Anthrax bacteria.
Photo: wikipedia.org On Tuesday, August 2, 90 people were hospitalized with suspected anthrax at the Salekhard district hospital of the Yamalo-Nenets Autonomous Okrug (YNAO). According to local authorities, the outbreak of the disease is located in the Yamal region, where the day before a dangerous infectious disease was diagnosed in eight representatives of the indigenous population, three of whom were children. As it became known later, one child died in the hospital.
Article on the topic
Gennady Onishchenko: bio-attacks on our country cannot be ruled out “Every person with the slightest deviation in health - scratches, boils, itching, runny nose - is sent for additional examination to the district hospital.
It was decided to check all children of reindeer herders even in the absence of signs of illness. Today, 90 people taken from the anthrax outbreak are in the Salekhard hospital. All the dynamics are good. Doctors monitor their condition around the clock. There are about 50 children among those hospitalized,” said Natalya Khlopunova, press secretary of the governor of the Yamal-Nenets Autonomous Okrug. Earlier it was reported that on July 25, a quarantine was introduced in the Yamal-Nenets Autonomous Okrug due to anthrax, which killed more than 2.3 thousand deer.
According to local authorities, the outbreak of infection was caused by an unusually warm summer for the Far North: for a month in Yamal there was an abnormal heat of up to 35 degrees. Dozens of reindeer herders and their families were taken from the quarantine zone to an area “clean” from anthrax - 60 km from the outbreak. Anthrax is a deadly infectious disease that can be transmitted from a sick animal to humans and is characterized by a high degree of intoxication and, mainly, specific skin damage.
Article on the topic
Mister Quicksilver, aka Prodigy. Ilya Mechnikov experimented on himself. Anthrax has been known since ancient times. It is also called a malignant carbuncle or anthrax (translated from Greek as coal). The disease received its current name “anthrax” from the region where the epidemic spread, when in the 18th-19th centuries in pre-revolutionary Russia the disease covered a significant part of the territory of western Siberia.
In 1788, the Russian doctor Stepan Andreevsky conducted extensive research on a little-known disease that affected the Western Siberian provinces, and described the results in his work “On Anthrax,” which has not lost its significance to this day. In addition, during the self-infection experiment, Andreevsky established the identity of anthrax in animals and humans and proved the possibility of its transmission from animals to people.
The causative agent of the disease
The causative agent of anthrax is the bacterium Bacillus anthracis. It looks like a large stick with the ends cut off. Outside the human or animal body, it forms spores that can persist in the environment for years. The optimum temperature for growth is 35-37 °C. The spores are very stable and can persist for a long time under the most unfavorable conditions.
Article on the topic
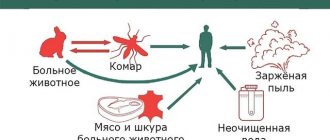
Benefactor of humanity. How Louis Pasteur created the first vaccinations Sources of the disease are herbivores, cattle, horses, sheep, goats, pigs, camels, and deer. Cats, dogs and birds almost never get this disease. The source of infection is the feces, saliva and other secretions of sick animals, which remain extremely contagious throughout the entire period of the disease. Transmission of bacteria occurs through the bites of burner flies and horse flies, which carry the pathogen from sick animals, infected corpses and environmental objects to healthy animals. After the death of animals with anthrax, the bacteria affect all organs, even the skin, fur and bones. In the soil, the pathogen can not only persist, but also under certain conditions (temperature not lower than 12-15 ° C, humidity 29-85%, neutral or slightly alkaline environment, etc.) continues to multiply for many years.
