Personality disorder or psychopathy is a disorder of a person’s mental activity, characterized by disharmony in the development of certain aspects of the personality. The first inconsistencies with generally accepted norms in behavior can be visible already at an early age. They become more noticeable during puberty, and over the years the symptoms become more pronounced.
Psychopathy is considered a kind of borderline state, bordering between health and disease. It is seen as a painful deviation from the norm, but is not a mental illness. Personality disorders have many types and forms, so treatment is selected individually, taking into account clinical characteristics.
Causes
According to statistics, about 12% of the population suffers from personality disorders. The reasons for their occurrence are ambiguous in most cases. The main predisposing factors to the development of mental disorders are of a genetic nature - the presence of mental illnesses, alcoholism, personality disorders in parents or close relatives.
In addition, the development of personality disorders can occur as a result of traumatic brain damage before the age of 3-4 years. Also, social factors can play a leading role in the emergence of this kind of pathology - inadequate upbringing of a child in the event of the loss of parents or in a family suffering from alcoholism. Violations arise against the background of inflicted psychological trauma - intimate abuse, manifestations of sadism, moral cruelty towards a child.
At first, the manifestations of the pathology have a clear picture, but with age, the symptoms have no specific boundaries and are reflected in all areas of life.
Causes
It is believed that this is a polyetiological disease. Genetic predisposition plays a major role. This theory is supported by clinical studies conducted in the 1970s and 1980s. When studying the anamnesis of patients with a similar mental disorder, it was found that the incidence of symptoms of the disease is 5 times higher in children whose parents suffered from a similar pathology.
Considerable importance is also attached to exogenous organic lesions of the brain during intrauterine development, during childbirth or infancy. These injuries are not severe enough to cause significant symptoms of neurological disease, but are sufficient to impair mental functioning.
Symptoms
Personality disorder is characterized by alternating periods of social compensation and decompensation.
Compensation is manifested by the individual’s temporary adaptation to society. During this period, a person does not have problems communicating with people around him, and personal deviations are hardly noticeable. During decompensation, pathological personality traits become pronounced, which contributes to a significant disruption of the adaptive capabilities of social interaction.
This period can take either a short period of time or last for a long time.
Personality disorders during exacerbation may be accompanied by symptoms such as:
- distortion of perception of reality;
- a feeling of emptiness and meaninglessness of existence;
- hypertrophied reaction to external stimuli;
- inability to establish relationships with other people;
- asociality;
- depression;
- feeling of uselessness, increased anxiety, aggression.
The diagnosis of “Personality disorder” can be made only if there is a triad of Gannushkin-Kerbikov criteria for psychopathy, which includes the totality of personality disorders, the severity of the pathology, as well as the relative stability of the individual’s condition.
Now, in order. What to do about it?
Step one.
And the easiest. Because at this stage there are practically no changes. The first step is to determine whether the patient meets the general definition of a personality disorder. According to the idea of the new classification, this diagnosis can be made by both a psychiatrist and a doctor of the primary network, since the approach to the definition does not have serious differences from ICD-10. Using the following criteria, without going into categories, the specialist determines the presence of a personality disorder:
- the presence of progressive disturbances in the way a person thinks and feels about himself, others and the world around him, which manifests itself in inadequate ways of cognition, behavior, emotional experiences and reactions;
- the identified maladaptive patterns are relatively rigid and are associated with pronounced problems in psychosocial functioning, which is most noticeable in interpersonal relationships;
- the disorder manifests itself in a variety of interpersonal and social situations (i.e., is not limited to specific relationships or situations);
- the disorder is relatively stable over time and has a long duration. Most often, a personality disorder first appears in childhood and clearly manifests itself in adolescence.
If the disorder is first detected in adulthood, the qualifier “late onset” may be used. This qualifier should be used in cases where the history does not provide clear evidence of detectable disorders at an earlier age.
It is very important to determine the area of detected violations. Problems in interpersonal interaction in personality disorders are characterized by general disturbances in relationships with people that interfere with mutual understanding. This needs to be understood because most mental disorders are related in one way or another to social dysfunction. Thus, difficulty in completing tasks, organizing life's responsibilities, free time, maintaining adequate relationships at work, as well as lack of harmony in the family, are very different from the disorders associated with the inability to get along with the rest of the human race, which is exactly what is observed for personality disorders. A person whose life is turned upside down by a family feud does not necessarily have a personality disorder. A diagnosis should only be made if there is clear evidence of widespread deterioration in relationships with everyone around them.
Step two: determining the severity of RL.
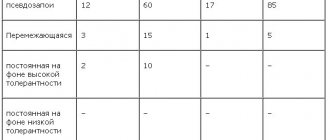
Currently, personality disorders are an exclusively qualitative category, which often leads to the fact that two patients with the same diagnosis can be strikingly different from each other. ICD-11 offers 3 degrees of severity of personality changes (see Table 1), each of which can include one or several pathological signs. Ranking by severity takes into account that although LC is supposed to be a lifelong diagnosis, its severity may change over time.
Tab. 1 Degrees of severity of personality disorders in ICD-11
| Degree of expression | Main characteristics |
| Mild severity of personality disorders | - there are pronounced difficulties in constructing a significant part interpersonal relationships and in fulfilling expected professional and social roles; — the ability to perform certain social or professional roles and maintain some relationships is retained; - not associated with causing significant harm to oneself or others. |
| Average severity of personality disorders | - serious problems are observed in most interpersonal relationships and in fulfilling expected professional and social roles; - these problems are identified in a wide range of situations, most of which are compromised to some extent; – often involves a history or expected future harm to oneself or others, but NOT to a degree that would cause long-term harm or be life-threatening. |
| Severe severity of personality disorders | - serious problems in interpersonal functioning, affecting all areas of life; - the person's general social dysfunction becomes profound, and the ability and/or willingness to perform expected professional and social roles is absent or seriously compromised; – often involves a history and expectation of future serious harm to oneself or others, to a degree that may cause long-term harm or be life-threatening. |
In addition, a subthreshold level of disorder is identified, which corresponds to the familiar concept of “personality accentuations” and is designated as “personality difficulty” (complex/difficult personality) (see Table 2). “Personality difficulty” will not be a diagnosis, and, in its essence, will correspond to the existing code Z in ICD-10. Registration of accentuations is necessary, since its presence increases the risk of the need for medical intervention in certain conditions, for example, under stress or in certain conditions environment. At the same time, it is necessary to understand that some cases of mild personality disorders may not require specialist supervision. According to modern epidemiological estimates, 1 out of 14 people in the population suffers from a personality disorder, and treatment of each, firstly, is not necessary, and secondly, incurs huge economic costs. The presence of ranking by severity will allow a more professional approach to identifying indications for therapeutic interventions.
