Historical information
The first experimental studies, which later led to the discovery of vitamin A, belong to Stepp (1909).
Studying the question of the ability of the animal body to synthesize the necessary components, he showed that food, quite sufficient to ensure the normal growth and development of mice (bread and milk), loses its nutritional qualities after being treated with alcohol and ether. Adding the extract obtained from it to the extracted food again made it suitable for nutrition. Stepp believed that such processing removes from food those lipids that the mammalian body is not capable of synthesizing. This problem was further developed in the work of Collum and Davis (1913), who conducted a study on young, growing rats. Feeding animals with a food mixture of specially processed products - protein (casein), carbohydrates and a mixture of salts led to growth cessation, which resumed after adding butter or an ethereal extract of egg yolk to the diet. Reporting more than half a century later about the individual stages of the discovery of vitamins A and D, Collum (1967) pointed out the role played in these discoveries by the work of N.I. Lunin, carried out back in 1880. In studies published in 1913, Osborne and Mendel confirmed that the addition of butter to an artificially compounded food mixture ensured normal growth of animals. They also isolated the active fraction of butter and drew attention to the fact that in young rats that received artificially formulated food mixtures, in addition to growth arrest, eye diseases were observed, which were cured after adding butter or cod oil to the food.
Collum and Davis found that the active principles of butter and fish oil are associated with the unsaponifiable fraction and gave it the name “fat-soluble factor A.” In 1916, Drummond named this factor vitamin A. Subsequently, it was shown that a number of plant products have an effect similar to that of vitamin A. Such activity of such products is associated with the presence of plant pigments in them - carotenoids. According to Steenbock, plants that are richest in carotenoids also have the most pronounced A-vitamin activity, and crystalline carotene isolated from plants is able to support the normal growth and development of animals receiving food deprived of vitamin A. However, all these studies did not provide a satisfactory explanation of the nature of the connection between vitamin A and the yellow plant pigment carotene. The nature of this connection was established by Moore (1930), who showed that carotene contained in food is converted into vitamin A in the body and is thus its biological precursor. This was confirmed later when the chemical structure of carotene and vitamin A became known.
What to eat?
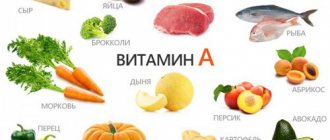
The highest levels of retinol are found in fish oil and beef liver. There is enough of it in dairy products - milk, cream, butter and cheeses, as well as chicken eggs.
Almost all bright yellow and red vegetables and fruits, as well as dark green leafy crops such as spinach, broccoli or green onions, are rich in carotenoids. There are carotenoids in legumes. Together with fats, beta-carotene is absorbed 30 percent better. But only if it enters the body on an empty stomach, so this is not a reason to consume excess fat. For normal absorption of beta-carotene, the fats that a person receives during the day from food are sufficient.
Physicochemical properties and structure
Carotenoids and carotenes
Carotenoids belong to a large group of hydrocarbon compounds - pigments synthesized by higher plants, fungi, and bacteria. According to their structure, carotenoids can be divided into a number of groups: carotenoids themselves, hydroxyl-containing carotenoids, carotenoids containing carbonyl groups, etc. Carotenoids themselves are designated by the term “carotenes”. Carotenoids of other groups, containing oxygen in their molecule, should be considered as derivatives of carotenes. Carotenoids and carotenes are capable of forming structural and spatial isomers.
The undoubted and so far only indicator of the biological value of carotenoids is their ability to be converted in the body into vitamin A. Carotenoids capable of such conversion are collectively called provitamins A. These include structural isomers of carotene - alpha, beta and gamma carotenes.
The most common structural isomer is beta-carotene, the molecule of which consists of two beta-ionone rings connected by an aliphatic chain having 9 unsaturated double bonds. One such bond is found in each ionone ring. Alpha-carotene, with the same structure of the aliphanic chain, contains only one beta-ionone ring, while the second ring is replaced by an alpha-ionone ring. Gamma-carotene contains 12 unsaturated double bonds, one beta-ionone ring and an open ring at the other end of the molecule.
