What is this?
Tularemia is a bacterial infection that can be contracted through contact with wild animals or ticks.
It is not as well known as rabies or tick-borne encephalitis, although it causes a lot of problems for humans. The disease causes inflammation and suppuration of the lymph nodes, which sometimes have to be removed. The clinical form of tularemia depends on the method of penetration of the pathogen into the human body. Most often, after infection with tularemia, damage to the lymphatic system develops (the lymph nodes become inflamed); the disease affects the skin and mucous membranes of the eyes, pharynx and lungs. An acute disease is accompanied by high fever and signs of intoxication.
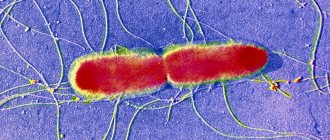
The source of tularemia infection is the bacterium Francisella tularensis. This is a very tenacious microbe that can survive for a long time in water, soil, grain and straw. It is stable in the environment, able to survive at very low temperatures. Surprisingly, F. tularensis remains viable even after being deep frozen for a long time. It can be stored in ice for more than 10 months, and in frozen meat for up to 3 months. At the same time, the bacterium is sensitive to ultraviolet radiation, heat and the effects of disinfectants. For example, upon contact with a Lysol solution, the causative agent of tularemia dies within 3–5 minutes.
How does infection occur? Vectors of infection and routes of transmission
Various types of rodents, birds, dogs, sheep and goats make a major contribution to the spread of infection. Despite the fact that the natural reservoir of tularemia is mainly mammals, the main carrier of the disease is insects that feed on the blood of infected animals, including ticks of the genus Ixodes. In addition to a tick bite, the cause of illness in humans can be:
- direct contact with an infected animal;
- eating raw foods and unboiled water;
- inhalation of dust in industries where plant materials are processed or livestock is slaughtered (Fig. 1).
The disease is not transmitted from person to person.
Important! Tularemia is extremely contagious and, when it enters the human body, causes disease in almost 100% of cases.
Figure 1. How a person becomes infected with tularemia. Source: CC0 Public Domain
Foci of tularemia appear every now and then in: Russia, Kazakhstan, Turkmenistan, countries of Eastern Europe. To a lesser extent, tularemia is common in Western Europe, the USA, Canada, China and Japan.
In Russia, the European part of the country and Siberia are considered dangerous from the point of view of tularemia infection. The spread of the infection is being carefully monitored, despite the relatively low incidence - in 2021, only 71 cases of the disease were registered in our country.
The seasonality of the infection (increased incidence usually occurs in summer and autumn) is associated with the period of activity of ticks and other blood-sucking insects. Previously, most human cases were recorded in rural areas, where people are more likely to come into contact with animals and be in nature. However, in recent years, about ⅔ of all cases are city residents. The reason for this is the frequent trips of city residents to the forest or to their dachas, as well as the consumption of raw meat.
Who is at risk?
The risk group for tularemia includes people who frequently come into contact with animals or agricultural raw materials:
- hunters,
- fishermen,
- veterinarians,
- shepherds,
- animal shelter staff,
- livestock workers,
- cooks,
- agricultural workers, etc.
Forms of the disease
After entering the body, the tularemia bacillus attacks the lymph nodes, as well as internal organs - the liver, spleen, and less often - the lungs. Depending on how a person became infected, the disease manifests itself differently (Table 1).
| Table 1. Clinical forms (classification) of the disease | |||
| Form of the disease | Type of infection | Which organs are affected? | Symptoms |
| Bubonic | Through the skin | The lymph nodes | Lymph nodes enlarge significantly, sometimes reaching the size of a chicken egg. The contours of the lymph nodes (buboes) are clear. They hurt when pressed. As the disease progresses, the buboes may dissolve or fester. Possible formation of abscesses and fistulas |
| Ulcerative bubonic | After being bitten by a tick or other insect | Bite site | A small ulcer with a dark bottom appears at the site of the bite, which heals very slowly |
| Oculo-bubonic | In case of contact with eyes with dust or dirty hands | Eyes, lymph nodes | Conjunctivitis: inflammation of the eyes with redness, swelling, tenderness and stinging. Papular formations, which then turn into wounds and purulent ulcers |
| Anginal-bubonic | After drinking contaminated food or water | Pharyngeal mucosa, lymph nodes | High temperature, enlarged lymph nodes. Sore throat, problems swallowing, redness and swelling of the tonsils. The tonsils are enlarged and covered with a gray coating that is difficult to remove. Later, long-healing ulcers form on the tonsils, and then scars |
| Abdominal | After drinking contaminated food or water | Lymphatic vessels in the intestines | Abdominal pain, nausea, vomiting, weight loss |
| Pulmonary | After inhalation of contaminated dust | Bronchial lymph nodes, lungs | Fever, cough, chest pain |
| Generalized | Does not depend on the type of infection, but most often develops when the pathogen is inhaled | Spread of infection through blood, sepsis | Fever, weakness, confusion, headache, muscle pain |
The incubation period of tularemia, when there are no symptoms yet, usually does not exceed 3-7 days. The first manifestation of the disease is a high temperature, which rises to 38-40 °C. After this, the patient begins to suffer from muscle pain and headaches, feels constant weakness and dizziness. The fever lasts a long time and subsides only after 2-3 weeks.