Tab. 2Dimensional system for classifying personality disorders by severity.
| Degree of expression | Name | Main characteristics |
| 0 | Lack of radar | No personality disorders |
| 1 | Personality difficulty (accentuation) | There are some disorders that appear in a limited range of situations, but not all the time |
| 2 | Personality disorder | The presence of a clearly expressed personality disorder manifested in a wide range of situations |
| 3 | Integrated radar | The presence of pronounced problems affecting several domains and manifested in all situations |
| 4 | Severe RL | Presence of significant problems affecting (usually) multiple domains and occurring in all situations resulting in significant risk to self or others |
The difficult-to-understand comorbidity of different types of personality disorder has been eliminated, which may lead to a decrease in the number of patients with unspecified/mixed personality disorder. The designation of “complex personality disorder” reflects a universal finding in research on this topic that as the problem becomes more pronounced, the diagnostic boundaries between different personality disorders become blurred.
Step three.
Where you need to forget everything you knew before. The classification we are familiar with implies that personality disorders are discrete and qualitatively different syndromes and, at their core, work according to an all-or-nothing scheme. The changes that affected the problem of personality disorders in ICD-11 indicate that PDs are maladaptive variants of personal qualities that can imperceptibly transform into normal ones, or one into another, being a kind of continuum without any strict distinctions.
The new approach was based on the line started by G. Allport, G. Eysenck and R. Cattell about the dispositional (from the English disposition - predisposition) model of human personality or the so-called “Big Five”. The essence of this model is that the levels of dominance of the described personality traits form a person’s individuality and, in turn, predetermine the ability to adapt this personality. Empirically, using scales, questionnaires and expert assessments, five properties were identified (see Table 3).
Tab. 3 Comparative characteristics of the Big Five domains and RDOC
| Big Five | RDoC |
| Neuroticism - emotional stability | Negative affect |
| Extraversion - withdrawnness | Positive affect |
| Benevolence (friendliness, ability to reach agreement) - antagonism | Social processes |
| Conscientiousness (conscientiousness) - impulsiveness | Excitation/Regulation Systems |
| Openness to experience - conservatism | Cognition |
The same idea was taken up by the developers of the alternative RDOC classification. The features identified by these researchers can fully prove the validity of both the Big Five theories and the domains used in ICD-11 (see Table 4) and DSM 5.
Tab. 4 Personality trait domains ICD-11.
| ICD-11 domain | Characteristics |
| Negative affective features signs of negative affectivity (neuroticism in Big Five) | Characterized by a tendency to exhibit a wide range of distressing emotions, including anxiety, anger, self-loathing, irritability, vulnerability, depression, and other negative emotional states, often in response to even relatively minor actual or perceived stressors. |
| Dissocial features dissocial symptoms (antagonism - contrasted goodwill in Big Five) | The core of the dissocial trait domain is disregard for social obligations and conventions and the rights and feelings of others; traits in this domain include: callousness, lack of empathy, hostility and aggression, ruthlessness, and an inability or unwillingness to maintain prosocial behavior, often manifested by an overly positive view of the self and a tendency to manipulate and exploit others. |
| Features of disinhibition disinhibitory signs (impulsivity - contrasted integrity in Big Five) | The disinhibitory trait domain is characterized by a persistent tendency to act impulsively in response to immediate internal or external stimuli without consideration of long-term consequences; traits in this area include: irresponsibility, impulsiveness without considering risks or consequences, distractibility, and recklessness. |
| Anankastic features anancaste signs (conservatism - contrasted openness to experience Big Five) | This domain is characterized by having a narrow focus on controlling and regulating one's own behavior and that of others to ensure that things conform to an individual's ideal; Traits in this area include: perfectionism, perseveration, emotional and behavioral limitations, stubbornness, conscientiousness, orderliness, following rules and obligations. |
| Features of detachment signs of isolation (low level extraversion in Big Five) | Emotional and interpersonal distance, manifested in noticeable social isolation and/or indifferent attitude towards people; isolation with very little or no attachments, including avoidance not only of intimate relationships but also of close friends; Traits of this domain include: aloofness or coldness towards other people, reserve, passivity and lack of self-confidence, as well as reduced experience in experiencing and expressing emotions (especially positive ones), to the extent of weakening the ability to experience pleasure. |
The DSM has a similar domain model: negative affective, dissocial, disinhibited, and detached domain traits; and instead of anancast, the domain of psychoticism, which is absent in ICD-11.
Each of the domains can be found both in relatively healthy members of the population and among patients with a personality disorder, but in patients with PD they indicate the focus in which the disorder manifests itself to a greater extent. For a diagnostician, it will be necessary to identify the characteristics of domains in a particular patient, even if the clinical picture reveals phenomena characteristic of all five domains. The proposed innovations will help eliminate the temptation to make a diagnosis that bypasses a comprehensive personality assessment. The need for such a vague diagnosis as “mixed personality disorder” is lost. Modern studies examining this approach are identifying specific therapies that may be effective when symptoms of individual domains predominate. For example, the domain of disinhibitory symptoms requires structured psychological intervention, patients with signs of the domain of negative affectivity respond well to cognitive behavioral therapy, and patients with dissocial symptoms are resistant to therapeutic interventions and are more likely to require social changes.
Prepared by: Chesnokova O.I.
Sources:
1 – Clark LA, Livesley WJ, Morey L. Special feature: Personality disorder assessment: The challenge of construct validity //Journal of Personality Disorders. – 1997. – T. 11. – No. 3. – pp. 205-231.
2 – Coid J. et al. Prevalence and correlates of personality disorder in Great Britain //The British Journal of Psychiatry. – 2006. – T. 188. – No. 5. – pp. 423-431.
