viral or bacterial nature. |
| SEVERE (agranulocytosis) | It is characterized by ulcerative-necrotic processes, severe viral, fungal or bacterial infections, and symptoms of intoxication. The risk of sepsis and mortality increases due to inadequately selected therapy. |
The most serious complication of neutropenia is febrile neutropenia. This is a combination of fever with a decrease in the number of neutrophils; at least a two-fold increase in body temperature >38.0°C per day, or a single increase in temperature >38.3°C with a neutrophil content <0.5×109/l.
Main causes of neutropenia
- Some drugs can cause bone marrow problems, reducing the production of neutrophils.
- Some forms of tumor affect the bone marrow directly (including leukemia or lymphoma), and can crowd out normal bone marrow cells.
- Radiation therapy can also affect the bone marrow, especially if it irradiates large areas of the body or bones in the pelvis, legs, chest, or abdomen.
What main treatment regimens lead to the development of neutropenia?
Chemotherapy regimens with a high risk of febrile neutropenia (more than 20%):
- Breast cancer: oxorubicin, cyclophosphamide/paclitaxel once every 2 weeks
- Bladder cancer: methotrexate, vinblastine, doxorubicin, cisplatin, paclitaxel, cisplatin
- Cervical cancer: paclitaxel, cisplatin
- Non-small cell lung cancer: docetaxel, carboplatin
- Small cell lung cancer: cyclophosphamide, doxorubicin, etoposide
- Gastric cancer: docetaxel, fluorouracil, cisplatin
- Ovarian cancer: topotecan 1.5 mg/m2 (days 1–5)
- Testicular tumors: etoposide, ifosfamide (+ mesna), cisplatin
- Head and neck tumors: paclitaxel, ifosfamide, cisplatin
- Sarcomas: doxorubicin, ifosfamide, dacarbazine
Symptoms of febrile neutropenia
- Against the background of a sharp drop in the absolute number of neutrophils (this indicator is less than 500) or granulocytes (this indicator is less than 1000), there is a sharp increase in the patient’s body temperature to 38 °C or more.
- A general drop in the tone of the whole body, up to severe asthenic syndrome.
- Minor tremor (involuntary small trembling of body parts).
- Increased heart rate.
- Reduced blood pressure. This manifestation can lead to shock or cardiovascular collapse.
- Possible heavy sweating.
Are there factors that increase the risk of developing febrile neutropenia?
- age over 65 years;
- female;
- antimicrobial prophylaxis was not carried out;
- late stage of the disease;
- there have already been episodes of FN;
- there are severe concomitant diseases;
- severe general condition of the patient;
- there are open wounds or infections;
- malnutrition;
- chemo-radiation therapy;
- damage by a bone marrow tumor;
- hemoglobin below 120 g/dl
The occurrence of a symptom complex of febrile neutropenia is a direct basis for a number of diagnostic procedures and immediate (within 1 hour) prescription of antibacterial therapy. See a doctor immediately!
- temperature 38 degrees and above;
- chills, sweat;
- cough or shortness of breath;
- sore throat or mouth ulcers;
- redness or swelling of the skin;
- loose stools;
- difficulty urinating - increased frequency or burning sensation;
- vaginal discharge or itching;
- flu-like symptoms;
- soreness at the insertion site of a dropper needle, syringe or other device through which medications enter the body.
Treatment and prevention of neutropenia
To prevent the development of febrile neutropenia (FN) and its treatment, colony-stimulating factors (CSF) are prescribed. Recommendations for prescribing CSF:
- When FN develops, it is mandatory to prescribe systemic antibiotics (intravenously) of a wide spectrum (in patients with a low risk of severe infections, tablets are possible). The administration of G-CSF does not replace the administration of systemic antibiotics.
- Before each course of chemotherapy, individual factors that may increase the risk of FN should be assessed (see above).
- The use of CSF should be prescribed when there is an increased risk of FN and/or when using certain chemotherapy regimens (see above).
- Risk factors are assessed immediately before starting chemotherapy.
- The use of targeted drugs (cetuximab, bevacizumab, retuximab) in combination with cytostatics increases the incidence of FN! KSF are prescribed!
