Published: 03/30/2021 17:00:00 Updated: 03/30/2021
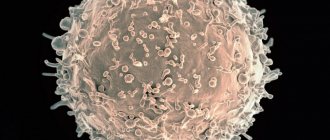
Erythrocytes are red blood cells, the most numerous blood cells. Formally, they are not cells, since during the process of maturation they lose many of the structures necessary for cells. For example, they lack nuclei and do not synthesize any protein molecules, unlike other cells in the body. So the name “cell” in this case is used for convenience. Red blood cells are formed in the bone marrow and constantly circulate in the body, performing the most important function of maintaining life - they carry oxygen from the lungs to tissues and organs and remove carbon dioxide.
In addition to red blood cells, blood contains plasma, platelets, and leukocytes. However, the number of red blood cells is so large that just a couple of drops of blood contains about one billion of these cells. They make up about 40% of the total blood volume. Actually, it is red blood cells that give our blood its characteristic red color due to its hemoglobin content.
Red blood cells do not last forever, they wear out over time and eventually die. The average life cycle of a red blood cell is approximately 120 days—a total of four months. However, do not worry, the bone marrow is constantly producing new cells and maintaining the required level of red blood cells. Various unfavorable circumstances can reduce or, conversely, increase their reproduction rate and affect their life expectancy - thus, the balance of blood composition is disrupted. An increase or decrease in red blood cells is associated with various pathological conditions. Let's consider this issue in more detail.
Red blood cells are normal
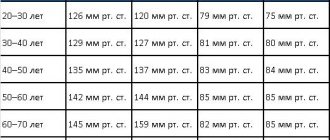
The normal limits vary depending on gender, age and other characteristics.
So, for an adult man it ranges from 4.0 to 5.1 × 10¹² units per liter of blood, and for women - 3.7 to 4.7 × 10¹² per liter.
In pregnant women, red blood cells may decrease to 3–3.5 x 10¹² per liter.
In children under one year of age, the concentration of red blood cells is constantly changing, so to assess the composition of their blood there is a special table that doctors use when interpreting tests.
In childhood, after one year there are still slight deviations from the “adult” norm, but by adolescence the level of red blood cells levels out.
Prevention of increased red blood cells
The cause of the increased production of red blood cells is determined by the doctor. To maintain normal red blood cell levels, it is enough to adhere to preventive measures.
To avoid increased blood concentrations, it is recommended to drink more fluid. The water must be purified, so it is better to buy it in bottles or collect it from wells.
Eating fresh vegetables and fruits has a good effect on blood composition. They contain many vitamins and microelements that regulate the content of red blood cells.
You can reduce the concentration of red cells in the blood by eliminating foods containing iron from your diet. You will have to give up red meat, liver, beans, lentils, spinach, cabbage, prunes and raisins. Avoid drinking caffeinated drinks, smoking or taking aspirin. Regular physical activity will help regulate red blood cell levels.
Elevated red blood cells
Red blood cells can be elevated due to many reasons, ranging from banal dehydration to erythremia - chronic leukemia.
Therefore, if there are any deviations in test results, you should consult a specialist to determine the cause. An increase in the number of red blood cells is called erythrocytosis, which can be: 1. Primary. A rare hereditary disease characterized by loss of energy, dizziness and darker color of the mucous membranes. 2. Secondary. Caused by other diseases or conditions (for example, smoking or staying in high mountains) and is associated with oxygen starvation of cells.
Thus, the following reasons for the increase in red blood cells can be identified:
- Dehydration. When the volume of fluid in the body is reduced, the percentage of red blood cells (and other blood cells) artificially increases.
- A lack of oxygen, which the body tries to compensate by producing more red blood cells.
- Congenital heart defect. If the heart cannot pump blood effectively, the amount of oxygen reaching the tissues is reduced. The body creates more red blood cells to compensate for oxygen deprivation.
- Genetic causes (changes in sensitivity to oxygen, impaired release of oxygen by hemoglobin).
- Polycythemia vera is a rare disease in which the body produces too many red blood cells.
