What it is
Lysate (from the Greek “lysis” - “decomposition”) is a suspension that is formed due to the destruction of bacterial cells. It includes particles of bacteriophages and fragments of the walls of microorganisms that are not pathogenic and, accordingly, do not pose an infectious risk to the body.
The “debris” retains a specific structure and receptors that are recognized by the immune system as hostile. At the same time, the body concentrates its defenses to resist the “onslaught.” As a result, a selective immune response is formed against the strains of bacteria that were used in the production of the lysate.
All bacterial lysates are polyvalent, that is, they contain several strains of microorganisms. Typically, these are the pathogens that most often cause infections.
Each strain of bacteria is cultivated in vitro, inactivated and lysed either chemically or mechanically, and then lyophilized - “cold dried”. After this, the resulting lysates are mixed in certain proportions [1].
Uro-Vaxom bacterial lysate
Uro-Vaxom is an immunostimulating agent used to treat pathologies of the genitourinary system. The drug is prescribed for combination with other drugs to block urinary tract infections and cystitis. Uro-Vaxom is often prescribed for preventive purposes in the presence of chronic pathologies. The drug is not used during pregnancy and breastfeeding. It is allowed to carry out therapy with bacterial lysate from the age of four.
Uro-Vaxom in rare cases leads to the development of adverse reactions.
This can happen if the wrong dosage is selected or if there is hypersensitivity to the active ingredient.
Side symptoms include: nausea, vomiting, itching, severe headache, diarrhea and stomach upsets. It is prohibited to carry out therapy within 2 weeks after using immunobiological products. It is allowed to combine Uro-Vaxom with antibiotics, anti-inflammatory and antimicrobial agents.
Everything is not so clear
In 2021, Italian scientists analyzed 170 articles on lysates in Pubmed, the largest English-language text database of medical and biological publications. They concluded that many of the properties and features of the action of drugs in this group have not yet been sufficiently studied, and the quality of the research itself is not satisfactory. According to the authors of the analysis, further good quality studies are needed to more fully explore the capabilities of the lysates [2].
Thus, the effectiveness of bacterial lysates cannot be called obvious from the point of view of evidence-based medicine.
However, they are prescribed to stimulate the immune response in various diseases, including urology (for chronic cystitis), gynecology (to restore microflora) and pulmonology (to prevent exacerbations of COPD). But bacterial lysates have gained the greatest popularity as drugs for the treatment and prevention of respiratory tract infections.
The main hypothesis explaining the mechanism of action of lysates involves enhancing the immune response due to stimulation of the cellular and humoral components. It is believed that the effect of lysates on the body is physiological, since they naturally stimulate their own reactions to antigen and exhibit a complex immunotropic effect [4]:
- They increase the production of specific antibodies to pathogens, the lysates of which are included in the drug.
- They enhance the production of anti-inflammatory cytokines (interleukins and others).
- Stimulate phagocytosis.
- Increase the synthesis of interferon and other components of the immune response.
Local lysates, when they come into contact with the mucous membrane of the upper respiratory tract, form a thin protective layer. Their action is based on increased synthesis of IgA and decreased production of IgE, which is associated with hypersensitivity and allergization [5]. At the same time, local drugs, as well as systemic ones, act on factors of specific and nonspecific immunity.
Bacterial lysate Ismigen
Ismigen is a combined medicinal product of bacterial origin that has an immunostimulating and vaccinating effect. The drug affects various parts of human immunity. It helps stimulate cellular, humoral and systemic responses. As a result of the use of Ismigen, the patient’s recovery in acute viral pathologies is accelerated: cough disappears, runny nose decreases, fever is blocked. Indications for use:
- bronchitis;
- rhinitis;
- sinusitis;
- flu;
- laryngitis;
- tonsillitis.
Ismigen is prohibited for use by pregnant women, as well as by patients who are breastfeeding. The drug is used to treat children from the age of three. Contraindications include a tendency to allergies, hypersensitivity to the active component in the composition. As adverse reactions, the patient may experience symptoms such as urticaria, folliculitis, acute laryngitis. Ismigen can be used in complex therapy with other anti-inflammatory drugs, including antibiotics and immunostimulants.
We recommend topical lysates
Topical bacterial lysates belong to the OTC group. Their range includes only 2 drugs, which differ significantly in both composition and indications.