- Prophylactic use of CSF is recommended if the risk of functional failure during chemotherapy is ≥ 20%. If the likelihood of FN is lower, individual risk factors are assessed.
- If chemotherapy is palliative in nature, the choice of a less myelosuppressive combination or a change in dose/regime of drugs to prevent the risk of developing FN should be discussed.
- Mandatory administration of CSF during intensive chemotherapy regimens.
- Treatment with CSF drugs should be carried out in the presence of febrile neutropenia and ineffectiveness of antibiotics. This may reduce the likelihood of developing infectious complications and death from them in patients with an extremely high risk of life-threatening infections associated with febrile neutropenia, such as sepsis or septic shock.
The most effective drugs currently are filgrastim, lenograstim and pegfilgrastim.
How to protect yourself with low white blood cells?
- Wash your hands often: for at least 10 seconds, before and after using the toilet, and before eating.
- Take a warm shower every day; Wipe yourself dry.
- Use moisturizing skin creams.
- Maintain good oral hygiene; The toothbrush should be soft.
- Prevent constipation: try to have bowel movements every day.
- After defecation, clean the area around the anus well. Women should wipe from the front to the anus.
- In case of acute neutropenia, sex should be avoided. It is recommended to use water-soluble lubricants during sex and maintain personal hygiene after it.
- To prevent injury, use gloves when cleaning the house and working in the garden.
- Avoid sunburn.
- Be sure to tell your doctor that your white blood cells are low.
What is best to avoid if you have neutropenia?
- crowded places or public places;
- any vaccinations without the permission of the oncologist;
- contacts with people who have recently received a live vaccine;
- contact with pet feces or material on which they urinate/defecate;
- carrying out dental procedures without the permission of an oncologist;
- eating raw fish or meat that has not undergone sufficient culinary processing; visiting buffet restaurants;
- manicure, pedicure.
There is no single diet that can raise white blood cell levels.
You should not rely on folk remedies.
General dietary recommendations for neutropenia
- It is recommended to check the expiration dates of products and avoid expired ones.
- It is recommended to discard cans that are swollen or damaged.
- It is not recommended to store thawed food.
- It is recommended to keep hot foods hot and cold foods cold.
- It is recommended to avoid old, crushed, or damaged fruits and vegetables.
- It is recommended that meat, poultry and fish be thoroughly cooked.
- It is recommended to thoroughly wash fruits and vegetables.
- It is not recommended to eat raw eggs and fish.
Nutrition for neutropenia
The list was compiled based on the recommendations of the American Association of Hematologists, adapted for the Russian Federation.
| PRODUCTS | ALLOWED | FORBIDDEN |
| DAIRY | Pasteurized milk, yogurt made from pasteurized milk, pasteurized non-dairy cream products, packaged ice cream, frozen yogurt, sorbet, frozen desserts without nuts and raisins, cottage cheese, cheddar, mozzarella, parmesan, Swiss. | Unpasteurized dairy products, ice cream, frozen yogurt from the machine, soft cheeses: sharp cheddar, camembert, feta, gorgonzola, goat's milk, Roquefort, blue cheese (unless well prepared), any cheese containing vegetables, herbs or chili peppers , peppers (unless well prepared), sliced cheese, cold appetizers. |
| MEAT PRODUCTS, FISH, SEAFOOD | Well-cooked beef, pork, lamb, fish, poultry, homemade meat and seafood salads, cooked, processed, smoked meats: bacon, hot dogs, sausage. | Undercooked meat, beef, pork, lamb, fish, poultry, bone-in meat, store-bought salads, chilled fish products, raw meat. |
| EGGS | Hard-boiled. | Raw or undercooked. |
| SOUPS | Freshly prepared or chilled homemade soup. | Cold vegetarian or fruit soups. |
| FRUITS | Oranges, grapefruits, tangerines, bananas, melons, cooked, frozen or canned fruits, pasteurized fruit juices, canned or vacuum-packed roasted nuts. | Any unlisted fruits, any freshly squeezed unpasteurized juices, kvass, raw dried fruits. |
| POTATOES AND SIDE DISHES | Any cooked potatoes, noodles, rice, pasta. | Store-bought ready-to-eat French fries and baked potatoes. |
| FLOUR PRODUCTS | Packaged bread, muffins, cookies. | Cookies, pies, cakes that require refrigeration, such as custard, etc., unpackaged bread, muffins, biscuits. |
| Sauces, seasonings, dressings | Ready-made mayonnaise and salad dressings. | Salad dressings made from mixtures containing herbs/spices. |
| BEVERAGES | Alcoholic drinks (after consultation with a doctor), pasteurized fruit juices, boiled water. | Unpasteurized fruit juices, bottled water, kvass, home-brewed beer. |
| OTHER | Herbal nutritional supplements, brewer's yeast. |
Rehabilitation for neutropenia
Performing a complex of exercise therapy including aerobic exercise during chemotherapy reduces the duration of leukopenia.