Increased production of red blood cells can cause blood to thicken, slow blood flow, and related problems (eg, headaches, dizziness, vision problems, excessive blood clotting).
Often, elevated red blood cell levels are due to dehydration, hot weather, extreme stress, or excessive exercise. A pathological increase in red blood cells is a fairly rare pathology. Much more often, patients encounter reduced levels.
Description of the causes of erythrocytosis
An excess of red blood cells in the blood plasma is called erythrocytosis. As a result, the blood begins to thicken and moves through the capillaries with difficulty. Red blood cell production spontaneously increases in the body when oxygen levels in cells decrease. Lack of oxygen can be caused by congenital pathology of the heart muscle, heart failure, hemoglobinopathy, chronic obstructive pulmonary disease, and excessive smoking.
It is possible to regulate the formation of red blood cells with the help of certain drugs. These include anabolic steroids, erythropoietin protein and some groups of antibiotics intended for the treatment of infectious and inflammatory processes in hematopoiesis.
The consequence of an increase in red blood cells in blood cells can be dehydration, which occurs as a result of an increase in temperature in the body, the occurrence of gag reflexes and loose stools. During such deviations, the concentration of red blood cells increases, but their number does not change.
Decreased red blood cells
The main symptoms of low red blood cell count are:
- Weakness or fatigue.
- Lack of energy.
- Paleness of the skin.
Reduced red blood cells are a relatively common pathology.
A low number of red blood cells and/or hemoglobin is called anemia. If there are few red blood cells, there is correspondingly less hemoglobin in the bloodstream, which carries oxygen. Thus, the body experiences oxygen starvation, and we feel weakness, drowsiness, loss of vitality, and dizziness. Due to anemia, hair falls out, the skin becomes pale and dry. There are many forms of anemia, each with its own cause. Anemia can be temporary or acquired; depending on severity - from mild to severe. According to a 2015 publication in The Lancet, about one-third of the world's population is anemic.
The most common causes of low red blood cells are:
- Unbalanced diet with deficiency of iron, vitamin B12 or folic acid.
- Damage to the bone marrow (toxins, radiation or chemotherapy, infection, certain medications).
- Any bone marrow disease.
- Chronic inflammatory processes.
- Bleeding in the digestive tract (for example, from ulcers, polyps, colon cancer).
- Heavy menstrual bleeding.
- Trauma with massive blood loss.
- Conditions that cause the destruction of red blood cells (for example, hemolytic anemia caused by autoimmune processes or defects in the red blood cells themselves).
- Kidney failure – serious kidney pathologies lead to a decrease in erythropoietin (or hematopoietin), a kidney hormone that promotes the production of red blood cells.
The risk of anemia is higher in the following groups:
- children aged from 6 months to 2 years;
- pregnant or recently given birth women;
- following a diet low in vitamins, minerals and iron, red meat;
- patients who regularly take medications that cause inflammation of the gastric mucosa (for example, ibuprofen);
- having a family history of hereditary anemia such as sickle cell anemia or thalassemia;
- patients with an intestinal disorder that affects the absorption of nutrients (eg, Crohn's disease);
- have recently experienced major blood loss due to surgery or injury;
- people with chronic diseases (HIV, diabetes, kidney disease, cancer, rheumatoid arthritis, heart failure, liver disease).
Cases of complications
Sometimes not only red blood cells are found in the urine, but also other blood cells - leukocytes, as well as protein compounds. This is clearly a pathological condition, which indicates the development of pathogenic processes. As a rule, they are associated with the following reasons:
- hemorrhagic cystitis;
- urolithiasis;
- inflammation in the kidneys;
- tuberculosis;
- tumors of various nature in the urinary tract.
It is important to take action immediately and get tested. Otherwise, kidney pathology can become chronic, resulting in renal failure.
Deviation from the norm is not always a disease
If the level of red blood cells during the first analysis is slightly outside the normal range, do not panic.
