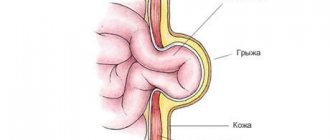
A hiatal hernia (HH, hiatal hernia, gastric hernia) is an enlargement of the esophageal opening of the diaphragm through which the esophagus normally penetrates into the abdominal cavity, and with a hernia, an abdominal organ, most often the stomach, penetrates into the chest. Sometimes intestinal loops and, extremely rarely, the spleen penetrate into the chest with hiatal hernia. This disease is quite common, it is found on average in 40% of the world's population. Fortunately, for the majority it does not cause any problems, but in 5 - 7% of all gastroenterological patients, complaints are caused by this particular disease (Figure 1).
Causes of hiatal hernia
Most often, it is not possible to find out the cause of the development of this disease in a particular patient. In general, hiatal hernia is a multifactorial disease and it can be difficult to identify one single cause unless there is a clear connection with trauma.
The following reasons for the development of a hiatal hernia are identified:
- Increased intra-abdominal pressure, for example due to overeating at night, or chronic constipation. Another reason for increased intra-abdominal pressure, and hence the development of hiatal hernia, is heavy physical labor.
- Congenital degenerative changes in the ligamentous apparatus and connective tissue.
- Age and associated connective tissue degeneration. Therefore, in these patients it is not uncommon to have a combination with an inguinal or ventral hernia.
- Blunt abdominal trauma.
- The presence of chronic diseases that disrupt the normal motility of the gastrointestinal tract (peptic ulcer, reflux esophagitis, cholelithiasis, diseases of the large intestine).
- Excess weight. In overweight people, intra-abdominal pressure increases, which leads to “squeezing” the stomach into the chest
Symptoms of the disease
The patient may not notice a small hernia at all - it does not manifest itself in any way and does not affect the quality of life.
Most patients report the following symptoms:
- Heartburn
- Belching
- Abdominal pain (stomach area)
- Discomfort behind the sternum
- Shortness of breath and rapid heart rate
- Feeling of fullness in the epigastric region
- Dysphagia (difficulty swallowing)
Symptoms may appear during abdominal exercises, sudden bending, or wearing tight clothes that are tightly tied at the waist.
Non-food manifestations include:
- Cough with no other proven cause
- Sore throat, nasal congestion
- Damage to tooth enamel
- Anemia.
Often the doctor has to exercise deductive abilities, finding a connection between a lingering cough of unknown etiology or low hemoglobin in a blood test and a hiatal hernia that no longer manifests itself.
Classification of hiatal hernia
In our country, unfortunately, there are many classifications of this disease, but the most common classification proposed by B.V. Petrovsky and N.N. Kanshin. Following it, the following variants of the hiatal hernia are distinguished:
Axial:
- fixed
- unfixed
Without shortening of the esophagus
- cardiac
- cardiofundic
- subtotal
- total
With shortening of the esophagus
1st degree of cardia is fixed 4 cm above the diaphragm
Grade 2 cardia is fixed more than 4 cm in the chest
Paraesophageal
- fundamental
- antral
- intestinal
Now let's figure out what is what. So, a hiatal hernia is called axial if the esophagogastric junction is located above the diaphragm. It is called cardiac if only the cardia (upper part of the stomach) is located above the diaphragm, cardiofundal hernia is called if both the cardia and the fundus of the stomach go into the mediastinum, subtotal hernia is called if 2⁄3 of the stomach goes into the mediastinum (above the esophageal opening of the diaphragm), and, accordingly, total This is when the entire stomach is located in the chest.
A paraesophageal hernia is a situation when the esophageal-gastric junction (cardia of the stomach or simply cardia) is located in the abdominal cavity, and any part of the stomach or other organ penetrates through the esophageal opening of the diaphragm into the mediastinum (Figure 2).
Complaints with esophageal hernia
The most common complaint with hiatal hernia is heartburn.
. You can read more about heartburn here. Heartburn most often occurs at night or after eating while lying down; it often occurs after physical activity, especially in an inclined position. Sometimes heartburn is accompanied by chest pain. Most often, relief from this condition comes from taking antacids, such as reni, or drugs that reduce the production of hydrochloric acid in the stomach, such as omeprazole.
