What is lactulose
Lactulose is a natural component consisting of galactose and fructose molecules. It is obtained by isomerizing lactose, which is isolated from whey, which is why the substance has a slight sweetish taste.
Lactulose is a prebiotic - substances that serve as food for intestinal microflora. These are indigestible food components that selectively stimulate the growth and activity of the protective intestinal microflora and thereby improve its health. Prebiotics mainly include a type of dietary fiber that is not broken down in the stomach due to the lack of specific enzymes.
Lactulose was first discovered in 1948 in women's breast milk, then numerous studies have shown its positive effect on the proper functioning of the gastrointestinal tract in infants. Scientists F. Mayerhofer and F. Petuely in 1959 recorded the positive effect of lactulose on the intestinal microbiota of bottle-fed newborns: the population level of bifidobacteria increased from practically zero to 80-100%.
The following positive properties of lactulose can be highlighted:
- has a mild laxative effect;
- normalizes the functioning of the digestive tract;
- triggers the body's defense mechanisms and helps eliminate toxins;
- promotes better absorption of calcium and magnesium.
Lactulose Farmland syrup 667 mg/ml in 15 ml bags No. 10
Name
Lactulose Farmland syrup 667 mg/ml per bag. 15 ml in pack No. 10
Description
Transparent viscous liquid from light yellow to brownish yellow, sweet in taste.
Main active ingredient
lactulose as lactulose
Release form
Syrup
Dosage
15ml
Pharmacological properties
Lactulose is a synthetic derivative of lactose. It does not disintegrate in the stomach and small intestine due to the lack of appropriate enzymes and is practically not absorbed. Once in the intestines, it stimulates peristalsis, improves the absorption of phosphates and calcium salts, increases the diffusion of ammonia from the blood into the intestines and promotes its excretion from the body. In the large intestine, lactulose, under the influence of intestinal flora, is broken down into low molecular weight organic acids - mainly lactic acid and partially formic and acetic acids. At the same time, the osmotic pressure increases and the pH in the lumen of the large intestine decreases, the volume of stool increases, which stimulates the peristalsis of the large intestine and normalizes the consistency of the stool. This helps eliminate constipation and restore the physiological rhythm of bowel movements. The removal of bound ammonium ions occurs with the development of a laxative effect. The laxative effect appears 24 to 48 hours after administration. In addition, lactulose removes bile acids from feces, resulting in a decrease in cholesterol levels in the blood and bile. In hepatic encephalopathy or hepatic precoma/coma, the effect is attributed to suppression of proteolytic bacteria by increasing the number of acidophilic bacteria (eg, lactobacilli); the transition of ammonia into ionic form due to acidification of the contents of the colon; bowel emptying due to decreased pH in the colon and osmotic effect; as well as reducing nitrogen-containing toxic substances by stimulating bacteria that utilize ammonia for bacterial protein synthesis. Lactulose, as a prebiotic substance, promotes the growth of bifidobacteria and lactobacilli, while the growth of opportunistic clostridia and Escherichia coli can be suppressed. This promotes a favorable balance of intestinal microflora.
Indications for use
— constipation: regulation of the physiological rhythm of bowel movements; - softening of stool for medical purposes (hemorrhoids, operations on the colon and anus, in the postoperative period); - hepatic encephalopathy: treatment and prevention of hepatic precoma or coma.
Directions for use and doses
Lactulose Farmland is taken orally. The duration of treatment and dose are determined by the doctor individually. Farmland lactulose can be taken either diluted or undiluted. It is necessary to immediately swallow the single dose taken without holding it in the mouth. All dosages must be selected individually. If a single daily dose is prescribed, it must be taken at the same time, for example, during breakfast. During laxative therapy, it is recommended to take a sufficient amount of fluid (1.5-2 liters) per day. Prevention of constipation: Should be taken once a day. The clinical effect occurs within 1-2 days. The dose is increased if no improvement in the patient's condition is observed within 2-3 days of taking the drug. Adults and adolescents: the initial dose is 15-45 ml, the maintenance dose is 15-30 ml. Children: up to 1 year of age, initial dose – up to 5 ml, maintenance dose – up to 5 ml; from 1 year to 6 years, the initial dose is 5-10 ml, maintenance dose is 5-10 ml; from 7 to 14 years, the initial dose is 15 ml, maintenance dose is 10-15 ml. As a rule, the dose can be reduced after 2 days of administration depending on the patient's needs. Reception for softening stool: The dosage of the product for softening stool is the same as for constipation. For the prevention of hepatic encephalopathy, hepatic precoma or coma (adults): Initial dose of 30-45 ml 3-4 times a day, and then switch to an individually selected maintenance dose so that there are soft stools 2-3 times a day. Children The safety and effectiveness of use in children (under 18 years of age) with hepatic encephalopathy has not been established due to a lack of data. Elderly patients and patients with renal or hepatic impairment: There are no specific dosing recommendations as systemic exposure to lactulose is negligible.
Use during pregnancy and lactation
Before using the drug, pregnant and lactating women should consult a doctor. If necessary, the drug can be prescribed during pregnancy and lactation, since the systemic effect of lactulose is insignificant. No effect on reproductive function is expected.
Precautionary measures
If abdominal pain of unknown origin occurs before starting treatment or there is no therapeutic effect several days after starting the drug, you should consult your doctor. Lactulose should be administered with caution to patients with lactose intolerance. The dose usually used in the treatment of constipation does not require adjustment for patients with diabetes mellitus. When treating hepatic encephalopathy, higher doses are usually prescribed, which should be taken into account in relation to diabetes mellitus. Continuous use of uncorrected doses and abuse can lead to diarrhea and fluid and electrolyte imbalance. It must be taken into account that the drug contains lactose, galactose and a small amount of fructose, therefore this drug should not be prescribed to patients with galactose or fructose intolerance, lactase deficiency or glucose-galactose malabsorption. Lactulose can be used in small children and infants only in exceptional cases under the supervision of a physician. Taking lactulose in children may cause disruption of the voiding reflex.
Interaction with other drugs
Interaction studies with other drugs have not been conducted.
Contraindications
- hypersensitivity to the components of the drug; - galactosemia; - obstruction of the gastrointestinal tract, perforation or risk of perforation of the gastrointestinal tract.