https://rassc.org/ru/oslozhneniya/nejtropeniya/37-neutropeniaincancer-patients-risk-factors-and-management https://rassc.org/ru/oslozhneniya/nejtropeniya/38-koloniestimuliruyushchie-faktory-v-onkologii https://rassc.org/ru/oslozhneniya/nejtropeniya/39-prevention-of-febrile-neutropenia https://rosoncoweb.ru/calculators/febrile_neutropenia/ https://www.cancer.net/coping-with-cancer /physical-emotional-and-social-effects-cancer/managing-physical-side-effects/neutropenia https://www.cdc.gov/cancer/preventinfections/pdf/neutropenia.pdf
Classification
Depending on the severity of neutropenia, the following forms of this condition are distinguished:
- mild (neutrophil count - 1000–1500/μl);
- moderate (500–1000 µl);
- severe (less than 500/μl).
Depending on the characteristics of the process, the following forms are distinguished:
- Acute – develops quickly, over several hours or days. It results from the very rapid destruction or consumption of neutrophils.
- Chronic – develops over several months or years. As a rule, it develops due to a decrease in the production of neutrophils and excessive splenic sequestration.
Depending on the origin, the following forms of neutropenia are distinguished:
- Primary – associated with an internal lack of myeloid cells in the bone marrow.
- Secondary – associated with the influence of external factors.
According to the pathogenetic factor, the following forms of this condition are distinguished:
- Myelotoxic agranulocytosis - develops due to exposure to ionizing radiation and the influence of benzene vapor. Also, myelotoxic agranulocytosis can be a consequence of the use of cytotoxic agents.
- Immune agranulocytosis is a consequence of the influence of autoantibodies and antibodies to granulocytes after taking hapten drugs. Immune agranulocytosis can be observed with systemic lupus erythematosus , etc.
- Idiopathic form - has an unknown etiology.
Depending on the characteristics of the condition, the following forms are distinguished:
- Absolute neutropenia is a decrease in the absolute number of neutrophils in the blood. Absolute neutropenia is characteristic of a number of conditions and diseases: acute and chronic viral, bacterial and fungal diseases, autoimmune diseases, acute leukemia , lymphoma , etc.
- Relative neutropenia is a decrease in the specific gravity of neutrophils in the blood against the background of a normal or increased number of these cells.
Treatment
There is no specific treatment regimen for neutropenia: the disease has a varied course and causes. The intensity of therapy will depend on the patient: his condition, age, degree of damage and spread of the inflammatory process. Mild forms of neutropenia do not require any treatment. Exacerbations of infections are treated in the same way as in all patients.
Patients with severe neutropenia need to be under constant medical supervision - they are admitted to the hospital. Antiviral, antibacterial, antifungal drugs are prescribed with increased doses. When choosing a medicine, it is necessary to analyze the sensitivity of the microflora to the active substances. Until the results are obtained, the patient is given intravenous broad-spectrum antibiotics. If his condition has not improved after 3 days of drug therapy, increase the dose of the antibiotic or change the drug.