The provitamin activity of structural and spatial isomers of carotene is different. The trans-transform of any isomer has the most pronounced provitamin activity. Among the individual structural isomers, beta-carotene is the most active, the activity of which is taken as 100%. Compared to beta-carotene, the activity of alpha and gamma carotene and cryptoxanthin is 53, 27 and 57%, respectively. The lower activity of cis-isomers compared to the trans-trans form can be explained by the fact that the carotenoid molecule, as a result of trans-trans isomerization, loses its original structure, which hinders the action of the enzyme system or systems involved in the conversion of this carotenoid into vitamin A.
Vitamin A and its derivatives
The chemical properties and structural formula of vitamin A were established back in 1931. At the same time, it was shown that it is an unsaturated alcohol with the empirical formula C20 H30 O, with five double bonds - one in the beta-ionone ring and four in the aliphatic side chain. Crystalline preparations of vitamin A were obtained in 1937. Vitamin A is a cyclic unsaturated monohydric alcohol that is soluble in most organic solvents, unstable in the presence of atmospheric oxygen, sensitive to light and heat, forms ethers and esters, most of which are more stable than itself vitamin A.
When oxidized in the body, vitamin A alcohol (retinol) is converted into vitamin A aldehyde (retinal). In addition to vitamin A alcohol, its esters and aldehyde, natural derivatives of vitamin A include 3-dehydrovitamin A, or vitamin A2, and some stereoisomers of these vitamins. Apparently, vitamin A acid (retinoic acid) can also be considered a natural compound of vitamin A.
Physicochemical properties and biological activity of vitamin A and its derivatives
| Vitamin A and its derivatives | Molecular melting point weight | Absorption maximum in standard in nm | E1 cm at 328 nm in the reference | Biological activity of ME/gXI-6 | |
| Alcohol | 286,4 | 64 | 324-325 | 1780 | 3,33 |
| Esters: | |||||
| acetic | 328,5 | 57-58 | 326 | 1510 | 2,91 |
| palmitic | 524,8 | 27-28 | 325-328 | 940 | 1,6 |
| p-phenylazobene- | |||||
| ashy | 494,6 | 80 | 330 | 1550 | |
| amber | 654,9 | 77-78 | 325-328 | 1240 | 2,5 |
Physiological action of vitamin A
Vitamin A absorption
The absorption of vitamin A is a complex process, including emulsification and hydrolysis of its esters in the lumen of the gastrointestinal tract, adsorption of retinol by the absorption border and its transport into the cells of the mucous membrane, re-esterification of retinol in them and the subsequent entry of vitamin A into the liver. Vitamin A absorption occurs mainly in the small intestine, mainly in its upper section.
Vitamin A under normal conditions, when consumed in physiological doses, is absorbed almost completely. Thus, 93% of vitamin A acetate orally administered to chickens was absorbed within 1 hour, 4% of the vitamin not absorbed by this time was found in the wall of the stomach and intestines, and 3% in their contents. However, the complete absorption of vitamin A largely depends on the amount taken. In particular, when the dose of vitamin A administered orally was increased from 3,000 to 100,000 IU, the relative amount of vitamin A absorbed decreased from 100% to 10%. This decrease is apparently associated with increased oxidation and disruption of the mechanisms of active absorption of vitamin A in the intestine, which is due to adaptive mechanisms aimed at protecting the body from vitamin A intoxication.
Ingestion of fatty foods, as well as stimulation of the digestive process, improves the absorption of retinol, which is consistent with the beneficial effect of bile on the absorption of vitamin A. This was convincingly shown in rats with a bile duct fistula, in which the absence of bile sharply reduced the absorption of vitamin A in the intestines.
Emulsification of retinol is a necessary step in the process of its absorption in the gastrointestinal tract.
Natural sources of vitamin A contain it primarily in the form of esters. In this regard, the body receives mainly vitamin A esters with food, mainly in the form of palmitate.
Hydrolysis of vitamin A esters in the intestine is carried out by enzymes of the pancreas and epithelial cells of the small intestinal mucosa.