Compound
1 ml of syrup contains the active ingredient: lactulose in the form of lactulose (liquid) – 667 mg.
Overdose
Symptoms: when using a very high dose, diarrhea and abdominal pain are possible. Treatment: The dose should be reduced or the drug should be stopped. Large fluid losses due to diarrhea or vomiting may require correction of electrolyte imbalances.
Side effect
In the first days of taking lactulose, flatulence may occur. As a rule, it disappears after a few days. If high doses are used for a long time in the treatment of hepatic encephalopathy, the patient may develop electrolyte imbalance due to diarrhea. If the recommended doses are exceeded, abdominal pain and diarrhea may occur, which requires a dose reduction. Frequency of these undesirable effects: very often ≥1/10; often from ≥1/100 to ˂1/10; infrequently from ≥1/1000 to ˂1/100; rarely from ≥1/10000 to ˂1/1000; very rarely ˂1/10000. Gastrointestinal disorders: very often – diarrhea; often – flatulence, abdominal pain, nausea, vomiting. Impact on the results of laboratory and instrumental studies: infrequently - electrolyte imbalance due to diarrhea.
Storage conditions
Store at a temperature not exceeding 25ºС. Keep out of the reach of children.
Buy Lactulose Farmland syrup 667 mg/ml in a 15 ml package in pack No. 10 at the pharmacy
Price for Lactulose Pharmland syrup 667 mg/ml per bag. 15 ml in pack No. 10
Instructions for use for Lactulose Pharmland syrup 667 mg/ml per bag. 15 ml in pack No. 10
Lactulose: what products contain it?
For proper and stable functioning of the body, it is important to eat foods rich in fiber. Some of them also contain lactulose. Fiber and lactulose are not absorbed by the body, but they create a feeling of fullness and help you avoid overeating. They also improve intestinal motor function and promote the elimination of toxins.
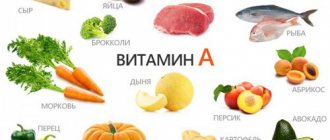
In food products, lactulose is found in:
- breast milk;
- yogurt;
- cottage cheese;
- apricots and dried apricots;
- asparagus;
- lettuce leaves;
- daikon;
- cauliflower;
- broccoli;
- corn;
- garlic;
- onions;
- black currant;
- lingonberries;
- papaya;
- beans;
- pineapple
Lactulose in the treatment of functional constipation
About the article
4699
0
Regular issues of "RMZh" No. 13 dated June 15, 2010 p. 834
Category: Digestive diseases
Author: Shifrin O.S.
For quotation:
Shifrin O.S. Lactulose in the treatment of functional constipation. RMJ. 2010;13:834.
Chronic constipation is a medical and social problem of great importance [1]. In economically developed countries, up to 40% of the total adult population suffers from them. Disruption of the normal functioning of the intestine sharply reduces the quality of life of people, reduces their performance, and increases the risk of developing serious diseases, including colorectal cancer [2]. Acceptance of the diagnostic concept of primary functional constipation (combining the concepts of primary functional constipation itself, constipation against the background of the clinical course of irritable bowel syndrome - IBS - and constipation associated with dyssynergia of the pelvic floor muscles) requires the preliminary mandatory exclusion of organic (mechanical) constipation as a consequence of various forms of intestinal and extraintestinal obstruction, secondary functional constipation associated with metabolic, endocrine, toxic, neurogenic and other reasons [2]. Although in most cases chronic constipation is primarily functional in nature, unfortunately, in many cases, insufficient examination of patients leads to late diagnosis of many serious diseases, including colon cancer.
The high incidence of primary functional constipation in economically developed countries is associated primarily with the peculiarities of people's lifestyle: the relatively low physical activity of large sections of the population, the consumption of refined foods with low fiber content. In addition, it is necessary to take into account the increasing proportion of elderly and old people in the general population, who are much more prone to developing primary functional constipation. At the same time, the problem of constipation does not at all act as only a problem of gerontology, since IBS with a predominance of constipation is widespread in both young and middle-aged people. The average age of such patients is 24–41 years. The incidence of IBS has been growing significantly in recent years and is about 14% in Russia. The incidence of patients with a similar form of IBS, according to the outpatient department of the Clinic of Propaedeutics of Internal Medicine, Gastroenterology and Hepatology named after. V.Kh. Vasilenko, in recent years accounts for 15 to 20% of all requests from gastroenterological patients. Patients with primary forms of functional constipation should be treated, as a rule, on an outpatient basis. An indication for hospitalization may be the need for a clinical examination to clarify the diagnosis, although in most cases clinical examination in this category of patients is performed on an outpatient basis. Therapeutic measures for chronic functional constipation cannot be limited to purely drug therapy, but must include a whole range of measures that largely ensure a change in the stereotype of human behavior [3]. In practice, implementation of such recommendations may be accompanied by significant difficulties. In most cases, general recommendations can be to increase the daily amount of dietary fiber and fluid consumed [4]. At the same time, elderly people often have difficulty chewing in the presence of dentures in the oral cavity, which does not allow them to fully use fibers as a laxative. In addition, the presence of large amounts of phytin in bran can reduce the absorption of vitamins and calcium, which are essential in old age. With a combination of painful and constipative forms of IBS, excessive consumption of dietary fiber may be accompanied by increased abdominal pain. Therefore, all patients with functional constipation should be instructed to carefully self-assess their tolerance to various forms of fiber and promptly inform their physician about possible problems associated with this. Significant importance should be given to increasing the physical activity of patients and regular self-massage of the abdominal wall. However, in reality, older people who suffer from chronic constipation and other diseases (including the cardiovascular system) often find it difficult in practice to follow the doctor’s recommendations to significantly increase physical activity. Explaining to a patient the need to change his daily routine in order to develop conditioned reflexes to defecation often encounters the inertia of a person’s behavior in terms of changing stable habits and an established behavioral stereotype. Thus, according to our clinical experience, in a group of 30 patients with IBS (a form with a predominance of constipation), who were given appropriate dietary recommendations, 6 patients (20%) actively complained about the inability to significantly change their diet for a long time according to the doctor’s recommendations. It is difficult to believe that the remaining patients firmly adhered to these recommendations. If general recommendations (diet with a high content of dietary fiber, regimen, self-massage of the