This type of mental illness may also be called psychosis or paranoid symptom in medical practice. It is characterized by the presence of delusions in the patient, which are characterized by systematization. The patient is convinced that there is something false. At the same time, the perceived false is devoid of imagination and whimsicality. Among the manifestations there are the following variants of delirium:
- jealousy;
- persecution;
- dysmorphophobia;
- sensations of unrequited love and others.
Often the perceived manifestations are noticeably exaggerated or completely untrue. Diagnosis of the pathology is complicated by the variability of manifestations. Experts identify several of the most common manifestations.
Organic delusional disorder
The specificity of this variant of delusional personality disorder is a serious physiological disorder associated with the presence of focal lesions in the temporal and parietal regions of the brain, temporal lobe epilepsy. A common cause is previous encephalitis. This pathology also includes epileptic psychoses that are not accompanied by impaired consciousness. It is distinguished by specialists as a separate type of pathology.
Often accompanied by hallucinatory-delusional attacks. With them, patients lose control over aggressive impulses. Accompanied by unmotivated actions and other manifestations of instinctive behavior.
At the moment, doctors are not able to accurately determine the cause of the onset of manifestations. Observations have shown that the onset of the disease may be equally associated with bilateral genetic predisposition and damage to specific brain structures. Delusional disorders in this pathology can be acute or transient organic.
Regardless of the type, the onset is characterized by an acute onset, accompanied by symptoms such as hallucinations, perception disorders, and delusions. There is a severe disturbance in everyday behavior. Often the trigger is serious stress experienced by the patient up to 1-2 weeks before the incident.
Delusions in paranoid schizophrenia
Delirium, as the main symptom of the disorder, develops in several stages and symbolizes the “heyday” of the disease.
The first stage of its formation is called paranoid. It is characterized by systematized, interpretive delusions. The concept of systematization means that nonsense has a fairly logical, plausible structure. This stage of the disorder is not accompanied by disturbances of perception, such as hallucinations and mental automatisms.
The most common plot (theme) of delusion is the ideas of persecution, greatness and jealousy, invention, and violation of rights. Thus, a patient who lived with his father and became dependent on his sister after the death of his parent began to rave about damage caused to him by his sister. The patient stated that she infringed on him “in everything,” mocked him, took possession of his father’s inheritance and spent his, the patient’s, money.
Typically, the paranoid delusional stage is accompanied by increased activity. That is, if a person shows delusional ideas of jealousy, then he tries hard to expose his lovers, find his rival and deal with him. In the case of delusions of reformism, the patient turns to all sorts of authorities and looks for resources to implement his ideas.
Delusional themes in paranoid schizophrenia can develop gradually, subacutely or acutely.
Its acute development is accompanied by suddenness and unexpectedness in the patient’s behavior. Unreasonable aggressiveness and motor agitation appear. Thinking is disorganized, torn, or the patient develops fear of something, suspicion, anxiety, he literally becomes numb with horror.
The gradual development of delusional ideas does not cause sharp dissonance in behavior. Oddities in the patient's actions and judgments, inappropriate gestures and grimaces, and changes in interests are periodically observed. A person may complain of confusion of thoughts, emptiness in the head, and inability to concentrate.
A delusional thought, before “settling down” in the mind of a paranoid person, goes through several stages:
- expectation - the patient feels internal anxiety, tension. It is accompanied by the feeling that something big is about to happen, shedding light and dispelling darkness;
- insight - suddenly to the patient “everything becomes clear” in his unrealistic ideas. He begins to look at the world with different eyes, and he himself transforms into a different personality. The true, crazy truth is born, shedding light on the previously incomprehensible;
- systematization - this process is similar to making a mosaic. When individual pieces come together and create a complete picture. Delusional themes completely cover a person, filling his thoughts, past, future and present.
Paranoid delusions can persist for quite a long time. In this case, a diagnosis of paranoid schizophrenia is made.
Chronic delusional disorder
In chronic delusional personality disorder, persistent delusions become a persistent symptom. It accompanies a number of mental disorders. They can be characterized as:
- schizophrenic;
- affective;
- organic.
A single picture of delirium or a series of interconnected pictures develops. They can last about three months or be lifelong. The forms of the disease are varied. At the moment, experts identify several leading ones:
- Paranoid syndrome, in which delusions are not accompanied by hallucinations. Delusional states change personality, but in this situation they do not have signs of dementia, due to which patients often seem completely normal to others.
- Paranoid syndrome, in this case, delusion fits into a certain system, but is less logical and more contradictory. Hallucinations become persistent. Patients constantly hear voices in their heads. Without treatment, it leaves an imprint on your professional and personal life.
- With Paraphen syndrome, delirium becomes obsessive, fantastic, fictitious.
Determination of the type of condition is carried out only by a doctor. As well as developing a course of treatment.
Delusional disorder treatment
Therapy includes psychotherapy and medication. It is psychotherapy that turns out to be more effective, as it allows you to solve behavioral and psychotherapeutic problems. After the courses, the patient begins to control his condition and behavior. Family therapy becomes a mandatory step.