The next common symptom of this disease is pain
. It is of a burning nature, localized behind the sternum, and radiates to the right shoulder. The pain intensifies most often after eating or lying down. Sometimes it is accompanied by heart rhythm disturbances. Most often, the pain goes away after belching, or if the patient gets up and walks around. Sometimes pain in people with a hiatal hernia is confused with pain in the heart, especially since with hiatal hernia pain is often accompanied by arrhythmia. Pain is most often relieved by antispasmodics, no-spa, etc.
Another complaint among patients is belching
. Belching occurs with both food debris and air. Sometimes it is uncontrollable and occurs without reference to food intake. Often, this lack of control and unpredictability of the occurrence of the latter is the main reason for surgical treatment of patients with hiatal hernia.
Regurgitation
- throwing food into the oral cavity while lying down or bending over. This complaint is relatively uncommon and occurs more often with large hernias.
Dysphagia
- difficulty passing food through the esophagus, develops at the stage of complications of the hiatal hernia. Dysphagia is caused either by an inflammatory process in the walls of the esophagus, or by a cicatricial stricture (narrowing) of the esophagus. Dysphagia requires hospital treatment
Extraesophageal manifestations of hiatal hernia are also distinguished. The most common of this group of complaints is cough.
. Often a cough accompanies the patient for years. It occurs more often in a lying position or when bending over, after eating. The cough is accompanied by a constant sore throat.
The second most common extraesophageal complaint is arrhythmia
. Most often, arrhythmia occurs with a large hiatal hernia, when most of the stomach is in the chest. In this case, the arrhythmia is associated with eating or bending, or occurs in a lying position. Typically, when examining such patients, cardiologists do not find heart pathology. Another manifestation of hiatal hernia is chronic diseases of the ENT organs, pharyngitis and laryngitis. The connection between laryngitis or pharyngitis and the hiatal hernia can be confirmed or refuted using daily pH measurements of the esophagus.
In addition, the consequence of a hiatal hernia can be dental damage, hoarseness, bronchitis, and bronchial asthma.
Gymnastics
For hiatal hernia, physical therapy is recommended. The following exercises help a lot:
- Lie on your side and rest your head on the cushion. Inhale deeply and inflate your stomach as much as possible, then exhale slowly and relax. Repeat 4-5 times.
- Get on your knees, straighten your back, inhale and slowly bend to the right, exhale and return to the starting position, repeat the exercise 6-7 times.
- Lie on your back. Breathing is even and calm. Slowly turn to your left and then to your right side, trying not to lose your breath.
Course of hiatal hernia
HH is a very common disease. As I already wrote, up to 40% of the world's population have this disease, but most of them do not even suspect it. Problems begin when the sphincter between the esophagus and stomach stops working and the contents of the latter enter the esophagus. Or if the hernia of the PAD reaches a large size and causes complications associated with neighboring organs (arrhythmias, pneumonia, etc.). In most cases, with proper treatment, the course of the disease is favorable, and conservative therapy is sufficient. Therapy is aimed at reducing the reflux of gastric contents into the esophagus, relieving inflammation, and normalizing gastrointestinal motility. If conservative therapy is not effective, surgical intervention must be resorted to.
Postoperative period
In cases of uncomplicated course of the disease and successful laparoscopic surgery, postoperative management of patients does not go beyond standard measures (pain relief according to indications, antibiotic prophylaxis during surgery and on the 1st day after it, nutrition with liquid food from the 1st day, removal of safety drainage through 12-24 hours). The duration of hospitalization is on average from 2 to 5 days.
If complications develop, appropriate therapy is provided. To evaluate the results of treatment, it is recommended after 3-6 months. perform gastric X-ray, endoscopy and pH monitoring.
Complications of hiatal hernia
Erosion and ulcers of the esophagus occur in 7 - 9% of cases in patients with hiatal hernia. This complication is associated with the aggressive action of gastric juice, which enters the esophageal mucosa. Usually the presence of ulcers and erosions is accompanied by the most severe complaints of patients. The danger of an ulcer is that if not treated correctly, a scar may form at the site of the ulcer, which in turn can lead to obstruction of the esophagus. In the presence of multiple erosions, chronic anemia may develop. The presence of an ulcer in the esophagus is an indication for surgery.