Bile acids are involved in many phases of vitamin A absorption: emulsification, hydrolytic cleavage of retinol esters, solubilization of hydrolysis products and their transport to intestinal epithelial cells. It is also possible that they take a certain part in the re-esterification of retinol inside the epithelial cells of the mucous membrane. Bile acids also apparently prevent the oxidation of vitamin A and its esters, as well as carotene in the intestinal contents and thereby increase their digestibility.
Regardless of the type of ester bond of vitamin A present in food or pharmacological preparations, upon absorption in the intestine, complete hydrolysis of these esters occurs and free retinol enters the epithelial cells of the mucous membrane. The next stage in the metabolism of vitamin A is the re-esterification of retinol in epithelial cells with the formation of predominantly its higher esters, mainly retinol palmitate.
As is known, vitamin A absorbed in the intestines is transported to the liver and other organs mainly through the thoracic lymphatic duct. Consequently, the detection of vitamin A in the thoracic lymphatic duct predominantly in the form of its higher esters after A-vitaminization may indicate that the site of re-esterification of retinol is intestinal epithelial cells.
It should be noted that intestinal epithelial cells perform another important function in the process of assimilation of natural forms of vitamin A: in them, low-active cis-forms of vitamin A, contained in some foods, are converted into highly active transforms.
Thus, in the epithelial cells of the mucous membrane of the small intestine, re-esterification of retinol occurs, which is formed as a result of the hydrolysis of nutritional ester forms of vitamin A under the influence of retinyl ester hydrolases of the pancreas and intestines. These resynthesized retinol esters (mainly retinyl palmitate) are attached to specific aminoproteins and transported as part of chylomicrons through the lymphatic system to the liver. It should be noted that some amounts of retinol and its esters taken are absorbed through the portal vein, and not just through the lymphatic system. In the liver, retinyl esters are released and hydrolyzed to form free retinol. Subsequently, free retinol in the liver is secondarily re-esterified and converted into retinyl palmitate, which is bound by liver proteins and forms a reserve form of vitamin A.
The absorption of vitamin A in the gastrointestinal tract is influenced by many factors: the composition of the diet, especially its protein and lipid components, the digestibility of food and the presence of oxidizing and reducing agents in it, the state of the gastrointestinal tract (in particular, the biliary function of the liver, hepatic - intestinal circulation of bile acids, secretory function of the pancreas and small intestine, integrity of the intestinal mucosa), the amount of vitamin A administered and the nature of the bond of its ester, hormonal status and physiological state of the body. Depending on the impact of these factors, a certain part of dietary retinol is excreted in feces without being absorbed in the digestive tract.
Thus, the presence in the diet of such a natural antioxidant as vitamin E, as well as sufficient secretion of bile acids, protects retinol from oxidative transformations and promotes its more complete absorption in the intestines. The presence of nitrates in the diet, on the contrary, leads to the destruction of vitamin A and disruption of its absorption in the gastrointestinal tract. Eating food, especially fatty foods, and sufficient secretion of bile and enzymes by the pancreas and intestines contribute to more complete absorption of retinol. Vitamin A in the form of emulsified and water-dispersed preparations is absorbed faster and more completely than in the form of oil solutions.
As already indicated, among nutritional factors, the protein composition of the diet has a significant impact on the absorption of vitamin A in the digestive tract.
Protein deficiency also has a significant effect on the absorption of carotene in the gastrointestinal tract. The study of this issue is of great practical importance, since carotene (mainly beta-carotene), being a provitamin A, widespread in nature, is one of the main sources of vitamin A in the diet of humans and animals.
The bulk of the absorbed carotene is already converted within the intestinal epithelial cells into vitamin A, which is then metabolized like retinol received from the outside. The central place in the metabolic transformations of vitamin A in general and in the process of its absorption in the intestine in particular is occupied by retinal, which is an intermediate product in the reactions of conversion of beta-carotene into vitamin A and the oxidation of retinol into retinoic acid.