intestines) are insufficiently effective in combating functional constipation, one should switch to drug therapy. In this case, the optimal drug for long-term maintenance therapy should be considered not a drug that gives an immediate effect, but a drug with a mild laxative effect, made from natural raw materials, and with a pharmacological effect as close as possible to the natural physiological processes in the body. Most laxatives, especially with long-term use, can have an adverse effect on digestion and water-electrolyte metabolism. Thus, loss of sodium can cause the development of secondary hyperaldosteronism, and loss of potassium, leading to weakened intestinal motility, can aggravate constipation [2]. Laxatives that stimulate intestinal motility (anthronoids and diphenylmethane derivatives) have an oncogenic effect. Most laxatives decrease in effectiveness over time and require a constant increase in dose to achieve the desired effect. Many of the drugs cannot be prescribed to young children, the elderly, pregnant women and during lactation, as well as in the presence of a number of diseases of the internal organs and nervous system. Based on the above, if non-drug management of patients with chronic functional constipation is insufficiently effective, lactulose (Duphalac) should be used as a drug that is closest to the concept of an “ideal laxative”. Lactulose was discovered by the Austrian pediatrician Petueli. In 1948, while studying the cause of dyspepsia in young children, he isolated a substance from human milk that activated the growth of protective intestinal microflora (bifidobacteria and lactobacilli). The researcher named it lactulose. Petueli's research showed that when a baby was fed with regular infant formula or milk, the content of bifidobacteria in the fecal microflora was 20%, but when 2% lactulose was added to baby food, the content of bifidobacteria increased 4 times. Numerous subsequent studies of lactulose have proven its therapeutic and preventive properties, which stimulated the introduction of the drug into both the pharmaceutical and food industries. Lactulose is a white crystalline substance, odorless, highly soluble in water. It is produced by deep processing of milk from milk sugar - lactose. Lactulose belongs to the class of oligosaccharides, a subclass of disaccharides: its molecule consists of galactose and fructose residues. This substance is not broken down by digestive enzymes in the upper sections of the gastrointestinal tract and reaches the colon unchanged. Here, lactulose is broken down by enzymes of the intestinal microflora (bifidobacteria and lactobacilli) into organic acids: lactic, acetic, butyric, etc. Since the middle of the last century, a large number of studies have been conducted to decipher the mechanism of action and confirm the effectiveness of lactulose for constipation. The mechanism of its action for constipation primarily comes down to an increase in the concentration of short-chain carboxylic acids of the aliphatic series, which reduce the intraintestinal pH level and thereby stimulate intestinal motility. On the other hand, an increase in the osmotic pressure of intestinal contents leads to fluid retention, liquefaction and an increase in its volume, and consequently to activation of intestinal peristalsis. An increase in the volume of intestinal contents also occurs due to the accelerated growth of saccharolytic microflora. The effect of lactulose, unlike other laxatives, is more complex, since it affects the main pathophysiological mechanisms of constipation. On the one hand, the drug increases the volume and softens the intestinal contents, and on the other, it enhances intestinal peristalsis. In a comparative clinical study, which included 65 patients with chronic constipation, the effect of lactulose and polyethylene glycol-4000 on intestinal microflora was studied in parallel. The authors concluded that lactulose increases the number of bifidobacteria and increases the activity of microbial b-galactosides [5]. Another comparative study of laxatives to clarify the effect of lactulose and polyethylene glycol on the composition of the intestinal microflora revealed a significantly more pronounced effect of lactulose on increasing the population of bifidobacteria, 72 and 17%, respectively [7]. In parallel with the increase in the number of bifidobacteria, when lactulose was prescribed, there was a decrease in the number of bacteroides and clostridia. Such changes in the ratio of different populations of microorganisms in the intestine contribute to an increase in the production of short-chain fatty acids by intestinal bacteria, which improves the trophism of the intestinal epithelium. This positive effect improves the absorption of water and electrolytes and normalizes motor function. The possibility of widespread use of lactulose (Duphalac) in the treatment of functional constipation in both adults and children is determined, in addition to the high clinical effectiveness, by the physiological mechanism of action of the drug, the low frequency of side effects (most often a feeling of moderate bloating) compared to other laxatives. In addition, when the dose of the drug is reduced, these clinical symptoms often significantly decrease or disappear completely. The safety of lactulose allows its use even in children at an early age [6]. Constipation is one of the most common complaints in pregnant women. The exact etiological reasons for the development of constipation in pregnant women are not entirely clear, but an important place in its genesis is given to a general decrease in smooth muscle tone due to hyperprogesteronemia, which naturally leads to a decrease in the propulsive function of the intestine. On the other hand, constipation may be caused by changes in the topographic relationships of organs in the abdominal cavity and pelvis. Taking iron supplements, often prescribed during pregnancy (due to the development of iron deficiency anemia in women), can also lead to disturbances in the normal functioning of gastrointestinal motility. The Consultation Center of the University of Ulm conducted a study involving about 100 thousand pregnant women on the effectiveness and tolerability of lactulose in the treatment of constipation. There are no recorded harmful effects on the fetus from taking the drug during pregnancy. The researchers concluded that lactulose acts as the laxative most preferred by pregnant women. The effectiveness of using lactulose in pregnant women, as well as in elderly patients, has been proven in numerous other clinical studies. A high degree of safety of the drug has also been proven, since the main side effect of lactulose was minor transient flatulence. The drug’s ability to help patients who have been taking irritating laxatives for a long time (more than 8 years) before prescribing lactulose, as well as after operations for hemorrhoids, is attractive. In the latter case, it is advisable to start taking lactulose at least 4 days before hemorrhoidectomy. We assessed the effectiveness and safety of the use of lactulose (the drug Duphalac) in 80 patients (40 patients of which were patients with IBS, constipation, and 40 with functional primary constipation). The group of patients with IBS consisted of 24 women and 16 men, the average age was 36.6±4.3 