3 – Crawford MJ et al. Classifying personality disorder according to severity //Journal of personality disorders. – 2011. – T. 25. – No. 3. – pp. 321-330.
4 – Emmelkamp PMG et al. Comparison of brief dynamic and cognitive-behavioural therapies in avoidant personality disorder //The British Journal of Psychiatry. – 2006. – T. 189. – No. 1. – pp. 60-64.
5 – Huang Y. et al. DSM–IV personality disorders in the WHO World Mental Health Surveys //The British Journal of Psychiatry. – 2009. – T. 195. – No. 1. – pp. 46-53.
6 – Mulder RT et al. The central domains of personality pathology in psychiatric patients // Journal of personality disorders. – 2011. – T. 25. – No. 3. – pp. 364-377.
7 – Oldham JM, Skodol AE, Bender DS (ed.). The American Psychiatric Publishing textbook of personality disorders. – American Psychiatric Pub, 2007. – pp. 33-36.
8 – Tyrer P. et al. Randomized controlled trial of brief cognitive behavior therapy versus treatment as usual in recurrent deliberate self-harm: the POPMACT study //Psychological medicine. – 2003. – T. 33. – No. 6. – pp. 969-976.
9 – Tyrer P. et al.The rationale for the reclassification of personality disorder in the 11th revision of the international classification of diseases (ICD-11) //Personality and Mental Health. – 2011. – T. 5. – No. 4. – pp. 246-259.
10 – Ranger M. et al. Prevalence of personality disorder in the case-load of an inner-city assertive outreach team //The Psychiatrist. – 2004. – T. 28. – No. 12. – pp. 441-443.
11 – Verheul R., Bartak A., Widiger T. Prevalence and construct validity of personality disorder not otherwise specified (PDNOS) // Journal of personality disorders. – 2007. – T. 21. – No. 4. – pp. 359-370.
12 – Verheul R., Widiger TA A meta-analysis of the prevalence and usage of the personality disorder not otherwise specified (PDNOS) diagnosis //Journal of Personality Disorders. – 2004. – T. 18. – No. 4. – pp. 309-319.
13 – Yang M., Coid J., Tyrer P. Personality pathology recorded by severity: national survey //The British Journal of Psychiatry. – 2010. – T. 197. – No. 3. – pp. 193-199.
Schizoid personality disorder
Persons suffering from this type of pathology are characterized by excessive isolation, emotional detachment, and sociopathic tendencies. They do not need contact with people, prefer a solitary lifestyle, and most often choose work with the possibility of minimal communication.
When interacting with others, such people experience internal discomfort, a feeling of uncertainty, tension, and therefore avoid establishing trusting relationships and do not have close friends.
Patients with this diagnosis show interest in everything unusual, have non-standard views on things and well-developed logical thinking. They are also characterized by a passion for various philosophical problems, ideas for improving life, and exact sciences.
People suffering from this type of disorder often achieve excellence in mathematics or theoretical physics, have musical talent, and also the ability to establish unexpected patterns.
Therapy for personality disorders
Depending on the type of disorder, the degree of suffering of the person who has these changes, the ability or inability to control the impulses generated by this disorder, as well as the level of personality, psychiatrists, psychotherapists, and sexologists treat this pathology. In the mildest cases, psychologists work with such people. Therapy for personality disorders requires long-term and painstaking psychological work. Progress in drug treatment for personality disorders is inconsistent and often questionable. If we set the task of working with personality traits and reactions that burden the patient, then psychological work, in general, can achieve more impressive results than drug assistance.
Telephone for consultations:
+7(495) 726-36-42+7(965) 152-76-09
All materials on the site are presented for informational purposes only, approved by certified physician Mikhail Vasiliev, diploma series 064834, in accordance with license No. LO-77-005297 dated September 17, 2012, by a certified specialist in the field of psychiatry, certificate number 0177241425770.
Paranoid disorder
Personality disorder of the paranoid type is characterized by increased distrust, pathological suspicion, and an exaggerated perception of injustice towards one’s own person. Patients with this diagnosis tend to see negative intent in everything, constantly feel a threat from the outside, and attribute negative intentions to others.
A paranoid person is characterized by increased confidence in his own importance, does not recognize that others are right, and is convinced of his own infallibility. Such a person is extremely sensitive to criticism addressed to him and interprets any actions and words of others in a negative way.
In a state of decompensation, the clinical picture is complemented by pathological jealousy, a craving for constant disputes and proceedings, and aggression.
Dissocial disorder
Pathology is manifested by an indifferent attitude towards the feelings of others, irresponsible behavior, and disregard for social rules and responsibilities. Individuals with this diagnosis are characterized by behavioral non-compliance with social norms; they are characterized by open confrontation with the outside world and a criminal predisposition.
In childhood, the characteristic features of such individuals are increased conflict, lack of desire to learn, and opposition to any established rules. During puberty, persons suffering from this pathology show a tendency to theft, hooliganism, and frequent running away from home.
An adult with a dissocial disorder has no spiritual values, is unable to experience warm feelings, and blames everyone but himself. Such people assert themselves at the expense of the weak, do not feel pity, have sadistic tendencies, and are aggressive in bed.
Hysterical disorder
This kind of disorder occurs in 2-3% of the population, most often in females. This type of mental disorder is characterized by theatrical manifestation of emotions, frequent mood swings, shallow perception of phenomena, and inconsistency in attachments. Such people love increased attention to their person, so they try in every possible way to achieve this.
Patients with hysterical disorder are overly concerned with their appearance, strive for ostentatious external brilliance, and need constant confirmation of their irresistibility.
When building personal relationships, individuals with this diagnosis put their own interests first and try to achieve their goals at the expense of others through manipulation. They are painfully aware of the indifferent attitude of others.
Obsessive-compulsive disorder
This type of disorder is characterized by increased caution, a tendency to doubt, a desire to keep everything under control, and obsessive thinking. People suffering from this type of personality disorder strive for perfection in everything, which greatly interferes with the completion of the task itself. They are overly conscientious, scrupulous, too pedantic and demanding of themselves and others.
Such patients are convinced that only their lifestyle and concepts are correct, and therefore demand that others conform to their ideas. Often, these individuals develop obsessive thoughts and peculiar rituals, expressed in the constant need to count objects, repeatedly check whether household appliances are turned off, whether the entrance doors are closed.