Transport and distribution of vitamin A
The bulk of vitamin A absorbed in the gastrointestinal tract, mainly in the form of retinol palmitate, is transported to the liver, which is the main storage site for this vitamin. To meet the body's needs, reserves of vitamin A esters in the liver are hydrolyzed to form retinol, which, combining with a specific retinol binding protein, is transported to various organs and tissues.
In the blood, more than 90% of vitamin A is represented by retinol.
The specific carrier of vitamin A in the blood is the so-called retinol binding protein, which carries out its transport function in close interaction with the thyroxine-binding prealbumin fraction. It was then repeatedly confirmed that vitamin A is bound by retinol binding protein with a relatively low molecular weight, which then enters into a complex with a protein of much higher molecular weight - thyroxine-binding prealbumin and is transported in the form of a complex complex: retinol + retinol-binding protein + thyroxine-binding prealbumin.
The binding of vitamin A by retinol binding protein has significant physiological significance, which consists not only in solubilizing water-insoluble retinol and delivering it from the depot (liver) to target organs, but also in protecting the unstable free form of the retinol molecule from chemical degradation (for example, retinol becomes resistant to the oxidative effects of liver alcohol dehydrogenase). Retinol binding protein has a protective function in cases of high doses of vitamin A entering the body, which manifests itself in protecting tissues from the toxic, in particular membranolytic, effects of the vitamin.
Vitamin A intoxication occurs when retinol in the plasma and membranes is not in a complex with retinol binding protein, but in a different form.
The liver is not only the main depot of vitamin A, but also the main site of synthesis of retinol binding protein. The biosynthesis of this protein in the liver is carried out on ribosomes, as evidenced by the results of studying its subcellular distribution.
Small amounts of vitamin A are also localized in the small intestine, blood, heart, lungs, retina and cornea, spleen, thyroid gland, adrenal glands, pancreas, epidermis and sebaceous glands of the skin, renal pelvis, bladder mucosa, testes and sperm.
The content of vitamin A in the whole body, as well as in different organs and tissues, has been confirmed by seasonal and age-related changes and may depend on the dose, the nature of the solvent (fat or water emulsion of vitamin A) and the route of administration (oral or parenteral) of vitamin A.
Vitamin A is deposited in the liver only when there is sufficient intake from food and when the concentration of retinol in the blood is normal.
A certain part of vitamin A in the body is found in the membranes of cells and their organelles. Thus, vitamin A and carotenoids are found in the membranes of red blood cells, cells of the intestinal mucosa and organelles of liver cells. Vitamin A, localized in membranes, apparently plays a certain role in the regulation of their structure and functions.
Thus, the transport of vitamin A in the blood is carried out by a complex protein complex consisting of retinol binding protein - the direct carrier of retinol and thyroxine-binding prealbumin, which, when combined with retinol binding protein, protects the latter from glomerular filtration and excretion in the urine. The binding of vitamin A to these proteins is of great physiological importance in terms of solubilizing water-insoluble retinol, protecting it from rapid chemical breakdown and elimination in the urine, as well as in terms of delivering retinol from the depot to target organs and transferring it to specific receptor molecules of cells, which is necessary for the manifestation of specific metabolic functions of vitamin A in these organs and tissues. The concentration of proteins transporting vitamin A in blood plasma under normal conditions correlates with the body’s supply of vitamin A. The possibility of such a correlation is to a certain extent due to the fact that vitamin A is one of the regulators of the metabolism of its own transport proteins.
The metabolism and manifestation of the functions of proteins involved in the transport of vitamin A largely depend on the protein composition of the diet.
Under normal conditions, the level of vitamin A in the blood is maintained at a fairly constant level without significant fluctuations. A decrease in plasma retinol concentration can be observed only after complete depletion of vitamin A reserves in the liver. Even with a small reserve of vitamin A in the liver, as a rule, there is no decrease in the level of retinol in the blood.
Considering the constancy of the concentration of vitamin A in the blood, which is quite clearly maintained under normal conditions by various regulatory mechanisms, including retinol-transporting proteins, it can be assumed that it is with a normal content of vitamin A in the blood that the need for retinol in various organs and tissues is optimally met. It should, however, be noted that the need of different organs can be met at different concentrations of vitamin A in the blood. For example, the organs of vision can effectively accumulate the required amount of retinol even when its content in the blood is low compared to other organs. This is due to the specificity of retinol-binding cell receptors and the difference in the functions of vitamin A in different organs and tissues.