years. In the group of patients with primary functional constipation, there were 55 females and 25 males; the average age of people in this group is 53.8±9.3 years. Against the background of 10-day treatment with lactulose at 30–40 ml/day. a positive effect on the normalization of stool was noted in 33 patients with IBS (82.7%) and in 31 with primary functional constipation (77.5%). The appearance of a feeling of bloating during treatment was noted only by 3 patients with IBS and 4 with functional constipation. When the dose of lactulose was reduced to 15–20 ml, the feeling of bloating persisted in only one patient with IBS (2.5%), and in 2 with functional constipation (5%), which was the reason for discontinuation of the drug in these few cases. In the vast majority of the remaining patients, after achieving a clinical effect, the dose of lactulose was reduced to 15–20 ml and left as maintenance during the subsequent months of treatment. The high willingness of patients in both groups to receive therapy is noteworthy. Thus, lactulose treatment was assessed as effective or highly effective by 30 patients with IBS (75%) and 31 patients with primary functional constipation (77.5%). The criteria for an optimally selected dosage of lactulose, in our opinion, can be the patient’s defecation 4–7 times a week with the presence of formed or semi-formed stool, while the act of defecation itself does not require any painful or excessive effort from the person. Thus, the use of lactulose (Duphalac) in the treatment of patients with primary functional constipation and the constipated variant of IBS can be recommended as the second phase of treatment for such patients. The use of this drug can be very useful if the patient’s compliance with general recommendations for basic diet therapy (ballast substances) and behavioral measures (development of conditioned reflexes to defecation, physical activity, self-massage of the intestines, etc.) is insufficiently effective. Literature 1. Gastroenterology. National leadership / Ed. V. T. Ivashkina, T. L. Lapina. M.: “Geotar-Media”, 2008. 700 p. 2. Rational pharmacotherapy of diseases of the digestive system / Ed. V. T. Ivashkina. M.: Publishing house “Literra”, 2003. 3. Irritable bowel syndrome / Ed. I. V. Maeva. M.: “GOU VUNMTs MH and SR RF”, 2004. 70 p. 4. Henderson D.M. Pathophysiology of the digestive organs / Trans. from English M. – St. Petersburg: Binom – Nevsky Dialect, 1997. – 287 p. 5. Bouhnik Y, Neut C, Raskine L, Michel C, Riottot M, Andrieux C, Guillemot F, Dyard F, Flourie B. Prospective, randomized, parallel–group trial to evaluate the effects of lactulose and polyethylene glycol–4000 on colonic flora in chronic idiopathic constipation.//Aliment.Pharmacol.Ther.– 2004.– Vol. 19(8).– P.889–899 6. Gleason W, Figueroa–Colon R, Robinson LH et al. A double-blind, parallel-group, placebo-controlled study of lactulose in the treatment of encopresis in children with chronic constipation.// Gastroenterol.– 1995.– Vol. 108 (suppl. 4).– P.A606. 7. Mangin I et al.: Molecular Analysis of Intestinal Microbiota Composition to Evaluate the Effect of PEG and Lactulose Laxatives in Humans.// Microbial Ecology in Health and Disease.– 2002.– Vol.l4(l).– P.54 –62 8. Zdunczyk Z, Juskiewicz J, Wroblewska M, Krol V. Physiological effects of lactulose and inulin in the caecum of rats.//Arch Anim Nutr.– 2004,– Vol.58 (1).– P.89– 98
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Lactulose for weight loss
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Perhaps half of overweight people dream of a miracle diet that will help them lose 5 or even 10 extra pounds in a week. Nutritionists, hearing this, say: “Nonsense! This cannot be! But advertising promises something else. Most drugs that quickly get rid of excess weight work on the principle of a laxative. For this reason, lactulose is sometimes also used inappropriately. By consuming drugs based on this substance, obese people want to achieve a laxative effect to reduce weight.
But a laxative, even the strongest one, has no effect on fat deposits. And false weight loss occurs only due to loss of moisture. Continuing this “weight loss” for several days, the only result that can be achieved for sure is dehydration and leaching of nutrients from the body. And even the beneficial properties of lactulose will not save the situation.
But there are options when lactulose can be taken for weight loss, or more precisely, as an adjuvant. When following a diet, especially if there are few foods rich in fiber in the diet, constipation often occurs. This is where lactulose comes to the rescue - it will help quickly remove waste products from the body, cleanse the intestines and take care of the correct microflora. As a result, this will affect your overall well-being, increase your tone and strengthen your immune system. This means you will have the strength to exercise, without which there will definitely be no effective weight loss.
Lactulose for children
The fact that lactulose can be beneficial for children was established by pediatricians in Austria back in the late 1940s. Observing bottle-fed babies, we noticed that dysbacteriosis occurs in such babies several times more often than in babies fed breast milk. After a series of experiments, it turned out that human milk contains lactulose, and this, in turn, provides healthy intestinal microflora.
Chemists have learned to synthesize this substance from lactose. And pharmacists introduce it into syrups that improve the microflora of children's intestines. This syrup can be given to children of all ages. The instructions for use describe in detail the dosages for each age group.
For adults, lactulose is available in the form of dietary supplements, laxative tablets, and other pharmaceutical forms. At the same time, the effect on the body is the same.
Lactulose: arguments and facts
Lactulose (4-O-beta-D-galactopyranosyl-D-fructose) is a synthetic disaccharide consisting of residues of galactose and fructose molecules. Lactulose is a stereoisomer of lactose. Medicines based on lactulose are available in the form of syrup or tablets. Indications for the use of lactulose preparations include: treatment of acute or chronic constipation, the need to achieve a soft stool consistency (in case of painful processes, the need for surgical intervention in the colon and/or anal area, in the postoperative period); treatment and prevention of hepatic encephalopathy; hyperammonemia of various origins. Lactulose is also used in the hydrogen breath test to detect bacterial overgrowth in the small intestine and assess motility. An extensive series of works by domestic and foreign authors is devoted to the study of the effect and tolerability of lactulose in various diseases. Among them, a prominent place is occupied by studies of the drug Normaze (lactulose syrup, Dr. Reddy's), which is widely used in Russia.
Lactulose in the treatment of constipation
One of the most important areas of application of lactulose is the treatment of acute and chronic constipation of various etiologies in patients of all age categories, including newborns and elderly patients. Lactulose can be prescribed as monotherapy, as well as in conjunction with laxatives based on dietary fiber, polyethylene glycol, and simultaneously with short courses of stimulant laxatives.