The financial side of life plays a special role for such people. They are overly frugal in spending, which they also demand from others; money is perceived as something that needs to be put aside in case of a global catastrophe.
During the period of compensation, individuals with this diagnosis are distinguished by reliability, pedantry, and correctness in communication. During decompensation, they are bothered by a growing feeling of anxiety, due to which the patient becomes irritable, remains in a gloomy state, and has hypochondriacal tendencies.
Types of Disorders and Personality Changes
Personality disorders and changes are described, on the one hand, by a set of specific traits, values and attitudes inherent in a particular character; on the other hand, according to the level of personality development.
Personality disorders
In this regard, they are divided into several types:
- paranoid (excessive sensitivity to failures, constant dissatisfaction with what is happening around, vindictiveness, refusal to forgive insults, a tendency to accept neutral actions of people as hostile, conspiratorial interpretation of many events)
- schizoid (emotional coldness, weak interest in social contacts, inability to show any feelings towards other people, preference for solitary activities, preoccupation with fantasies, theories or one’s own inner world, insensitivity to social norms, lack of close friends and desire to have close contacts)
- dissocial (heartlessness, indifference to other people's feelings, disregard for social norms, one's rights and responsibilities; inability to maintain relationships, despite the fact that they are established well; intolerance of refusal, ease of aggression up to violence and causing injury, inability to learn lessons from life experience, inability to feel guilty, tendency to blame others for everything, completely justifying oneself)
- emotionally unstable (emotional instability, difficulty in self-control, frequent outbursts of aggression, intolerance of refusal (frustration), impulsivity)
- hysterical (exaggerated expression of emotions, theatricality, suggestibility, susceptibility to the influence of the opinions of others or circumstances, superficiality and instability of emotions, constant desire for strong emotions, desire to be the center of attention, constant desire for recognition from others, excessive preoccupation with physical attractiveness, excessive desire to seduce , seduce others, touchiness, egocentrism, constant manipulation of others)
- anancaste (excessive caution, a tendency to constantly doubt, excessive concern with rules, schedules, schedules, details; perfectionism, the desire for perfection, which prevents the completion of tasks; inadequate concern for productivity and implementation of the plan to the detriment of pleasure and maintaining social connections; pedantry, weak variability of behavior , stubbornness)
- anxious (avoidant, avoidant) (constant heavy apprehension, anxiety, self-image as unattractive, unworthy, inferior to others; preoccupation with criticism or social rejection; increased sensitivity to rejection and criticism; reluctance to enter into relationships no guarantee of being liked; reluctance to engage in work that involves the possibility of being rejected or criticized)
- dependent (the desire to shift the solution of important issues in one’s life to others, the subordination of one’s needs to the needs of the one on whom one depends; reluctance to make even reasonable demands on those on whom one depends; a feeling of helplessness in loneliness due to the inability to live independently; constant fear of being abandoned by a person dependent; reduced ability to make decisions in everyday life without outside advice and encouragement)
- other personality disorders: expansive, passive-aggressive, narcissistic, unrestrained, disinhibited, eccentric, and others
Personality changes
- after experiencing a disaster (hostile or distrustful attitude towards the world, emptiness, a feeling of hopelessness, social isolation, constant feeling of threat, “existence on the brink of a disaster” for at least 2 years after the disaster)
- after suffering a mental disorder (excessive dependence on others and placing excessive demands on them; persistent belief in one’s own change, “wrongness” due to the illness, which makes it difficult to establish relationships and connections; passivity, decreased interests and passion for what was of interest before; constant complaints illness, hypochondriasis; sad-angry (dysphoria) or mood swings; significant decline in social and work functioning)
Among other things, there is a whole class of mature personality disorders that currently cannot be fully explained by either hereditary or environmental factors.
Anxiety disorder
This type of pathology is accompanied by a constant feeling of anxiety, unpleasant premonitions, and low self-esteem. Such people try to avoid any contact with people, considering themselves socially inferior and personally unattractive. They are too shy, indecisive, and often lead a reclusive lifestyle.
Individuals with an anxiety disorder are pathologically afraid of criticism in their direction; they are hypersensitive to any negative assessments, and therefore try to avoid social and professional activities.
As a rule, people with this diagnosis adapt well to society, since in most cases the environment is sympathetic to the problem of such a person.
Level of personality development
(according to N. McWilliams) can be neurotic, borderline or psychotic.
Neurotic level of personality development
characterized by the presence of an “internal observer” (a person can evaluate himself, as if looking from the outside), mature internal identity, continuity of “I” over time. People with a neurotic level are in full contact with reality and can well describe themselves, their beliefs, character, values, habits. Their main intrapersonal conflict is between desires and the obstacles that they create for themselves.
Borderline level of personality development
The “I” of people with a borderline level is contradictory and torn; they cannot create an objective, consistent story about themselves. Their values and attitudes largely negate each other. People with a borderline level are prone to polar assessments of reality (“it’s either good or not at all”, “I don’t tolerate mediocrity, I must always win”, “if I can’t live normally, I’d rather die”, etc.), they use primitive mental defenses: denial (“no, it didn’t happen”), projective identification (“what, I don’t see what kind of person this is? - he hasn’t opened his mouth yet, but I immediately understood everything about him”), splitting ( “If I’m not God, I’m nobody”). Their main intrapersonal conflict is between the fear of absorption and the fear of abandonment.
Psychotic level of personality development
These people are very poor at testing reality and are often unable to distinguish between reality and fantasy. They are in constant anxiety and fear of being swallowed up or destroyed by this reality. Their main task is to ensure their own safety. The main conflict is between the desire to live and the fear of being “crushed” by this world.
Narcissistic disorder
A clear manifestation of this kind of disorder occurs in adolescence. Patients experience an increased need for admiration from others, exaggerate their own importance in society, and do not accept critical judgments.
The main character traits of such individuals are complete conviction of their own greatness and the need to indulge all their whims. They are convinced of their superiority over other people, have an inflated opinion of their talents and achievements, and are absorbed in fantasies about their successes. They need increased attention and are focused exclusively on themselves.
Narcissistic individuals are clever exploiters and manipulators, thanks to which they achieve the fulfillment of their desires at the expense of others. Such people prefer a certain social circle that meets their high standards. They do not accept criticism and comparisons with “ordinary” people.
