Hepatocellular carcinoma is the most common type of primary liver cancer and is diagnosed in approximately 90% of cases. More than 600,000 new cases are diagnosed each year worldwide.
In the early stages - when there is one node in the liver no more than 5 cm or up to three nodes no more than 3 cm each - hepatocellular carcinoma is quite successfully treated with liver resection or transplantation, ablation techniques (radiofrequency ablation, RFA).
If cancer spreads beyond the liver, the prognosis worsens. The average survival of such patients is 4–6 months. There are not many effective treatments. For example, most intravenous and oral chemotherapy drugs do not improve quality of life or survival. Because chemotherapy drugs are broken down by hepatocytes, large doses are required and carry a high risk of serious side effects.
Currently, for unresectable liver cancer that has spread beyond the organ, targeted drugs, in particular Sorafenib (Nexavar), are prescribed as first-line therapy. It is a kinase inhibitor that inhibits cancer cell proliferation and angiogenesis, is well tolerated by most patients, and can be used for the long-term treatment of hepatocellular carcinoma.
Mechanism of action and effectiveness of Sorafenib
The drug is a low-molecular-weight multikinase inhibitor. It was obtained through a series of modifications to the experimental drug GK-00687. Sorafenib was approved by the US Food and Drug Administration (FDA) in 2006 for the treatment of advanced renal cell carcinoma and on November 19, 2008 for the treatment of advanced hepatocellular carcinoma.
The drug's FDA approval for the treatment of liver cancer follows the results of an international, randomized, placebo-controlled (phase III) trial that began in March 2005 and included patients with unresectable hepatocellular carcinoma in the United States, Europe, Australia, and New Zealand. 602 participants were randomly assigned to two groups, one of which received Sorafenib 400 mg twice a day, the other received placebo therapy.
The study ended in 2007 and survival rates were compared between the groups. In patients receiving the drug, it was 10.7 months, and in the placebo group - 7.9 months. Slower tumor progression was observed in patients treated with Sorafenib.
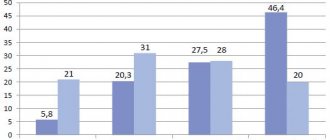
Previously, in the second phase of clinical trials, 137 patients took part; they received Sorafenib at the same dosage - 400 mg 2 times a day. 3 (2.2%) patients achieved a partial response, 8 (5.8%) had a minor response, and 46 (33.6%) showed stability for at least 16 weeks. Median survival was 9.2 months. The mechanism of action of the drug is based on the fact that Nexavar blocks different groups of kinases:
- Intracellular: BRAF (including mutants), c-CRAF, serine/threonine kinases.
- Located on the surface of cells: VEGFR-1, VEGFR-2 and VEGFR-3 (vascular endothelial growth factor receptors - this ensures inhibition of angiogenesis), RET, PDGFR-β, FLT-3, KIT.
The role of many drug target molecules in the progression of primary liver cancer has long been quite well studied:
- VEGFRs are endothelial growth factor receptors (VEGF). As a result of the interaction of the growth factor with the receptor, which is located on the surface of endothelial cells, autophosphorylation of the intracellular receptor tyrosine kinase occurs and a cascade of biochemical reactions is triggered, which leads to the induction of proliferation and migration of endothelial cells, protecting them from “aging” and apoptosis. Thus, VEGFRs are responsible for angiogenesis in both healthy and tumor tissue.
- Raf is a serine/threonine kinase that is activated by the membrane-bound protein Ras. This enzyme stimulates the transcription of genes in the nucleus, thereby causing various effects that promote the growth of a malignant tumor.
- PDGFR is a receptor that binds to platelet-derived growth factor (PDGF), a protein that plays an important role in angiogenesis by influencing endothelial cell trafficking and apoptosis.
Sorafenib is prescribed for advanced hepatocellular carcinoma at a dosage of 400 mg, 2 times a day. The drug has a bioavailability of 38–49%, its half-life is 25–48 hours, and it is metabolized in the liver approximately equally well in patients with Child-Pugh functional classes A and B (there are currently no data for class C).