Complex preparation of bacterial lysates “IRS 19”
Client Requests:
- drugs for the prevention of ARVI;
- drugs for the treatment of upper respiratory tract diseases of a viral and infectious nature (including influenza and other acute respiratory viral infections);
- means for restoring local immunity after acute respiratory viral infections.
Properties
The mixture of lysates included in IRS 19 is used in the form of an intranasal spray in 35 countries around the world [5]. The drug contains a combination of lysates of the most common pathogens of bacterial infections of the respiratory tract, including pneumoniae streptococci, Haemophilus influenzae, Staphylococcus aureus, Moraxella, Enterococci and some others.
Interestingly, the composition of the drug is periodically updated and changed taking into account the predominance of the main pathogens of diseases of the ENT organs and respiratory tract [5].
"IRS 19" can be used for acute and chronic diseases, as well as as a means for the prevention of infections and during the recovery period after an illness.
How to use?
The medicine is used intranasally, the dose and course depend on the purpose (prevention or treatment) and the age of the patient.
What should the client pay attention to?
At the beginning of treatment, sneezing and increased nasal discharge may occur. Usually this effect is short-term. If the reaction becomes severe, it is recommended to reduce the frequency of administration of the drug or completely discontinue it [6].
"Imudon"
Client Requests:
- drugs for the treatment and prevention of pharyngitis, tonsillitis, periodontal disease, periodontitis, stomatitis, gingivitis;
- means for preventing infection after tooth extraction;
- a drug for the treatment of ulcerations caused by dentures.
Properties
The drug is a mixture of lysates of bacteria that most often cause inflammatory processes in the oral cavity and pharynx, including several strains of lactobacilli, Staphylococcus aureus, Escherichia coli, Klebsiella, and Candida fungi.
How to use?
"Imudon" is used to treat adults and children over 3 years of age. The dose and course of treatment depend on the indication and age. The tablets dissolve in the mouth without chewing.
What should the client pay attention to?
Within an hour after taking the drug, you should not eat or drink water [7].
General information
Products based on bacterial lysates are similar in their principle of action to standardized vaccination. That is, their intake stimulates the natural protective functions of the human body. Most modern bacterial lysates are most often produced on the basis of a mixture of different bacteria: streptococci, staphylococci, as well as pathogens that provoke the development of ENT pathologies. The advantages of such medicinal products include:
- Low likelihood of developing adverse reactions. The exception is if the patient is allergic to the active ingredient in the product.
- Treatment effectiveness. With complex therapy with other drugs, recovery occurs faster than without the use of bacterial lysates.
- Preventive action. Medicines have a preventive effect, preventing the likelihood of becoming chronic.
These medications also have a negative side. Bacterial lysates do not treat viral infections on their own; they only work in tandem with other antiviral products and immune-stimulating agents. Below is a list of the best bacterial lysates for children and adults that stimulate the immune system.
Systemic lysates: working from the inside
Systemic bacterial lysates, according to some experts, are more active than local ones, since they provide longer and stronger contact with the mucous membranes (they are not washed off by saliva) [8]. The only OTC representative of this group today is the drug Ismigen.
"Ismigen"
Client Requests:
- drugs for the treatment of infections of the upper and lower respiratory tract, ENT organs (bronchitis, tonsillitis, pharyngitis, laryngitis, rhinitis, sinusitis, otitis, etc.);
- means for the prevention of exacerbations of recurrent infections of the upper and lower respiratory tract, chronic bronchitis.
Properties
“Ismigen” is a bacterial lysate obtained mechanically and is highly immunogenic [9]. The product contains 14 strains of 8 types of inactivated pathogenic bacteria, the most common causative agents of upper and lower respiratory tract infections, including Staphylococcus aureus, Streptococcus pyogenes, Streptococcus pneumoniae, Klebsiella, Haemophilus influenzae, Moraxella and others. Its cardinal difference from other systemic lysates is the sublingual (sublingual) route of administration.
The drug has been extensively studied: data from 15 randomized studies involving more than 2,500 patients confirm that taking Ismigen can reduce the number of respiratory infections compared to placebo in children and adults [9].
How to use?
The drug is used for the treatment and prevention of infections in adults and children over 3 years of age. The dosage for treatment and prevention is the same - 1 tablet per day. The course of treatment lasts at least 10 days, the course of prophylaxis is three cycles of 10 days at 20-day intervals [10].