The inner world of these individuals is quite fragile and vulnerable, the emotional state is unstable and completely depends on external circumstances. Arrogance and arrogance are a protective mask that hides excessive sensitivity to rejection and criticism.
Dependent personality disorder
People suffering from this type of disorder are characterized by shifting responsibility for solving most life issues. The pathology is accompanied by a feeling of helplessness, pathological fear due to the inability to independently manage one’s own life.
As a rule, dependent people try to find a kind of patron with the help of whom they can at least somehow realize themselves in society. Such individuals need constant encouragement, advice, and approval of actions. Patients with this diagnosis are fearful, timid, unsure of their own abilities, unable to live without constant guidance.
The period of decompensation begins in the event of the loss of a patron, when life tasks must be performed independently, without prior agreement with him. The clinical picture during this period worsens significantly, which can lead to severe panic attacks without any particular reason.
Publications in the media
Personality disorders are long-term and persistent disorders of various spheres of mental activity, devoid of productive psychotic symptoms and manifested by behavior from which either the patients themselves or society suffer. The disorders usually begin in childhood or adolescence and continue throughout later life. In foreign psychiatry, since the 70s of the 20th century, the term “psychopathy”, “which has become not a clinical diagnosis, but a synonym for the asociality of the subject,” has been replaced by the concept of “personality disorder.”
To make a diagnosis of personality disorder, it is necessary to exclude organic brain damage, which can cause similar behavioral disorders. If a somatic and/or neurological disease (for example, a brain tumor) leading to central nervous system dysfunction is detected, a diagnosis of “organic personality disorder” is made. In Russian psychiatry, starting from the 30s and until now, the doctrine of personality disorders (psychopathy), belonging to P.B., is most recognized. Gannushkin (1933). In accordance with the teachings of P.B. Gannushkin use the following provisions: • disorders are so pronounced that they lead to disruption of the patient’s adaptation to society; • totality of disorders; in this case, we are not talking about individual abnormal character traits, but about the fact that the personality as a whole is woven from pathological characterological properties; • persistence, stability and low reversibility of disorders throughout the patient's life. Frequency : 6–9% of the population. Classification and clinical picture The classification of personality disorders is conditional, because in most cases we are talking about mixed types, including symptoms of different types of personality disorders. • Paranoid personality disorder (paranoid psychopathy) •• Patients experience unreasonable suspicions that others are using, deceiving, or harming them. They are unkind to others, unable to forgive insults or disrespect, and express unreasonable doubts about the fidelity of their spouse or sexual partner. Patients persistently believe that they are right in all situations •• Patients with paranoid personality disorder seem unemotional and lack warmth. They are impressed only by strength and power, only in these cases do they pay attention to people, while those whom they consider weak, sick, infirm, inferior, they deeply despise •• In case of decompensation under the influence of emerging conflicts, systematic persecution begins “ offenders,” endless complaints are written to state, public and judicial authorities, in which any minor miscalculations of opponents are qualified as malicious and criminal, and defamatory anonymous letters are sent. The circle of persecuted persons is constantly expanding due to all those who took part in the analysis of conflicts and who, in the patient’s opinion, did not show due integrity and impartiality. In such situations, the development of overvalued delusions is possible, incl. delirium of jealousy. Patients with overvalued delusions are dangerous because they are prone to committing aggressive actions against their “enemies” or a sexual partner suspected of adultery. • Schizoid personality disorder (schizoid psychopathy) •• Patients are characterized by a reluctance to have close relationships with others and a lack of joy from such relationships. As a child, they like to play quiet and calm games alone, most often at home, never share their experiences with their parents, and cannot find a common language with their peers •• Schizoid individuals remain cold and distant, do not take part in everyday life, are uncommunicative, silent, do not follow fashion. They have no or poorly developed need for emotional contact with other people, no close friends, but at the same time they can be strongly attached to animals •• Patients strive for individual activities that do not require competition, and are able to spend an unusually large amount of effort and time on studying abstract sciences, such as mathematics, astronomy, philosophy •• Characterized by reduced interest or absence of interest in sexual relations. Men often don't get married because... they are unable to maintain intimate contact; women sometimes passively submit to an aggressive man, agreeing to marry him if he wants •• Patients are indifferent to praise or criticism. They respond to most threats, real or imaginary, by fantasizing about omnipotence and withdrawing from real life •• Despite social isolation and detachment from the outside world, patients can think and develop so far that they are able to give the world truly original, creative ideas. • Dissocial (antisocial) personality disorder •• Patients are prone to lies and impulsive actions; unable to plan. Patients are often irritable and aggressive. Ignoring personal safety or the safety of others is typical; irresponsible attitude towards one's responsibilities; indifference •• Lying, truancy, running away from home, theft, fighting, drug use and illegal activities are typical manifestations that begin in childhood. Antisocial personalities do not have depression or anxiety, which is surprising given the situation they are in, and their own explanations for what is happening to them seem crazy •• They like to manipulate others and often involve others in plans for easy money or achievement fame or notoriety, which in the end almost inevitably leads to financial ruin. A notable feature is the lack of regret about one's actions. • Emotionally unstable personality disorder (excitable psychopathy) •• In situations that do not meet the interests of patients, they give violent reactions of irritation, dissatisfaction and anger. Outside of situations that are emotionally significant for patients, reactions are often quite adequate. Outbursts of intense anger can lead to violence, especially if the patient's wishes and actions are resisted and criticized by others. Conflictful relationships with loved ones often lead to auto-aggression, including suicide attempts and self-harm •• Patients are desperately trying to avoid loneliness. They form unstable interpersonal relationships with people with alternating fluctuations between extreme idealization and extremely negative assessment •• Characterized by a violation of self-awareness (pronounced and long-lasting instability in the self-image) and a lack of adequate assessment of their reactions and behavior. Patients try to find reasons and circumstances that justify such behavior •• Patients are prone to impulsive actions that are committed without sufficient logical assessment, without taking into account their possible consequences and are associated with potential risks (wasting money, promiscuity in sexual relations, disregard for traffic rules) • • Mood is unpredictable and capricious (episodic dysphoria, irritability, short temper, anxiety) •• ICD-10 distinguishes two types of disorder: the impulsive type, characterized primarily by emotional instability and lack of emotional control, and the borderline type, which is additionally characterized by a disorder of self-perception and goals and internal aspirations, a chronic feeling of emptiness, tense and unstable interpersonal relationships and a tendency towards self-destructive behavior, including suicidal gestures and attempts.