Your doctor will help you interpret the results correctly, taking into account your individual characteristics and medical history. A single slightly elevated or slightly decreased result may have no medical significance. There are several factors that can cause a test result to fall outside the established reference range without pathological reasons:
- Under the influence of external factors (stress, previous infections, physical activity), the results of the analysis of the same person may differ slightly. In this case, a person can be healthy. If the analysis shows a slight deviation, retake the test on another day.
- Individual characteristics. For some people, the boundaries of the norm may differ slightly from generally accepted ones. Reference values are valid for the vast majority of people, but we are all different, and in some rare cases, a healthy person may have their own norms, slightly different from the usual values.
Only a doctor can accurately determine this after conducting additional research.
Cell shapes
A healthy red blood cell has a classic appearance: a smooth and rounded surface, elastic walls, and a flattened central part. Deviations in the structure are rare; the main varieties are presented:
- Spherocytosis - abnormal elements have a spherical shape associated with pathology of the cell membrane. Red blood cells are characterized by increased fragility; their destruction is fixed in the spleen, which leads to the formation of anemia. When an organ is removed, the processes of destruction of red blood cells stop.
- Elliptocytosis is a similar pathology to the previous one. The cells have a non-standard cake-like appearance. Both diseases are associated with genetic predisposition.
- Acanthocytosis - the elements develop a star structure. The deviation is associated with hereditary factors and liver diseases.
- Sickle-shaped erythrocytosis - formed after malaria, formed when the erythrocyte membrane ruptures. In such cells, hemoglobin e performs its main functions due to crystallization.
Tests for red blood cells
A red blood cell count and cell count is usually done as part of a complete blood count (CBC).
A general blood test is the most common analysis, informative for almost any pathological process. This test can also be used to diagnose and/or monitor a number of diseases that affect the production or lifespan of red blood cells. You can take a general blood test with determination of 5 fractions of leukocytes at any CityLab medical center.
For an accurate diagnosis, the doctor may prescribe additional tests:
- Reticulocyte count - determines the number of immature red blood cells.
- Iron test - this trace element plays an important role in the production of red blood cells.
- Vitamin B12 and folic acid levels – these vitamins are also important for red blood cell production.
- A blood test for ferritin reflects iron reserves in the body.
- Serum iron, total iron-binding capacity of blood serum are additional parameters reflecting the process of iron metabolism in the body.
How is an increased content of red blood cells in urine determined?
The analysis consists of 2 stages:
- Studying the color - if the urine has a brown, reddish tint, this indicates a repeated violation of the norm.
- Microscopic examination - if there are more than 3 red blood cells in the urine, doctors diagnose microhematuria.
When establishing an accurate diagnosis, doctors determine the type of red blood cells:
- Unchanged - they contain hemoglobin, and are found in the urine in exactly the same form as in the bloodstream.
- Modified - alkaline. They do not contain hemoglobin, and the cells lose their red color and become colorless. They look like rings (normally they should look like disks with a biconcave surface).
If blood elements are found in the urine, this clearly indicates a pathological process, and it can be very dangerous. Therefore, you must immediately consult a doctor for further examination and consultation.
Changes in childhood
A pathological increase in the number of red blood cells in children is associated with various factors:
- with a low level of oxygen in maternal blood - the anomaly manifests itself in newborns;
- regular exposure of the baby to tobacco smoke (passive smoking);
- living in high mountain areas;
- regular sports activities.
A list of probable sources of deviation in children is presented:
- congenital heart defects;
- bone marrow dysfunction;
- hypertension in the pulmonary circulation;
- blood pathologies;
- obstructive pulmonary lesions with a chronic course;
- acute bronchitis, rhinitis or allergies;
- obesity of the last two degrees;
- dehydration caused by vomiting or diarrhea;
- disruption of the adrenal cortex.
Serious diagnoses associated with changes in the number of red blood cells include cancer of the kidneys and liver. Erythrocytosis is not an independent disease; it indicates latent pathologies or the presence of external influence factors.
General principles of the existence of red blood cells
An erythrocyte is a cell derived from the red germ of hematopoiesis. About 2.4 million of these cells are produced per day, they enter the bloodstream and begin to perform their functions. During the experiments, it was determined that in an adult, red blood cells, the structure of which is significantly simplified compared to other cells of the body, live 100-120 days.