Patients with neutropenia whose disease developed during chemotherapy or radiation exposure are advised to take antibiotics until the number of neutrophils reaches 500 mg/μl of blood. If a fungal one joins the infectious process, it is necessary to take fungicides. To minimize the risk of bacterial infection, the patient is prescribed trimethoprim sulfamethoxazole. Colony-stimulating factors are increasingly being used to treat neutropenia. To maintain immunity, it is necessary to take glucocorticosteroids and vitamin complexes.
If neutropenia causes destruction of the spleen, surgical removal is indicated. However, surgery is strictly contraindicated for septic complications and severe forms of pathology. In the most advanced cases, a bone marrow transplant may be required.
Causes
Granulocytopenia can develop due to a number of reasons, which depend on the type of disease.
- Myelotoxic agranulocytosis develops against the background of suppression of the production of myelopoiesis precursor cells in the bone marrow. It can develop as a result of exposure to cytostatic drugs, ionizing radiation on the body, and also develop as a result of taking other medications ( Streptomycin , Levomycetin , Gentamicin , Colchicine , Penicillin , etc.).
- Immune agranulocytosis develops due to the formation of antibodies that attack one’s own leukocytes. The development of hapten immune agranulocytosis is associated with the use of sulfonamides, NSAIDs-derivatives of pyrazolone, drugs prescribed to patients with tuberculosis , diabetes mellitus , and helminth infections . Haptens form complex compounds with blood proteins or leukocyte membranes and become antigens to which the body begins to produce antibodies. The immune form of the disease also develops in a number of diseases - influenza , yellow fever , malaria , infectious mononucleosis , viral hepatitis, typhoid fever , polio , etc.
- Autoimmune agranulocytosis develops as a result of a pathological reaction of the immune system, as a result of which antineutrophil antibodies are formed. A similar form is observed in patients with autoimmune thyroiditis , systemic lupus erythematosus , rheumatoid arthritis , etc.
- Severe agranulocytosis can develop as a result of chronic lymphocytic leukemia , aplastic anemia , Felty's syndrome .
- The congenital form of the disease develops due to genetic disorders.
Neutropenia, associated with insufficient bone marrow production, is observed in megaloblastic anemia associated with deficiency of folic acid and vitamin B 12 .
The process of neutrophil production can be disrupted by multiple myeloma, leukemia, lymphoma, or metastatic tumors.
Febrile neutropenia (neutropenic fever) is a condition that threatens the patient’s life and develops acutely. At the same time, the number of neurophils in the blood decreases to below 500/mm3. Febrile neutropenia occurs during or after cytostatic chemotherapy for leukemia, and is less common during cytostatic chemotherapy in the treatment of other cancers. It is also possible for this condition to develop after radiation therapy, etc.
NEUTROPENA is a complication that reduces the effectiveness of chemotherapy
Breast cancer is a disease entity, especially early breast cancer, for which it is fundamental to administer the right regimens at the right doses and the right timing in neoadjuvant and adjuvant treatment (that is, either before surgery or after surgery, respectively). When carried out in full - and only in full, in compliance with the doses and timing of treatment - the entire planned course of chemotherapy can increase life expectancy. We are not talking about something like that now, we are talking about months, about years of life.
Fortunately, recently, to improve the results of treatment of early breast cancer - this has already been confirmed in serious large-scale studies - more “strict” drug treatment regimens have been used, which can improve long-term results, that is, increase the number of people cured, surviving and living without symptoms. patient illnesses. But these regimens, which are called dose-consolidated, involve reducing the intervals between injections. Usually, everyone is accustomed to the fact that after the administered course of chemotherapy, some interval is planned - 3-4 weeks, during which the patient usually recovers and is ready for the next administration: blood counts are restored (primarily neutrophils), because, as we have already discussed with you before This means there is a threshold, safe level of neutrophils that allows you to continue/start the next treatment cycle. If it is impossible to achieve it, we cannot begin therapy, which leads to a delay in the planned cycle.
