Author:
Butriy Sergey Alexandrovich pediatrician
Quick transition Treatment of atopic dermatitis in children
Atopic dermatitis is a disease in which the skin becomes very itchy, irritated, red, dry, and uneven.
Atopic dermatitis is a common skin disease that is part of a group of skin diseases combined under the broader term “eczema.”
There are other types of eczema: nummular, dyshidrotic, etc. However, the terms “eczema” and “atopic dermatitis” are often used interchangeably.
As a rule, atopic dermatitis debuts in infancy (3–6 months) and occurs in 15–20% of children. Most often, its course is most severe in the first 1–3 years of life; as the child grows older, the severity of the disease decreases. Atopic dermatitis usually disappears by school age or puberty. However, in some people the disease can persist throughout their lives, occasionally worsening, or appearing constantly.
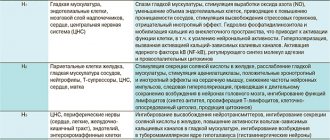
Pharmacodynamics and pharmacokinetics
Pharmacodynamics
An antihistamine (an active metabolite of loratadine ) has a long-lasting effect. Inhibits various reactions of allergic inflammation (release of pro-inflammatory cytokines, pro-inflammatory chemokines, production of superoxide anions, chemotaxis and adhesion of eosinophils, release of adhesion molecules, release of histamine, leukotriene C4, prostaglandin D2). Thus, it prevents the development and reduces the manifestations of allergic reactions. The drug has an antiexudative and antipruritic effect, reduces capillary permeability, relieves spasm of smooth muscles and tissue swelling.
The drug does not have a sedative effect and does not act on the central nervous system, does not affect psychomotor reactions. The effect of the drug, after oral administration, appears after 30 minutes and lasts throughout the day.
Pharmacokinetics
After oral administration, the drug is quickly and well absorbed into the gastrointestinal tract. In blood plasma it is determined after 30 minutes. Does not penetrate the BBB. There is no clinically significant accumulation when taking therapeutic doses. The maximum concentration in the blood is after 3 hours. Strong connection with blood proteins (85-87%). Metabolized in the liver to form desloratadine. A small portion (<2%) is excreted by the kidneys and (<7%) in the feces. The half-life is on average 27 hours.
Erius in the treatment of allergic skin diseases
The significant dynamics of the increase in the number of these diseases is due to a number of factors - environmental pollution, especially in industrialized countries, constant contact in everyday life and at work with a variety of chemicals (household chemicals, cosmetics, building materials, metals, synthetic materials for clothing and footwear) . The rise in the incidence of allergic dermatoses is undoubtedly facilitated by the use of a large number of medications, including vitamins and nutritional supplements, canned food and fast food. An important factor in the development of chronic allergic dermatoses is the pathology of the gastrointestinal tract. An equally important role is played by hereditary predisposition to allergies, especially in patients with atopic dermatitis. The urban population suffers from allergic dermatoses more often than the rural population. City dwellers are more susceptible to environmental pollution and more often experience a variety of stress due to the busy pace of life. The chronic course with frequent relapses, the insufficient effectiveness of existing methods of prevention and treatment, and the worsening course of the disease make the problem of allergic dermatoses one of the most pressing in modern medicine. To relieve allergic reactions, antihistamines play an important role, having the ability to bind H1-histamine receptors and block histamine activity. It is known that 11 histamine molecules are attached to one protein molecule. Protein-bound histamine is not active and does not cause an inflammatory response, but this bond is