What should the client pay attention to?
Sublingual tablets are taken on an empty stomach. They are kept under the tongue until completely dissolved, without dissolving or chewing.
Imudon for viral infections
Imudon is a lyophilisate that has an immunostimulating effect and is used for topical use in dentistry and otorhinolaryngology. The medicinal product enhances the production of lysozyme and promotes the activation of phagocytosis. Imudon also increases the production of secretory immunoglobulin. Indications for drug therapy are the following diseases:
- pharyngitis;
- laryngitis;
- chronic tonsillitis;
- periodontal disease;
- ulcerative gingivitis;
- dysbacteriosis of the oral cavity;
- conditions after tooth extraction.
Imudon is not recommended for use during pregnancy and lactation. The drug is used in childhood (from 3 years), but in a reduced dosage. Contraindications include a tendency to allergies and intolerance to the active substance. The studies did not reveal any negative consequences when combining Imudon with other antiviral and immunostimulating drugs.
Immunomodulatory therapy: questions and answers. Focus on bacterial lysates (OM-85)
A class of drugs widely used in clinical practice are immunomodulatory drugs. However, a lack of understanding of the mechanisms of action, a low degree of awareness of the direction of the impact on immunopathology of representatives of different classes of immunomodulators gives rise to myths and rumors about ineffectiveness, danger, “counterfeits”... The current situation ultimately leads to the indiscriminate, unjustified use of modern drugs from the group of immunomodulatory agents, which are becoming better In cases, they are absolutely useless, and in the worst case, they can also cause a number of side effects. To select an individual treatment trajectory when there are indications for the use of immunomodulators, it is fundamentally important to follow the principles of rational pharmacotherapy:
1) sufficient level of evidence of effectiveness; 2) sufficient level of evidence of safety; 3) clear points of application of the drug’s action on the immune system; 4) ease of use (compliance).
When chosen correctly, immunomodulatory therapy demonstrates high clinical effectiveness, acting selectively on the defect of the immune system without changing its normal parameters.
Immunomodulator OM-85. General provisions
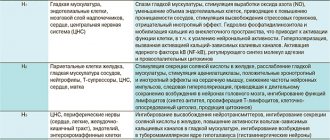
Systemic mechanisms that initiate the innate and adaptive immune systems determine the effectiveness of the oral standardized lyophilisate of lysates of 8 species of bacteria OM-85 (Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus viridans, Streptococcus pyogenes, Klebsiella pneumoniae, Klebsiella ozaenae, Staphylococcus aureus, Moraxella catarrhalis) [1 ] . The initiation mechanism begins with the delivery of bacterial antigens (AGs) and microbe-associated molecular patterns (MAMPs) to the primary targets, the intestinal M-cells of Peyer's patches, which deliver the Ags and patterns and activate dendritic cells. Next comes the activation of T and B lymphocytes either in the plaques themselves or in the mesenteric lymph nodes. Activation of adaptive immunity leads to an increase in the production of secretory immunoglobulin A (sIgA) not only in the gastrointestinal tract, but also in the upper and lower respiratory tract. This phenomenon is described as mucosal solidarity. Oral bacterial lysates, in addition to stimulating mucosal sIgA-mediated adaptive immunity in the respiratory tract, increase the level of systemically circulating antibodies of various isotypes to the corresponding bacterial antigens. After taking OM-85, a much broader response is formed, and not only in relation to pathogens, the lysates of which are part of this immunomodulator. OM-85, during the first hours after oral administration, stimulates the innate components of the immune response - the activity of macrophages, natural killer cells, the synthesis of alpha, beta and gamma interferons [22, 23], the action of which is directed against any pathogens, regardless of their taxonomic affiliation [1] , as a result of which epigenetic reprogramming of innate immune cells occurs [2] and stable tolerance is created towards various viral and bacterial infections.
The high level and degree of evidence for the effectiveness of OM-85 in relation to the number and severity of respiratory infections in adults and children has been documented in many clinical trials and meta-analyses [3–6]. In the light of the criteria for rational pharmacotherapy, there is no doubt about the high effectiveness of OM-85 as one of the most well-studied immunomodulators. The feasibility of choosing this drug for the treatment and prevention of respiratory infections, as well as for preventing/reducing the severity of exacerbations of chronic lung diseases is determined by its effective composition, disclosed and understandable molecular mechanisms of action, irrefutable evidence base and physiological influence on the course of the anti-infectious immune response [3].