Surveys show that, unfortunately, up to 40% of clinicians prefer to modify regimens rather than do something different. As we have already established, modification of the regimen, changing the intervals between cycles, and reducing the dose lead to a loss of effectiveness of the treatment. It has been proven, for example, that reducing the dose of adjuvant chemotherapy prescribed for early breast cancer by 15% already leads to a significant decrease in life expectancy, and reducing the dose by 35% or more, that is, by a third, completely eliminates the value of this chemotherapy. The survival rate of patients is the same as if they had not received chemotherapy at all.
Therefore, with the introduction of dose-dense chemotherapy regimens into our daily practice and taking into account that the normal bone marrow of any person in most cases does not have time to recover within this short interval, something needs to be done about this in order to carry out the desired cycle at the right time in the right dose treatment. Chemotherapy regimens, which are used specifically in the treatment of early breast cancer, when we really give a chance and must do so in order to cure the patient (we are not talking about metastatic disease, where the goals and principles of therapy are completely different), stimulate the development of neutropenia of 3-4 degrees gravity.
Developed neutropenia, as a rule, leads to a change in the treatment regimen (namely, a reduction in drug doses) and to prolongation of the intervals between cycles. If we do nothing or do it after the fact, when trouble has already happened, and not in advance, we lose the effectiveness of treatment and completely nullify all our efforts. Therefore, it has long become obvious that in order to comply with the planned treatment regimen, it is necessary to use
Symptoms of neutropenia
As a rule, symptoms of neutropenia in children and adults do not develop until the infectious process begins to progress in the body.
Most often, the main manifestation of infectious processes is fever. In this case, the typical symptoms of focal inflammation - pain, swelling, redness, infiltrates - may be absent. Sometimes focal symptoms develop in adults and children, such as mouth ulcers. But they can also be insignificant.
Signs of drug-induced neutropenia may include fever, rash, and lymphadenopathy.
In general, signs of agranulocytosis may be as follows:
- Manifestation of severe weakness.
- Joint pain.
- Pale skin.
- Heavy sweating.
- High body temperature.
- Ulcerative lesions of the pharynx and oral cavity.
Signs of myelotoxic agranulocytosis, in addition to those listed above, include moderate hemorrhagic syndrome . In this case hematomas , nosebleeds and hematuria develop. Myelotoxic agranulocytosis can lead to vomiting and stool containing blood, and bleeding gums.
Signs characteristic of immune agranulocytosis, as a rule, develop acutely. The immune type of the disease is manifested by fever , weakness , and sweating . Ulcerative-necrotic processes develop in the oral cavity. As a result of lesions of the pharynx and oral cavity, stomatitis , pharyngitis , gingivitis , tonsillitis , etc. can develop. Ulcerations with a grayish coating, necrotic plaques, and ulcers on the tonsils (the so-called agranulocytic tonsillitis) appear on the mucous membrane.
lymphadenitis may develop .
When should you contact your healthcare provider?
Contact your healthcare provider immediately if you have any of the following signs of infection:
- temperature 100.4°F (38°C) or higher;
- tremendous chills;
- persistent nausea and vomiting;
- facial redness;
- sweating;
- cough;
- lightheadedness or dizziness;
- diarrhea (loose or watery stools);
- constipation (bowel movements occur less frequently than usual);
- Mouth ulcers
- Headache
- pain in a new place;
- Irritability
- pain or burning when urinating (when you go to the toilet in small quantities);
- feeling weak, especially when combined with flu-like symptoms (such as fever, sore throat, and chills).
to come back to the beginning
Tests and diagnostics
Doctors may suspect neutropenia in people who have frequent, severe infections or unusual infections. This condition is also highly likely to occur in patients undergoing radiation therapy and receiving cytotoxic drugs.
- Anamnesis must be taken into account: the doctor must know what medications or toxic substances the patient took.
- Granulocytopenia is determined by conducting a laboratory blood test to determine the leukocyte formula. A blood test can detect agranulocytosis.
- Culture may also be done to determine infection.
- However, in the diagnostic process, it is important not only to determine the presence of this phenomenon, but also to find out the mechanism and reason for its development. For this purpose, the doctor conducts a physical examination and questioning of the patient.
- A urine and stool test is performed.
- An informative method of investigation is chest radiography.
- People who are immunocompromised have a chest CT scan.