A person can become infected with anthrax through contact with sick animals, processing their skins, eating foods contaminated with spores, as well as through water, soil, and fur products. The infection is practically not transmitted from person to person.
anthrax
Anthrax (malignant carbuncle, anthrax) is a particularly dangerous infectious disease of agricultural and wild animals of all types, as well as humans. The disease occurs with lightning speed, hyperacute, acute and subacute (in sheep and cattle), acute, subacute and anginal (in pigs), mainly in the carbunculous form in humans. There are also oropharyngeal and gastrointestinal forms[1]. Characterized by intoxication, the development of serous-hemorrhagic inflammation of the skin, lymph nodes and internal organs; occurs in the skin or septic form (intestinal and pulmonary forms are also found in animals).
origin of name
Anthrax, known since ancient times under the names “sacred fire”, “Persian fire”, etc., was repeatedly mentioned in the works of ancient and oriental writers and scientists. A detailed description of the clinical picture of this disease was made by the French physician Moran in 1766. In pre-revolutionary Russia, due to its predominant spread in Siberia, this disease was called “anthrax,” when the Russian doctor S. S. Andreevsky in 1788 described in his essay “On Anthrax” a large epidemic of this infection in the Western Siberian provinces, and in the experience of self-infection he established the identity of anthrax in animals and humans and proved the possibility of its transmission from animals to humans.
Pathogen
The causative agent of the disease was almost simultaneously described in 1849-1850 by three researchers: A. Pollender, F. Brawell and K. Daven. In 1876, R. Koch isolated it in pure culture. Of all the bacteria pathogenic to humans, the causative agent of anthrax was the first to be discovered. The generally accepted name for anthrax today is anthrax, from ancient Greek. ἄνθραξ “coal, carbuncle”: this name was given by the characteristic coal-black color of anthrax scab in the skin form of the disease. The causative agent of anthrax is the bacillus Bacillus anthracis. It is a large spore-forming gram-positive rod measuring 5-10 × 1-1.5 microns. Anthrax bacilli grow well on meat-peptone media, contain capsular and somatic antigens and are capable of secreting an exotoxin, which is a protein complex consisting of an edema-causing (increased cAMP concentration), protective (interacts with cell membranes, mediates the activity of other components) and lethal (cytotoxic effect, pulmonary edema) components. Capsule - antiphagocytic activity. The anthrax bacterium forms spores outside the body when oxygen is available, as a result of which it is highly resistant to high temperature, drying and disinfectants. Anthrax spores can persist for years; pasture contaminated with feces and urine from sick animals can retain anthrax spores for many years. Vegetative forms of anthrax bacillus quickly die when boiled and exposed to conventional disinfectants. When autoclaving, spores die at a temperature of 110 ° C only after forty minutes. Dry heat at 140°C kills spores in two and a half to three hours. Anthrax spores can withstand direct sunlight for ten to fifteen days. Activated solutions of chloramine, hot formaldehyde, and hydrogen peroxide also have a sporicidal effect.
Epizootology
The source of infection are sick farm animals: cattle, horses, donkeys, sheep, goats, deer, camels, in which the disease occurs in a generalized form. Pets - cats, dogs - are not very susceptible.
Anthrax in animals is characterized by the following features:
- short incubation period, usually not exceeding 3-4 days;
- pronounced clinical picture in the form of a severe febrile state, decline in cardiovascular activity, meningeal phenomena, bloody diarrhea and vomiting;
- rapid development of the infectious process, ending in the death of animals within, as a rule, the first 2-3 days.
Cattle and horses: usually occurs acutely and subacutely. Characterized by: (septic form) a sharp increase in temperature, apathy, decreased productivity, swelling of the head, neck and chest; (intestinal form) apathy, refusal to feed, bloody diarrhea and vomiting, tympany.
Pigs: (anginal form) occurs only in pigs and is asymptomatic; changes can be detected only during a veterinary and sanitary examination of carcasses based on characteristic catarrhal-hemorrhagic inflammation of the lymph nodes. Epizootics of anthrax are geographically tied to soil foci - repositories of pathogens. Primary soil foci are formed as a result of direct infection of the soil with secretions of sick animals on pastures, in places where animals are kept in stalls, in places where corpses are buried (cattle burial grounds), etc. Secondary soil foci arise by washing off and introducing spores into new territories by rain, melt and sewage waters. Infection can occur with the participation of a large number of transmission factors. These include secretions from the skin of sick animals, their internal organs, meat and other food products, soil, water, air, and environmental objects contaminated with anthrax spores. Susceptibility to anthrax in humans does not depend on age, gender and other physiological characteristics of the body; it is related to the routes of infection and the magnitude of the infectious dose.