not stable and under the influence of various factors it is broken and leads to the formation of free histamine. An increase in its concentration in the body is carried out both by an IgE-dependent mechanism - immediate hypersensitivity, and as a result of non-immunological stimuli leading to increased activity of mast cells and basophils. In clinical practice, various antihistamines are widely used, which are divided into three groups. The first includes diphenhydramine, chloropyramine, promethazine, etc., which have both an antihistamine and a pronounced sedative effect and the ability to penetrate the blood-brain barrier with an effect on the receptor structures of the central nervous system. This property of the drugs, on the one hand, narrowed the range of their use due to side effects, and on the other hand, at one time ensured their attractiveness for skin itching, atopic dermatitis, eczema, lichen planus and other skin diseases due to its pronounced sedative effect. The price of these drugs also plays an important role for patients [7,10,14,15]. The second and third groups do not have the disadvantages of first-generation antihistamines. It included terfenadine, astemizole, acrivastine, ebastine, cetirizine, fexofenadine, loratadine and desloratadine [3,18,19]. It should be emphasized that terfenadine and astemizole were banned for use in Russia shortly after their registration due to the risk of cardiotoxic effects and fusiform tachycardia in patients [10]. A special place among these drugs is occupied by desloratadine (Erius) - a metabolite of loratadine, synthesized in 1998 and registered in Russia in 2001. Desloratadine (Erius) is a non-sedating, long-acting selective blocker of H1-histamine receptors, has remarkable properties, including the absence of influence on ECG indicators and potentiation of the effects of alcohol. The drug stabilizes mast cells and basophils, inhibits the formation and release of histamine, cytokines - PGD2, LTC4, IL-4, IL-6, IL-13, chemokines and suppresses the expression of adhesion molecules, stopping the migration of cells into target tissues and thereby providing anti-inflammatory action [16,20]. Desloratadine (Erius) inhibits the formation of eosinophilic spongiosis, reduces the chemotaxis and adhesion of these cells, slows down the production of superoxide radical by activated polymorphonuclear neutrophils, increasing anti-inflammatory and antiallergic activity. Desloratadine (Erius) has a number of advantages that significantly distinguish it from first-generation drugs, including high efficiency and safety, duration of action up to 24 hours, absence of sedation, tachyphylaxis, which makes it possible to use it once a day [15]. The wide range of therapeutic properties of the drug Erius allows clinicians to use it for various diseases of an allergic nature: from bronchial asthma, atopic vasomotor rhinitis, urticaria, to skin itching, eczema, atopic dermatitis and other skin diseases [1,2,4–6,9,13 , 16,17]. During a clinical study of the effectiveness of Erius, Korsunskaya I.M. [11] divided patients into 3 groups. The first included patients with photodermatitis, solar eczema and solar urticaria, the second - with acute and chronic recurrent urticaria, the third - patients with eczema and atopic dermatitis. All patients with an acute course of the Erius process were prescribed 5 mg per day for 2 weeks; in case of a chronic course, the duration of therapy was 3 weeks. In all cases, the therapy was effective, the positive effect was achieved within 3–7 days. In the first and second groups, clinical recovery was confirmed 3 months after the end of therapy; in the third group, patients with eczema and atopic dermatitis showed significant improvement in the form of absence of itching, reduction of erythema, signs of improvement in the clinical picture were observed throughout the entire observation period. Serious clinical studies to study the effectiveness of Erius were conducted by N.V. Kungurov. et