The pathology is chronic. Long-term remissions are possible. In some cases, complete recovery is noted.
Organic delusional schizophrenia-like disorder
The disorder is not of endogenous origin. Manifestations lead to the formation of a schizophrenic effect. With this lesion, the following is formed:
- pretentious nonsense;
- delusional disorders of a religious type;
- interpretive nonsense.
Hallucinations are a common secondary manifestation. An astatic and depressive-dysphoric affect occurs. During treatment, medications are used that are determined by the physician.
Hallucinatory delusional disorders
With this lesion, a characteristic feature is the presence, in the complete absence of signs of confusion, of pronounced delusional and hallucinatory disorders. Among the differences:
- confusion;
- severe anxiety;
- motor excitations.
All these manifestations are caused by the constant presence of hallucinations, which are short-lived and occur without provoking factors. They have acute and chronic forms. As the hallucinations become chronic, they become monotonous. The patient adapts to his condition and the pathology becomes less visible to others. The individual distances himself from violations.
Acute delusional disorder
Delusional disorder does not have an organic form. Delirium is devoid of bizarreness. The paranoid personality structure becomes a provocateur. The number of confirmed diagnoses increases in families where there are people with schizophrenia. Due to sthenicity, patients often convince others of the reality of delusional manifestations. Patients often suffer from persecution syndrome and change their place of residence. They are inclined to join heretical sects due to religious ideas and ideas of greatness. The object of love is often chosen by famous stage personalities who do not know about the object experiencing love. A factor confirming pathology is the presence of delusional ideas, the duration of which exceeds three months. Delusions and hallucinations do not meet the criteria for schizophrenia.
Affectively delusional disorder
Disorders associated with disturbance of affect, involving disturbances in the emotional state. They include several pathologies, the most well-known of which are bipolar or major depressive disorder. Often characterized by the manifestation of inappropriate emotions.
The classification is divided into several types of disorders:
- depressive spectrum;
- bipolar spectrum;
- manic spectrum.
Doctors often associate the presence of affective delusional disorder with creativity.
Induced delusional disorder
The pathology initially occurs in a person who is part of a close circle of relatives or friends. The patient in this situation becomes only a recipient, transmitting delusional ideas and disorders of the dominant. Moreover, a mental disorder in this “pair” is present only in the dominant personality. The recipient only copies the behavior and thoughts of the leader.
The couple is often isolated from the outside world. Only the recipient maintains minimal contact. The danger becomes the indignation experienced by the dominant when there is excessive adoration. Such relationships can occur in the same family. Recipients are often women. The patient is unable to distinguish between reality and his own view of the world, accepted from the dominant one.
First manifestations
It should be noted that the negative symptoms of the disorder are changes in the emotional background, apathy, lack of will, etc. in paranoid schizophrenia, they are noticeably less pronounced than productive symptoms. The latter include delusions, hallucinations, and thinking disorders.
At the beginning of the disease, in its initial stage, the patient may experience obsessive ideas or thoughts. For example, the fear that something bad will happen if he doesn’t count to 100 right now. Hypochondriacal thoughts, that is, increased concern about one’s health, the conviction of the presence of some kind of disease, in some cases serious, without reliable reasons, is also present. Senestopathies often appear: unusual, tormenting sensations in the body. They are characterized in a rather pretentious manner: the head is compressed by a hoop; stabbing pain in the heart, as if a needle was sticking out of it and gradually moving into its thickness. Sleep is disturbed, the patient suffers from insomnia.
The emotional background becomes scarce and inflexible, emotions are dulled, and the person is perceived as a rigid, emotionless individual. His circle of interests narrows, but isolation, suspicion and distrust appear. Patients are capable of showing aggression towards loved ones, sharply narrow their social circle, and find it difficult to establish friendly connections.
There may be manifestations of cruelty. For example, a young man suffering from paranoid schizophrenia, before the development of a full-blown clinical picture, experienced cruelty to animals. He tortured and beat cats and dogs, and hung birds by the neck.
Other signs include anxiety, concern, and fear. This makes a person confused. It is difficult for him to navigate a given situation, he hesitates, and cannot make a decision.
Symptoms of excitement and increased activity appear. The initial period of paranoid schizophrenia can last more than 10 years.
Depersonalization in a patient with paranoid schizophrenia is manifested by the feeling that something is happening to the body and thoughts, as if they do not belong to him. He cannot control his actions; he looks at them as if from the outside. Derealization makes the world around us cloudy, without colors, alien and incomprehensible.
The typical age for the onset of the disease is 30 years. Although there are often cases when it begins to manifest itself at an earlier period.
Patient L., 20 years old. He received a head injury and a fractured lower jaw as a result of being beaten by a neighbor in the yard. He underwent treatment that lasted several months. When I returned to work after sick leave, I began to show increased activity and efficiency. He tried to leave home early for work, citing the fact that they couldn’t cope there without him. I approached the mayor of the city with proposals for organizing folk festivals, holidays, and special events. He became especially agitated, lost sleep, and refused to eat. He ran through the streets, handing out invitations to City Day.