Bleeding and anemia with hiatal hernia occur in 11 - 20% of cases. Bleeding most often occurs due to vomiting, for example after poisoning. Such bleeding can be quite massive and require emergency hospitalization. Bleeding can be manifested by vomiting blood, or so-called coffee grounds, dark coffee-colored contents. Sometimes bleeding may appear as black, tarry stool. In case of repeated episodes of bleeding, surgical treatment is indicated.
Anemia occurs in two cases. The first is chronic minor blood loss against the background of the presence of multiple erosions of the esophageal mucosa. This bleeding occurs periodically and goes unnoticed, and can continue for months. The second reason is a violation of iron absorption against the background of inflammatory changes in the stomach. This anemia is called iron deficiency and develops when most of the stomach is in the chest. Anemia manifests itself as severe weakness.
Cicatricial stricture of the esophagus. With a long-term inflammatory process in the wall of the esophagus against the background of the hiatal hernia, scars are formed that narrow the lumen of the esophagus. A stricture appears, a disruption in the passage of food through the esophagus. This complication is manifested not by the ability to eat, first with solid food, but as the process progresses, with liquid
Incarcerated hiatal hernia. A very rare complication, but extremely dangerous, which in the absence of qualified medical care leads to death. This complication is manifested by the sudden appearance of severe bursting pain in the chest, a feeling of fullness. Patients constantly try to induce belching, which is either impossible or does not bring relief. This complication requires emergency surgery.
To summarize, I would like to repeat that with proper treatment, complications of the hiatal hernia develop quite rarely.
Diagnosis of hiatal hernia
The main role in diagnosis is played by X-ray examination with barium and gastroscopy.
X-rays are performed on an empty stomach using a barium contrast solution. The doctor monitors the passage of contrast through the esophagus and stomach on the X-ray machine screen. Thanks to X-ray examination, it is possible to identify the size of the hernia, the presence or absence of reflux of gastric contents into the esophagus, the presence or absence of disturbances in the passage of contrast through the esophagus and stomach.
Gastroscopy allows you to assess the condition of the esophageal mucosa, the presence or absence of inflammation, erosions, ulcers, and the presence of narrowing. In the vast majority of cases, these two studies are sufficient to make the correct diagnosis. In some cases, a CT scan is performed to evaluate the presence or absence of a hiatal hernia and its size. If there are non-esophageal manifestations or an unclear clinical picture, daily pH measurements are performed. A thin probe is installed into the lumen of the esophagus for 24 hours, which records the reflux of gastric contents into the esophagus, making it possible to identify the connection between complaints and reflux of gastric contents.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a gastroenterologist (primary) | 4 200 |
| Fluoroscopy and radiography of the esophagus | 2 600 |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Treatment of hiatal hernia
In the vast majority of cases, conservative therapy is carried out, which in fact is symptomatic and is aimed at improving the well-being of patients and preventing the development of complications. The main cause of complaints from patients is the reflux of aggressive gastric contents into the esophagus. Therefore, proton pump inhibitors (esomeprazole, Nexium, etc.) are prescribed. This is a group of drugs that reduce the acidity of gastric juice, thereby minimizing the damaging effect on the esophageal mucosa. Enveloping drugs in the form of suspensions are also used, such as Gaviscon, Maolox, Almagel. These drugs effectively reduce the acidity of gastric juice and, by enveloping the walls of the esophagus, protect them from reflux. And the third group of drugs are prokinetics (Motilium, Ganaton). These are medications that improve and normalize the motility of the esophagus and stomach, thereby reducing the frequency of reflux.
This therapy leads to improved well-being and quality of life. Unfortunately, up to 80% of patients experience a relapse of complaints immediately after stopping taking the drugs and therefore have to take them constantly. Complete removal of a hiatal hernia is only possible through surgery. You can read about surgical treatment of hiatal hernia here
Author: Ph.D. Siyukhov R.Sh.