There are different types of cells in the blood. One of them are monocytes. These are large cells that literally absorb bacteria, damaged structures of their own body and destroy them. An increase in the level of monocytes is a normal reaction of the body during an infectious disease or inflammatory process. But often an excess of monocytes can also indicate pathology. To reliably establish the cause, it is necessary to carry out appropriate diagnostics.
What are monocytes in the blood
Monocytes are a type of leukocyte - white blood cells. These are large formations with large nuclei. They are involved in protecting the body from inflammatory processes. Monocytes can penetrate the walls of blood vessels, leaving the blood and rushing to the site of inflammation. They destroy bacteria, viruses, as well as dead cells of their own body. It turns out that monocytes perform an important sanitary function.
This is especially important during infectious diseases. For example, if a person is sick with the flu, at this moment many cells of the oropharynx and nasal cavity are destroyed. Then monocytes will arrive in large numbers to the appropriate areas and digest the dead parts of the cells. In this case, the tissues will recover faster, which will contribute to overall recovery.
Functions of monocytes
When aggressive substances or microorganisms enter the surface of the mucous membrane of the nasopharynx or intestine, histiocytes flock to the lesion. These are “ripe” monocytes, adapted to life in tissues. If necessary, new portions of histiocytes-macrophages are urgently prepared.
They surround bacteria, viruses, fungi, and foreign particles, draw them into the protoplasm and provide work to lysosomes to completely dissolve unnecessary molecules.
Having cleared the “battlefield” of toxins and decayed leukocytes, macrophages move on to the process of transmitting information to subsequent generations. This ensures quick recognition of “friends” and “strangers” and aims the body at defense.
Unlike eosinophils, neutrophils, and lymphocytes, cells of the monocyte series are able to “fight” large species of the “enemy” and do not die immediately after the “attack.” Can be reused.
What does it mean if monocytes are elevated?
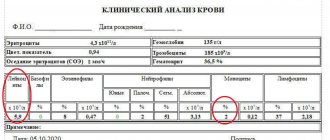
In a normal state, the number of monocytes in the blood is as follows (per 1 liter of blood):
- for adults: from 0.04 to 0.08*109 cell units;
- for children: from 0.05 to 1.1 * 109 cell units.
If we talk about the norm in relative terms, then the number of monocytes should be 1% -10% of the total mass of leukocytes. Moreover, for children the optimal range is from 2% to 7%, and for adults – from 1% to 8%. If the concentration is greater than the specified values, this indicates increased monocytes in the blood. This disorder is called monocytosis.
When is monocytosis not dangerous?
A harmless moderate increase in monocytes can occur against the background of a decrease in lymphocytes and eosinophils. Similar situations are possible with a severe allergic reaction, in the initial stage of childhood viral acute infections (whooping cough, scarlet fever, chicken pox, measles).
An allergic reaction to the skin is accompanied by monocytosis
Significant death of other immune cells occurs. Therefore, the body produces more phagocytes for compensatory purposes to close the gap in protection.
After 2–3 days, with an uncomplicated course of the disease, the required level of eosinophils and lymphocytes is restored. Elevated monocytes during the recovery period are even considered a positive prognostic sign.
The main reasons for the increase in monocytes in the blood
The main causes of monocytosis include:
- Infectious processes of bacterial origin, including syphilis, brucellosis, tuberculosis, endocarditis.
- Viral infections – hepatitis, mononucleosis.
- Diseases of the hematopoietic organs - leukemia.
- Malignant tumors.
- Rheumatism.
- Systemic lupus erythematosus.
- Recovery from infectious diseases.
- Previous surgical interventions.
- Entry of non-infectious substances (mainly through the lungs).
Important!
An increased level of monocytes does not always indicate a disorder. In some cases, this is a normal physiological state, for example, after eating, at the end of the menstrual cycle, and also in children under 7 years of age.
When is the indicator normal?
So, you have a piece of paper in your hands with a summary of various parameters, including: leukocytes, erythrocytes, platelets, hemoglobin level and some others. We reach with our eyes the point “monocytes”. Normally, this figure in a healthy person ranges from 3 to 11%. If your level is higher, it means your body is fighting some kind of disease and you should visit your doctor for further testing. It should be noted that this parameter varies for different age groups and genders. And if in adult men and women the monocyte rate is approximately the same (3-10%), then for children there are some nuances. So, the optimal content of mononuclear phagocytes is:
- For newborns: 3-12%
- For babies up to two weeks: 5-15%
- From one month to a year: 4-10%
- Up to two years: 3-10%
- For children under 16 years old: 3-9%
Monocytosis in children
An increase in monocytes in childhood is also often associated with infectious pathologies, mainly of a viral nature. If monocytosis is diagnosed based on a blood test, this means that the body is actively fighting disease-causing processes.