al. [12] in patients with atopic dermatitis, eczema and malignant lymphomas. Atopic dermatitis was characterized by a torpid course, a large area of skin damage, accompanied by severe itching, erythema, severe lichenification, and white dermographism. In patients with eczema, the lesions were localized on the extremities and were accompanied by bright erythema, weeping, severe itching and red dermographism. The authors showed that in atopic dermatitis and eczema, along with histamine, pruritogenic effects were supported by an increased content in the body of other biologically active substances (serotonin, bradykinin, collectrein, poroteases, prostaglandins, leukotrienes and eicosanoids). Factors that provoked an exacerbation of eczema were diet disorders, stress, contact with detergents and physical activity. Therapy with Erius 5 mg per day in combination with external non-hormonal therapy gave positive results, characterized by a decrease in itching lasting from 6 to 24 hours, recorded in 90% of patients. The use of Erius in 10 patients with malignant lymphomas and mycosis fungoides, 5 mg in the daytime or before bed with a 2-week course, led to a significant reduction in itching, a decrease in erythema, and improved sleep in 90% of patients, in the absence of clinical dynamics of proliferative elements. Thus, an analysis of the literature shows that Erius has a broad therapeutic antiallergic, anti-inflammatory, antihistamine, antiserotonin effect, blocking cytokines, homokines, proteases and other biologically active substances. No adverse reactions or toxic effects have been reported with the use of Erius. Erius can be used for acute and chronic skin diseases, both in the form of mono- and complex therapy. Literature 1. Bulgakova V.A., Balabolkin I.I., Ksenzova L.D., Sentsova T.B., Lukina O.F., Sedova M.S. Current trends in pharmacotherapy of allergic rhinitis in children. Issues of modern pediatrics. 2007. t. 6. No. 6. p. 85–91. 2. Vishneva E.A., Alekseeva A.A., Gevorkyan A.K. Use of desloratadine for allergic rhinitis and concomitant bronchial asthma in children. Pediatric pharmacology. 2008. T. 5. No. 2. P. 33–37 3. Gevorkyan A.K., Tomilova A.Yu., Namazova L.S., Botvineva V.V. Allergic rhinitis: diagnosis and treatment (based on materials from the educational program for pediatricians) Pediatric pharmacology. 2008. vol. 5. No. 1. p. 62–67. 4. Geppe E.A., Seliverstova E.A., Farber I.M., Babushkina N.G., Utyusheva M.G., Malyavina U.S. The relationship between allergic rhinitis and bronchial asthma in children. Russian allergological journal. 2007. No. 1. p. 75–80. 5. Geppe N.A., Seliverstova N.A., Utyusheva M.G. The effectiveness of desloratadine in atopic dermatitis in children. Allergology. 2005. No. 2. p. 9–11. 6. Goryachkina L.A., Demborinskaya A.S., Borzova E.Yu. Clinical efficacy and safety of desloratadine in the treatment of seasonal allergic rhinitis. Allergology. 2003. No. 2. p. 1–6. 7. Gushchin I.S., Poroshina Yu.A., Mikeladze K.R., Zuikova I.N., Shulzhenko A.E. Antiallergic effect of desloratadine and loratadine in vivo in humans. Allergology. 2004. No. 2. p. 10–15 8. Ilyina N.I., Fedenko E.S.. Skin manifestations of allergies. Physiology and pathology of the immune system, 2004, 2, p. 125–134 9. Karpov V.P., Karpova E.E. The use of drugs "Nasonex" and "Erius" in the treatment of allergic rhinosinusitis. Russian rhinology. 2009. No. 2. p. 77 10. Korostovtsev D.S. Desloratadine (Erius) is a new non-sedating antihistamine (highly selective H1 receptor antagonist) Allergology. 2002. No. 1. p. 44–50. 11. Korsunskaya I.M., Shashkova T.V. The effectiveness of Erius for various skin diseases. Allergology. 2003. No. 3. p. 46–47 12. Kungurov N.V., Kokhan M.M., Keniksfest Yu.V., Grishaeva E.V., Khoseva E.N. The use of the antihistamine drug Erius (desloratadine) in the complex therapy of chronic dermatoses. Allergology. 2005. No. 3. p. 51–55. 