Instructions for use ROACCUTAN
Roaccutane should only be prescribed by physicians, preferably dermatologists, who are experienced in the use of systemic retinoids and are aware of the drug's teratogenic risks. Both female and male patients should be given a copy of the Patient Information Leaflet.
To avoid accidental exposure of the drug to the body of other people, donated blood should not be collected from patients who are receiving or have recently (1 month) received Roaccutane.
It is recommended to monitor liver function before treatment, 1 month after treatment, and then every 3 months or as indicated.
A transient and reversible increase in liver transaminases was noted, in most cases within normal values. If the level of liver transaminases exceeds the norm, it is necessary to reduce the dose of the drug or discontinue it.
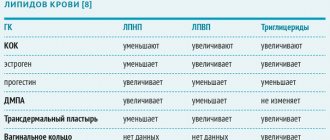
Fasting serum lipid levels should also be determined before treatment, 1 month after the start of treatment, then every 3 months or as indicated. Typically, lipid concentrations normalize after dose reduction or discontinuation of the drug, as well as with diet. It is necessary to monitor a clinically significant increase in triglyceride levels, since their rise above 800 mg/dL can be accompanied by the development of acute pancreatitis, possibly with a fatal outcome. In case of persistent hypertriglyceridemia or symptoms of pancreatitis, Roaccutane should be discontinued.
In rare cases, depression, psychotic symptoms and suicidal attempts have been described in patients treated with Roaccutane. Although their causal relationship with the use of the drug has not been established, special caution should be exercised in patients with a history of depression and all patients should be monitored for the occurrence of depression during treatment with the drug, if necessary, using consultations with appropriate specialists.
In rare cases, at the beginning of therapy, an exacerbation of acne is observed, which resolves within 7-10 days without adjusting the dose of the drug.
Several years after the use of Roaccutane in large doses for the treatment of dyskeratosis, bone changes developed, incl. premature closure of the epiphyseal growth zones, therefore, when prescribing the drug to any patient, the ratio of possible benefits and risks should first be carefully assessed.
Patients receiving Roaccutane are recommended to use moisturizing ointment or body cream, lip balm to reduce dry skin and mucous membranes at the beginning of therapy.
Patients receiving Roaccutane require careful monitoring to identify severe skin reactions and, if necessary, consider discontinuing the drug.
While taking Roaccutane, pain in muscles and joints and an increase in CPK activity are possible, which may be accompanied by a decrease in tolerance to intense physical activity.
Deep chemical dermoabrasion and laser treatment should be avoided in patients undergoing treatment with Roaccutane, as well as for 5-6 months after the end of treatment due to the possibility of increased scarring in atypical places. During treatment with Roaccutane and for 6 months after it, hair removal using wax applications cannot be performed due to the risk of epidermal detachment, scar development and dermatitis.
During the period of taking Roaccutane, you need to carefully monitor your visual acuity. Dryness of the conjunctiva of the eyes, clouding of the cornea, deterioration of night vision and keratitis usually disappear after discontinuation of the drug. If the mucous membrane of the eyes is dry, you can use applications of a moisturizing eye ointment or an artificial tear preparation. Patients with dry conjunctiva should be monitored for possible development of keratitis. Patients with vision complaints require an examination by an ophthalmologist, after which it is necessary to consider the advisability of discontinuing Roaccutane. If you are intolerant to contact lenses, you should use glasses during therapy.
Exposure to sunlight and UV rays should be limited. If necessary, use sunscreen with a high protection factor of at least 15 SPF.
Rare cases of the development of benign intracranial hypertension (“pseudotumor cerebri”) have been described, incl. when used in combination with tetracyclines. In such patients, Roaccutane should be discontinued immediately.
During therapy with Roaccutane, inflammatory bowel disease may occur. In patients with severe hemorrhagic diarrhea, Roaccutane should be immediately discontinued.
Rare cases of anaphylactic reactions that occurred only after previous external use of retinoids have been described. Severe allergic reactions dictate the need to discontinue the drug and carefully monitor the patient.
Patients at high risk (with diabetes, obesity, chronic alcoholism or lipid metabolism disorders) may require more frequent laboratory monitoring of glucose and lipid levels when treated with Roaccutane. If you have diabetes or suspect it, more frequent determination of glycemia is recommended.