In all vertebrates (with rare exceptions), oxygen is transferred from the respiratory organs to the tissues through hemoglobin in erythrocytes. There are exceptions: all representatives of the family of “white-blooded” fish exist without hemoglobin, although they can synthesize it. Since at the temperature of their habitat, oxygen dissolves well in water and blood plasma, these fish do not require more massive oxygen carriers, which are erythrocytes.
- Indicators of red blood cells and how they are indicated in a blood test, red blood cell mass and treatment of anemia
Primary sources of increasing values
Changes of physiological nature are provoked by:
- severe emotional stress;
- severe dehydration;
- long-term sports activities;
- living in high mountain areas.
The pathological form of erythrocytosis is associated with:
- with erythremia - tumor damage to the hematopoietic organs;
- heart defects - when arterial and venous blood is mixed, there is an insufficient supply of oxygen to the tissues; to compensate for the deviation, the bone marrow begins to produce a larger number of red blood cells;
- neoplasms in the kidneys, pituitary gland, adrenal glands or liver - the organs are responsible for the disposal of old elements in the blood, the formation of the disease leads to the cessation of this function, the tests indicate a predominance of mature forms;
- diseases of the respiratory tract and heart, infectious pathologies - a large number of young or reticular types of elements are observed;
- primary pulmonary hypertension;
- Pickwick's syndrome caused by obesity, pulmonary insufficiency, high blood pressure.
Less dangerous sources of development of an increased number of red blood cells include:
- lack of digestive enzymes;
- dehydration due to heat or prolonged physical activity;
- low-quality water: with chlorine, contaminated, highly carbonated;
- vitamin deficiency or deficiency due to liver dysfunction;
- smoking.
Against the backdrop of a large number of reasons causing changes in tests, only a doctor can correctly determine the original source of the deviation.
Important Notes
Material for research
Children under 7 years of age: venous blood/capillary blood (for special indications).
Children over 7 years of age and adults: venous blood.
Capillary blood collection for research is carried out only for children under 7 years of age (for special indications).
According to GOST R 53079.4-2008, indications for taking capillary blood are possible in newborns, in patients with very small or hard-to-reach veins, with large-area burns, and in severely obese patients.
What are red blood cells?
Even those who are far from medicine sometimes ask questions: what are red blood cells in the blood? What are they needed for? Along with platelets and leukocytes, these blood cells are formed in the red bone marrow of vertebrates, including humans. They are the most numerous and participate in the life of all systems, facilitating the movement of oxygen through tissues and organs. Because of their shape and unique plasticity, red blood cells can easily move through capillaries, facilitating gas exchange.
The structure of red blood cells
The structure and functions of red blood cells make them plastic and easily deformable. The liquid contents of cells - the cytoplasm - is rich in hemoglobin, which contains a divalent iron atom that binds oxygen. The same pigment gives the bodies their red color. Red blood cells are disc-shaped and do not have a nucleus, which is lost during maturation. The composition of red cells is as follows:
- reticular stroma;
- hemoglobin-filled cell;
- dense shell.
The structure of human red blood cells is simplified: inside there is a membrane resembling a mesh, while the plasma membranes of leukocytes and platelets are more complex. The membrane of red cells is special - it is impermeable to cations (with the exception of potassium), but it allows chlorine anions, oxygen molecules and carbon dioxide to pass through well.
How are red blood cells formed in the blood?
How are red blood cells formed? Tissue growth occurs through the multiplication of one cell, called proliferation. After this, the stem cells, as the ancestors of hematopoiesis, form a large body with a nucleus, which is lost as the red blood cell grows. Once in the bloodstream, the body is transformed into a ready-made red blood cell. The process takes up to 3 hours, and red cells are formed in the body without interruption.
Every second, more than 2 million red blood cells are formed in the bone marrow of the spine, skull and ribs, in addition - in the endings of the arms and legs (in children). Circulating in the blood for 3-4 months (about 110 days), red blood cells are absorbed by macrophages and destroyed in the spleen and liver. A small part of them undergoes phagocytosis - capture by solid particles of cells - in the vascular bed. The transfer of oxygen throughout the body and participation in the transfer of carbon dioxide are the central functions of red blood cells. Cell production begins in the fifth month of fetal development.