So, the transport of vitamin A in the body is carried out mainly by a specific protein complex consisting of retinol-binding protein and thyroxine-binding prealbumin. The secretion of transport proteins from the liver is regulated with the participation of vitamin A. The main depot of vitamin A is the liver, from where retinol enters the blood through the lamellar complex (Golgi complex) to meet the metabolic needs of organs and tissues. Protein deficiency disrupts the biosynthesis of retinol binding protein and thyroxine-binding prealbumin in the liver and leads to a decrease in their levels in the blood. Deficiency of transport proteins for vitamin A, which develops with protein deficiency, disrupts the mobilization of retinol from the depot and its transport to target organs. In this regard, with protein deficiency, the utilization of even existing retinol reserves is disrupted and the so-called protein deficiency functional hypovitaminosis A develops. Prevention and treatment of it should be carried out with mandatory correction of the protein composition of the diet.
Beneficial features
Each vitamin has its own function in the body. Retinol has several of them.
- It has a positive effect on the functioning of the visual organs. This is a means of preventing senile blindness.
- Vitamin A is essential for maintaining the integrity and function of skin cells, as well as the respiratory and digestive systems.
- Retinol plays an important role in the development of lymphocytes (white blood cells). They are key agents in the immune system response.
- Prescribed for pregnant women: participates in the growth of limbs, the formation of the baby’s heart, eyes and ears. Also responsible for growth hormone: a deficiency can provoke a birth defect.
- Considered a strong antioxidant. It has the ability to neutralize free radicals that lead to the development of chronic diseases (for example, diabetes).
- Retinol is the key to healthy bones. With enough of it, the risk of fractures is reduced by 6%.
Biological role
Vitamin A affects the barrier function of the skin, mucous membranes, the permeability of cell membranes and the biosynthesis of their components. The effect of vitamin A in these cases is associated with its involvement in protein synthesis.
Currently, the importance of vitamin A in the process of photoreception has been clarified in more detail.
The retina of most vertebrates contains two photoreceptor systems: the rod apparatus, sensitive to low light intensity, i.e. twilight vision and cone vision - adapted to high light intensity and for color vision. Photosensitive pigments, called rhodopsin, are chromoproteins consisting of a chromophore group - vitamin A-aldehyde (retinal) and a protein - opsin. The cone photoreceptor systems (iodopsin and cyanopsin) consist of the same chromophore groups connected to a protein that is structurally different from opsin. In the light, rhodopsin is broken down into the protein opsin and retinal; the latter transforms into a trans form; These transformations are associated with the transformation of the energy of light rays into visual stimulation. In the dark, the reverse process occurs - the synthesis of rhodopsin, which requires the presence of an active form of aldehyde - 11-cis-retinal, which can be synthesized from cis-retinol or trans-retinal, or the trans form of vitamin A with the participation of specific dehydrogenases and isomerase.
Under the influence of a quantum of light, rhodopsin, through a series of intermediate products (“orange” and “yellow” proteins), breaks down into opsin and allo-trans-retinal, which is an inactive form of vitamin A aldehyde. Allo-trans-retinal can be partially converted into active 11-cis -retinal under the influence of light (dotted arrow in the diagram). However, the main route of formation of 11-cis-retinal is the enzymatic conversion of the trans form of vitamin A into the cis form (under the action of isomerase), and its subsequent oxidation with the participation of alcohol dehydrogenase.
Distribution in nature and daily requirement
Vitamin A is found only in products of animal origin, mainly in ethereal form, in the form of palmitate.
The following animal products are richest in this vitamin: liver of cattle and pigs, egg yolk, whole milk, sour cream, cream. The liver and internal fat of some types of fish (halibut, cod, sea bass) and sea animals (whales, seals) are especially rich in vitamin A. The amount of vitamin A and carotene in these products is subject to seasonal fluctuations and depends on the feeding conditions of livestock and poultry. Typically, in summer and autumn, milk and eggs are richer in vitamin A and carotene than in winter and spring.