13. Onu V.F., Gribinyuk A.I., Dumbrava V.A., Kasapchuk M.L., Kharya G.G., Kornagolub L. Use of the drug Erius in the treatment of atopic bronchial asthma combined with allergic rhinitis. Allergology and immunology. 2006. t. 7. No. 3. p. 317 14. Sergeeva I.G., Krinitsyna Yu.M. Modern antihistamines in complex therapy of allergic skin diseases. Allergology. 2003. No. 4. p. 42–43. 15. Sulima V.V., Suleymanov S.Sh., Vasilyeva M.M., Abrosimova N.V., Molchanova O.V. Pharmacoeconomic aspects of the use of antihistamines in the treatment of allergic diseases. Allergology. 2005. No. 3. p. 46–50. 16. Bachert C, Maurer M. Safety and efficacy of desloratadine in subjects with seasonal allergic rhinitis or chronic urticaria: results of four postmarketing surveillance studies. Clin Drug Investig. 2010;30(2):109–22. doi: 10.2165/11530930–000000000–00000 17. Belsito DV. Second–generation antihistamines for the treatment of chronic idiopathic urticaria. J Drugs Dermatol. 2010 May;9(5):503–12. 18. Berger WE. The safety and efficacy of desloratadine for the management of allergic disease. Drug Saf. 2005;28(12):1101–18. 19. Lachapelle JM, Decroix J, Henrijean A, Roquet–Gravy PP, De Swerdt A, Boonen H, Lecuyer M, Suys E, Speelman G, Vastesaeger N. Desloratadine 5 mg once daily improves the quality of life of patients with chronic idiopathic urticaria. J Eur Acad Dermatol Venereol. 2006 Mar;20(3):288–92. 20. Singh–Franco D, Ghin HL, Robles GI, Borja–Hart N, Perez A. Levocetirizine for the treatment of allergic rhinitis and chronic idiopathic urticaria in adults and children. Clin Ther. 2009 Aug;31(8):1664–87. 21. Staevska M, Popov TA, Kralimarkova T, Lazarova C, Kraeva S, Popova D, Church DS, Dimitrov V, Church MK. The effectiveness of levocetirizine and desloratadine in up to 4 times conventional doses in difficult–to–treat urticaria. J Allergy Clin Immunol. 2010 Mar;125(3):676–82.
Indications for use
- Rapid relief of allergy symptoms, including rhinitis of allergic origin and seasonal hay fever (swelling of the mucous membrane of the nasopharynx, itching, sneezing, nasal congestion, rhinorrhea , conjunctival hyperemia, lacrimation, cough).
- Reduction of rash and skin itching in chronic idiopathic urticaria .
Indications for the use of the drug, on the recommendation of a doctor, can be expanded and prescribed for other allergic conditions and diseases.
Side effects
When taking tablets, you may experience increased fatigue, headache, dry mouth, nausea, and vomiting. Much less common - palpitations, tachycardia bilirubin concentration and liver enzyme activity, diarrhea, drowsiness, dizziness, local allergic reactions.
When taking syrup, children under 2 years of age may experience insomnia , diarrhea , and increased body temperature. Children over 12 years of age may experience increased fatigue, headache, and dry mouth.
Instructions for use of Erius (Method and dosage)
Erius tablets, instructions for use
Adults are prescribed one 5 mg tablet once a day. It is recommended not to chew the drug, but to swallow the tablet whole with water. The duration of taking the drug is determined by the course and severity of the disease. Most often, treatment is stopped after relief of the symptoms of the disease, but it can be long-term for allergic rhinitis throughout the entire period of contact with the allergen.
Erius syrup, instructions for use
Children from 6 months to five years are prescribed 2.5 ml of syrup once a day. For children 6 to 11 years old, 5 ml of syrup, and for adolescents over 12 years old, the medicine is prescribed in a dose of 10 ml once a day. Drops of syrup must be washed down with water.
Instructions for use of AERIUS®
Desloratadine begins to be detected in plasma within 30 minutes after administration. Cmax of desloratadine in plasma is achieved on average after 3 hours, T1/2 is on average 27 hours. The degree of accumulation of desloratadine corresponds to its T1/2 (approximately 27 hours) and frequency of use (once daily). The bioavailability of desloratadine was dose proportional, ranging from 5 to 20 mg.