In adults, for the treatment of constipation, an initial dose of lactulose of 15–30 ml at night (if taken systematically in the morning) is recommended, with subsequent modification based on the frequency and consistency of stool [1].
According to surveys and analysis of medical records, approximately a quarter of the population of developed countries suffers from chronic constipation. A significant proportion of cases are primary, or idiopathic, constipation associated with poor lifestyle or functional disorders [2]. In the treatment of constipation, non-drug methods are not effective in all patients; there is a need to prescribe laxatives [2].
A systematic review by D. Ramkumar and SS Rao (2003) and a review by J. Johanson (2007) analyzed randomized trials (over the period 1966–2006) that assessed the effectiveness and safety of various laxatives in the treatment of chronic constipation in adults. The most convincing efficacy data corresponding to levels of recommendations A and B are obtained for polyethylene glycol (PEG), lactulose, psyllium and tegaserod [2, 3].
A systematic review of drugs for the treatment of constipation in adults recommended by the FDA (Food and Drug Administration) emphasizes that, despite some methodological shortcomings of the clinical studies conducted, the effectiveness of lactulose is beyond doubt (recommendation level B), although it is slightly inferior in severity of action PEG and dietary fiber preparations in combination with senna preparations [4].
Experts - authors of recommendations for the treatment of chronic constipation - believe that for irritable bowel syndrome with constipation, lactulose is most effective in cases where abdominal pain is significantly reduced after defecation. Due to the insufficient amount of research on the safety of lactulose in irritable bowel syndrome with constipation, it is more advisable to prescribe a disaccharide as an alternative to PEG - if the latter is ineffective or intolerable [1].
Lactulose is effective in the treatment of constipation, which develops when the urge to defecate is often ignored (in children and adults), since with systematic use of the disaccharide, a distinct and persistent urge is formed. Treatment begins with a low dose, with a gradual increase over several weeks until the effect is achieved, when the patient cannot ignore the urge to defecate. The effect lasts for several weeks and even months after discontinuation of the drug.
Dietary fiber and lactulose exhibit prebiotic properties and serve as sources of short-chain fatty acid (SCFA) production in the colon. The similarity and “naturalness” of the action of laxatives of these two classes served as the basis for organizing comparative studies.
A randomized, open-label, parallel group study of 124 patients with chronic idiopathic constipation compared the effectiveness of psyllium and lactulose. The duration of treatment was 4 weeks. Both laxatives showed similar positive effects on stool frequency, consistency, and general symptoms; were equally effective in reducing abdominal pain and the need to strain. Patients noted a more pleasant taste of lactulose [5].
A study of similar design and duration by N. Quah et al. was designed as a crossover study with a minimum washout period of 1 week. The number of participants was 50. The authors of the publication emphasize a more distinct and predictable effect of lactulose: with its use, the average frequency of stools was 7.3 times per week (95% CI (confidence interval): 5.7–8.9), whereas with taking dietary fiber – 5.5 times a week (95% CI: 4.4–6.5); p = 0.001. The consistency of stool on a conventional scale was 3.4 (95% CI: 3.1–3.7) and 2.9 (95% CI: 2.5–3.3) points, respectively; p = 0.018. A scale for assessing difficulty with defecation showed similar results. There were no significant differences in drug tolerability, although adverse events were recorded somewhat more frequently when taking lactulose. The final scale for assessing the effectiveness of patients when treated with lactulose was 6.2 points (95% CI: 5.5–7.0), when treated with dietary fiber – 4.8 (95% CI: 4.0–5.9); p = 0.017. Of the 39 patients who completed the study, 24 (61.5%) preferred lactulose, 14 (35.9%) preferred dietary fiber [6].
French researchers compared different regimens of lactulose for chronic idiopathic constipation: 20 g per day in one or two doses. The study was designed as a multicenter, double-blind, crossover design (2 dosing regimens, 3 weeks each). The total number of participants was 121. The results showed that the number of bowel movements per week (7.29 ± 3.20 vs. 7.08 ± 3.03), stool consistency, ease of defecation, frequency and severity of side effects were not significantly different [7 ].
A serious problem is the high prevalence of constipation in elderly and senile patients and its features - frequent slowing of intestinal transit, weakening of the pelvic floor muscles, decreased sensitivity of the rectum, and a tendency to irritate the mucous membrane with dense feces. The use of some laxatives in the elderly carries a high risk of complications - fecal impaction (when prescribing dietary fiber), water and electrolyte disorders (when prescribing salts and careless use of stimulants). Today, researchers are unanimous that in the elderly and senile age, bulk and osmotic laxatives - polyethylene glycol and lactulose - are most suitable as the main means of treating chronic constipation. Lactulose preparations do not irritate the colon mucosa and are not addictive; the active substance and metabolites do not enter the systemic circulation. Stimulant laxatives - senna preparations, bisacodyl, sodium picosulfate - are prescribed in short courses when osmotic agents are insufficiently effective or for occasional constipation [8, 9, 10].
Lactulose has been successfully used to treat symptomatic constipation.
The administration of lactulose (Normaze) in the early period after colon surgery significantly improves treatment results compared to the group of patients taking petroleum jelly. In particular, the duration of postoperative ileus is significantly reduced [11].
For constipation during treatment with opioid analgesics, the use of lactulose or PEG preparations has shown its effectiveness and safety [12, 1].
Lactulose in the form of monotherapy has an effect in some cases of laxative abuse.
Unlike the vast majority of other laxatives, lactulose is approved for use in pregnant and lactating women. Up to 66% of pregnant women note such manifestations of constipation as rare stools, dense stool consistency, and the need for additional straining. The reasons for this are the influence of progesterone on the excitability of intestinal smooth muscle cells, a sedentary lifestyle, taking iron supplements, compression of the intestines by the uterus, etc. Untimely bowel movements can have an adverse effect on the course of pregnancy. In the postpartum period, the cause of bowel dysfunction is changes in the sensitivity and strength of the pelvic floor muscles. The FDA classifies lactulose as a pregnancy risk category B drug. Lactulose does not have embryotoxic or teratogenic effects; in adequate doses does not cause a pronounced increase in intestinal motility and fluid loss, which could have a negative effect on uterine tone and placental blood flow [13]. Lactulose does not enter the systemic circulation and is not found in breast milk.