Pathogenesis
The portal of infection for anthrax is usually damaged skin. In rare cases, the bacillus penetrates the mucous membranes of the respiratory tract and gastrointestinal tract. At the site of penetration of the pathogen into the skin, an anthrax carbuncle appears in the form of a focus of serous-hemorrhagic inflammation with necrosis, edema of adjacent tissues and regional lymphadenitis. The local pathological process is caused by the action of anthrax bacillus exotoxin, individual components of which cause severe microcirculation disorders, tissue edema and coagulative necrosis. Regardless of the entrance gate of the infection, the first stage is a localized lesion of regional lymph nodes, the second stage is the generalization of the process. Generalization of infection with the breakthrough of anthrax pathogens into the blood and the development of a septic form occurs extremely rarely with cutaneous anthrax. Anthrax sepsis usually develops when the pathogen enters through the mucous membranes of the respiratory tract or gastrointestinal tract. In these cases, disruption of the barrier function of the tracheobronchial or mesenteric lymph nodes leads to generalization of the process. Bacteremia and toxinemia can cause the development of infectious-toxic shock.
The pathogenesis is based on the action of the pathogen exotoxin, which consists of at least three components or factors:
- first (I), edema (inflammatory) factor;
- second (II), protective (protective) factor;
- third (III), lethal factor. Adding factor I to factor II increases the immunogenic properties, factor III reduces them.
A mixture of factors I and II causes an increase in the inflammatory response and edema due to an increase in capillary permeability. A mixture of factors II and III enhances the effect of the lethal factor and leads to the death of guinea pigs, rats and mice. A mixture of three factors of anthrax toxin (I, II, III) has an inflammatory (edematous) and lethal effect. The morphological essence of anthrax sepsis is acute serous-hemorrhagic, hemorrhagic, and less often - fibrinous-hemorrhagic inflammation. The leukocyte reaction in foci of inflammation during sepsis is weak or absent. In the organs of immunogenesis (spleen, lymph nodes, thymus) there is suppression of the body’s immune defense with the replacement of lymphoid tissue by macrophages and the presence of a primitive protective reaction in the form of macrophage incomplete phagocytosis of the pathogen.
Clinical picture
The duration of the incubation period ranges from several hours to days, most often 2-3 days. The disease can occur in a localized (skin) or generalized (pulmonary and intestinal) form.
Cutaneous anthrax
Occurs in 98-99% of all anthrax cases. Its most common type is the carbunculous form; edematous, bullous and erysipeloid forms of the disease are less common. Predominantly exposed parts of the body are affected; The disease is especially severe when carbuncles are localized on the head, neck, mucous membranes of the mouth and nose. The clinic of generalization of anthrax infection, regardless of the form - cutaneous or visceral - with an extreme variety of manifestations in the initial period of the disease in the terminal stage is the same: it is accompanied by the emergence of peripheral blood of anthrax bacteria, the concentration of which reaches hundreds of thousands and millions of bacterial cells in 1 mm³ of blood, which can be considered as anthrax sepsis (see), and represents a clinic of infectious-toxic shock. These are severe disorders of the blood coagulation and anticoagulation systems, acidosis, acute renal failure, a drop in body temperature below normal, and severe intoxication. Usually there is one carbuncle, but sometimes their number reaches 10-20 or more. At the site of the entrance gate of infection, a spot, papule, vesicle, and ulcer develop successively. A painless spot of a reddish-blue color and a diameter of 1-3 mm, resembling an insect bite, after a few hours it turns into a copper-red papule. Itching and burning sensation increases. After 12-24 hours, the papule turns into a blister with a diameter of 2-3 mm, filled with liquid, which darkens and becomes bloody. When scratching (sometimes spontaneously), the vesicle bursts, and in its place an ulcer forms with a dark brown bottom, raised edges and serous-hemorrhagic discharge. After a day, the ulcer reaches 8-15 mm in diameter. As a result of necrosis, after 1-2 weeks the central part of the ulcer turns into a black, painless, dense scab, around which there is a pronounced red inflammatory ridge. Externally, the scab resembles a coal in a flame, which was the reason for the name of this disease (Antrax - coal). This lesion is called a carbuncle.