Desloratadine is moderately (83-87%) bound to plasma proteins. When using desloratadine at a dose of 5-20 mg 1 time / day for 14 days, no signs of clinically significant accumulation of the drug were found.
When conducting cross-comparative studies with the same dose of the drug, the bioequivalence of the drug in the form of tablets and syrup was revealed.
Desloratadine is effectively converted to the active metabolite 3-hydroxy-desloratadine and then glucuronidated. The enzymes responsible for the metabolism of desloratadine have not yet been established, and therefore the possibility of interaction with other drugs cannot be completely excluded. The results of in vivo and in vitro studies showed that desloratadine does not inhibit CYP3A4 or CYP2D6.
In part of the population, the conversion of desloratadine to 3-hydroxy-desloratadine is clearly slowed down due to an as yet unknown phenotypic polymorphism in metabolism. Approximately 2% of Caucasians and more than 20% of black patients have the following AUC ratio: DL/3-OH-DL>10 (normal:
- <4), and these patients are characterized as "slow inactivators". In adults classified as slow inactivators, desloratadine exposure (AUC) after multiple doses was 6 times higher than in adults with normal metabolism. The pharmacodynamic effects of these options, particularly the effect on the QTc interval, have not yet been fully established.
Studies of the effects of repeated doses of desloratadine in children have not been conducted.
When conducting pharmacokinetic studies in pediatric practice, it was found that the AUC and Cmax of desloratadine (when used in recommended doses) were comparable to the same indicators in adults taking desloratadine in the form of desloratadine syrup at a dose of 5 mg.
Patients with impaired renal function
There is no experience with repeated use of desloratadine in renal failure.
In patients with stable dysfunction, desloratadine after administration of its single dose was increased by 1.5-2.5 times, and the concentration of 3-hydroxy-desloratadine changed minimally. By hemodialysis, desloratadine was excreted only in small amounts (0.3%). In addition, plasma protein binding of desloratadine and 3-hydroxy-desloratadine was not altered in kidney disease; as a result, the concentration of unbound active substance remained unchanged.
Patients with liver dysfunction
In patients with moderate hepatic impairment, AUC may increase 3-fold. Plasma protein binding of desloratadine and 3-hydroxy-desloratadine was not altered in patients with liver disease. The incidence of adverse effects did not increase when treated for a maximum of 10 days and in patients with moderate liver damage (Child B).
A study with a single dose of desloratadine 7.5 mg found that food (high-fat, high-calorie breakfast) or grapefruit juice did not affect the distribution of desloratadine.
Erius for children
Prescribing antiallergic drugs of the 2nd and 3rd generations is more appropriate in children. It is important that the drug has no effect on psychomotor functions or cardiotoxicity. It is highly safe for children and has a special release form for this age category.
The instructions for Erius syrup for children indicate that syrup for children is contraindicated for children under 6 months, and tablets for children under 12 years of age, since the safety of its use has not been established. The important thing is that with long-term use, the effectiveness of the drug is maintained and there is no need to replace it with another drug. This is important in the treatment of chronic allergic diseases, which sometimes require constant use.
Erius syrup for children, reviews of which are positive, are often prescribed for allergic rhinitis . Parents note that in the first week of treatment, nasal discharge, itching and sneezing decrease, and symptoms, including nasal congestion, are completely relieved after 2 weeks. In children with atopic dermatitis, there was a disappearance of itching on the 5th day, and a decrease in rashes on the 7th day.
What are the causes of the disease?
It is necessary to distinguish between the cause and triggers of atopic dermatitis.
The reason is not fully known to modern science; the main version is a set of genetic, immune and skin changes, in particular, a deficiency of the skin protein filaggrin, which is responsible for retaining moisture in the skin.
The triggers of atopic dermatitis are very diverse, atopic skin is overly sensitive to irritation, so exacerbation can be caused by increased sweating, heat, rough clothing, detergents, dry air, etc. Children with atopic dermatitis may simultaneously have allergies to food, household or other animals, dust mites, tree and grass pollen - these allergens can also be triggers for exacerbations.