Sorafenib - Nativ, 200 mg, film-coated tablets, 112 pcs.
Treatment with Sorafenib-native should be carried out under the supervision of a specialist with experience in the use of antitumor drugs.
During therapy with Sorafenib-native, it is necessary to periodically monitor peripheral blood counts (including leukocyte count and platelets).
The most common adverse reactions when taking sorafenib are skin reactions in the extremities (palmoplantar erythrodysesthesia) and rash. In most cases they are grade 1 or 2 and occur mainly during the first six weeks of sorafenib therapy. To treat skin toxic reactions, topical medications with symptomatic effects can be used. If necessary, temporarily stop treatment and/or change the dose of Sorafenib-native, or in severe or recurring cases of skin reactions, therapy with Sorafenib-native is discontinued.
The incidence of arterial hypertension may increase in patients treated with sorafenib. Arterial hypertension is usually mild or moderate in nature and is observed at the beginning of treatment and can be treated with standard antihypertensive drugs. During treatment with Sorafenib-native, blood pressure should be regularly monitored and, if necessary, its increase should be corrected with antihypertensive therapy. In cases of severe or persistent arterial hypertension or the occurrence of hypertensive crises despite adequate antihypertensive therapy, discontinuation of therapy with Sorafenib-native should be considered.
Taking sorafenib may increase the risk of bleeding. Heavy bleeding is rare. If any bleeding requiring medical intervention occurs, it is recommended to consider stopping treatment with Sorafenib-native. Given the potential risk of bleeding in patients with differentiated thyroid cancer, local treatment of tumor infiltrates of the trachea, bronchi and esophagus should be performed before prescribing sorafenib.
When warfarin and sorafenib are co-administered, rare episodes of bleeding or an increase in INR may occur. When warfarin and sorafenib are co-administered, regular determination of prothrombin time INR for clinical signs of bleeding is necessary.
In case of surgical interventions, it is recommended to temporarily discontinue therapy with Sorafenib-native for precautionary purposes. Clinical observations regarding the resumption of sorafenib after surgery are very limited. Therefore, the decision to restart therapy with Sorafenib-native after surgery should be based on a clinical assessment of the adequacy of wound healing.
If ischemia and/or myocardial infarction occurs, therapy with Sorafenib-native should be temporarily or permanently discontinued.
It has been established that the use of sorafenib leads to a prolongation of the QT/QTc interval, which may increase the risk of developing ventricular arrhythmias. Sorafenib-native should be used with caution in the following patients with current prolongation of the QTc interval or at risk of developing such a condition: with congenital long QT syndrome; receiving anthracycline therapy in a high total dose; taking certain antiarrhythmic drugs or other drugs leading to prolongation of the QT interval; and also in patients with electrolyte disturbances including hypokalemia, hypocalcemia or hypomagnesemia. When using the drug Sorafenib-native in such patients, periodic electrocardiographic monitoring should be carried out and the concentration of electrolytes (magnesium potassium calcium) in the blood plasma should be measured.
Gastrointestinal perforation is uncommon and has been reported in less than 1% of patients treated with sorafenib. In some cases, it is not associated with tumors in the abdomen. In case of perforation of the gastrointestinal tract, treatment with Sorafenib-native should be discontinued.
There are no data on the treatment of patients with severe hepatic impairment (Child-Pugh class C) with sorafenib. Since sorafenib is eliminated primarily by the liver, in patients with severe liver dysfunction, the effect of Sorafenib-native may be enhanced.
