Home | About us | Delivery | Advertisers | Login | Registration
The pharmacy is closed on Sundays and holidays.
- Medicines
- dietary supplementsVitamins
- Categories from A to Z
- Brands from A to Z
- Products from A to Z
- Medical equipment
- beauty
- Child
- Care
- Honey products appointments
- Herbs and herbal teas
- Medical nutrition
- Journey
- Making medicinesStock
Pharmacy online is the best pharmacy in Almaty, delivering medicines to Almaty. An online pharmacy or online pharmacy provides the following types of services: delivery of medicines, medicines to your home. Online pharmacy Almaty or online pharmacy Almaty delivers medicines to your home, as well as home delivery of medicines in Almaty.
my basket
Apteka84.kz is an online pharmacy that offers its customers medicines, medicinal and decorative cosmetics, dietary supplements, vitamins, baby food, intimate products for adults, medical equipment and thousands of other medical and cosmetic products at low prices. All data presented on the Apteka84.kz website is for informational purposes only and is not a substitute for professional medical care. Apteka84.kz strongly recommends that you carefully read the instructions for use contained in each package of medicines and other products. If you currently have any symptoms of the disease, you should seek help from a doctor. You should always tell your doctor or pharmacist about all the medicines you take. If you feel you need further help, please consult your local pharmacist or contact our GP online or by telephone.
© 2021 Pharmacy 84.
Fibrocystic disease (FCD) is the most common disease of the mammary glands of women of reproductive age and, according to WHO definition, includes a hyperplastic process characterized by a wide range of proliferative and regressive changes in breast tissue with an altered, disrupted ratio of epithelial and connective tissue components.
Among the risk factors for the occurrence of FCD, including proliferative forms, there are: low frequency of births; low frequency of the first pregnancy ending in childbirth (induced abortion is much more often the outcome of the first pregnancy); high frequency of induced abortions, combination with hyperplastic processes in other organs of the reproductive system [6].
Clinical symptoms of FCD are pain, nipple discharge and changes in the consistency of the mammary glands. Mastalgia is the main symptom of the disease. It was first described by A. Cooper [8] in 1829. Mastalgia is a nonspecific symptom of FCD: about 70% of women of reproductive age have it, and only in every third of them changes characteristic of FCD are detected by palpation [19]. With FCD, pain in most cases is cyclical, with the appearance or increasing intensity in the second phase of the menstrual cycle, on the eve of menstruation. Cyclic mastalgia occurs in 67-80% of patients who report chest pain [1]. In a small percentage of patients, it may not be associated with the menstrual cycle [19]. About 15% of women with FCD do not experience any pain [5].
Mastalgia is most often observed in the upper outer quadrants of the mammary gland and axillary region. The pain is of a different nature: pulling, aching, stabbing pains are described. The pain can be local or radiate to the scapula, collarbone, hypochondrium, neck, armpit, shoulder. Differential diagnosis of mastalgia is carried out with pain syndrome due to cervicothoracic osteochondrosis, radiculoneuritis, intercostal neuralgia, plexitis, myositis, Titz syndrome, as well as angina pectoris [19]. It is assumed that mastalgia is caused by irritation of sensory nerves due to swelling, fibrosis of connective tissue, as well as the presence of cysts. Painful sensations disrupt the quality of life of patients and reduce their ability to work. Mastalgia disrupts social adaptation in 12% of patients, worsens working and studying conditions in 8%, and reduces sexual activity in 48% [12]. Some patients with FCD have autonomic neuroses, manifested by sleep disturbances, frequent migraine-like headaches, and often a depressive syndrome, weakness, tearfulness, anxiety, and cancer phobia [11]. It has been proven that proliferative forms of FCD are a risk factor for breast cancer [9]. In recent years, there has been an increase in the incidence of oncological pathology of the mammary glands, which occupies a leading place in the structure of oncological morbidity and mortality, amounting to 19.8 and 17.2%, respectively [5]. The five-year survival rate of breast cancer patients is 55%, and this is explained by the fact that tumor cell invasion, canceremia, and the resulting formation of micrometastases in various organs precede in many cases the possibility of early diagnosis of the tumor [9, 10]. Thus, the treatment of FCD is relevant in many aspects. Until now, there is no unified model of pathogenetic therapy; there are no standard treatment programs for various types of FCD. When identifying signs of FCD and excluding a malignant tumor, the doctor’s tactics most often consist of dynamic observation and the use of drugs that reduce the severity of mastalgia.
To relieve mastalgia, a fairly wide arsenal of effects is used, including medications. For a long time, the main method of treating patients with mastopathy was physiotherapeutic treatment and various non-hormonal medications. In the presence of severe pain symptoms in FCD, anti-inflammatory drugs from the group of non-steroidal anti-inflammatory drugs were used [18]. One of the areas of complex treatment of mastopathy is various dietary recommendations, exclusion or limitation of consumption of methylxanthines [13, 14, 16, 17].
Various herbal preparations and phytotherapeutic mixtures [3, 6] based on kelp, twig, indole-3-carbinol, and evening primrose have become widespread in the treatment of mastopathy.