In general, atopic dermatitis has a wave-like course, periods of exacerbations (most often occurring for unobvious reasons or for no reason) are replaced by periods of remission - hence there is a great temptation to associate exacerbations with factors that are not directly related to the disease, and vice versa - to attribute healing properties to completely extraneous factors (for example, a diet that parents started by mistake or out of desperation).
It is impossible not to mention the established harmful domestic tradition of calling atopic dermatitis allergic (usually associating it with an allergy to cow’s milk protein) and treating it with diets (a strict “hypoallergenic” diet for a nursing mother, and/or a hydrolysis/amino acid mixture for a child). Indeed, if a child has an intolerance to cow's milk proteins, it may aggravate or cause atopic dermatitis, but not vice versa. Not every child with atopic dermatitis has an intolerance to cow's milk proteins or any other allergens. This means that by prescribing a diet, or an expensive and unpleasant-tasting mixture, the doctor adds problems to the family without helping them. In most cases of atopic dermatitis, identifying allergies and excluding allergens does not provide any benefit.
Analogues of Erius
Level 4 ATX code matches:
Dezal
Histaphene
Clarisens
Telfast
Claridol
Claritin
Loratadine
Fexofast
Peritol
Desloratadine
LauraHEXAL
Clarotadine
Rupafin
Ciel
Dramamine
Lordestin
Lomilan
Fenkarol
Kestin
Loratek
Analogues of Erius, which have the same active substance and ATX code: Alergomax , Alernova , Alersis , Allergo -Norm , Allergostop , Desloratadine , Desorus , Lordes , Lordestin Trexil Neo , Telfast , Fribris , Edem , Eridez and others.
The price of analogues varies widely; there are analogues at a higher and lower price than Erius, but in many ways, the price depends on the manufacturer, packaging, and the number of tablets in the package. If the patient has a special sensitivity desloratadine For example, the drug "Zodak" can be used as an analogue of "Erius" syrup.
Which is better: Erius or Telfast?
Telfast belongs to the second generation of (non-sedating) antihistamines. These 2 drugs differ in the active substance, in this case it is fexofenadine , which is not metabolized in the body, so its pharmacokinetics do not change if liver and kidney function are impaired. Maximum safe. The effect appears after 1 hour, and maximum after 6 hours. The terminal half-life is 11-15 hours, so in some cases the drug is prescribed 2 times a day. There is no syrup form, which limits use in young children. The drug can be used in children over 6 years of age (30 mg tablets).
Desloratadine , the active ingredient in Erius, is the only H1-histamine receptor blocker that has shown in studies a decongestive effect - it reduces nasal congestion in seasonal allergic rhinitis . Effective for a combination of allergic rhinitis and bronchial asthma , as well as for chronic urticaria . In terms of activity against H1 receptors, Erius is 3-4 times superior to second generation drugs. Its important property is the presence of anti-inflammatory activity. The action begins after 30 minutes and reaches a maximum after 1 hour. The long half-life provides a therapeutic effect throughout the day. Characterized by a high level of safety. It does not cause negative effects on the cardiovascular system and is well tolerated. It is used in children from 1 year (syrup) and over 12 years (tablets).
What to choose: Lordestin or Erius?
Lordestin and Erius have the same active ingredient - desloratadine, and apparently the effectiveness of the drugs is the same. Available in the same dosage, the half-life is up to 27 hours, so it is taken once a day. There is no syrup form. The drug is taken by children from 12 years of age.
The drugs differ in manufacturer and cost. Lordestin is a generic, manufactured by Gedeon Richter-RUS (Russia), the cost of 30 tablets is 752 rubles. The second drug is original, manufactured by Schering-Plough Labo NV (Belgium), the cost of 10 tablets is 548 rubles.