- Other tests are also ordered depending on signs of infection.
Bone marrow testing is performed to determine whether the development of neutropenia is due to decreased production of neutrophils by the bone marrow.
Diagnostic methods
Neutropenia often develops in patients who are susceptible to infections. People who have undergone radiation or chemical therapy are at increased risk. Neutropenia can be detected by a general blood test. Based on the results, the doctor will be able to determine the infectious process in the body. Additionally, diagnostics includes the following studies:
- Bacterial blood culture – identifies pathological agents;
- General urinalysis – determines kidney function;
- Myelograms – studies of bone marrow composition;
- X-ray of the lungs – diagnoses pneumonia.
Treatment with folk remedies
The use of traditional methods can help improve the body's defenses, since when the number of neutrophils decreases, the body's resistance decreases. Folk remedies can be used as a complement to the main treatment, after consulting with a doctor.
- Infusion of walnut leaves . Chop young walnut leaves (30 g) and pour 300 ml of boiling water into a thermos. Leave for 12 hours, drink 50 ml of the drink once a day. It is also recommended to eat a few walnuts every day.
- Onion infusion . Mix 250 onions, pre-finely chopped, with 1 tbsp. sugar and pour a glass of water. Cook for an hour, then cool and store in the refrigerator. Consume several spoons every day.
- Herbal teas . To boost immunity, it is recommended to drink herbal tea with honey. Its composition in different variations may include chamomile, mint, strawberry and blueberry leaves, lemon balm, etc.
- Blend to boost immunity . To prepare it, mix 500 g of cranberries and apples with 200 g of sugar. Add 1 tbsp. water and bring to a boil. When the mixture has cooled slightly, add 300 g of honey. Use 1 tbsp. l. three times a day.
- Remedy for immunity with aloe . It is necessary to keep 500 g of aloe leaves from a plant at least 3 years old in the refrigerator for about 5 days. Before picking the leaves, aloe should not be watered for two weeks. Next, the leaves should be twisted into a meat grinder, add 300 g of honey and 300 ml of Cahors. Drink 1 tbsp three times a day. l. before eating.
Prevention
- The essence of preventing agranulocytosis is to provide patients at risk of developing this condition with careful and regular hematological monitoring. This is necessary, first of all, during the period of use of myelotoxic drugs.
- It is important to exclude the use of those medications that have previously provoked manifestations of immune agranulocytosis .
- It is also important to practice general preventive measures: strengthen the body's defenses, practice physical activity, healthy eating.
- All infectious diseases should be treated promptly and under the supervision of a physician.
Neutropenia in children
Neutropenia in children under one year of age and older can occur due to various reasons. Pediatrician Komarovsky and other well-known experts note that this condition can develop as a result of severe viral, bacterial and fungal lesions, as well as exposure to radiation, radiation therapy, and toxic damage. Neutropenia in infants can also be associated with genetic disorders, as well as with treatment with drugs that interfere with hematopoiesis. A rare condition is congenital agranulocytosis , where a child develops severe immunodeficiency .
As a rule, severe symptoms of this condition do not appear in children, so most often the problems are determined only after a blood test. But if agranulocytosis is not detected for a long time, then a number of symptoms associated with intoxication of the body develop. Therefore, as pediatrician Komarovsky and other doctors note, it is important to monitor the condition of children who have an increased risk of developing neutropenia, and take timely measures to normalize the body’s condition in order to avoid complications.
Diet
Diet 13 table
- Efficacy: therapeutic effect after 4 days
- Time frame: no more than 2 weeks
- Cost of products: 1500-1600 rubles per week
If the number of neutrophils in the body is reduced, it is necessary to especially carefully monitor nutrition so as not to provoke complications dangerous to health. First of all, it is important to avoid those foods that could potentially contain germs or bacteria.
It is recommended to include the following foods in your diet:
- Pasteurized milk, yogurt, cheese.
- All types of meat and fish that have previously undergone thorough heat treatment.
- Hard-boiled eggs.
- Citrus fruits, bananas, frozen fruits.
- Porridge, pasta.
- Nuts.