When using the drug Sorafenib-native in patients with differentiated thyroid cancer, it is recommended to monitor the concentration of calcium in the blood plasma. Patients with differentiated thyroid cancer, especially those with a history of hypoparathyroidism, experience more frequent and severe manifestations of hypocalcemia than patients with renal cell and hepatocellular cancer. There is evidence that in some patients with differentiated thyroid cancer receiving sorafenib, the concentration of thyroid-stimulating hormone in the blood plasma exceeded 05 mU/l. When using the drug Sorafenib-native in such patients, the concentration of thyroid-stimulating hormone should be monitored. The drug Sorafenib-native should be prescribed with caution together with drugs that are metabolized/excreted primarily with the participation of UGT1A1 (for example, irinotecan).
Concomitant use of docetaxel (75 or 100 mg/m2) and sorafenib (200 or 400 mg twice daily at 3-day intervals before and after docetaxel administration) is accompanied by an increase in docetaxel AUC by 36-80%. Caution should be used when sorafenib and docetaxel are co-administered.
Concomitant use of neomycin may result in decreased bioavailability of sorafenib.
Side effects
The drug is well tolerated by most patients. Possible side effects are due to the fact that Sorafenib is able to inhibit kinases not only in tumor cells, but also in healthy cells. Most often, 30–40% of patients experience diarrhea and dermatological disorders, such as palmoplantar erythrodysesthesia, rash, seborrheic dermatitis, stomatitis, alopecia, erythema multiforme. These side effects rarely require discontinuation of treatment; most often they can be managed with maintenance therapy and reducing the dose of the drug. Other side effects are relatively rare:
- increased fatigue - 18%;
- hypertension - 8–16%;
- pancreatitis - less than 1%.
Patients taking Sorafenib have an increased risk of bleeding and myocardial ischemia. The drug is contraindicated in pregnant and lactating women.
Sorafenib
special instructions
Treatment with sorafenib should be supervised by a specialist experienced in the use of anticancer drugs.
Carefully _
used for skin diseases, arterial hypertension, increased bleeding or a history of bleeding, unstable angina, previous myocardial infarction, simultaneously with irinotecan and docetaxel.
During therapy with sorafenib, peripheral blood counts (including leukocyte count and platelets) should be periodically monitored.
The most common adverse reactions with sorafenib were skin reactions in the extremities (palmoplantar erythrodysesthesia) and rash. In most cases they were grade 1 and 2 and appeared mainly during the first 6 weeks of treatment. To treat skin toxic reactions, topical medications with symptomatic effects can be used. If necessary, temporarily stop treatment and/or adjust the dosage of sorafenib or, in severe or recurrent cases of skin reactions, discontinue sorafenib therapy.
An increased incidence of hypertension has been reported in patients treated with sorafenib. Arterial hypertension was usually mild or moderate in nature, was observed at the beginning of treatment and was treatable with standard antihypertensive drugs. During treatment with sorafenib, blood pressure should be regularly monitored and, if necessary, its increase should be corrected with antihypertensive therapy. In cases where severe or persistent hypertension develops or hypertensive crises occur despite adequate antihypertensive therapy, discontinuation of treatment with sorafenib should be considered.
Sorafenib may increase the risk of bleeding. Heavy bleeding is rare. If any bleeding requiring medical intervention occurs, it is recommended that discontinuation of sorafenib treatment be considered. When warfarin and sorafenib were co-administered, some patients experienced rare episodes of bleeding or increased MHO. When prescribing warfarin and sorafenib together, regular determination of prothrombin time, MHO, and clinical signs of bleeding is necessary.
In case of surgical interventions, temporary discontinuation of sorafenib therapy is recommended from a precautionary position. Clinical observations regarding the resumption of sorafenib after surgery are very limited. Therefore, the decision to restart sorafenib therapy after surgery should be based on clinical assessment of the adequacy of wound healing.
If ischemia and/or myocardial infarction occurs, sorafenib therapy should be temporarily or permanently discontinued.
Gastrointestinal perforation is uncommon and has been reported in less than 1% of patients treated with sorafenib. In some cases, these events were not associated with tumors in the abdominal cavity. In the event of gastrointestinal perforation, treatment with sorafenib should be discontinued.
The use of sorafenib in patients with Child-Pugh class C hepatic impairment has not been studied. Because sorafenib is eliminated primarily by the liver, increased effects of the drug may be possible in patients with severe hepatic impairment.