Treatment of atopic dermatitis in children
There is no complete treatment for atopic dermatitis, that is, there are no methods of therapy that would lead to complete recovery (change the long-term prognosis of the disease). All existing methods of therapy change only the short-term prognosis - for the coming months.
However, treatment is necessary:
- to improve the quality of life of the child and family; for the prevention of secondary local complications (infections, skin atrophy, etc.);
- for the prevention of psychological problems (sleep disorders, depression, etc.).
Treatment is divided into lifestyle changes (eliminating triggers) and drug interventions (eliminating symptoms).
Change of life. What can parents do themselves?
Don't let your baby's skin become excessively dry, severe itching, and avoid triggers. Try following these simple tips:
- Children with atopic dermatitis should take short baths or shower with warm (not hot) water. Use mild, unscented soap or soap-free cleansers. Do not wipe, but pat your skin with a towel after washing. Immediately after bathing, apply moisturizer to your entire skin. Teenagers prefer to use unscented cosmetics and oil-free facial moisturizers.
- Consult your doctor; if your child has no contraindications, add oat decoction to the bath when bathing; it can reduce itching.
- Preference should be given to soft children's clothing made from breathable fabrics, such as cotton. Wool or polyester may be too harsh or irritating for atopic skin.
- Your child's nails should be trimmed regularly and short to prevent scratching of the skin. If your child scratches himself at night, try putting him to bed in comfortable, lightweight mittens or with the sleeves of his pajamas sewn up.
- Overheating of children should be avoided, as sweat can lead to exacerbations. This is especially true for Russian parents who are accustomed to hot temperatures in the apartment and wrapping their children up during walks.
- Children should be encouraged to drink plenty of water.
- Try to get rid of common allergens in and outside your home, such as pollen, mold and tobacco smoke.
- Stress can make atopic dermatitis worse. Help your child find ways to cope with stress (such as exercise, deep breathing, or talking to a counselor).
Reviews about Erius
Reviews of Erius tablets
In most reviews, patients speak of the drug as a good remedy.
- “... I have been an allergy sufferer since I was 16 years old. Dust mite allergy. I constantly do wet cleaning. I have tried all sorts of allergy pills. Now I’m taking Erius - it’s an excellent medicine for allergies, you could say it’s my salvation. Quickly suppresses the effect of allergens, there is no drowsiness. After completing the ten-day course, I do not feel allergy attacks. I can visit you freely without any problems.”
Reviews of Erius syrup
Reviews are varied, but mostly positive.
- “... The child is 14 months old. Allergy from birth, manifested by swelling and rash. The doctor prescribed syrup and told me how to take it. A wonderful result, on the second day the allergy symptoms disappear, we can walk with the baby as much as we want. The effect after the course of treatment lasts for another 10-15 days. We took 2 courses, the allergy symptoms after its discontinuation became less pronounced. The syrup tastes good, the child drinks it without objection.”
Reviews from doctors
A drug with clinically significant antiallergic properties and proven anti-inflammatory activity. It inhibits the development of the initial phase of the allergic response, relieves allergic inflammation, thereby increasing the quality of life of patients. Good tolerability and a high degree of safety allow us to recommend the drug for the treatment of adults and children with allergic seasonal rhinitis and chronic urticaria. With long-term use of Erius, resistance to it does not arise, which allows it to be prescribed for a long period (up to a year) for diseases such as allergic rhinitis, atopic dermatitis, and bronchial asthma.
Diagnostics
There is no specific test or examination to confirm the diagnosis of atopic dermatitis; the diagnosis is made clinically. The doctor will examine the rash and ask about the child's symptoms and family history of atopy and allergies. A history of eczema in family members (either as a child or still today) will be an important clue.
Your doctor will rule out other conditions that may cause your skin to become inflamed or itchy. In case of difficulties with diagnosis or severe course of the disease, the pediatrician will refer the child to a pediatric dermatologist or pediatric allergist.