I drove to a neighboring town in my father’s car. On the way, he stopped at a store to buy provisions, but he did not have the money to pay for the goods, and he left the documents for the car as collateral. He was driving in the oncoming lane when the police stopped him. I came home by taxi to get money to buy documents. He left for documents and a car, which he left somewhere. But he returned home barefoot, on foot. He couldn't explain what happened to him.
Treatment of delusional disorder
An important feature of therapy is contacting a specialist. Only a high-level professional is able to adequately convince a patient of the unreality of his ideas.
It is for this reason that psychotherapy courses play a leading role:
- individual;
- family;
- group.
During the course, the psychiatrist and psychotherapist jointly develop a course of procedures focused on the characteristics of each individual patient.
In cases where delusional disorders are severe, medications may be prescribed. The main place on this list is occupied by antidepressants and antipsychotics. If possible, the doctor tries to give up medications in favor of folk remedies, physiotherapy, and massages. Patients are recommended to take long walks and exercise. An effective way is to choose a new hobby, a hobby that distracts you from hallucinations and delusional thoughts. Such gentle therapy is recommended in the early stages of pathology.
Service price
- HOSPITAL Day hospital5 000
- Day hospital with intensive care8,000
- 24-hour hospital (all inclusive, cost per day) 12,000
- 24-hour hospital (all inclusive, cost per day). Single occupancy24,000
- 24-hour hospital (all inclusive, cost per day). Single occupancy in a superior room 36,000
- Primary family counseling for relatives of patients undergoing inpatient treatment free of charge
- Group psychotherapy for relatives of patients undergoing inpatient treatment free of charge
- Group psychotherapy for 24-hour and day hospital patients free of charge
- Individual post for a hospital patient (if indicated)6,000
Delusional disorders in psychiatry are quite common, and they are characterized by certain conclusions that have no basis. A person comes to such false conclusions not from a real assessment of the surrounding reality, but from internal pathological disorders of thinking, perception and mood.
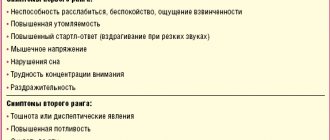
Symptoms of delusional disorder
The presence of delusions distinguishes these disorders from schizophrenia. Pathology is characterized by delusional ideas. Disorders associated with delusions of grandeur may appear; the patient may be tormented by attacks of increased jealousy. The list also includes erotomania, litigiousness and other deviations that are not characteristic of the behavior of a healthy person. The appearance of disorders is often associated with some limitations in life activity. For example, emigrants who are forced to constantly be in an unusual social environment, people suffering from hearing loss or vision loss often suffer from pathology.
The disorder rarely has an organic form. Although a connection has been identified with some neurological or oncological diseases.
The diagnostic process takes into account maintaining an understanding of what is happening and the socialization of patients.
Causes of the occurrence and development of the disease
The exact causes of the disease have not been established. It is known that the condition can develop under the influence of the following factors:
- Genetic predisposition. The presence of mental disorders in close blood relatives.
- Endogenous factor. Imbalance of special neurotransmitter substances in the human brain.
- External influences. The “trigger” for the development of pathology can be alcoholism, drug addiction, stress, and failures in personal life.
Delusional disorders in the elderly
The appearance of delusional disorders in the elderly is often associated with traumatic situations associated with the decline of the body. The most common symptom is the idea of damage; ideas of persecution of different directions are formed. There may be unmotivated complaints about the poor attitude of relatives.
In old age, the occurrence of pathology is often associated with an imbalance of substances responsible for transmitting signals in brain cells of neurotransmitters. In old age, patients often suffer from symptoms of several delusional disorders at once. They rarely manifest themselves in an acute form and usually have a chronic course. Auditory hallucinations associated with delusional symptoms often occur.
The course of therapy necessarily includes a combination of medications and psychotherapy. The pathology can be treated quite successfully, but in some situations, doctors may recommend going to a nursing home, where the elderly patient can receive constant care.
A woman is talking nonsense: what to do
Self-medication is usually ineffective. Doctor's help is needed. An integrated approach, including:
- medicinal methods,
- restorative psychotherapy,
- cognitive trainings,
- restoration of social activity,
- training for relatives and caregivers.
The psychiatrist’s task is to “switch” the patient to real phenomena. Treatment is predominantly outpatient, inpatient - in case of a serious patient’s condition and significant adaptation disorders.
Ignoring delusional disorder can lead to problems in the family, social maladjustment, and loss of relationships with loved ones. There is a risk of developing depression and paranoia.
The Leto Mental Health Center provides effective treatment for delirium in women. Our staff has extensive experience working with mental illness. We use all modern methods of therapy and help the most complex patients. Do not delay contacting until later, because the sooner help is provided, the more favorable the prognosis. We work around the clock. Call us now. Just dial 8(969)060-93-93!