In the study by T.N. Sokur et al. studied the effectiveness and tolerability of lactulose (Normaze) in women at different stages of pregnancy who suffered from constipation resistant to non-drug treatment methods. The total number of participants was 150. The recommended dose of Normaze was 20–45 ml per day and was selected individually; Duration of treatment: 7–28 days. As a result of treatment, 145 (96.7%) pregnant women had normal stools, a feeling of complete bowel movement, and in 98 (65.3%) the feeling of heaviness and pain in the hypochondrium decreased. Normalization of intestinal function contributed to an improvement in overall well-being. Side effects such as nausea, flatulence, abdominal pain, loose stools with tenesmus were recorded in isolated cases, were moderate and did not require discontinuation of the drug. In no case was there any emergence or worsening of signs of threatened miscarriage, deterioration in general health, or an increase in the severity of preeclampsia [13].
A multicenter, open-label, controlled study of the efficacy and tolerability of lactulose in pregnant women with chronic or episodic constipation (n = 62) was conducted in Switzerland: in 34% of patients, constipation existed before pregnancy, and in the rest it was regarded as “constipation of pregnancy.” Lactulose was prescribed for 4 weeks. Stool frequency increased after a week and reached an optimum (6 times per week) after 2 weeks of treatment; The consistency of stool was normalized. “Good” and “very good” overall assessment of the effect of lactulose was given by 84% of attending physicians and 81% of patients [14].
Lactulose can be recommended for widespread use in rheumatological practice. In patients receiving NSAIDs and cytotoxic drugs, chronic constipation is often associated with hemorrhoids, anal fissures, complicated by dangerous bleeding or infection. It is preferable for such patients to be prescribed laxatives that do not have an irritating effect on the intestinal mucosa.
In the work of A.E. Karateev studied the tolerability of lactulose (Normaze) in patients with rheumatic diseases and chronic constipation. The study included 50 patients. The initial dose of lactulose was 30 ml at night, with subsequent adjustment - 15–60 ml per day; Duration of treatment – 2 weeks. In two patients, lactulose was discontinued due to undesirable effects (increased hemorrhoidal bleeding, severe flatulence). Normalization of stool was achieved in a quarter, significant improvement in 19 (39.6%) patients. The general well-being of patients improved [15].
It should be noted that in randomized studies of the effectiveness and safety of lactulose for chronic constipation in adults (including the elderly), the maximum duration of treatment was 12 weeks [16, 17]. New studies are needed on the safety of the drug with longer use. According to the instructions for lactulose preparations, when taking it for 6 months or longer, it is necessary to control the content of potassium, chlorides and carbon dioxide in the plasma, since long-term diarrhea can lead to disturbances in water and electrolyte balance.
In children, constipation often leads to the development of encopresis - fecal incontinence, inability to control bowel movements, and is also very often combined with delayed gastric emptying and pathological gastroesophageal reflux [18].
Many studies have been devoted to assessing the effect of lactulose in acute or chronic constipation in children, both in Russia and abroad. However, the lack of large randomized trials currently does not allow for a meta-analysis and the development of strict recommendations on dosage and duration of treatment [19].
In the study by L.N. Tsvetkova et al. 135 children aged from 1 to 15 years with constipation duration from 1 week to 4 months participated. The majority were patients aged 1 to 3 years. Triggering factors in the development of acute constipation were the prescription of medications, intestinal infections, changes in habitual lifestyle, etc. Children 1–6 years old were prescribed lactulose (Normaze) 5–10 ml 2–3 times a day, over 6 years old – 10–15 ml 2-3 times a day until stable regular bowel movements are achieved. In 121 children (89.6%) a positive effect was obtained within 7–12 days from the start of therapy; at the same time, abdominal pain and other complaints associated with constipation resolved; in a significant proportion of cases, normalization of the microbial composition of the microflora of feces was noted [20]. The use of lactulose and normalization of stool in children are accompanied by positive dynamics in the manifestations of reflux disease, reducing the frequency of its relapses and the development of severe complications [18].
Experiments with manometry have shown that after oral or rectal administration of lactulose, a decrease in gastric tone is observed and its ability to stretch increases; this effect appears to be of a reflex nature [21].
Lactulose in the treatment and prevention of hepatic encephalopathy
Another important area of application of lactulose is the treatment and prevention of hepatic encephalopathy (HE).
The therapeutic mechanism of action of the drug is not limited to the ability to increase the excretion of ammonia by changing the intestinal pH and laxative effect. In all likelihood, the prebiotic potential of lactulose is also important: by maintaining the mass of saccharolytic bacteria, the ammonium-producing population of intestinal microorganisms is suppressed. Some probiotics also exhibit these mechanisms of action, although evidence is currently insufficient [22, 23]. According to modern concepts, the development of PE is associated with impaired permeability of the intestinal barrier, changes in intestinal microbiocenosis and secondary inflammation. Liver cirrhosis, especially complicated by PE, is accompanied by significant changes in fecal microflora. The quantitative content of some of them (families Alcaligeneceae, Porphyromonadaceae, Enterobacteriaceae) in feces is associated with the severity of brain dysfunction and signs of inflammation [24].
In the intestine, ammonia is formed primarily as a result of bacterial deamination of amino acids. The use of antibiotics as first line of therapy can lead to the selection of resistant strains of ammonium-producing bacteria, and their use is not always justified. Non-absorbable disaccharides - lactulose, lactitol - as a result of laxative action and gas formation, cause rapid evacuation of bacteria and ammonia [25].
The effect of lactulose in the treatment of clinically manifest stages of PE has been shown in numerous works by domestic and foreign authors; lactulose has earned a reputation as an effective and reliable agent in the management of such patients. However, it should be noted that there is a lack of well-designed controlled studies on this issue.