In patients at risk of renal dysfunction, it is necessary to monitor water and electrolyte balance. The use of sorafenib in patients undergoing hemodialysis has not been studied.
Sorafenib should be used with caution concomitantly with drugs that are metabolized/excreted primarily by UGT1A1 (eg, irinotecan).
Caution is necessary when using sorafenib and docetaxel concomitantly.
Resistance
Sorafenib has helped to significantly improve the effectiveness of treatment of advanced primary liver cancer, but it is not without pitfalls. Many patients do not respond to the drug, and the reasons remain to be understood in detail, although some mechanisms of resistance are already known.
Some patients have primary resistance, meaning Nexavar does not help them initially. This is primarily associated with overexpression of genes encoding the epidermal growth factor receptor (EGFR) and its ligand. Studies show that the effectiveness of treatment depends on the activity of the MAPK family signaling pathway - Ras/Raf/MEK/ERK. c-Jun terminal kinase (JNK), another member of the MAPK family, has been considered as a biomarker of sensitivity to sorafenib.
Acquired resistance may be associated with the PI3K/Akt, JAK/STAT molecular pathways, epithelial-mesenchymal transition, hypoxia and changes in the tumor microenvironment, and epigenetic factors. The situation with autophagy, provoked by insufficient supply of nutrients to the tumor, is ambiguous. Experiments have shown that it promotes the development of resistance, but can also cause the death of tumor cells. This issue remains to be studied.
Modern possibilities of using sorafenib in solid tumors
Sorafenib is a small molecule inhibitor of several proteins with tyrosine kinase activity. The main targets of sorafenib are proteins of the RAF/MEK/ERK signaling pathway [1], however, it also has the ability to inhibit proteins of the RAF family (BRAF, CRAF), transmembrane protein C-kit, vascular endothelial growth factor receptors (VEGFR) ) (types 2 and 3) and platelet-derived growth factor receptors (PDGFR). The mechanism of action of the drug is due to the ability to inhibit these proteins: sorafenib inhibits the intracellular RAF/MEK/ERK pathway, the transmembrane C-kit-dependent pathway, and also suppresses angiogenesis by binding to VEGFR and PDGFR [2].
In preclinical trials, the drug showed effectiveness against a wide range of malignant tumors, which served as the basis for initiating phase I of its clinical trials.
The results of the phase I study were obtained in 2005. The data obtained from studying the effectiveness of sorafenib in doses from 50 to 1200 mg per day made it possible to establish the optimal regimen and dosage of the drug - 400 mg orally 2 times a day [3].
The most common side effects, regardless of severity, were weakness (40% of cases), anorexia (35%), diarrhea (34%), rash (27%) and hand-foot syndrome. The most common grade 3 or higher toxicities were hand-foot syndrome (8% of cases), weakness (6%), and diarrhea (4%). Typically, the severity of all types of side effects did not exceed grade 2 and was observed in 89% of patients. Toxicity was easily resolved by dose reduction or drug interruption. According to three different clinical short-term studies, when taking sorafenib at a dose of 400 mg 2 times a day, the severity of most side effects did not exceed grade 2. However, it should be noted that in the study of long-term sorafenib therapy, two patients had grade 3 alopecia.
Grade 3 cutaneous toxicity occurred in 9 of 14 patients receiving sorafenib 600 mg twice daily. Grade 3–4 myelosuppression and abnormal biochemical parameters were observed rarely. No severe hematologic, cardiovascular, hepatic, or renal toxicities were observed with sorafenib in these clinical trials. In four phase I studies, hypertension requiring medical intervention was observed in 5–11% of patients (grade 3 or 4 in 0–5% of cases). In addition, other types of toxicity were observed: mucositis, musculoskeletal pain, increased levels of liver enzymes. Cases of diffuse yellow pigmentation, as well as reversible dorsal leukoencephalopathy and reversible erythrocytosis have been described [3].