Also, a similar condition is observed with helminthic lesions - enterobiasis, ascariasis and others. After the destruction of helminths, the content of monocytes returns to normal. The cause may also be associated with tuberculosis, but such pathologies are rare. Monocytosis can be observed due to oncological processes. The most common are leukemia and lymphogranulomatosis.
Other common reasons:
- poisoning;
- allergic reactions;
- inflammation in the gastrointestinal tract;
- autoimmune pathologies;
- rheumatoid type arthritis;
- Crohn's disease;
- infections due to surgical interventions.
Diagnostic value of simultaneous increase in other types of leukocytes
To make a diagnosis in a blood test, it is important to detect not only elevated monocytes, but also other cells of the leukocyte series. Together they:
- indicate the stage of the disease;
- determine the prognosis;
- confirm the type of infectious agent;
- determine the degree of loss of immunity.
Let's look at the most common reactions of blood cells.
Monocytes + lymphocytes
When monocytes and lymphocytes are elevated, an acute viral infection should be suspected: influenza, respiratory disease, measles, rubella, chickenpox. Against this background, a decrease in neutrophils is observed.
It is clear to the doctor that it is necessary to prescribe antiviral drugs.
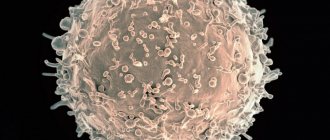
This is what different types of leukocytes look like under a microscope
Monocytes + eosinophils
For elevated monocytes and eosinophils, the necessary conditions are usually allergic reactions and parasitic infection (chlamydia and mycoplasma).
A distinctive symptom in patients is a long, painful dry cough in the absence of wheezing in the lungs and other clinical manifestations.
Monocytes + basophils
Basophils are fast-reacting cells; they manage to approach the source of infection while others are still “considering the information received.” If monocytes and basophils increase, it is necessary to exclude the influence of long-term treatment with hormonal agents.
The growth of basophils always accompanies an increase in macrophages and lymphocytes. They act by producing serotonin, histamine and other substances that increase inflammation.
Symptoms of monocytosis
An increased content of monocytes can be reliably determined only by the results of a blood test. In this case, the disorder manifests itself with certain symptoms:
- apathy, decreased or lack of appetite;
- weight loss for no specific reason;
- high fatigue, general weakness of the body without an objective reason;
- depression;
- high level of anxiety, even panic states;
- emotional overexcitation for no specific reason;
- aversion to meat, aversion to it (occurs suddenly);
- bloating;
- constipation;
- diarrhea;
- discharge of large volumes of mucus with feces;
- dry cough that lasts for a long time (sometimes with blood discharge);
- muscle pain in the back area;
- pain in the legs;
- skin rash;
- rash in the genital area.
Monocytes during pregnancy
In pregnant women, monocyte levels may increase or decrease. Monocytosis means the presence of any infection in the pregnant woman’s body - mononucleosis, herpes virus, influenza or ARVI. If monocytes are elevated during pregnancy, you should definitely inform your obstetrician-gynecologist about this.
He will choose the treatment tactics that are safest for the unborn child.
During the first months of pregnancy, monocytosis is considered normal due to a general increase in the level of leukocytes. Monocytes perform a protective function to a greater extent, helping the mother’s body maintain a healthy fetus. They increase the release of special anti-inflammatory substances into the blood - cytokines, which affect the general defenses of the immune system.
A drop in the number of monocytes indicates the following:
- Unbalanced or poor nutrition of a pregnant woman,
- Lack of vitamins
- Exhaustion of the body
- Anemia.
In this case, you need to reconsider your diet and include more fruits, vegetables, meat and dairy products in the pregnant woman’s diet.
Why is an increase in monocytes dangerous?
An increase in monocytes in the body in most cases indicates the presence of pathology. When an infectious disease appears, the body begins a stubborn fight against it by additionally producing white cells to actively fight the disease. It seems that the more monocytes, the better, because this way you can quickly cope with the disease. In fact, there is a downside, since an excessive amount of them can itself provoke inflammation.