• Histrionic personality disorder (hysterical psychopathy) •• Characterized by a feeling of discomfort in situations where the patient is not the object of attention. Patients try to evoke sympathy, an attitude of admiration, and surprise. This is achieved by extravagant appearance, boasting, deceit, fantasy, inappropriate sexual charm in appearance or behavior •• Patients are capricious and inconsistent. Their emotional reactions are labile, superficial and theatrical. The mood is extremely changeable. They are characterized by suggestibility, susceptibility to the influence of people or circumstances •• A low level of self-awareness does not allow them to objectively assess their behavior: they see themselves as people capable of self-sacrifice for the sake of their loved ones and friends, not noticing their actual selfish attitude towards them •• Being sweet and flirtatious with people on whom they want to make a good impression, they become tyrants in the family, showing callousness and even cruelty towards their loved ones •• In an effort to attract attention to themselves with their weakness and helplessness, such people become regular visitors to medical institutions, making complaints about unbearable physical and mental suffering •• Psephologists (pathological liars) predominate among men. Characterized by a tendency to fantasize, stories about extraordinary events in which they assign themselves a spectacular role, about meeting outstanding people, trying to present themselves as a more significant person than they actually are. Among them there are many petty scammers, imaginary psychics, and marriage swindlers.
• Anancastic personality disorder (anancastic psychopathy, obsessive-compulsive personality disorder) •• The basis of a psychasthenic personality is anxiety and self-doubt. Since childhood, such individuals have been characterized by shyness, increased impressionability, and constant fear of doing something wrong •• Patients are absorbed in organizing or planning their activities to such an extent that the main goal of the work is not achieved. They strive for improvement, which prevents them from completing the task. Patients are busy working and achieving results to such an extent that relationships with other people are sometimes very difficult for them •• They are not characterized by impulses or spontaneous impulses. Before taking any step, they evaluate it for a painfully long time, doubt its expediency •• Characterized by excessive conscientiousness, scrupulousness and lack of flexibility in matters of morality, ethics or moral values •• Patients are unable to get rid of worn-out or unnecessary things, even if they not associated with sentimental memories •• They are unwilling to share responsibilities or work with others unless others perform the work to the fullest extent of the patients' requirements •• Possible intrusive thoughts and actions that do not reach the severity of obsessive-compulsive disorder.
• Anxious (avoidant) personality disorder (inhibited type psychopathy) •• These patients are usually considered “complex people” in everyday life. The central clinical feature of this disorder is increased sensitivity to criticism, disapproval and dissatisfaction from others, as a result of which patients avoid contact with people. They are reserved in intimate relationships due to fear of reproaches or ridicule from a sexual partner •• Patients are afraid to speak in public or make requests of others (the disorder is often combined with social phobia). They sometimes misinterpret people's statements as demeaning or ridiculing them. Refusal of any request is accompanied by withdrawal on their part, and they feel insulted •• In the professional sphere, such patients often avoid taking on responsibilities or participating in new activities for fear of being in a difficult situation, and rarely achieve great success or earn authority . On the contrary, at work they show themselves to be shy and try to please everyone in everything •• Failure of social support can lead to anxiety and depression. • Dependent personality type disorder •• The core manifestation of the disorder is self-doubt, low self-esteem. Patients avoid responsibility; the need to perform leadership functions causes severe anxiety. In relationships with others, patients play only auxiliary, subordinate roles, are humiliated in order to be accepted and are often unfairly exploited in the interests of others. The loss of a meaningful relationship with a dominant person is fraught with the subsequent development of a depressive episode •• They find it difficult to do some work for themselves, but it is easy to do similar tasks for someone else. Patients find it difficult to make decisions in everyday life without outside help or reassurance. Characterized by fear of loneliness. Patients seek care and support from others, going so far as to voluntarily perform activities that are not enjoyable. Patients can endure insults, infidelity or drunkenness of their spouse for a long time. In the event of the loss of a close relationship, there is a need to find a new close connection as a source of care and support.
• Narcissistic personality disorder. Patients tend to exaggerate their own achievements and talents. They are characterized by preoccupation with fantasies of unprecedented success, unlimited power, brilliance, beauty or ideal love. Patients are convinced of their own uniqueness and ability to communicate or be related to other special or high-status people (or institutions). They easily develop a need for excessive admiration from others, unreasonable expectations of very good treatment or unquestioning submission to demands. Patients often use others to achieve their own goals. Patients with narcissistic disorder are characterized by an inability to show empathy; envy of others and the belief that others are jealous of him. • Passive-aggressive personality disorder •• The core feature of the disorder is a constant attitude towards passive resistance to management. Patients cannot stand up for themselves or speak directly about their needs and desires. At the same time, they are always dissatisfied, irritated and disappointed with someone or something. Patients constantly look for flaws in the authoritarian figures to whom they are subordinate and do not make any attempts to free themselves from their dependent position. Passive-aggressive individuals are envious and spiteful towards those who are more fortunate. Patients believe that they work much better than others think about it, reacting with indignation to the suggestion that their productivity could be higher •• When forced to achieve success at work, they experience severe anxiety. Those with whom patients are in close relationships are rarely calm and happy. Patients can, for example, ruin a party with their complaints and claims, without making, with some excuses, their positive contribution to it •• Patients often even find it difficult to formulate what a situation should look like in which they would be satisfied. Such patients often threaten to commit suicide, but as a rule, things do not go as far as suicide attempts. •• The disorder is often complicated by alcoholism, depression and somatization disorder.