In phase I studies, sorafenib demonstrated antitumor activity; predominantly, the effectiveness of the drug was expressed in stabilization of the disease. In all 4 studies, patients were divided into groups and received the drug at a dosage of 200 mg twice daily or more. There was no convincing dependence of the effect of therapy on the dose of the drug. Among the cases of effective treatment, stabilization of the disease prevailed, its frequency was 28% (38/137), only two patients out of 137 had partial regression. In the extended phase I study, 5 patients (11%) showed long-term disease stabilization for more than 12 months. One patient with renal cell cancer experienced stabilization of the disease for about two years (prior to this, the patient had progression of the disease after three lines of treatment). In addition, two patients with renal cell carcinoma had stable disease lasting more than 1 year, and 50% of patients with hepatocellular carcinoma had stable disease lasting at least 6 months [3].
The results of phase I clinical trials served as the basis for continuing further study of the drug.
MJ Ratain et al. published the results of a phase II study, which included 202 patients with metastatic renal cell carcinoma [4]. Patients received 400 mg of sorafenib twice daily for 12 weeks, after which the effectiveness of treatment was assessed using radiological methods. Patients who experienced partial tumor regression of greater than 25% (79 of 202 patients) continued sorafenib; in patients with an increase in control lesions by more than 25%, sorafenib was discontinued. The remaining 65 patients who had a tumor reduction of less than 25% were randomized into 2 groups: patients in the first group received the study drug, patients in the second group received placebo.
Treatment was continued for 12 weeks. When analyzing the results, it turned out that in the sorafenib group, recruited from 65 patients who demonstrated a tumor reduction of less than 25% in the first stage of treatment, progression-free survival within 12 weeks was much higher compared to the placebo group - 50% (16 patients of 32) versus 18% (6 patients of 33). Progression-free survival was also longer in the sorafenib group (median 163 days) compared with placebo (median 41 days). Based on the results obtained, phase III clinical studies were conducted.
RJ Motzer et al. published data from an international multicenter, randomized, double-blind, placebo-controlled study of the effectiveness of sorafenib compared with placebo in patients with progression of renal cell carcinoma after first-line treatment [5]. Patients were randomized into two groups: a group of patients receiving sorafenib at a dose of 400 mg 2 times a day intermittently, and a placebo group. The study included 902 patients; the purpose of the study was to evaluate overall and disease-free survival. Patients in the sorafenib group were statistically significantly superior to patients in the placebo group in terms of disease-free survival (median: 167 days and 84 days, respectively).
The results obtained did not depend on the characteristics of the patients - objective condition, age, previous therapy and membership in any of the risk groups according to the Memorial Sloan-Kettering Cancer Center (MSKCC) scale. Due to the established efficacy of sorafenib, the study committee recommended pausing the study and initiating sorafenib therapy in patients in the placebo group, after which 48% of patients in this group began receiving sorafenib. As a result, when analyzing the results obtained after changing therapy in the placebo group, it turned out that sorafenib statistically significantly increased overall survival: 17.8 months compared with 14.3 months, respectively.
The effectiveness of sorafenib in renal cell cancer served as the basis for studying combinations based on it. S. Bracarda et al. studied the combination of sorafenib and interferon-alpha in high-dose and standard regimens [6]. A total of 63 patients were included in the study, making up 2 groups: group A - 31 patients received sorafenib at a dose of 400 mg 2 times a day + interferon-2-alpha 3 million units 5 days a week, group B - 32 patients received sorafenib at the same dose + interferon-2-alpha 9 million units 3 times a week. Partial response in both groups was 25.4%: 29% in group A and 22% in group B. Stabilization of the disease was observed in 41.3% of cases (26 patients): in 29% of cases in group A and 53% in group B. Disease progression was observed in 33.3% (21 people).