The doctor may ask you to eliminate certain foods (such as eggs, milk, soy, or nuts) from your child's diet for 2 to 3 weeks before reintroducing them and monitoring symptoms. If the diet leads to relief of the rash, and provocation leads to its obvious exacerbation, this will confirm the diagnosis and the need for a diet.
Since there are no accurate laboratory methods for confirming the diagnosis of atopic dermatitis, there are criteria for standardizing the clinical diagnosis (the best known are the Hanifin and Raika criteria).
The criteria are divided into “large” and “small”. To make a diagnosis of atopic dermatitis, it is necessary and sufficient to detect three major and three minor criteria in the patient.
The big ones include:
- itching;
- dermatitis affecting the flexor surfaces in adults, or the face and extensor surfaces in infants;
- chronic or recurrent dermatitis;
- a personal or family history of skin or respiratory allergies.
Small ones include:
- specific facial features: facial pallor, erythema, hypopigmented spots, dark circles under the eyes, cheilitis, infraorbital folds, recurrent conjunctivitis, anterior neck folds;
- typical triggers: emotional factors, environmental factors, food, skin irritants;
- typical complications: susceptibility to skin infections, impaired cellular immunity, predisposition to keratoconus and anterior subcapsular cataracts, immediate skin reactivity;
- other signs: early age of onset, dry skin, ichthyosis, hyperlinearity of the palms, piliary keratosis, dermatitis of the hands and feet, nipple eczema, white dermographism, white pityriasis, perifollicular accentuation.
An explanation of each of these symptoms is beyond the scope of this article; The criteria are given here to help you understand what the doctor is guided by when making a diagnosis of atopic dermatitis.
There are also various scales for assessing the severity of atopic dermatitis used by doctors and scientists, the most famous of which is the SCORAD scale. In this scale, the doctor must note the number, prevalence and severity of symptoms of atopic dermatitis, express them in points, sum up the points and, based on this sum, set the severity of the disease.
Erius price, where to buy
The price of Erius in tablets 5 mg No. 7 in Moscow pharmacies varies between 365 -460 rubles per pack; No. 10 - from 482 to 628 rubles.
The price of Erius syrup 2.5 g in a 60 ml bottle ranges from 525 to 646 rubles; A 120 ml bottle of syrup for children costs from 670 to 870 rubles per package.
The price of Erius in Ukraine for tablets No. 7 varies between 167 – 226 hryvnia; No. 10 —240 -258 hryvnia per package. Drops (syrup) in a 60 ml bottle in pharmacies in Ukraine (Kyiv) costs an average of 180 hryvnia; in a 120 ml bottle - 328 hryvnia. These allergy pills can be bought in other cities of Ukraine. Their cost in pharmacy chains in Dnepropetrovsk or Odessa is almost the same as their price in Kyiv.
You can buy all forms of the drug without difficulty in most pharmacies in Moscow and other Russian cities, as well as in the pharmacy chain of Ukraine.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Erius syrup 2.5 mg/5 ml 60 ml Schering-Plough Labo NV
RUB 419 order - Erius tab. p/o captivity. 5mg 10pcs Bayer Bitterfeld GmbH
RUR 596 order
Pharmacy Dialogue
- Erius tablets 5 mg No. 10Shering-Plough
RUB 619 order
- Erius syrup 60mlShering-Plow
460 rub. order
show more
Pharmacy24
- Erius 5 mg N10 tablets Schering-Plough Labo N.V., Belgium
223 UAH.order - Erius 60 ml 0.5 mg/ml syrup Schering-Plough Labo N.V., Belgium
161 UAH order
PaniPharmacy
- Erius tablets Erius film-coated tablets 5 mg No. 10 Belgium, Schering-Plough Labo
281 UAH order
- Erius liquid Erius syrup 60ml Belgium, Schering-Plough Labo
216 UAH order
show more