Septic anthrax
The septic form is quite rare. The disease begins acutely with tremendous chills and an increase in temperature to 39-40 ° C. Severe tachycardia, shortness of breath, tachypnea, chest pain and cough with the release of foamy, bloody sputum are observed. Signs of pneumonia and pleural effusion are determined. With the development of infectious-toxic shock, hemorrhagic pulmonary edema occurs. A large number of anthrax bacteria are found in the blood and sputum. Some patients experience abdominal pain, nausea, bloody vomiting, and loose bloody stools. Subsequently, intestinal paresis develops, and peritonitis is possible. Symptoms of meningoencephalitis are detected. Infectious-toxic shock, edema and swelling of the brain, gastrointestinal bleeding and peritonitis can cause death in the first days of the disease.
Diagnostics
The diagnosis is made on the basis of clinical, epidemiological and laboratory data. Laboratory diagnostics include bacterioscopic and bacteriological methods, and for the purpose of early diagnosis - immunofluorescence. Allergological diagnosis of anthrax is also used using an intradermal test with anthraxin, which gives positive results after the 5th day of illness. The material for laboratory research is the contents of vesicles and carbuncles, as well as sputum, blood, feces and vomit in the septic form. Anthrax is distinguished from glanders, common boils and carbuncles, plague, tularemia, erysipelas, pneumonia and sepsis of other etiologies.
Treatment and prevention
Causal therapy for anthrax is carried out with antibiotics. Penicillin is prescribed. In pathogenetic therapy, colloid and crystalloid solutions, plasma, albumin, and glucocorticosteroids are used. Surgical interventions for the skin form of the disease are unacceptable: they can lead to generalization of the infection. Preventive measures are carried out in close contact with the veterinary service. Identified sick animals should be isolated and their corpses burned; infected objects must be disinfected. Chamber disinfection is used to disinfect wool and fur products. Persons who have been in contact with sick animals or infectious material are subject to active medical observation for 2 weeks. Vaccination of people and animals with dry live anthrax vaccine is important. The first vaccine was invented and tested by the French microbiologist and chemist Louis Pasteur.
Forecast
The prognosis is largely determined by the form of the disease, in general it is conditionally unfavorable and death is possible even with adequate and timely treatment. In the absence of appropriate treatment for the cutaneous form, the mortality rate is 10-20%. In the pulmonary form of the disease, depending on the strain of the pathogen, mortality can exceed 90-95%, even with appropriate treatment. Intestinal form - about 50%. Anthrax meningitis - 90%.
Epizootological situation
Outbreaks of anthrax are recorded in Russia to this day. So on July 23, 2021, a notification from the veterinary supervision appeared about the death of deer in one area of tundra in the Yamal region. On August 3, 2021, reports of an anthrax epidemic appeared in the Yamalo-Nenets Autonomous Okrug. The Armed Forces of the Russian Federation were involved in eliminating the anthrax outbreak. On November 9, 2016, in the north of the Volgograd region, in the Nekhaevsky district, bordering the Rostov and Voronezh regions, a case of death of a cow was established
Forms of the disease
This disease usually occurs in the cutaneous form; pulmonary, intestinal and septic forms are rare. Even with timely treatment, anthrax can be fatal.
Article on the topic
"Gift" from Utah. The US military mistakenly sent out anthrax. Thus, with the pulmonary form (inhalation of spores or vegetative pathogens), the mortality rate reaches 100%. With the intestinal form, the patient does not survive in 50% of cases.