However, despite many years of successful experience in using OM-85, there are a number of pressing issues that trouble the minds of practical healthcare and form opposing opinions.
Is it advisable to prescribe bacterial lysates in the treatment of acute respiratory infections and can additional administration of an immunostimulant in ARI “overstimulate” the immune system?
The erroneous terminology “stimulate”, “raise” is quite widely used in relation to the prescription of immunomodulatory therapy for various disorders of the immune system by both patients and doctors. It is also customary to talk about “reduced immunity”, without going into details at all, that each time we are talking about various defects in the immune system and only an understanding of the pathology can help in the strategy for choosing an effective immunomodulator.
So, why is it really advisable to use OM-85 for acute respiratory infections?
OM-85 stimulates the innate immune system during the first hours after administration, triggering a response against any pathogens [1]. The validity of the use of OM-85 in the treatment of acute respiratory diseases (ARI) can be confirmed by the fact that many living pathogens are able to evade the immune response and even suppress the immune response [24, 25].
The use of OM-85 in the acute period of infection of the upper and lower respiratory tract is relevant when rapid stimulation of anti-infective defense is necessary. The advisability of prescribing OM-85 in the first hours of acute respiratory infections is also justified by the fact that the starting capabilities of the adaptive (antibody-dependent) components of the pharmacological action of OM-85 will begin to work 4–5 days from the start of administration, which will coincide with the stage of the disease, when the risk of developing secondary bacterial infections [3].
Action of bacterial lysates
The mechanism of action of OM-85, described in the literature, is based on stimulation of dendritic cells through TLR2, TLR4 [7, 8], whose task is to capture and destroy pathogens, as well as present their antigens to lymphocytes. Dendritic cells, after stimulation, produce IFN-α and IFN-β, which have direct virostatic activity, and promote increased secretion of IFN-γ and IL-2 [10], thereby stimulating cellular antiviral responses. In addition, OM-85 promotes the production of antibodies that neutralize viruses, in particular influenza viruses [11]. The properties of OM-85 are described to suppress the replication of rhinoviruses in the culture of bronchial epithelial cells and increase the viability of infected cells by reducing the expression of ICAM-1 intercellular adhesion molecules by infected epithelial cells, which rhinovirus uses to penetrate the cell [12].
Of the described immunological effects, the impact of OM-85 on the mucosal immune system is extremely important by increasing the concentration of IgA, IgG, IFN-γ and hBD-1 (an antimicrobial peptide in epithelial tissues, which plays an important role in the formation of resistance to viruses, bacteria on the surface of mucous membranes membranes) and a decrease in the content of IL-4 and NF-κB in the blood serum [13].
Thus, data from both preclinical and clinical studies demonstrate the ability of the bacterial lysate OM-85 to increase the body's resistance to respiratory viruses.
How often can OM-85 be prescribed within one year both for the purpose of prevention and in the complex treatment of acute respiratory infections?
On the issue of duration and frequency of use of immunomodulatory therapy, during numerous discussions in the professional community, a confident opinion has emerged that leaves the decision of this issue up to the attending physician, however, taking into account the provisions of the instructions for the drug. The effectiveness of use in a preventive regimen has been proven by numerous clinical studies. According to research, the use of OM-85 for a course of 3 months leads to an increase in the level of IgA in saliva and persists for at least 100 days, increased levels of IgG and IgM in the blood persist for at least 5 months, which makes it possible to recommend a preventive course of an average of 1 once every six months [26]. Prescription of the drug in the complex therapy of acute respiratory infections (ARI) is possible at any stage of the disease and is aimed at reducing the duration of the disease, the severity of symptoms and the risk of bacterial infection. The minimum course of admission is 10 days. Then you can continue using OM-85 as a prophylactic course.
The following statement, which also applies to OM-85, is extremely important: after repeated use of the immunomodulator, its effectiveness increases rather than decreases (from the principles of using immunomodulatory therapy).