Large accumulations of white bodies in the vessels can:
- Disrupt blood flow.
- Strengthen atherosclerosis.
- Reduce blood flow to the heart muscle.
- Cause damage to the vessel wall.
Biological role in the body
The biological role of monocytes is very diverse. The largest phagocytes are necessary for many functions:
- Phagocytosis.
During this process, monocytes and macrophages identify proteins, bacteria, and viruses that are dangerous to the body, capture them and absorb them (phagocytose).
- Participation in the development of specific immunity.
Monocytes produce special cytotoxins, interferon, to counteract pathogenic viruses, bacteria and fungi.
- Assistance in the formation of allergic reactions.
Thanks to monocytes, specific elements of the compliment system are produced. Due to these processes, foreign proteins - allergens - are identified.
- Protection against tumors.
It is carried out through the production of tumor necrosis factor.
- Regulation of hematopoiesis and blood clotting processes
- carried out through the synthesis of specific elements.
Monocytes have special characteristics that distinguish them from neutrophils and other phagocytes:
- After absorbing a foreign element, monocytes do not die, but continue to function actively. In rare cases, the pathogen can defeat them.
- The life cycle of monocytes is longer than that of neutrophils.
- Monocytes have a pronounced antiviral effect, neutrophils have an antibacterial effect.
- When many monocytes are activated against a foreign agent, pus does not form.
- Chronic inflammatory process is a favorite place for concentration of macrophages and monocytes
Monocytes - what are they?
Monocytes are produced in the red bone marrow and enter the bloodstream completely unformed. Young cells have the maximum ability to absorb harmful elements.
Their main purpose is as follows:
- destruction of large and small foreign particles;
- strengthening the body's immune response;
- improvement of hematopoietic function;
- production of cytotoxin, which has antiviral, antitumor, antiparasitic effects;
- production of interferon and extracellular protein that destroys tumors.
Within 2-3 days, monocytes are in the blood. Afterwards, a certain part dies, and the other migrates outside the vessels and penetrates the tissues of the body, transforming into macrophages. These are cells that devour foreign tissues, toxins and play a primary role in homeostasis. Macrophages accumulate in the site of inflammation and cleanse it of pathogenic bacteria.
Monocytes and macrophages: what is the difference?
In the 70s of the last century, it was believed that all monocytes sooner or later turn into macrophages, and there are no other sources of “professional janitors” in the tissues of the human body. In 2008 and later, new studies were conducted that showed that macrophages are heterogeneous. Some of them actually originate from monocytes, while others arise from other progenitor cells even at the stage of intrauterine development.
The transformation of some cells into others follows a programmed pattern. Coming out of the bloodstream into the tissue, monocytes begin to grow, and the content of internal structures - mitochondria and lysosomes - increases. Such rearrangements allow monocyte macrophages to perform their functions as efficiently as possible.
How to decipher the leukocyte formula?
Leukocyte formula, microscopy of leukocytes, five fractions of leukocytes, differentiation of leukocytes - in doctor’s prescriptions you can find many names for the same thing. Where can I find it and how to decrypt it?
What are leukocytes?
Leukocytes (white blood cells) are a large group of blood cells. Their main purpose is to protect the body from infections. All leukocytes are part of the immune system; they are involved in allergic, autoimmune, and tumor processes. Each type of white blood cell has its own role and is important for the body.
A general blood test without a leukocyte formula speaks only about the total content of leukocytes and does not reveal what type of leukocytes is responsible for the increase (leukocytosis) or decrease (leukopenia) of white blood cells. The leukocyte formula determines five types of leukocytes and is assessed in a comprehensive general blood test. To decipher the leukocyte formula, you need to evaluate the content of each type of leukocyte and their ratio to each other.
The leukocyte formula is calculated by an automatic blood analyzer. Taking the content of all white blood cells as 100%, it gives the percentage (%) of each type of white blood cell. It also automatically measures their content in blood volume (per liter). Sometimes a “hand count” and visual assessment of the blood smear under a microscope is required. For example, when the white blood cell count is altered, there are strange or immature cells, there are signs of anemia or a decrease in platelets in the general blood test. In this case, you can only see the percentage of the leukocyte formula.