Currently, sorafenib is one of the standard effective treatment options for kidney cancer in the second and third lines of therapy. With low toxicity and significant antitumor effect, sorafenib can be recommended for use in all patients with renal cell carcinoma undergoing antitumor treatment. In combination with other drugs used for kidney cancer, sorafenib provides a significant increase in survival and long-term control of the disease.
Considering the effectiveness of sorafenib in several patients with hepatocellular carcinoma in phase I clinical trials, a phase II study was initiated. G. Abou-Alfa et al. studied the effectiveness of sorafenib at a dose of 400 mg 2 times a day in patients with hepatocellular cancer who had not previously received drug treatment [7]. During the study, which involved 137 patients, the following results were achieved: in 2.2% of cases (3 patients), partial regression of the tumor was observed, in 36.5% of patients (50 people), stabilization of the disease was noted. The duration of the achieved results was more than 16 weeks. The overall median time to progression was 4.2 months, but in patients with partial tumor regression it ranged from 12 to 14.5 months. Median overall survival was 9.2 months. The study showed good tolerability of treatment. Grade 3–4 toxicities were rare, with the most common types being asthenia in 9.5%, diarrhea in 8%, and hand-foot syndrome in 5%.
In 2007, the results of the randomized international multicenter placebo-controlled phase III SHARP trial were published [8], based on the results of which sorafenib was approved for use in hepatocellular cancer. The study included 602 patients with an objective ECOG (Eastern Cooperative Oncology Group) status of 0–2 points and liver function corresponding to class A on the Child–Pugh scale; After randomization, 299 of these patients were assigned to the sorafenib group and 303 to the placebo group.
At the time of the second interim analysis, overall survival of 321 patients had been studied. It turned out that the median overall survival in the sorafenib group was 10.7 months versus 7.9 months in the placebo group. On this basis, the study committee recommended early termination of the study, and all patients in the placebo group were then offered treatment with sorafenib. Disease control was achieved in 43% of cases, and the median time to progression was 5.5 months in the sorafenib group and 2.8 months in the placebo group. The incidence of grade 3 toxicity did not exceed 8% (diarrhea and hand-foot syndrome). The study results, published in 2008, changed the standard of care for hepatocellular cancer. Today, sorafenib is indicated for patients with this disease that is not amenable to surgery, liver transplantation, or in the presence of metastatic disease.
Currently, the drug is one of the few effective drugs for hepatocellular cancer, a disease for which until a certain time patients had no drug treatment options. The moderate toxicity profile and proven effectiveness allow us to consider sorafenib one of the few drugs of choice for hepatocellular cancer.
The effectiveness of sorafenib in thyroid cancer has been determined in several phase II studies. In 2008, G. Vandana et al. published data on the use of sorafenib in metastatic radioiodine-refractory thyroid cancer [9]. The study included 30 patients with metastatic or unresectable thyroid cancer who had disease progression after radioiodine therapy and one line of drug treatment (tyrosine kinase inhibitors, vaccine, or monoclonal antibodies). 7 patients (23%) had partial regression (lasting from 18 to 84 weeks), 16 patients (53%) had stable disease (lasting from 14 to 89 weeks). The median disease-free survival was 79 weeks. Toxicity in this study was low and similar to that in other studies of sorafenib.
M. Brose et al. in 2010, a multicenter, double-blind, randomized, placebo-controlled phase III study was initiated to study the efficacy and safety of sorafenib in patients with radioiodine-refractory differentiated thyroid cancer DECISION [10]. The final results of the study have not yet been published.
In phase I studies, sorafenib demonstrated efficacy against soft tissue sarcomas. Based on these data, a study of the drug for the treatment of sarcomas of various histological structures was initiated [11]. Patients were divided into several groups depending on the histological type of sarcoma. Each group included 12 patients; If, as a result of treatment, at least one case of an objective effect was observed among them according to RECIST criteria (Response Evaluation Criteria In Solid Tumors), an additional 25 patients were recruited. Only in the angiosarcoma group, an objective effect according to RECIST criteria was observed in 5 out of 37 patients (14%). The median disease-free survival was 3.2 months, the median overall survival reached 14.3 months.