The purpose of including OM-85 in the treatment regimen for acute respiratory infections in a child and the category of patients for whom such a prescription is justified
Immunomodulatory therapy OM-85 is of particular relevance in the group of immunocompromised patients due to the existing disturbances in the functioning of mucosal immunity, the weakness of the “barriers” and the colonization of the mucous membranes of the respiratory tract by opportunistic and pathogenic microorganisms.
The main purposes of prescribing OM-85 include restoring impaired parameters of mucosal immunity, reducing the pharmacological burden on the patient, shortening the duration of the disease, and reducing the risk of complications of ARI. The expected results are accelerated clinical recovery, effective elimination of the infectious agent, prevention of relapses and complications of infection, preserved quality of life in the immunocompromised patient and his family.
Can the use of immunomodulators in children with allergies lead to exacerbation/worsening of the allergic disease?
According to the latest literature data, the number of people suffering from allergopathology in different regions ranges from 15% to 40% of the population. On average, every third person on the planet suffers from some type of allergy. Therefore, the safety aspect of administering bacterial lysates in this group of patients is extremely important. The literature describes the ability of systemic bacterial lysates to increase not only the specific immune response, but also to activate nonspecific protection, which allows them to be successfully used in a group of children with allergic pathology. Prophylactic administration of bacterial lysates reduces the percentage of complications in “complex” patients with allergies, reliably promotes clinical improvement of the underlying disease, and reduces the need for basic pharmacotherapy. In this case, there is an increase in the level of IFN-γ, a decrease in total IgE and circulating immune complexes in the blood. It has been established that in children with allergies, the Th1/Th2 ratio significantly increases, which is an important fact that makes it possible to control allergic inflammation [14, 15].
Which method of obtaining bacterial lysates—mechanical or chemical (Broncho-munal®)—allows us to obtain a drug with greater efficiency and tolerability?
Bacterial lysates are obtained by mechanical or chemical lysis, followed by lyophilization and mixing in specified proportions. Chemical lysis involves denaturation of the cell wall. The mechanical method involves destroying the cell wall using high pressure or ultrasound without chemicals, which, according to some authors, better preserves the immunogenicity of bacterial lysates [16]. However, there is no convincing evidence of the benefits of bacterial lysate obtained chemically or mechanically. On the contrary, the high evidence base of category A for the drugs OM-85 (Broncho-munal®, Broncho-Vaxom®) confirms the high immunogenicity of the drug and its effective work with both the innate immune system and adaptive immunity [1–13].
Is an immunomodulator necessary for acute respiratory infections or is it sufficient to prescribe antiviral drugs in the case of a viral infection and antibacterial drugs in the case of a bacterial infection?
Features of the etiopathogenetic structure of acute respiratory infections at the present stage is the participation of viral-bacterial association in the formation of pathology. Today, up to 200 pathogens are considered as causative agents of acute respiratory infections [17, 18], so it is extremely difficult to choose an effective antiviral drug, and besides, antibacterial agents are not always used in the treatment of acute respiratory infections. The main blow of pathogens in acute respiratory infections is delivered precisely by the mucosal immune system, and the very fact of the development of respiratory pathology depends on its viability. Considering the interest of mucosal immunity and the weakness of barrier structures that develops during acute respiratory infections, it is extremely important for the patient’s recovery to restore the impaired barrier functions of the mucosal immune system. The only class of drugs that can restore impaired functions of the immune system are immunomodulators, and one of the effective drugs that take part in the correction of the pathology of mucosal immunity are bacterial lysates. It should be noted that the use of antiviral drugs in the treatment of acute respiratory infections is effective when prescribed in a timely manner. But unfortunately. the advisability of prescribing this group of drugs is limited to 24–48 hours from the moment of infection [27].
About polypharmacy
When building an individual treatment trajectory for a patient with acute respiratory infections, it is necessary to use a number of therapeutic interventions that fit into the modern strategy for treating acute respiratory infections. Along with symptomatic, pathogenetic, etiotropic therapy, a necessary and effective component of complex treatment is immunomodulatory therapy, which, with a timely approach, can significantly reduce the overall pharmacological burden on a patient with acute respiratory infections, reduce the duration of an acute respiratory infection episode, prevent the development of complications and improve the patient’s quality of life [17–21] . OM-85 has been shown to help reduce antibiotic prescription, which can be considered a strong argument for OM-85 in reducing medication burden [28]. Bacterial lysates, which have a high evidence base (OM-85 includes them), are one of the groups of immunomodulatory drugs that firmly occupy a leading position in the treatment of acute respiratory infections.