References
- Nazarenko G.I., Kishkun A.A. Clinical assessment of laboratory research results // M.: Medicine - 2006. - 544 p.
- Tatkov O.V., Stupin F.P. General blood test. Information collection // M.: Publishing solutions. — 2021. — 72 p.
- Fauci, Braunwald, Kasper, Hauser, Longo, Jameson, Loscalzo Harrison's principles of internal medicine, 17th edition, 2009
- Mosby's Diagnostic and Laboratory Test Reference 14th Edition, 3251 Riverport Lane
- St. Louis, Missouri 63043: Elsevier Publishing Hall 2019
General blood test: interpretation, table of normal values, preparation for donation
A clinical (general) blood test is a laboratory study of the qualitative and quantitative composition of a patient’s blood in order to diagnose and identify signs of infection and inflammatory processes in the body. A general blood test is always prescribed at the first sign of illness, but doctors recommend doing it for preventive purposes at least once a year. The results of the analysis are also entered into the sanatorium-resort card, therefore, without it, treatment in the sanatorium is not prescribed.
Subject of study and table of norms
To conduct a general blood test, venous or capillary blood is taken, which is examined for the levels of red blood cells, platelets, hemoglobin, the erythrocyte sedimentation rate, the number of leukocytes, hematocrit and a number of other parameters.
It is worth noting that for boys and girls under 12 years of age, the normal indicators are the same, and then a difference appears not only from the gender, but also from the age of the patient - when interpreting the results, the doctor always makes an allowance for this. When taking blood from a vein and from a finger, the results may differ slightly, so for a correct analysis of the dynamics, it is recommended to donate blood using the same method. Table of reference values for general blood test indicators
| Index | Designation | Norma (women) | Norma (men) | Units |
| Hemoglobin | HGB, Hb, hemohlobin | 117–155 | 132–173 | g/l |
| Average red blood cell volume | MCV, macrocytosis, normocytosis, microcytosis | 78–101 | 80–101 | fl |
| Distribution of red blood cells by volume | RDW, red cell distribution width | 11,6–14,8 | 11,6–14,8 | % |
| Total red blood cell count | RBC, red blood cells | 3,9–5,3 | 4,2–5,6 | million/µl |
| Total platelet count | PLT, PC, platelets, platelet count | 150–400 | 150–400 | thousand/µl |
| Erythrocyte sedimentation rate | ESR, ESR, ROE | 2–20 | 2–15 | mm/h |
| Hematocrit | HCT, hematocrit | 34–47 | 37–50 | % |
| Average erythrocyte hemoglobin | MCH | 27–34 | 27–35 | pg |
| Reticulocytes | RET | 0,5–1,2 | 0,5–1,2 | % |
| Total white blood cell count | WBC, white blood cells | 4,5–11 | 4,5–11 | thousand/µl |
| Leukocyte formula | ||||
| Neutrophils | NEUT | 47–72 | 47–72 | % |
| Lymphocytes | LYM | 19–37 | 19–37 | % |
| Monocytes | MON | 3–12 | 3–12 | % |
| Eosinophils | EO | 1–5 | 1–5 | % |
| Basophils | BAS | 0–1,2 | 0–1,2 | % |
Sanatorium
Tours
Flights
Transfers
Interpretation of a general blood test
Before moving on to describing the indicators of a general blood test, we emphasize that the information below is for informational purposes only and the results should be deciphered by a doctor. As a rule, diseases are complex in nature and simultaneously affect several blood parameters, the connection between which can only be made by a doctor. An attempt to engage in self-diagnosis is fraught with incorrect conclusions and, as a result, making decisions that are hazardous to health. Let us also pay attention to the fact that in 5% of healthy people, normal values may go beyond the accepted reference (statistical average) values.