The diverse effects of enzyme preparations on many physiological and pathophysiological processes in the body are known. In particular, they increase the ability of leukocytes to produce interferons, reduce the concentration of immune complexes, prevent their sedimentation and binding to cells, including tumor cells, destroy the so-called fibrin cover, and stimulate the production of tumor necrotic factor. This potentiates the anti-carcinogenic effects of the immune system. In the treatment of mastopathy, in particular, Wobenzym is used, which contains enzymes from papaya, pineapple and animal pancreas [2, 4].
The possible positive effect of non-hormonal agents on the clinical symptoms of FCD is usually short-term, and information about their effect on the mechanisms of disease development is limited and contradictory.
The use of hormonal drugs in the treatment of FCD is based on their antiestrogenic effect (antiestrogens), the ability to inhibit the hormonal and ovulatory functions of the ovaries (antigonadotropins, combined oral contraceptives, gonadotropin-releasing hormone agonists), and a decrease in prolactin production (dopamine receptor agonists).
It should be remembered: most patients of reproductive age with FCD require effective contraception. Hormonal contraception avoids induced abortion as a risk factor for FCD, promotes the regulation of the menstrual cycle, reduces the frequency of dysfunctional uterine bleeding caused by impaired hormonal function of the ovaries in the form of anovulation or the formation of an incomplete corpus luteum, which leads to relative hyperestrogenism. When taking hormonal contraceptives, the intensity of estrogenic effects decreases; gestagens included in contraceptives can have a positive effect on breast tissue. However, in 25–30% of women with FCD, mastalgia progresses while taking combined oral contraceptives (COCs), and is currently thought to be due to the estrogen component of COCs.
According to the eligibility criteria for contraceptive methods (WHO, 2009), benign breast disease and a family history of breast cancer are conditions for which there are no restrictions on the use of combined estrogen-progestin contraceptives (acceptability category 1). Women with undiagnosed breast diseases belong to category 2. Hormonal contraception is contraindicated in women with breast cancer at the time of examination (eligibility category 4) and a history of breast cancer (eligibility category 3). However, it should be remembered that there are a number of contraindications for the use of the estrogen component. Pure progestin contraceptives are one of the types of hormonal contraception, which was created due to the need to eliminate the estrogenic component, which causes most metabolic disorders, hypertension and especially the risk of thromboembolic conditions. Representatives of progestin contraceptives include the drug Lactinet, the main active ingredient in which is the progestogen desogestrel. The latter is quickly and almost completely absorbed from the gastrointestinal tract and is immediately metabolized in the liver and intestinal wall into 3-ketodesogestrel, which is a biologically active metabolite of desogestrel. The bioavailability of desogestrel is 62-81%; 3-ketodesogestrel binds to plasma proteins, mainly albumin and sex hormone-binding globulin. The products of further metabolism of ketodesogestrel are pharmacologically inactive; some of them are converted by conjugation into polar metabolites, primarily sulfates and glucuronides. The half-life of desogestrel is 38 hours. Metabolites are excreted through the kidneys and intestines. The Pearl index for the drug is 0.4, which is similar to the indicator when using combined hormonal contraceptives. It has been established that desogestrel inhibits estrogen-induced proliferative activity of breast cancer cells (MCF-7 line) and reduces the activity of α-estrogen receptors (Otto et al., 2008).
The purpose of this study is to study the effect of desogestrel on the condition of the mammary glands and the severity of mastalgia in patients of reproductive age with FCD who require contraception.
Material and methods
The criteria for inclusion in the study group were: age 18–40 years, body mass index 18.5–29.9 kg/m2, clinical signs of FCD (mastalgia, heterogeneity of breast tissue during physical examination), ultrasound signs of FCD, need for contraception.
Exclusion criteria: suspected or confirmed malignant process in the mammary gland, pregnancy, postpartum period, lactation, use of hormonal contraception within the last 6 months, severe extragenital pathology, malignant neoplasms.
17 patients with FCD who met the inclusion criteria for the study were examined. The average age of the patients was 29.4±1.2 years.
The examination of the patients included: assessment of the medical history, obstetric and gynecological history, patient complaints, as well as examination and palpation of the mammary glands. The following complaints from the mammary glands were taken into account: pain (mastalgia), discharge from the nipples and changes in the consistency of the mammary glands, identified by the patient herself.
To assess mastalgia, the following characteristics were used: the woman’s age at the onset of mastalgia, connection with the menstrual cycle, duration over the course of a month, intensity, character (bursting, aching, feeling of heaviness). To objectively characterize the intensity of the pain syndrome, a visual analogue scale was used, on which a segment of 1–3 cm indicated pain of mild intensity, 4–6 cm indicated pain of moderate intensity, and 7–10 indicated severe pain.
When examining the mammary glands, the following were assessed: size, contours, symmetry, condition of their skin (color, presence of swelling, ulcerations), nipple and areola (size, location, shape, discharge and/or ulcerations).
Palpation of the mammary glands was carried out with the patient lying on her back and standing. During palpation, the consistency, elasticity, homogeneity, tenderness (sensitivity) of the mammary gland and the presence of space-occupying formations were assessed. In addition, the condition of areas of possible regional metastasis (axillary and supraclavicular areas) was examined.