The main source of carotene in human nutrition is products of plant origin - vegetables, fruits, berries (carrots, red peppers, tomatoes, parsley, lettuce, spinach, apricots, sea buckthorn, rose hips, etc.). However, when using products containing carotene as sources of vitamin A, it should be borne in mind that their biological activity, taking into account the digestibility of carotene, is approximately 6 times less than the biological activity of vitamin A.
The daily requirement for vitamin A for an adult is 1.0 mg, for pregnant and lactating women 1.25-1.5 mg, for children and adolescents from 0.4 to 1.0 mg.
Contraindications and precautions
Consuming excess amounts of vitamin A can be dangerous to your health. With a balanced diet, the daily dose can be easily obtained without the use of specific additives, from ordinary products. For adults, the upper daily limit is 3,000 mcg (10,000 IU). Very high doses can cause severe poisoning and even death.
Overdose symptoms:
- Deterioration of visual function.
- Joint pain, bone pain.
- Lack of desire to eat.
- Nausea and vomiting.
- Photosensitivity.
- Baldness.
- Headache.
- Dry skin.
- Liver damage.
- Yellowing of the skin.
- Stunted growth.
- Dizziness.
- Skin itching.
Excessive amounts of vitamin A are dangerous during pregnancy. Overdose carries a risk to the health of the mother and fetus. There is evidence that hypervitaminosis of vitamin A increases the risk of developing lung cancer in smokers. Therefore, you need to take retinol supplements carefully and strictly follow the dosage.
Signs of severe vitamin A deficiency
Vitamin A deficiency develops if a person consumes few foods containing this substance. Alcoholism and malabsorption aggravate the situation. You can understand that the body is experiencing a lack of vitamin A by the following signs:
- Night blindness. This is the first signal of existing hypovitaminosis.
- Corneal ulcers. With severe vitamin A deficiency, vision can be lost completely.
- Immunodeficiency.
- Frequent respiratory infections. Among children with vitamin deficiency, there is a higher mortality rate from measles.
- Diarrhea.
- Impaired growth and bone formation.
- COPD, pulmonary emphysema. Obstruction most often develops in smokers.
Signs of excess vitamin A
Symptoms of acute vitamin A hypervitaminosis:
- Nausea.
- Headache.
- Decreased performance.
- Loss of appetite.
- Dizziness.
- Dry skin.
- Brain swelling.
Chronic hypervitaminosis of vitamin A can cause the development of osteoporosis, as well as birth defects in the fetus. In this regard, retinol derivatives are especially dangerous, so it is better for pregnant women to be prescribed beta-carotene.
People with an increased risk of lung cancer, smokers, and people whose bodies are exposed to asbestos should not take vitamin A supplements for a long time.
Methods for determining vitamin A and carotene
When determining the content of vitamin A in food products, biological objects and vitamin preparations, physicochemical, fluorometric, polarographic and histochemical methods, as well as the isotope dilution method, are used. The choice of any method is determined by the purpose of the study, the properties of the analyzed material, the expected content of vitamin A and carotene and the nature of the accompanying impurities.
For the quantitative determination of substances with vitamin A activity, the method of direct spectrophotometry can be used, based on the ability of these compounds to selectively absorb light at different wavelengths in the ultraviolet region of the spectrum. The direct spectrophotometry method is the simplest, fastest, quite specific and gives good results in determining the content of vitamin A and carotene in objects that do not contain impurities and have absorption in the same region of the spectrum. If there are substances that interfere with the determination, then this method can be used in combination with a chromatographic separation step. A method based on measuring the absorption of a vitamin A derivative, hydroretinol, formed in the presence of small amounts of mineral acids, has high sensitivity and specificity.
Compounds of the vitamin A group are characterized by the ability to form colored reaction products when interacting with a number of chemical substances: antimony chloride, trifluoroacetic acid, glycerol-1,3-dichlorohydrin, etc. The most widely used method for determining vitamin A by reaction with antimony chloride is the Kappa method -Price. But the disadvantage of this method is the instability of the developing color, making it difficult to determine.