Based on its mechanism of action (the ability to block transmembrane protein tyrosine kinase C-kit, inhibiting this signaling pathway), sorafenib was studied in preclinical trials, where it demonstrated efficacy in gastrointestinal stromal tumor (GIST) cell lines resistant to standard tyrosine kinase inhibitors [12]. This served as the basis for conducting phase II clinical trials of the use of sorafenib in GIST.
One of these studies included 38 patients with GIST who had disease progression after therapy with imatinib and sunitinib according to RECIST criteria [13]. 74% of patients had liver metastases at the time of inclusion in the study. Primary drug resistance to imatinib (IR) and sunitinib (RS) was observed in 3 and 59% of cases, respectively. Patients received sorafenib at a dose of 400 mg 2 times a day, the median number of cycles was 4 (1–40), 42% of patients received sorafenib for more than 6 months, 26% for more than 12 months. The drug dose was reduced in 61% of cases. Disease control was achieved in 68% of cases: partial tumor regression in 13% (1 patient with RI, 4 patients with MS), disease stabilization in 55% (3 patients with RI, 18 patients with MS). Median progression-free survival was 5.2 months and median overall survival was 11.6 months.
In 2011, A. Italiano et al. published a retrospective analysis of treatment results in 9 centers of patients with GIST resistant to therapy with imatinib and sunitinib [14]. The effectiveness of sorafenib in the 3rd and 4th line of treatment was studied, compared with imatinib or nilotinib, or maintenance treatment. It turned out that in the 3rd line of treatment, sorafenib achieved the longest disease-free survival of 6.1 months, without demonstrating an improvement in overall survival; in the 4th line of treatment, relapse-free survival was 7.5 months, and overall survival reached 11.5 months.
Thus, sorafenib can be considered as one of the options for effective drug therapy in the 3rd or 4th line of treatment of GIST. For patients whose disease has progressed after two or three lines of treatment with standard tyrosine kinase inhibitors, sorafenib may be an effective alternative to symptomatic treatment (primarily for fourth line treatment).
Sorafenib has also been effective in the treatment of desmoid tumors. M. Gounder et al. conducted a study that included 11 primary patients and 15 patients who received an average of 2 lines of treatment [15]. The median duration of treatment was 6 months (2–29). Efficacy was assessed according to RECIST 1.1 criteria, which included 24 patients. 6 out of 24 patients (25%) had partial regression, 17 patients (70%) had stable disease. Disease progression was recorded in 1 patient.
Given the limited range of drugs and the high probability of disease relapse after surgical treatment, the effectiveness of sorafenib, along with other drugs, gives patients who are not candidates for surgical treatment a significant additional option for drug therapy. For these patients, sorafenib may provide significant disease control benefits.
One of the promising directions is the study of combinations with the inclusion of sorafenib in the treatment regimen.
The efficacy of sorafenib in combination with capecitabine was studied in locally advanced and metastatic HER2-negative breast cancer in a randomized, double-blind, placebo-controlled, phase IIb trial. The study included 229 patients in need of first or second line treatment who received drug therapy in the following regimen: capecitabine 1000 mg/m2 ± sorafenib 400 mg twice a day. It was found that the addition of sorafenib to the treatment regimen significantly increases disease-free survival (6.4 versus 4.1 months) [16].
Sorafenib has been studied and found to be an effective treatment option as first, second and even third line treatment for a wide range of malignancies. For many patients who previously had no hope of any effective treatment, the drug has proven to be an opportunity to significantly increase survival, achieve disease control with a moderate and fairly narrow toxicity profile. The main and most relevant indications for the use of sorafenib are, of course, hepatocellular and renal cell cancer. However, as the data from these studies show, this is not the only niche for the drug, and it can be used to treat a number of malignant tumors.
Sorafenib continues to be studied in a large number of clinical trials, and a promising direction is its use in combination with various chemotherapy regimens and/or other targeted drugs.