On the 5th-7th day of the cycle, an ultrasound examination of the mammary glands was performed, during which the thickness of the glandular tissue, its echogenicity, the degree of fatty transformation, the diameter of the milk ducts, and the presence and diameter of cysts were determined.
In order to assess the state of ovarian function of the examined patients, before starting treatment, the blood levels of FSH, LH (on the 3-5th day of the cycle), and progesterone (on the 20-22nd day of the cycle) were determined using the enzyme immunoassay method. When the progesterone level was ≥25 nmol/l, the menstrual cycle was considered ovulatory, from 10 to 25 nmol/l - with luteal phase deficiency (LPF), ≤10 nmol/l - anovulatory.
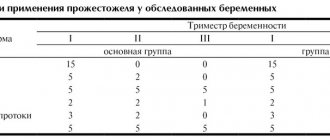
For contraception and treatment of mastalgia caused by FCD, all patients received the drug Lactinet (75 mcg desogestrel) for 6 months. The examination was carried out before the start, after 3 and 6 months of taking the drug. Clinical and ultrasound characteristics were used to assess the therapeutic efficacy of desogestrel against mastalgia.
Results and discussion
The average age of menarche in the examined women was 13.1±0.3 years. 7 (41%) women had a history of pregnancy, while only 4 had a pregnancy that ended in full-term birth, and 3 had an induced abortion. All 4 patients had lactation for more than 6 months. At the time of inclusion in the study, none of the patients were interested in pregnancy.
Of the gynecological diseases, intramural uterine fibroids (up to 1.5 cm in diameter) were identified in 2 patients at the time of inclusion in the study.
Five patients had previously received low-dose oral contraceptives for contraception for 3 to 6 months; the main reason for refusal was an increase in the intensity and duration of mastalgia.
The diagnosis of FCD was made based on clinical and ultrasound findings. Upon examination and palpation of the mammary glands in all women, diffuse compactions were determined, the boundaries of the compaction smoothly passed into the surrounding tissues.
The average age of onset of mastalgia was 19.4±1.5 years. In all patients, the pain was cyclical and bothersome in the second phase of the cycle. At the time of inclusion in the study, the average duration of mastalgia was 7.1±0.9 years. The duration of mastalgia before starting to take Lactinet was 8.4±0.6 days in each cycle.
The majority (56.8%) of women had a moderate degree of mastalgia, 25% had a strong degree of mastalgia, and only 18.2% had a mild degree of pain. According to the nature of the pain syndrome, bursting pain was observed in 45.7% of women, a feeling of heaviness - in 41.3%, aching pain - in 13%.
Before the start of therapy, the thickness of the glandular tissue layer was on average 17.9 ± 1.5 mm, the average diameter of the milk ducts was 1.44 ± 0.06 mm. In 35.3% of patients, cysts with a diameter of up to 10 mm were detected in the mammary glands. In 41.2% of patients, the echogenicity of organ tissue was average, in 58.8% it was increased.
After a comprehensive examination, the patients were prescribed desogestrel at a daily dose of 75 mcg. Nine patients experienced spotting and bleeding from the genital tract; therefore, for three of them, the drug was discontinued after 1-3 months. Thus, 14 patients took Lactinet for 6 cycles, and pregnancy did not occur in any case.
After 3 months from the start of taking Lactinet, the duration of mastalgia significantly decreased to 4.3±0.8 days (p<0.05) compared to the value before the start of therapy. The bursting pain and feeling of heaviness disappeared, all women still had aching pain after 3 months of taking Lactinet. Mild mastalgia prevailed; severe and moderate mastalgia was absent in all patients. Patients stopped noticing the cyclical nature of mastalgia (see table).
Ultrasound examination showed that after 3 months of taking Laktinet, the thickness of the glandular tissue layer was 12.7±1.1 mm (p<0.01), which was significantly less than before the start of therapy (17.9 mm). However, the diameter of the milk ducts did not change, and the cysts did not regress.
After 6 months of taking Lactinet, all women experienced further regression of mastalgia. In 2 patients this symptom was absent, in 12 patients the mastalgia was mild, in the form of aching pain. The duration of mastalgia was on average 3.1±0.8 days and there was no cyclicity.
The thickness of the glandular layer at the end of 6 months of taking Lactinet was 9.3±1.4 mm (p<0.05 - compared with the thickness of the glandular layer before treatment with Lactinet (see figure).
Figure 1. Thickness of the glandular layer before (a) and after 6 months (b) from the start of Lactinet therapy. Ultrasound data. The thickness of the ducts did not change significantly, the cysts did not regress, and cyst growth was also not observed.
When using the progestin contraceptive Lactinet for 6 months in women with mastalgia caused by FCB, the frequency, duration and intensity of mastalgia significantly decreased.
The change in the clinical picture of the disease was accompanied by a decrease in the thickness of the glandular layer of the mammary glands.
The highest rates of change in the clinical characteristics of mastalgia and ultrasound parameters were observed in the first 3 months from the start of therapy.