Difference in indications between bacterial lysates and oral vaccines
If we talk about vaccination, then first of all I would like to note its main objectives: targeting the formation of a specific immune response against specific pathogens, along with a preventive effect. The use of vaccination is not possible for therapeutic or curative purposes during the height of the disease. Returning to the huge spectrum of pathogens of acute respiratory infections, it is obviously impossible to create a specific response against all pathogens. Despite the highest effectiveness of vaccine prevention, vaccines have not been created against most respiratory pathogens. This situation is based on the high variability characteristic of respiratory pathogens, along with the short duration and instability of specific immunity. Since the purpose of vaccination is prevention, to obtain a more predictable preventive effect, vaccination is not recommended for acute diseases. Unlike vaccines, the use of OM-85 in complex treatment has a therapeutic purpose, with the aim of reducing the duration of the disease and reducing the risk of bacterial complications. Considering the mechanism of action of OM-85, its effect on factors of innate and acquired immunity, the possibility and effectiveness of use not only for the purpose of prevention, but also in the acute period and during the recovery period, it can be argued that OM-85 is an immunotropic agent with direct indications for use in complex therapy of acute respiratory infections.
conclusions
OM-85 is the most studied drug among immunomodulators, used for more than 30 years. This allows us to expect predictable efficiency and safety from OM-85. OM-85 increases immunity against both viruses and bacteria, which justifies the advisability of using the drug both in schemes for the prevention of recurrent respiratory infections and in treatment schemes for ARI.
Literature
- De Benedetto F., Sevieri G. Prevention of respiratory tract infections with bacterial lysate OM-85 bronchomunal in children and adults: a state of the art // Multidisciplinary Respiratory Medicine. 2013; 8 (1): Art. 33. DOI: 10.1186/2049–6958–8–33.
- Kalyuzhin O.V. The phenomenon of trained immunity and the mechanisms of action of nonspecific immunomodulators // Russian Journal of Allergology. 2015. No. 4. pp. 45–51.
- Kalyuzhin O.V. OM-85 in the prevention/treatment of respiratory infections and exacerbations of chronic lung diseases: selection criteria, mechanisms and evidence // Attending Physician. 2021, No. 3.
- De Benedetto F., Sevieri G. Prevention of respiratory tract infections with bacterial lysate OM-85 bronchomunal in children and adults: a state of the art // Multidisciplinary Respiratory Medicine. 2013; 8 (1): Art. 33. DOI: 10.1186/2049–6958–8–33.
- Schaad UB OM-85 BV, an immunostimulant in pediatric recurrent respiratory tract infections: a systematic review // World J. Pediatr. 2010; 6:5–12. DOI: 10.1007/s12519–010–0001x.
- Del-Rio-Navarro BE, Espinosa-Rosales FJ, Flenady V., Sienra-Mongen JJL Immunostimulants for preventing respiratory tract infection in children // Evid. Based Child Health. 2012; 7:629–717. DOI: 10.1002/ebch.1833.31.
- Yin J., Xu B., Zeng X., Shen K. Broncho-Vaxom in pediatric recurrent respiratory tract infections: A systematic review and meta-analysis // Int. Immunopharmacol. 2021 Jan; 54: 198–209. DOI: 10.1016/j.intimp.2017.10.032.
- Parola C., Salogni L., Vaira X. et al. Selective Activation of Human Dendritic Cells by OM-85 through a NF-kB and MAPK Dependent Pathway // PLoS ONE. 2013; 8(12):e82867. DOI: 10.1371/journal.pone.0082867.
- Zelle-Rieser C., Ramoner R., Bartsch G., Thurnher M. A clinically approved oral vaccine against pneumotropic bacteria induces the terminal maturation of CD83+ immunostimulatory dendritic cells // Immunol. Lett. 2001; 76(1):63–67.
- Huber M., Mossmann H., Bessler WG Th-1 orientated immunological properties of the bacterial extract OM-85 BV // Eur. J. Med. Res. 2005; 10 (5): 209–217.