Accentuations of character Accentuated personalities (K. Leonhard) occupy an intermediate position between mentally healthy people and patients with personality disorders. They adapt in life more easily than psychopathic ones, and their adaptation is more stable, however, even in unfavorable conditions, states of decompensation may arise in them. In their characteristics, they differ from ordinary people, and these characteristics (emphasis) are not considered as a manifestation of the disease, although in difficult conditions for the individual, failure of adaptation and disruption of interpersonal relationships may be possible. The leading signs of character accentuations may resemble reduced manifestations of the corresponding psychopathy. For example, accentuated personalities of the hysterical type are similar to those suffering from histrionic personality disorder: they are prone to theatricality, self-affirmation in the eyes of others, etc. However, these manifestations are not so vivid in them and the general disharmony of personality is much less pronounced. Within the framework of accentuated states, mixed variants are often noted, including signs of different types of character accentuations. The diagnosis of a personality disorder is invalid if there are only isolated characterological deviations that are well compensated and lead to pathological behavioral disorders only during relatively short periods of decompensation associated with mental trauma. In this case, a diagnosis of character accentuation is made. Research methods • EEG • MRI/CT • Psychological methods (MMPI, thematic apperception test, Rorschach test).
Differential diagnosis • Paranoid personality disorder differs from delusional disorder in the absence of delusional ideas. This disorder can be differentiated from paranoid schizophrenia on the basis that in paranoid personality disorder there are no hallucinations, emotional-volitional and thinking disorders. Patients with borderline personality disorder differ from this type in their ability to form strong emotional relationships with others. Paranoid personality disorder differs from antisocial personality disorder in that there is no history of antisocial behavior. They are similar to schizoid psychopaths by limited emotionality, but are distinguished by dominant suspicion and distrust. It is most difficult to distinguish paranoid disorder from schizotypal disorder, for which suspiciousness is also a characteristic feature. Unlike schizotypal patients, patients of this type do not have such a bizarre complex of behavioral, sensory and mental disorders; they are characterized not so much by the absence of distortions in communication skills, but by their characteristic orientation (eccentricity, eccentricity). • Schizoid personality disorder. Unlike schizoid disorder, patients with schizotypal disorder are characterized by more pronounced emotional-volitional and thinking disorders, subpsychotic episodes and less successful social adaptation. Patients of the emotionally unstable and anxious (evasive) type have a richer and more emotional social life, are sensitive to their loneliness, are more interested in interpersonal relationships and rarely resort to autistic fantasy. Patients with paranoid disorder are able to establish stable and emotionally rich relationships with others; they more often use psychological defense in the form of projection.
• Antisocial personality disorder. An antisocial psychopath differs from a mentally healthy criminal in that the criminality of his behavior is only one of the parameters of globally impaired personality functioning. When assessing antisocial behavior, it is very important to take into account the social norms of the cultural group to which the patient belongs. • Borderline personality disorder. Differential diagnosis with schizophrenia is based on the presence or absence of prolonged psychotic episodes of characteristic negative symptoms. Schizotypal individuals are characterized by strange behavior and fragmentary delusional ideas about relationships. Paranoid individuals are characterized by strong suspicion. Borderline individuals experience a chronic feeling of emptiness, impulsivity, short-term psychotic episodes, and suicidal attempts to manipulate others. • Histrionic personality disorder. It is most difficult to determine the difference between histrionic and borderline personalities. Suicides and subpsychotic episodes are more typical for the latter type. Brief reactive psychoses and dissociative disorders may coexist with a diagnosis of histrionic personality disorder. • Narcissistic personality disorder. Borderline, histrionic, and antisocial personality disorders are often comorbid with narcissistic disorders. Patients with narcissistic personality disorders are less anxious than patients with borderline disorders and their lives are less chaotic; Suicide attempts are more common in borderline than narcissistic personality disorders. Unlike the antisocial type, narcissistic patients are less impulsive, less likely to abuse alcoholic beverages and break the law. Hysterical personalities, like narcissistic ones, often display traits of exhibitionism and try to manipulate others, but they are more capable of warm emotional relationships. • Obsessive-compulsive personality disorder. Unlike obsessive-compulsive personality disorder, obsessive-compulsive disorder is characterized by true obsessions and compulsions. If the latter are present, a diagnosis of obsessive-compulsive disorder should be made. • Avoidant personality disorder. Avoidance of communication with other people is characteristic of both the schizoid and anxious types, but the schizoid patient is distinguished by the desire and lack of desire to communicate, while the anxious patient is distinguished by the desire to communicate, uncertainty and fear. The clinical pictures of the anxious and dependent types are similar, but with the anxious type, communication difficulties manifest themselves in the fear of communication, with the dependent type - in the fear of being left alone. The borderline and hysterical type are distinguished from the anxious type by the tendencies to manipulate other people, irritability and unpredictable behavior characteristic of these patients.
• Dependent personality disorder. Addiction features are found in many types of mental disorders, making differential diagnosis difficult. The clinical pictures of the anxious and dependent types are similar, but with the anxious type, communication difficulties manifest themselves in the fear of communication, with the dependent type - in the fear of being left alone. Dependence on others is also characteristic of the hysterical and borderline types, but dependent individuals usually maintain a long-term connection with the same person on whom they depend, and not with a group of people, and they have no tendency to manipulate others. Patients of the schizoid type and with schizotypal disorder tend to be isolated rather than dependent. Dependent behavior can be found in patients with agoraphobia, but agoraphobic patients also have a higher level of general anxiety or the possibility of developing panic attacks. • Passive-aggressive personality disorder. Despite the known external similarity, behavior in passive-aggressive disorder is less spectacular, dramatic, emotional and aggressive than in cases of hysterical and borderline disorders.
TREATMENT Psychotherapy and drug therapy are used to treat personality disorders. These treatments should not be pitted against each other. With the right combination of psychotherapy and drug treatment, an enhanced effect is noted. Drug therapy plays a small role in the treatment of patients with personality disorders • Antipsychotic drugs in small doses are prescribed for aggressive behavior, psychomotor agitation, decompensation of paranoid personality disorder (for example, levomepromazine 25–75 mg/day, haloperidol 5–15 mg/day) • Anxiolytic drugs (for example, diazepam, bromodihydrochlorophenylbenzodiazepine) reduce anxiety and improve the well-being of patients, but these drugs should be prescribed with extreme caution (if possible, do without them) due to the high risk of developing addiction and dependence in patients with personality disorder • With the development of depressive conditions antidepressants are used (for example, amitriptyline 75–150 mg/day). Antidepressants (especially clomipramine) are also effective in decompensating obsessive-compulsive personality disorder, manifested by symptoms of obsessive-compulsive disorder. Psychotherapy (group, family, individual, psychoanalysis) is the most preferred method of treatment. With the help of psychotherapy, they change the patient’s attitudes, his idea of his “I”, and help find ways to build correct interpersonal relationships.