In 2004, the Cochrane Hepato-Biliary Group published a systematic review regarding the effects of non-absorbable disaccharides (lactulose and lactitol) in hepatic encephalopathy. The analysis included 30 randomized trials that compared the effectiveness of lactulose and the natural disaccharide lactitol, placebo, antibiotics, and no intervention. The analysis showed that, compared with placebo or no intervention, administration of nonabsorbable disaccharides had no significant effect on mortality (OR death (RR) 0.41; 95% CI: 0.02–8.68). The results may have been influenced by methodological shortcomings of the studies. Disaccharides significantly contributed to reducing the severity of HE (OR no improvement 0.62; 95% CI: 0.46–0.84). The authors concluded that there is insufficient high-quality research evidence to definitively confirm the effectiveness of disaccharides in the treatment of PE [26].
Despite such uncertain data from a meta-analysis (2004), lactulose is included in modern recommendations for the treatment of type C HE (developing against the background of liver cirrhosis), in which hyperammonemia has an undoubted pathogenetic significance. Treatment of acute hepatic encephalopathy due to cirrhosis of the liver includes, among other things, the administration of lactulose in enemas (300 ml of syrup in 700 ml of water, trying to fill the entire colon) or through a naso-gastric tube (in case of deep encephalopathy). For oral administration, an initial dose of 45 ml and dose titration hourly until stool appears (usually 15–45 ml over 6–12 hours) are recommended; it is possible to replace lactulose with a non-absorbable antibiotic (neomycin, rifaximin).
In chronic encephalopathy against the background of liver cirrhosis (in the pathogenesis of which, apparently, hyperammonemia is even more important), the dose of lactulose is selected in such a way as to achieve 2-3 bowel movements per day and a soft stool consistency. Usually, 15–30 ml of syrup is first prescribed 2 times a day, then they switch to an individually selected regimen. Antibiotics are classified as reserve drugs in cases where the effect of lactulose is insufficient or it is poorly tolerated. A combination of lactulose, antibiotics, and zinc preparations is possible [27, 28, 29].
In recent years, close attention has been paid to the problem of so-called “minimally expressed” hepatic encephalopathy, in which brain dysfunction is detected only with special neuropsychological testing and instrumental studies. This form carries an increased risk of developing manifest PE, reduces the reaction rate, and can limit the patient’s daily activity.
M. Luo et al. published a meta-analysis of 9 studies (total number of participants 434) that examined the effect of lactulose in minimally severe PE. According to neuropsychological testing, lactulose significantly improved reaction time and attention (OR no improvement 0.52; 95% CI: 0.44–0.62; p
The effect of lactulose on intestinal microbiocenosis
Lactulose exhibits prebiotic properties, stimulating the growth of bifidobacteria and some lactobacilli. An increase in the biomass of saccharolytic bacteria appears to potentiate the laxative effect.
Unlike many probiotics, the therapeutic and preventive effect of lactulose is not reduced by antibiotic therapy.
A placebo-controlled study by J. Ballongue et al was devoted to studying the effect of lactulose and lactitol at a dose of 20 g per day on the growth of microorganisms in the colon in 36 healthy volunteers. With the use of both prebiotics, an increase in the mass of saccharolytic bacteria, a decrease in the activity of procarcinogenic enzymes and ureases in feces, an increase in the total content of SCFA, a slight decrease in pH and an increase in water content in feces were noted [32].
In the work of O.N. Minushkina et al. It has been shown that in case of duodenal ulcer, the administration of standard triple anti-Helicobacter therapy for 12 days in combination with lactulose (Normaze) is accompanied by improved tolerability of treatment. The frequency of bloating, the development of diarrhea and the identification of signs of disturbances in the composition of the intestinal microflora are reduced. The latter was assessed based on the study of the absolute concentration of SCFAs (C2–C6) and their profiles, as well as the values of anaerobic indices and the total relative content of isoacids in feces. The authors note that initially there was a decrease in the content of acetic acid in the patients’ stool, which may be explained by a decrease in the activity of obligate saccharolytic intestinal microflora. At the same time, the examined groups of patients were characterized by a SCFA profile indicating an increase in the activity of bacteroides, clostridia, eubacteria, fusobacteria, and coprococci [33].
Some studies have shown the ability of lactulose to suppress the growth of Salmonella, Shigella, Clostridia, Proteus, Klebsiella and Candida fungi, probably by reducing the pH of the environment and stimulating the growth of saccharolytic bacteria [34]. The experiment showed that if the number of viable pathogenic bacteria in the presence of ciprofloxacin decreased by approximately 100 times, then when ciprofloxacin was co-administered with lactulose, it decreased by 1000 times. In addition, a positive effect of lactulose on the spreading ability of neutrophils and mononuclear phagocytes has been established [35]. Lactulose (Normaze) is recommended to be prescribed during the period of early convalescence, with an emerging resolution of diarrhea and a decrease in symptoms of intoxication.
Y. Bouhnik et al. compared the effect of two osmotic laxatives - lactulose and polyethylene glycol - on the intestinal microbiocenosis in the treatment of chronic idiopathic constipation. The composition of fecal microflora was assessed. A multicenter, parallel-group, randomized controlled trial included 65 patients with idiopathic constipation. Patients received powdered lactulose or PEG-4000. In the first week the dose was fixed (20 g at night), during the next 3 weeks the dose could be adjusted based on the assessment of effect and tolerability (10–30 g/day). Bacteriological analysis of stool was carried out one day before the start of therapy and on the 21st and 28th days of treatment. The effectiveness and tolerability of laxatives was similar in both groups. In the group receiving lactulose, there was an increase in the population of bifidobacteria (p = 0.04), lactase activity (p
Considering the effectiveness of lactulose as a prebiotic and the high safety of its use, some authors recommend prescribing it not only for intestinal infections (in particular, salmonellosis), but also for patients with hemoblastosis during high-dose polychemotherapy [37].
Lactulose has been proposed to be used for sanitization of the birth canal (prevention of candidiasis and intrauterine infection of the fetus), prescribed 2–3 weeks before birth [38].
In their review article, S. Macfarlane et al. emphasize: despite the small number of randomized controlled studies assessing the probiotic effect of lactulose, oligofructose and galactooligosaccharides, promising results from animal experiments have been obtained, indicating that these substances have a distinct anti-inflammatory effect in the intestine and significantly improve calcium absorption. Perhaps in the future they will find application in the treatment of inflammatory bowel diseases and calcium metabolism disorders [39].