- Pasquali C., Salami O., Taneja M. et al. Enhanced Mucosal Antibody Production and Protection against Respiratory Infections Following an Orally Administered Bacterial Extract // Frontiers in Medicine. 2014; 1: 41. DOI: 10.3389/fmed.2014.00041.
- Roth M., Pasquali C., Stolz D., Tamm M. Broncho Vaxom (OM-85) modulates rhinovirus docking proteins on human airway epithelial cells via Erk1/2 mitogen activated protein kinase and cAMP // PLoS ONE. 2017; 12 (11): e0188010. DOI: 10.1371/journal.pone.0188010.
- Liu YW, Dong SH, Zhan GY, Tan HZ, Peng YQ, Wei F. Analysis of the effect of bacterial lysate and the immunologic mechanism in treating infant bronchiolitis // Eur. Rev. Med.Pharmacol. Sci. 2017; 21(14):3332–3336.
- Zaitseva O. N. Recurrent respiratory infections: can it be prevented? // Pediatrics. 2015. T. 94, 32, p. 185–192.
- Guseva E. D., Fayzulina R. M. Features of mucosal immunity in children with allergic rhinitis // Bulletin of Otorhinolaryngology. 2012, no. 6, p. 33–35.
- Ryazantsev S.V., Konoplev O.I., Sapova K.I. Bacterial lysates in the treatment of diseases of the respiratory tract and ENT organs // RMJ. 2015, no. 23, p. 1387–1390.
- Kalyuzhin O. V. Acute respiratory viral infections: modern challenges, antiviral response, immunoprophylaxis and immunotherapy. M.: Medical Information Agency, 2014. 144 p.
- Tataurshchikova N. S. Acute respiratory disease in a patient with allergies, key participants and problems: what to do and what to do // Farmateka. 2021, no. 18, p. 23–29.
- Tataurshchikova N. S., Sepiashvili R. I. Modern approaches to the use of immunomodulators in allergy practice. Educational and methodological manual. M., 2012. P. 40.
- Sepiashvili R.I. Classification and basic principles of using immunomodulatory drugs in clinical practice // Allergology and Immunology. 2002. T. 3, No. 3, p. 325–331.
- Khaitov R. M., Pinegin B. V. Modern immunomodulators. Classification, mechanism of action // Russian allergological journal. 2005. No. 4. P. 30–43.
- Kearney SC, Dziekiewicz M., Feleszko W. Immunoregulatory and immunostimulatory responses of bacterial lysates in respiratory infections and asthma // Annals of Allergy, Asthma & Immunology. 2015. T. 114. No. 5. pp. 364–369.
- Esposito S. et al. Nonspecific immunomodulators for recurrent respiratory tract infections, wheezing and asthma in children: a systematic review of mechanistic and clinical evidence // Current opinion in allergy and clinical immunology. 2021. Vol. 18. No. 3. pp. 198–209.
- Avondt KV et al. Bacterial Immune Evasion through Manipulation of Host Inhibitory Immune Signaling // PLoS Pathog. 2015, Mar; 11(3).
- Valle J., Latasa C., Gil C., Toledo-Arana A., Solano C., Penadés JR et al. Bap, a Biofilm Matrix Protein of Staphylococcus aureus Prevents Cellular Internalization through Binding to GP96 Host Receptor // PLoS Pathogens. 2012, 8(8): e1002843. DOI: 10.1371/journal.ppat.1002843.
- Mauël J. Stimulation of immunoprotective mechanisms by OM-85 BV. A review of results from in vivo and in vitro studies // Respiration. 1994; 61. Suppl 1: 8–15.
- Baranov A. A., Lobzin Yu. V. Federal clinical guidelines for the provision of medical care to children with acute respiratory viral infection (acute nasopharyngitis), 2015.
- Gutiérrez-Tarango MD et al. Safety and efficacy of two courses of OM-85 in the prevention of respiratory tract infections in children during 12 months // Chest. 2001; 119, 1: 742–748.
RU1809883743
N. S. Tataurshchikova, Doctor of Medical Sciences, Professor
Federal State Autonomous Educational Institution of Higher Education RUDN University, Moscow
Contact Information
Immunomodulatory therapy: questions and answers. Focus on bacterial lysates (OM 85) / N. S. Tataurshchikova For citation: Attending physician No. 9/2018; Issue page numbers: 78-81 Tags: antibodies, innate immunity, stimulation, pathogens