Course and prognosis. • Personality disorders usually begin in childhood or adolescence and continue throughout later life. The ability to adapt to personality disorders depends on the severity of the behavioral disorder and external factors. Patients can be adapted under conditions favorable to them (compensation) and maladapted with pronounced manifestations of their characteristic psychopathic manifestations under unfavorable conditions (decompensation). Decompensating factors can be somatic and infectious diseases, intoxication, and emotional stress. The dynamics of psychopathy are closely related to age. The most dangerous periods in terms of decompensation are puberty and involution. A common feature of all pathological conditions is non-progress. After decompensation, the patient's personality returns to its original state. • Patients tend to avoid treatment. The course is chronic and progressive, leading to social and labor decompensation, but some patients may experience improvement. Synonyms • Pathological personality development • Character anomaly • Pathological character • Psychopathy
ICD-10 • F68 Other personality and behavior disorders in adulthood •• F69 Personality and behavior disorder in adulthood, unspecified
Treatment
Treatment tactics depend on the causes of the pathology, the form and characteristics of the clinical picture. Only a psychiatrist can diagnose a personality disorder, and only a specialist should prescribe treatment measures. Self-prescribed therapy may not only not bring the desired results, but can also significantly aggravate the situation.
In a state of compensation, the patient does not need drug treatment. The basis of treatment measures in this case will be group or individual psychotherapy aimed at smoothing out pathological character traits. This method will allow the patient to learn how to respond correctly to certain life situations, which in turn will help him fully adapt to society.
During the period of decompensation, a person is considered disabled; if it lasts for a long period of time, there is a possibility of disability. Therefore, this condition requires immediate treatment. In this case, in addition to psychotherapeutic influences, drug therapy is prescribed to help relieve the symptomatic manifestations of the disorder.
To reduce anxiety, depression and other painful symptoms, selective serotonin reuptake inhibitors are usually prescribed. Anticonvulsants may be prescribed to control impulsivity and temper tantrums. To combat depersonalization and depression, drugs such as risperidone Risperdal are used.
The main goal of treatment is to eliminate the stressful state and isolate the patient from the external stimulus that caused the exacerbation of symptoms. This helps to reduce the severity of clinical manifestations - anxiety decreases, the feeling of hopelessness disappears, and depression is eliminated.
Personality disorder in children
In order to start treatment on time and prevent the pathological condition from worsening, you should be attentive to the psychological health of the child. As a rule, dependent and anxious personality disorders are the most common in childhood. Most often, the development of pathology is associated with a negative home or school environment, where moral as well as physical humiliation predominates.
The anxiety type of disorder is manifested by the following symptoms:
- low self-esteem;
- tendency to awkwardness;
- hypertrophied perception of problems;
- defensive behavior;
- reluctance to communicate with peers;
- increased anxiety.
If you have an addictive disorder, you may experience symptoms such as:
- victim behavior;
- excessive sensitivity to criticism;
- shifting responsibility to others;
- feeling of loneliness;
- reluctance to make decisions independently;
- lack of confidence in one's own strength;
- unstable emotional state.
If any symptoms appear, it is advisable to contact a qualified professional. Treatment for mental disorders in children is selected as carefully as possible. As a rule, therapeutic measures are based on the use of gentle drug therapy, long-term work with a psychologist, and constant monitoring by a psychiatrist.
General prevention
Unfortunately, there is no specific standard for the prevention of various personality disorders, since each person is individual. However, it is still possible to prevent the development of mental disorders in a child. For this purpose, many mental health programs have been developed today to help parents and children solve family problems.
These types of programs are mainly educational in nature - they involve lectures and discussions aimed at understanding developmental psychology.
Adults suffering from a personality disorder should not neglect the services of a psychiatrist. If you are unable to control your emotions and reactions, it is advisable to consult with a competent specialist who will prescribe appropriate therapy.
Despite the fact that this kind of personality disorder is not a mental illness, during the period of decompensation a person is not able to independently overcome painful symptoms. Therefore, to avoid undesirable consequences, you should definitely seek medical help.
Diagnostics
Psychiatrists and psychotherapists also note that the priority is to identify the internal experiences of a person that torment him. They will need to be eliminated. But first, identify the reasons behind them. Doctors specializing in the cognitive-behavioral field usually point out to patients their mistakes in life, teach them to see prospects for the future, especially with regard to inappropriate behavior, point out to patients the futility of life's realities and try to instill in them a more suitable behavioral option.
Patients with behavior prone to dramatic behavior (it can be described as borderline, asocial, staged, narcissistic behavior) need an active, sometimes involuntary, harsh, prohibitive attitude of a psychotherapist. Sometimes people with antisocial personality disorder cannot receive outpatient treatment; they must be forcibly placed in specialized hospitals.
There are two groups of psychotherapists who treat borderline patients receiving treatment for personality disorders. Some are confident in the effectiveness of occupational therapy treatment, while others are inclined to believe that the patient must be treated now. In both cases, treatment of patients is often stopped for a long time because the patient feels anger towards his doctor, when he is suicidal or has a psychotic decompensation and needs to be urgently hospitalized.
But such aggressive, in some way, cruel tactics towards the patient can be replaced with a more gentle, bright one, treat the patient with understanding, that is, find a friendly approach.
Duration of psychotherapeutic treatment
Psychotherapeutic treatment for personality disorder usually lasts a very long time, for several years.
But, despite such a difficult, long path to improving the patient’s condition, improvements are still observed, and a lot, but there is almost no control over the data. Therefore, problems still remain unresolved in terms of the effectiveness of diagnosis and basic psychotherapeutic approaches to treatment and identification of the sources of the disease.
Current recommendations for the treatment of personality disorder include comprehensive neurometabolic therapy. For example, patients with borderline disorders with frequently changing moods and lack of control often find relief from taking tricyclic antidepressants and MAO inhibitors. For patients with disorders of the cognitive process and adaptation, components of aggression and obsessions, antipsychotics are recommended in small dosages.