Granulocytes - shock forces
The largest part of leukocytes is represented by granulocyte cells. They got their name due to the presence of inclusions (granules). The granules contain immune chemicals. In the leukocyte formula you can see three types of granulocytes: neutrophils, eosinophils, basophils. They differ in the structural features of the core and the coloring of the granules with different dyes. Granulocytes are important in the development of inflammation and immune defense of the body. They are capable of absorbing and digesting proteins and chemicals. All granulocytes mature in the bone marrow, maintaining a supply of mature cells there for 3-4 days. Granulocytes circulate in the blood for no more than 6 hours, moving into the tissues where they perform their function.
Neutrophils make up the largest number of leukocytes circulating in the blood. Every day, 1010 neutrophils enter the bloodstream. Neutrophilia (an increase in the number of neutrophils in the blood) is an indicator of a bacterial infection. The more severe the infection, the more neutrophils come out to fight. Due to their low life expectancy (about 4 days), younger, immature forms of cells (band cells, metamyelocytes, and others) begin to enter the blood. Doctors call this a “leukocyte shift to the left.” When there are very few neutrophils in the blood (neutropenia), the body is not protected from infections.
Eosinophils in the blood make up no more than 5% of the total number of leukocytes. Their concentration fluctuates throughout the day due to the influence of adrenal hormones. In the morning it is maximum. They accumulate in the submucosal layer of the gastrointestinal tract. Eosinophilia (increased eosinophilia in the blood) occurs with parasitic infections, allergic and autoimmune processes.
Basophils make up the smallest number of leukocytes in the blood (less than 1%) and are involved in allergic reactions by releasing histamine. This substance is responsible for bronchospasm, itching, swelling, and redness. Depending on where the basophils get to, there will be manifestations of allergic reactions: an attack of bronchial asthma, skin rash, urticaria, Quincke's edema (swelling of the larynx).
Monocytes are tissue hunters
The second link of leukocytes is monocytes. In the bone marrow, having formed in 5 days, they do not form a reserve. In the blood, monocytes make up about 10% of the mass of leukocytes, quickly disappearing into the tissues. Tissue macrophages, and this is what monocytes will be called, are mainly found in the liver, spleen, and lungs. Their life expectancy is very long (60 days). They are the main hunters of the immune system, because... absorb and process thousands of foreign proteins, turning them into antigens accessible to immune cells.
Monocytosis (an increase in monocytes in the blood) is associated with chronic infections, as well as with infections whose pathogens are hidden in the body’s cells (viruses, chlamydia, mycoplasma).
Lymphocytes are reliable defenders
Antigens processed by monocytes-macrophages and other immune cells attract lymphocytes. Lymphocytes provide acquired immunity by producing antibodies and memory cells to protect against re-infection.
Lymphocytes are formed in the bone marrow and circulate both in the blood and in the lymphatic system. Important organs of cell maturation are the thymus (thymus gland) and lymph nodes. Lymphocytes perform various immune functions, representing the second largest group of leukocytes. There is a special blood test (immunophenotyping) that allows you to identify different types of lymphocytes. This can be important for diseases of the immune system, HIV infection, etc.
In the leukocyte formula, both an increase in lymphocytes (lymphocytosis) - more typical for viral infections - and lymphopenia (a decrease in their number) are important. A lack of lymphocytes reduces the body's defenses and is observed in immunodeficiencies (including HIV infection).
In the Lab4U laboratory you can take the following tests with a 50% discount:
- General blood test with leukocyte formula (automatic counting)
- General blood test with microscopy (manual leukocyte count)
What are monocytes and how are they formed?
Monocytes are a type of agranulocytic leukocyte (white blood cell). This is the largest element of the peripheral blood flow - its diameter is 18-20 microns. The oval-shaped cell contains one eccentrically located polymorphic bean-shaped nucleus. Intense staining of the nucleus makes it possible to distinguish a monocyte from a lymphocyte, which is extremely important in the laboratory assessment of blood parameters.
In a healthy body, monocytes make up 3 to 11% of all white blood cells. These elements are also found in large quantities in other tissues:
- liver;
- spleen;
- Bone marrow;
- The lymph nodes.
Monocytes are synthesized in the bone marrow, where their growth and development are influenced by the following substances:
- Glucocorticosteroids inhibit the production of monocytes.
- Cell growth factors (GM-CSF and M-CSF) activate the development of monocytes.
From the bone marrow, monocytes penetrate into the bloodstream, where they remain for 2-3 days. After a specified period, the cells either die through traditional apoptosis (cell death programmed by nature), or move to a new level - they turn into macrophages. The improved cells leave the bloodstream and enter the tissues, where they remain for 1-2 months.