When vitamin A interacts with glycerol-1,3-dichlorohydrin, a more stable compound is formed that maintains a constant color for 2-10 minutes. However, this method is inferior in sensitivity to the Carr-Price method: the color intensity of the resulting reaction product is 5 times weaker than in the reaction with antimony chloride.
The method using trifluoroacetic acid is interesting because it can be used for the separate determination of esters, alcohol, vitamin A acid, because the colored reaction products have maximum absorption at different wavelengths.
There is a method for determining the concentration of vitamin A (retinol) and retinol binding protein in plasma and liver - this method is high pressure liquid chromatography (HPLC), which makes it possible to accurately, quickly and with high reproducibility determine the individual metabolites of vitamin A.
When the concentration of vitamin A in plasma is above 0.7 µmol/l (20 µg/dl), deficiency cannot occur, but if the concentration is below 0.7 µmol/l, then deficiency occurs.
In experimental animals, an indirect method is used to determine the concentration of retinol in the liver, the essence of which is to assess the change in the concentration of retinol in plasma after oral administration of a certain dose of retinol acetate.
References
- Zaichik, A.L., Churilov, L.P. Pathochemistry. Endocrine and metabolic disorders. 3rd edition, 2007. - T. 2.
- Tanumihardjo, S., Mokhtar, N., Haskell, M. et al. Assessing the Safety of Vitamin A Delivered Through Large-Scale Intervention Programs: Workshop Report on Setting the Research Agenda, 2021. - Vol. 37(2). — P. 63-74.
- Debelo, H. Vitamin A. Adv Nutr., 2021. - Vol. 8(6). — P. 992-994.
- Maia, S., Souza, A., Costa Caminha, M. et al. Vitamin A and Pregnancy: A Narrative Review. Nutrients, 2021. - Vol. 11(3). - P. 681.
- Timoneda, J., Rodríguez-Fernández, L., Zaragozá, R. et al. Vitamin A Deficiency and the Lung. Nutrients, 2021. - Vol. 10(9). - P. 1132.
Clinical trial results
Visual symptoms
Characteristic symptoms of vitamin A deficiency in humans are eye lesions, including disorders of the retina, conjunctiva and cornea. The twilight vision disorder, known as night blindness, or hemeralopia, which deprives a person of orientation in space and the ability to move in the dark at dusk, is one of the early manifestations of vitamin A deficiency. Much later, the disorder of night vision is accompanied by lesions of the conjunctiva and cornea. The weakening of dark adaptation is associated with a decrease in the supply of vitamin A in the form of vitamin A-aldehyde to the retinal rods. Weakening of night vision long before the development of subjective manifestations of hemeralopia can be detected by scotometry, dark adaptation studies and electroretinography.
Morphological changes in the eye with vitamin A deficiency appear later than dark adaptation disorders. They arise as a result of keratinization of the epithelium of the conjunctiva, cornea and cessation of secretion of the lacrimal glands, which together leads to the development of xerosis. To more accurately describe the eye condition specific to vitamin A deficiency, it is recommended to use the narrower terms “conjunctival xerosis” and “corneal xerosis.” Conjunctival xerosis appears as one or more patches of dry, non-wetting conjunctiva. The spots are best seen in side lighting. Typical xerosis may be accompanied by varying degrees of thickening of the conjunctiva, its wrinkling and pigmentation. There is a decrease in the sensitivity of the bulbar conjunctiva, photophobia, and a feeling of the presence of a foreign body in the eye (“sand sensation”). Along with general changes in the conjunctiva, limited xerotonic changes can be observed on it - Bitot's plaques located on the conjunctiva of the sclera.
In older children, adolescents and adults, eye changes are limited to xerosis. In contrast, in infants and children under 4 years of age, eye changes due to vitamin A deficiency often extend to the cornea. Damage to the cornea begins with xerosis, decreased sensitivity and progressive opacification. Subsequently, keratomalacia develops, passing into the stage of infiltration, ulceration, softening and perforation. Keratomalacia often results in complete or partial loss of vision.
