Developmental defects and preterm birth are the leading causes of childhood mortality, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion of children with developmental disabilities through:
- developing and strengthening registration and surveillance systems;
- gaining experience and building capacity;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Causes and risk factors
Approximately 50% of all birth defects cannot be attributed to a specific cause, but some causes or risk factors are known.
Socio-economic factors
Although low income may be an indirect determinant, developmental disabilities are more likely to occur in families and countries with limited resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to enough and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down syndrome, while motherhood at a young age increases the risk of some congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and nearly doubles the risk of neonatal and infant mortality, mental retardation, and severe birth defects in children born to first-cousin couples. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of birth defects.
Infections
Maternal infections such as syphilis or measles are common causes of birth defects in low- and middle-income countries.
Maternal nutrition
Iodine deficiency, folic acid deficiency, obesity or conditions such as diabetes mellitus are associated with certain developmental defects. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of the fetus or newborn developing birth defects. Working or living near or in the vicinity of landfills, smelters, or mines may also be a risk factor, especially if the mother is exposed to other environmental hazards or is malnourished.
Indications for termination of pregnancy
Any detection of congenital malformation of the fetus presupposes a proposal to terminate the pregnancy for so-called medical reasons. If a woman refuses this and decides to keep the child, she is taken under special control and the pregnancy is monitored more carefully.
But the expectant mother should understand that not only her feelings and experiences are important here, but also the fact that children born with serious defects and pathologies often turn out to be unviable or remain deeply disabled for life, which, of course, is very difficult for any family.
There are other indications for termination of pregnancy:
- malignant neoplasms (pregnancy with cancer is contraindicated);
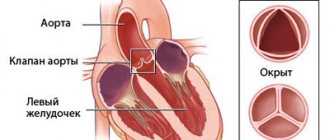
- diseases of the cardiovascular system (heart defects, deep vein thrombosis, thromboembolism);
- neurological diseases (multiple sclerosis, myasthenia gravis);
- infectious diseases (rubella, active tuberculosis, acute and severe viral hepatitis, syphilis);
- diseases of the blood and hematopoietic organs (hemoglobinopathy, aplastic anemia, leukemia);
- eye diseases (diseases of the optic nerve and retina);
- kidney diseases (urolithiasis in acute form and with large stones, acute glomerulonephritis);
- diffuse connective tissue diseases;
- endocrine disorders (diabetes mellitus, thyrotoxicosis, uncompensated hypothyroidism in severe forms);
- some gynecological diseases;
- obstetric indications (refractory gestosis and severe toxicosis of a pregnant woman, accompanied by severe vomiting, gestational trophoblastic disease, severe hereditary diseases identified during pregnancy, etc.)
Abortion for medical reasons is carried out only with the consent of the patient.
Prevention
Preventive health measures taken in preparation for pregnancy and the period of conception, as well as prenatal care, reduce the incidence of some congenital malformations. Primary prevention of developmental defects includes the following measures:
- Improving women's nutrition throughout the reproductive years by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour.
- Monitoring that the pregnant woman does not consume or consumes in limited quantities unhealthy foods, especially alcohol.
- Prevention of diabetes in preparation for pregnancy and during pregnancy through counseling, weight control, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous substances contained in the environment (for example, heavy metals, pesticides, certain medications).
- Ensure that any exposure of a pregnant woman to drugs or radiation for medical purposes (such as X-rays) is justified and based on a careful analysis of risks and health benefits.
- Expanding vaccination coverage for women and children, especially against the rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who have not received the vaccine or who did not have rubella in childhood.
- Expanding vaccination coverage for women and children, especially against the rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine can also be given to women who are not immune to the disease at least one month before becoming pregnant.
- Expanding and strengthening training for health care workers and other staff involved in strengthening the prevention of developmental disabilities.
What to do if your baby has a congenital malformation?
Any married couple who has a sick child, especially one with congenital defects of the nervous system, experiences a state of psychological shock. In order to cope with it, contact geneticists and find out the exact cause that led to the development of the pathology. A sick child should definitely undergo a cytological examination. This is necessary not only for its treatment, but also for predicting the likelihood of rebirth of a sick baby in these spouses.
The final medical genetic consultation should be carried out no earlier than three months after birth. During this time, psychological tension in the family usually decreases, and the spouses will be able to adequately perceive all the information they need.
Video from YouTube on the topic of the article:
Revealing
Health care before conception (preconception) and around the time of conception (periconception) includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be done during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on certain health conditions to their children. Screening includes reviewing the family's medical history and screening to identify a carrier of infection. Screening is especially important in countries where incestuous marriages are common.
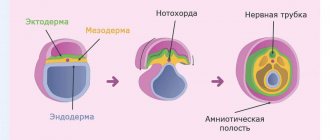
- Preconception screening: Maternal characteristics may increase risk, and screening results should be used to guide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound examination methods can be used to detect Down syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis can help identify neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
- Newborn screening involves a clinical examination as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart defects and early detection of birth defects can facilitate life-saving treatment and prevent the progression of the defect, which may lead to some form of physical, mental, or vision or hearing disability. In some countries, all newborn babies are screened for thyroid and adrenal pathologies before being discharged from the maternity ward.
Classification of fetal malformations
The most common malformations of intrauterine development of the fetus:
- Aplasia (absence of any organ);
- Dystopia (location of an organ in an uncharacteristic place);
- Ectopia (displacement of an organ outward or into an adjacent body cavity);
- Hypotrophy, hypoplasia (decreased fetal body weight, underdevelopment);
- Hypertrophy, hyperplasia (increase in the size of any organ);
- Atresia (closure of natural openings);
- Fusion of paired organs;
- Stenosis (narrowing of the canals and openings of the fetal organs);
- Gigantism (increase in size of the body and internal organs of the fetus);
- Dyschronia (acceleration or inhibition of development of processes).
I would like to note that the severity of pathologies can be completely different. This depends on the location of the genetic defect, as well as on the duration and intensity of the toxic effect on the fetus. There is no clear relationship between them.
A woman who has been exposed to toxicity during pregnancy can give birth to a completely healthy baby. At the same time, the risk of developmental delays in the future offspring of this fetus remains, as a consequence of genetic damage with the absence of clinical manifestations.
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing effective and cost-effective actions to improve newborn health and children.
WHO is also working with the National Center on Birth and Developmental Disabilities, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop global policies to fortify foods with folate at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance for neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess the risks of birth defects prevented by folic acid salts.
The International Clearinghouse for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects birth defects surveillance data and research programs around the world to study, prevent, and mitigate the effects of birth defects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearinghouse for Birth Defects Surveillance and Research and the CDC National Center for Birth Defects and Development, organize annual workshops on birth defect surveillance and prevention and premature birth. The WHO Department of HIV/AIDS is working with these partners to strengthen surveillance of malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programmes.
The GAVI Alliance, whose partners include WHO, is helping developing countries to strengthen the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative instruments, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health and rehabilitation services into general primary health care systems, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their linkages with community-based rehabilitation centres.
Treatment methods for congenital malformation
The treatment method for congenital malformation can vary significantly with different nature and severity of the defect. According to statistics, a quarter of children with congenital malformation die in the first years of life. Another 25% live with permanent mental and physical disabilities. Unfortunately, only 5% of cases have the possibility of treatment. One hundred percent of correctable cases are treated surgically. For some forms of congenital defects, it makes sense to use conservative treatment methods.
Certain types of malformations become noticeable as the child grows older, and some are asymptomatic. Timely prevention of congenital malignancies provides excellent results.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: children's unique vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation; mixed influence of factors related to the social environment, professional activity and nutrition, as well as the living conditions of children (home, school).