Impact on the ability to drive vehicles and operate machinery
Since some patients may experience a decrease in night vision acuity, which sometimes persists even after the end of therapy, patients should be advised to exercise caution when driving at night.
Roaccutane: Dosage
Good afternoon I was prescribed Roaccutane at a dosage of 20 mg 2 times a day. But now the warehouse where I buy only has a dosage of 10 mg. I would like to know if it is possible to take two 10 mg capsules instead of one 20 mg? - Olga
2009
Dear Olga! Yes, you can take two 10 mg capsules of Roaccutane instead of one 20 mg capsule. Do not forget to take the drug after meals (with fats), because in this case, the bioavailability of the active substance increases approximately 2 times. Dermatologist Panarin O.V.
Action of Roaccutane (Acnecutane)
Hello, Oleg Valerievich! I would like to ask how exactly Roaccutane works during treatment with it, does it restore metabolism or something else? Thank you in advance. - Paul
2009
Dear Pavel! With acne, the pathological process occurs in the sebaceous glands and hair follicles. Roaccutane or Acnecutane contain the active substance Isotretinoin (a retinoid, like vitamin A, but much more active). Isotretinoin and its metabolites (substances formed in the body from Isotretinoin) greatly reduce the production of sebum by the sebaceous glands, reduce the size of the sebaceous glands (the result of which is the elimination of black and white “dots” - comedones, a significant reduction in the number of bacteria that cause inflammation), themselves have an anti-inflammatory effect. Because Roaccutane (Acnecutane) can cause serious side effects (see instructions), it should be prescribed for severe forms of acne (for example, acne that leaves scars), if months of treatment with traditional methods of treatment are ineffective, if the patient is in a severe psycho-emotional state caused by a cosmetic defect ... Dermatologist Panarin O.V.
Roaccutane (Acnecutane) and pregnancy
Hello. I am 18 years old. The dermatologist prescribed Roaccutane. I took Roaccutane for 9 months: the first 2 months, 20 mg per day, then 10 mg per day. A month ago I stopped taking it due to the fact that I got married. Another dermatologist said that you should not become pregnant for at least 1–1.5 years. He said that the child might be born a deformity, etc. Is it true? I'm just shocked. – Zalina
2009
Indeed, if you take Roaccutane or Acnecutane capsules during pregnancy, fetal malformations and/or miscarriage may occur. It is safe (for mother and fetus) to become pregnant 5 weeks after finishing treatment with these drugs. Dermatologist Panarin O.V.
The use of isotretinoin for the correction of wrinkles –
But the retinoid isotretinoin can be used not only systemically (orally).
There are a small number of drugs with isotretinoin for external use, which were initially used exclusively for the treatment of acne and pimples, but later these drugs began to be used to correct the symptoms of photoaging. As in the case of the retinoid tretinoin, preparations with isotretinoin also help to increase skin elasticity and reduce the depth of wrinkles. What effects do external forms of isotretinoin cause in the skin:
- Peeling effect - the thickness of the superficial stratum corneum of the epidermis decreases (due to exfoliation of dead skin cells). This evens out skin tone and texture, leaving skin looking more youthful and radiant—like you've had a few superficial chemical peels.
- Increasing the thickness of the deep layers of the epidermis - isotretinoin affects stem keratinocytes located at the basement membrane, increasing the rate of their division and differentiation. This leads to an increase in the thickness of the deep layers of the epidermis, consisting of living keratinocytes. As a result, the hydrophobicity of the epidermis increases, which contributes to less evaporation of moisture from the surface of the skin. In addition, it prevents skin photoaging.
- Stimulation of the production of collagen and hyaluronic acid - isotretinoin affects not only the epidermis, but also the dermis. It promotes the proliferation (reproduction) of fibroblasts, and also significantly stimulates their activity, which leads to an increase in their production of collagen, elastin and endogenous hyaluronic acid. This leads to an increase in the thickness of the dermis, a decrease in the depth of wrinkles, and an increase in skin elasticity. It is known that thicker skin is less susceptible to the aging process.
Optimal concentrations of external forms of Isotretinoin –
There are a number of clinical studies where scientists have determined the optimal concentration of isotretinoin for the treatment of photoaging.