In the most common form, the cutaneous form, the mortality rate is 10-20%. With it, 2-3 days after infection, a person develops a reddish spot that turns into a vesicle. Then the bubble bursts, and in its place an ulcer with a black bottom appears. New blisters soon appear around this scab, and eventually a scab-carbuncle (necrotic inflammation of the deep layers of the skin) is formed. There is no sensitivity in the area of the ulcer, and the tissue around it swells.
With the development of ulcers, the patient's temperature rises, fever begins, and weakness, headache and tachycardia are also noted.
Classification
Anthrax is divided into two types - cutaneous and general (generalized). In turn, each of these varieties has several more forms.
There are three types of skin forms of the disease:
- Carbunculous - manifestations on the skin change from red spots to nodules, and then to dark ulcers. The patient is worried about weakness, chills, fever .
- Edematous - in the first days of the disease, large swelling appears on the skin. Later, a scab is observed, around which the skin turns red.
- Bullous - the disease begins with the appearance of blisters on the skin. Later they burst, resulting in extensive ulcers. Later, a characteristic black crust appears on their bottom.
The general (generalized) form is divided into three types:
- Pulmonary – the respiratory organs are affected. With this form of the disease, the prognosis is most often unfavorable.
- Intestinal - very difficult, there are signs of gastrointestinal damage and general intoxication. High risk of death, even if the patient is provided with adequate treatment.
- Septic – sometimes develops immediately, sometimes as complications of other forms. There is general intoxication and bleeding in the internal organs. Inflammation of the membranes of the brain and failure of internal organs often occur.
Treatment and prevention
Anthrax is treated with antibiotics. It is aimed at combating the pathogen and increasing the patient’s body’s defenses. If the course of the disease is favorable, after 5-7 days the temperature drops sharply, and a scar forms in place of the scab. If the outcome is unfavorable, secondary sepsis and death may develop.
Anthrax is a very dangerous disease, so the veterinary service takes preventive measures to prevent an epidemic. In areas where it is detected, quarantine is introduced, and the population is evacuated to safe places.
Animals with anthrax are isolated and their corpses are burned. Disinfection of infected objects is also carried out.
Vaccination of people and animals is of great importance for the prevention of anthrax.
Tests and diagnostics
If anthrax is suspected, doctors use a specific diagnostic algorithm based on laboratory and clinical-epidemiological data. Initially, the doctor analyzes the complaints, assessing the order in which they appeared. Also in the diagnostic process, an epidemiological history is important - an assessment of contact with infected animals, as well as contacts with other people after infection.
A general external examination is carried out, during which the doctor determines the presence of external signs of the disease, performs palpation and percussion to identify disorders of the internal organs.
The following laboratory methods are used in the research process:
- bacterioscopic;
- bacteriological;
- immunofluorescence (for early diagnosis).
Allergological diagnostics can also be used, which makes it possible to obtain a positive result after the fifth day of illness.
For laboratory tests, material is taken from carbuncles, and in the general form, blood, sputum, vomit, and feces are examined.
For complex diagnostics, the anthrax allergen is used - anthraxin .
Consequences and complications
Anthrax can lead to serious complications, including:
- Brain swelling.
- Inflammation of the membranes of the brain.
- Bleeding in internal organs.
- Intestinal paresis.
- Inflammatory process in the intestines and abdominal cavity.
- Pneumonia.
- Pulmonary edema.
- A drop in blood pressure to a state incompatible with life.
Diet
Diet 13 table
- Efficacy: therapeutic effect after 4 days
- Time frame: no more than 2 weeks
- Cost of products: 1500-1600 rubles per week
Patients are recommended to follow Diet 13 table . Recommended dishes include lean meat and fish, slimy soups and low-fat broths, dairy products, eggs, cereal porridges, vegetables, fruits, tea, rose hip decoction, etc.
A number of products are prohibited from consumption. This list includes:
- Spicy dishes.
- Fat meat.
- Fresh bread and pastries.
- Sausages and canned food.
- Fat cheeses and sour cream.
- Products that increase gas formation - legumes, cabbage.
- Coffee, alcohol.
More detailed information is contained in the “diet” presentation.