Red blood cells
Erythrocytes - red blood cells - act as couriers in the human body. Due to their elasticity, they penetrate into vessels of any diameter and transport oxygen from the lungs to all organs and tissues, and transfer carbon dioxide in the opposite direction. These gases are added to hemoglobin contained in red blood cells.
High values of red blood cells in the results may indicate dehydration, blood diseases, heart and respiratory failure.
A low level of red blood cells is observed with blood loss, leukemia, lymphomas, congenital disorders of hematopoietic function, malignant tumors, hemolytic anemia, as well as with a deficiency of protein, iron and vitamins in the body.
Platelets
The main functions of platelets are blood clotting, the creation of blood clots, maintaining the tone of vascular walls and feeding capillaries.
A high level of platelets in the patient’s blood can be interpreted as a consequence of resection of the spleen, exacerbation of chronic autoimmune diseases, anemia of various origins, and inflammatory processes. The number of platelets tends to increase in the third trimester of pregnancy, in the postoperative period, with the development of erythremia and malignant tumors.
A low platelet count in the patient's blood may indicate hemophilia, drug-induced thrombocytopenia, systemic lupus erythematosus, renal vein thrombosis, the presence of a viral or bacterial infection, aplastic anemia, Fisher-Evans syndrome.
Hemoglobin
Hemoglobin levels are tested to evaluate the severity of anemia or polycythemia and to evaluate the effectiveness of treatment for these conditions. Hemoglobin is an iron-containing protein found in red blood cells that performs a gas exchange function.
An increase in hemoglobin is observed with dehydration, cardiac and pulmonary failure, overdose of diuretics, heart defects, various diseases of the blood and urinary system.
Anemia of various etiologies, blood diseases, blood loss, deficiency of proteins, vitamins and iron lead to a decrease in hemoglobin.
Leukocytes
Leukocytes - white blood cells - are produced by the bone marrow and perform a protective function in the human body. They help fight foreign objects in the blood, infections, foreign protein molecules, and dissolve damaged tissue at the stage of inflammation.
The number of leukocytes in a general blood test can increase for many reasons of different nature: it can be pregnancy, physical stress or eating before donating blood, vaccinations, systemic or local inflammation, trauma, burns, autoimmune diseases, conditions after operations, oncology, leukemia and leukemia.
The leukocyte count decreases due to viral infections, systemic autoimmune diseases, leukemia, radiation sickness, vitamin deficiency, as well as due to the use of cytostatics and steroids.
Leukocyte formula
The leukocyte formula is a description of the various forms of leukocytes in the blood serum, expressed either in quantity or as a percentage. The leukocyte population includes 5 types of cells: neutrophils, lymphocytes, monocytes, eosinophils and basophils.
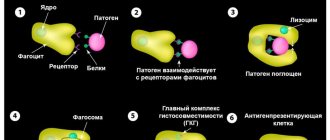
Neutrophils are always represented in the greatest numbers; they are the first to “fight” the infection, surround and eliminate bacteria by phagocytosis. The most common cause of increased neutrophil levels in the blood is acute bacterial and fungal infections. Other possible causes of an increase in the number of neutrophils are systemic inflammatory diseases, pancreatitis, myocardial infarction, conditions after burns, and malignant bone marrow tumors. The number of neutrophils decreases with massive bacterial infections, sepsis, viral infections, aplastic anemia, and tumor metastases to the bone marrow.
Lymphocytes are indispensable tools of the immune system; without them, viruses cannot be destroyed and infection can be fought. B-lymphocytes “specialize” in producing antibodies, T-lymphocytes – in destroying infected cells, preventing the spread of infection, as well as identifying and destroying cancer cells. Acute bacterial infections, influenza, aplastic anemia, AIDS, systemic lupus erythematosus, some congenital diseases and taking prednisolone lead to a decrease in the level of lymphocytes. Infectious mononucleosis, rubella, chickenpox and other viral infections, malignant tumors of the bone marrow and lymph nodes, as well as some bacterial infections lead to an increase in the level of lymphocytes.