Domestic pediatricians recommend the use of lactulose in order to normalize intestinal functions in formula-fed children of the first year of life and in premature infants in the first month of life with various concomitant pathologies [40, 41].
Various aspects of the therapeutic and preventive effects of lactulose in the treatment of constipation, liver and intestinal diseases continue to be actively studied; The website www.clinicaltrials.gov lists numerous clinical trials currently underway. The continued interest in this drug underscores its relevance in various areas of clinical practice.
Beneficial properties of lactulose, their effect on the body
Perhaps the main advantage and main property of lactulose is the ability to suppress harmful bacteria.
An undeniable property, confirmed by experts, is the ability of lactulose to rid the body of toxic substances and harmful enzymes, such as ammonia, skatole, nitroreductase. Often used as a laxative. Thanks to lactulose, calcium is better absorbed, which significantly increases bone strength.
Reducing disorders and disorders of the intestines is one of the important conditions for human health. A sufficient content of lactulose in the human body contributes to the full functioning of the intestines by improving the microflora.
Another useful property of lactulose is its anti-carcinogenic effect. Lactulose has proven itself well as a preventative against colon cancer. Lactulose is necessary to stimulate the growth of healthy microflora.
Interaction with other elements
Lactulose interacts in the body with microelements - calcium, magnesium, zinc, iron. Interacts with cholesterol and bile acids.
At the same time, cholesterol levels in the blood are normalized, and the synthesis of bile acids is also optimized. In addition, the absorption of magnesium, zinc, calcium and iron improves.
Signs of lack of lactulose in the body
- sudden weight loss;
- frequent constipation;
- aching pain in the abdominal area;
- colicky sharp pain in the navel area;
- nausea;
- vomit;
- metabolic disease;
- disruption of the digestive system.
Signs of excess lactulose in the body
- flatulence;
- diarrhea;
- sudden weight gain;
- infectious diseases of the urinary system.
Factors influencing the content of lactulose in the body:
Lactulose is not produced in our body and comes to us with food. To maintain normal levels of lactulose in the body, a complete, balanced diet and nutrition that includes foods containing it is sufficient.
In addition, today there is a huge selection of medications containing lactulose. Most often, such drugs have a minimal number of contraindications and are approved for use from birth.
Lactulose for beauty and health
This substance is included in the list of food additives that increase human immunity and improve metabolic processes in the body. Lactulose promotes rapid absorption of calcium. As you know, calcium promotes proper and healthy growth of hair, nails, and teeth. Accordingly, consuming products containing lactulose has an excellent effect on appearance and internal sensations.
When consuming at least 3 mg of lactulose per day, the gastrointestinal tract, genitourinary system, joints and skin are completely healed. All this allows you to look healthy and feel much better.
Today, lactulose is also used in the cosmetics industry, which helps rejuvenate and restore the condition of the skin. The smallest newborns receive lactulose from their mother's milk, which guarantees proper growth and healthy functioning of the digestive organs of infants.
Attention! The information is for informational purposes only and is not intended to make a diagnosis or prescribe treatment. Always consult a specialized doctor!
Tatyana Eliseeva chief editor of the Food+ project
Ask a Question
Rating:
7.7
/10
Votes: 3
Usefulness of material 8
Reliability of information 8
Formatting of Article 7
Prebiotic requirement
Lactulose can increase the concentration of beneficial bifidobacteria in the body by more than 10 times, and reduce the number of harmful microorganisms by almost a hundred times. But for this you need to consume foods or dietary supplements containing a prebiotic every day. As a result of the experiments, it was determined that 3-4 g of the substance is enough for adults to achieve the effect.
People with:
- chronic constipation;
- disruptions in the functioning of the gastrointestinal tract;
- pathogenic intestinal microflora;
- liver dysfunction;
- high cholesterol;
- improper metabolism.
Diabetes, high acidity in the stomach and low acidity in the intestines are good reasons not to abuse fermented milk products and other foods containing lactulose in high concentrations.
Deficiency Symptoms
You can understand that the body does not have enough lactulose by looking at several of the most common symptoms. The most common and most important symptom is regular constipation, and to eliminate the problem it is enough to treat the body with a prebiotic for several days. Other symptoms of dysbiosis (which is most often a consequence of lactulose deficiency) may include:
- nausea;
- vomiting;
- weight loss;
- stomach ache.
Well, in total, all these disorders lead to disruption of metabolic processes and the function of the digestive organs.
Properties of lactulose
As a result of almost a century of research, scientists have discovered that lactulose has a range of beneficial properties for humans, in particular:
- Activates bifidobacteria.
Japanese researchers have determined that 3 grams of lactulose consumed daily for 14 days can increase the number of bifidobacteria several times. The experiment recorded an increase from 8.3% (of the total number of bacteria) to 47.4% within two weeks. Along with the growth of beneficial microflora, the number of harmful bacteria has decreased.
- Improves the absorption of minerals.
Taking lactulose promotes more active calcium absorption. Scientists made these conclusions after observing rats with osteoporosis. When feeding them lactulose, they recovered faster from bone fractures.
- Activates liver function.
Impaired bowel function leads to the accumulation of ammonia in the body, which has a toxic effect on the liver, and it loses its ability to eliminate toxins. Lactulose neutralizes part of the ammonia (from 25 to 50 percent) and restores the detoxifying functions of the liver.
- Fights carcinogens and toxins.
Animal experiments have proven the antibacterial and immunological effect of lactulose. It helps eliminate carcinogens and toxic metabolites from the body, improves the general condition of the body in case of liver cirrhosis by strengthening the immune system. This effect is achieved due to the activation of bifidobacteria, which require lactulose for growth. It is suggested that this prebiotic may be an effective preventive agent against colon cancer.
- Treats constipation.
Lactulose has many properties that result in the prevention of constipation. By binding water, reducing intestinal acidity and stimulating peristalsis, lactulose plays the role of a gentle laxative (effective for 1-2 days). These abilities of the substance allowed pharmacists to actively use it in many drugs for constipation.
- Affects the formation of bile acids.
In healthy people consuming lactulose, there is a decrease in the production of secondary bile acids in the intestines.