The effect of hypovitaminosis on other organs
One of the clinical manifestations of vitamin A deficiency is skin changes known as follicular hyperkeratosis. The initial sign of skin changes is dryness and roughness of the skin, caused by increased keratinization of the surface epithelium and suppression of the activity of the sweat and sebaceous glands. Subsequently, skin changes occur according to the type of follicular hyperkeratosis and dryness is replaced by a papular rash. The rash occurs on the outer and lateral surfaces of the thighs, the back and lateral surfaces of the forearms, spreading further to the rest of the body.
In addition to the characteristic symptoms of vitamin A deficiency in humans and animals, symptoms such as growth inhibition, loss of body weight, and general exhaustion of the body also appear.
In cosmetology
Cosmetologists say: retinol is the gold standard in skin care. This is practically a magician who solves all problems (from acne to wrinkles). The positive effect is observed in the following:
- increased elastin production;
- stimulating the formation of new blood vessels;
- decreased activity of the sebaceous glands;
- reduction of sebum secretions;
- provoking the exfoliation of dead cells (a means of preventing clogging of pores).
Diagnosis of Vitamin A deficiency
To identify vitamin A deficiency in humans, the following is used:
- 1) determination of vitamin A content in the blood on an empty stomach and after a vitamin A load;
- 2) biomicroscopy of the cornea;
- 3) studies of dark adaptation;
- 4) visual field examination;
- 5) determination of the functional state of the retina using electroretinography;
- 6) examination of the condition of the skin and visible mucous membranes.
Much attention should be paid to carefully collecting information about the diet of the subjects over a long period of time and about the content of vitamin A in food. According to modern concepts, the content of vitamin A in 100 ml of blood in an amount of less than 10 mcg indicates insufficient, 10-19 mcg - low, 20 -50 mcg is acceptable and over 50 mcg is a high level in the blood.
What else is prescribed with this study?
Biochemistry 13 indicators
28.339. Ven. blood 1 day
3,490 ₽ Add to cart
Clinical blood test with leukocyte count and ESR (with microscopy of a blood smear to detect pathological changes) (venous blood)
3.9.1. Ven. blood 1 day
720 ₽ Add to cart
Complex blood test for vitamins (Vitamins A, D, E, K, C, B1, B5, B6)
4.26.1 Ven. blood 7 days
16,500 ₽ Add to cart
Combating vitamin A deficiency
Insufficient levels of vitamin A in the body can range from a borderline state, which is expressed in a decrease in the reserves of this vitamin without clinical manifestations, the presence of early or reversible clinical signs such as night blindness and conjunctival lesions, to a sharp decrease, manifested mainly by severe corneal lesions with a high probability of complete loss of vision. Therefore, a prevention program should be aimed at increasing vitamin A stores in the body or combating vision loss caused by vitamin A deficiency.
The purpose of the activity will depend on many factors, such as the severity of the problem, the availability of personnel, and technical and financial resources.
There are several strategic approaches to combat vitamin A deficiency; Specific interventions such as the distribution of vitamin A capsules and vitamin A fortification of consumer foods; and interventions such as nutrition education in schools and through the media, promotion of crop cultivation and consumption , rich in carotene, improving aspects of primary health care related to nutritional status.
The best results come from an integrated approach that combines short-term and long-term programs, which are usually mutually reinforcing. For example, periodic distribution of vitamin A capsules makes it possible to establish direct contact with patients and carry out health education work with them.
Author of the article: Associate Professor of the Department of Biochemistry, MBF RSMU, Ph.D. Adrianov Nikolay Vladimirovich. Especially for Electronic Medicine LLC.
Signs of deficiency
Vitamin deficiency is a pathological condition associated with a deficiency of a substance in the body. You can suspect something is wrong based on the following symptoms:
- deterioration of visual acuity;
- dry skin;
- respiratory tract diseases;
- long-term healing of wounds and skin abrasions;
- slow growth (in childhood);
- white spots on the oral mucosa;
- painful perception of bright light;
- dandruff;
- acne.;
- brittle nail plates.