monocytes in the blood, but they perform an important protective function. Monocytes have the ability to turn into macrophages, destroying damaged cells and retaining foreign proteins on their surface, thereby facilitating the work of lymphocytes. A decrease in the number of monocytes usually indicates aplastic anemia or accompanies treatment with prednisolone. An increase in the concentration of monocytes manifests itself in acute bacterial infections, tuberculosis, syphilis, sarcoidosis, connective tissue diseases, and oncological diseases of various localizations.
eosinophils in the blood relative to other leukocytes, and they also have the ability to phagocytose, but their main task is to fight parasites and regulate allergic reactions. An increased level of eosinophils accompanies allergic diseases (bronchial asthma, eczema, food allergies), allergic reactions to medications and infection with parasitic worms. Much less frequently, an increase in the number of eosinophils can be explained by the development of malignant tumors in the bone marrow and lymph nodes, systemic connective tissue diseases, or Lefler's syndrome. The number of eosinophils decreases during treatment with prednisolone, with Cushing's and Goodpasture's syndromes, as well as with acute bacterial infections.
basophils release histamine, a substance that causes allergy symptoms (itching, burning, redness). The concentration of basophils in blood test results decreases during the acute phase of an infectious disease, hyperthyroidism, and prolonged treatment with corticosteroids. An increase in the content of basophils is rarely observed, for example, with cancer of the bone marrow and lymph nodes, polycythemia vera, and some allergic diseases.
Reticulocytes
Reticulocytes are young red blood cells produced by the bone marrow. A quantitative study of reticulocytes in the blood provides insight into how adequately the bone marrow is producing red blood cells. The level of reticulocytes may deviate from the norm due to third-party reasons, such as: climbing to high altitudes, scuba diving, smoking, pregnancy, taking medications.
An increase in reticulocytes in the results of a general blood test is caused by bleeding, hemolysis, inflammation, cancer, polycythemia of various etiologies, the consequences of radiation therapy and chemotherapy, and side effects from the treatment of anemia.
Having detected a low level of reticulocytes in the results, the doctor may suggest iron deficiency, B12 deficiency or folate deficiency anemia, thyroid disease, aplastic anemia, kidney disease, chronic infections, uremia.
Hematocrit
Hematocrit, measured as a percentage, is the ratio of the volume of red blood cells to the volume of the liquid component of blood. An increased hematocrit is detected in iron-, B12- and folate-deficiency anemia, bleeding, impaired hemoglobin synthesis, liver cirrhosis, hemolysis, malignant tumors, or due to intravenous administration of significant volumes of fluids. A low hematocrit usually indicates dehydration, but can also be a sign of congestive heart failure, COPD, or polycythemia vera.
Erythrocyte sedimentation rate (ESR)
This test is designed to evaluate how quickly the blood separates into plasma and red blood cells. The test results are used to diagnose diseases associated with acute or chronic inflammation, including cancer, infections and autoimmune diseases. Infectious and inflammatory diseases, connective tissue diseases, cancer, myocardial infarction, anemia, burns and injuries increase the ESR value, while a decrease in ESR is usually caused by polycythemia and diseases associated with changes in the shape of red blood cells.
How to prepare to donate blood
- The day before the scheduled time of blood donation, stop drinking alcohol.
- It is recommended to avoid taking medications one day before blood sampling (requires separate approval from your doctor).
- 8 hours before the study, refuse to eat, drinking still water is allowed.
- Half an hour before donating blood, avoid physical and emotional stress.
- Also, stop smoking half an hour before the test.
Support
Are you not sure what criteria to use to choose a resort or sanatorium?
Don't know how to book?
Call us and our support staff will help you.
FAQ
Evgeniy Korostelev
Head of Help Desk
Help Desk Presentation
From Germany
+4974328093002
From other countries
+420355455981
The doctor's consultation
Free help from a health resort doctor
If you find it difficult to independently search for a resort and sanatorium that is optimally suited for treating your diseases, then take advantage of a free consultation with a health resort doctor Elena Khorosheva.
Submit your question here
Elena Khorosheva
Chief physician sanatoriums.com
Presentation by doctor Elena Khorosheva
From other countries
+420355455981