1) “Armstrong RB, Lesiewicz J, Harvey G et al. Clinical panel assessment of photodamaged skin treated with isotretinoin using photographs. Arch Dermatol 1992; 128:352–6.” 2) “Sendagorta E, Lesiewicz J, Armstrong RB. Topical isotretinoin for photodamaged skin. J Am Acad Dermatol 1992; 27:S15–18.”
In these studies, the concentration of Isotretinoin was increased from 0.05% at the beginning of the study to 0.1% at the end of the study. Despite the increase in concentration, the drug was well tolerated by patients without causing significant skin irritation. As a result of the treatment of photoaging skin with 0.1% Isotretinoin, the skin condition gradually improved throughout the 36-week treatment, and a decrease in the depth of wrinkles and fine lines was achieved.
3) The study “Maddin S, Lauharanta J, Agache P et al. Isotretinoin improves the appearance of photodamaged skin: results of a 36-week, multicenter, double-blind, placebo-controlled trial. J Am Acad Dermatol 2000; 42:56–63.” In this study, a combination of 0.05% Isotretinoin plus SPF sunscreen was used to treat photoaging. The result was that the condition of skin with visible photodamage was significantly improved, which was recorded using profilometry.
Conclusions: if you are interested in preventing skin photoaging, it is best to use a 0.05% concentration in combination with sunscreen. If you want to achieve an increase in skin elasticity and a decrease in the depth of wrinkles, then the main treatment should be carried out using a 0.1% concentration (it is better to use a 0.05% concentration for the first month so that the skin gets used to retinoids).
Isotretinoin has a delayed effect - it will take at least 8-12 weeks before you notice any positive changes, although the first positive effect associated with improved skin tone and texture will be noticeable after 4-6 weeks. It must be admitted that abroad isotretinoin is used for the correction of photoaging much less frequently than other types of retinoids - tretinoin or pure retinol.
Preparations with isotretinoin for external use –
- “Retinoic ointment” (Fig. 8) – is available with an isotretinoin concentration of 0.05% or 0.1%. The cost will be from 300 rubles for a 15 g tube. About a tenth of the volume is ethyl alcohol, so you should not use this drug if you have dry and/or sensitive skin. In principle, the manufacturer writes in this regard that this drug is intended for the treatment of acne in patients with oily skin.
- "Retasol" (Fig. 9) - is a solution for external use, with an isotretinoin concentration of 0.025%. But keep in mind that this drug also contains alcohol, but in less quantity than retinoic ointment. In addition, the drug contains propylene glycol, which may cause irritation in patients with sensitive skin. Cost from 400 rubles per 50 ml bottle.
Stepwise dose adjustment of Roaccutane (Acnecutane)
Dear Doctor! Tell me, how important is the stepwise dose adjustment of Roaccutane at the final stage of acne treatment? Why is this stepwise dose adjustment needed and is it necessary at all? Could the effectiveness of taking the drug really decrease if there was no stepwise correction? - Irina
2009
Dear Irina! Indeed, there are medications (for example, hormonal), in the treatment of which the daily dosage should be gradually reduced until complete withdrawal. However, Roaccutane (Acnecutane) is not one of these drugs. A “stepwise” dosage adjustment of Roaccutane (Acnecutane) upon completion of therapy is not necessary. Dermatologist Panarin O.V.
Roaccutane: Daily and cumulative doses
Hello, Oleg Valerievich! Under the strict supervision of a doctor, I started taking Roaccutane about 1.5 months ago: I started with 40 mg/day, then the dose was lowered to 30 mg/day, and now I take 20 mg/day. The only side effects are mild dry lips. My doctor claims that, according to the latest research, there is no need to take a cumulative dose; mg of the drug per kg of body weight has no meaning. And one should proceed only from visible results, and gradual and slow withdrawal of the drug is also important. Tell me, please, is this true? – Karina
2009
Dear Karina! I do not believe that “gradual and slow” withdrawal of Roaccutane or Acnecutane is important - I have not seen any clinical studies. It is possible to get rid of acne without reaching the cumulative dose, but the percentage of relapses is significantly higher than after reaching the recommended total dose. The daily dose of Isotretinoin capsules is determined mainly by the severity of acne, adjusted depending on tolerability, laboratory parameters, etc. Dermatologist O.V. Panarin.