During the examination of the patient, the doctor observes redness and swelling of the face, a noticeable increase in the vascular network of the eyes or “red eye” syndrome, and dark red spots – hemorrhages – are visible on the mucous membrane of the mouth. The tongue is covered with a white or gray coating. The main characteristic sign of infection is greatly enlarged lymph nodes (Fig. 2).
Figure 2. Lymphadenitis due to tularemia. The disease often affects the cervical lymph nodes. Source: Coronation Dental Specialty Group
In the later stages of the disease, blood pressure decreases and the pulse becomes rarer. On the fifth day from the moment the first symptoms appear, a severe dry cough develops. Most patients have an enlarged liver and spleen.
Pathogenesis
The entrance gates of infection often become microtraumas of the skin, less often the mucous membranes of the eyes and respiratory organs, and the digestive tract. For the development of the disease upon penetration through the skin or lungs, 10-50 viable microorganisms are sufficient.
After penetration into the body, the pathogen begins to rapidly multiply, and a primary focus of infection is formed. Then the bacteria penetrate the nearby lymph nodes and release toxins, which enter the blood and are carried throughout the body through the bloodstream, causing general intoxication (poisoning). As the disease progresses, multiple enlargement of the lymph nodes develops, granulomas (foci of inflammation) form in different organs (liver, spleen, lungs).
Diagnostics
Considering the strong seasonality, locality, occupation characteristic of a high risk of infection, and pronounced symptoms, the clinical diagnosis of tularemia is not very difficult.
Laboratory diagnosis is confirmed by identifying antibody titers or x-ray (for the pulmonary form). Bacteriological and PCR methods make it possible to detect the presence of a pathogen in biological samples taken from a patient.
Which doctor should I contact?
Having felt the symptoms and arrived at the clinic, the patient goes to the local therapist. He, in turn, gives a referral to an infectious disease specialist, who makes a decision on hospitalization.
An infectious disease specialist diagnoses and treats tularemia.
Tests for tularemia
There are several methods for laboratory diagnosis of tularemia.
Allergological methods
At an early stage of the disease, starting from the third day after the onset of symptoms, an allergy test is used for diagnosis. The test involves injecting the patient subcutaneously with tularemia antigen. In case of infection, the diameter of the swelling at the injection site is larger than usual in healthy people - at least 0.5 cm. The test results are assessed 24, 48 and 72 hours after the injection.
Serological methods
Serological diagnostic methods (agglutination reactions and passive hemagglutination) involve examining patient blood samples for the presence of specific antibodies. Depending on the chosen method, the disease can be diagnosed already on the 7-15th day of its course.
Bacteriological diagnostic methods
The bacteriological method consists of isolating the infectious agent from blood samples or the contents of the patient’s ulcers and buboes on days 7-10 after infection. The bacteria are then grown in a special nutrient medium. This approach to diagnosing tularemia is used very rarely because of its labor intensity, and also because not all laboratories have permission to work with F. tularensis.
Polymerase chain reaction
Polymerase chain reaction (PCR) is a diagnostic method that allows you to detect pathogen DNA in a biological sample. The sensitivity and specificity of PCR are not inferior to agglutination and passive hemagglutination reactions, and the method can be used already on the 10th day of illness.
“Tularemia in Russia in the recent past,” reports A.A. Nafeev, a sanitary doctor at the Center for Hygiene and Epidemiology in the Ulyanovsk Region, was one of the most common natural focal infections. Despite the successes achieved in the fight against this infection, cases of the disease are still registered annually. This dictates the need to improve sanitary and epidemiological surveillance, as well as the constant vigilance of outpatient doctors in relation to the first symptoms of tularemia.”
Diet for tularemia
Diet 13 table
- Efficacy: therapeutic effect after 4 days
- Time frame: no more than 2 weeks
- Cost of products: 1500-1600 rubles per week
The diet for hospitalization of patients with tularemia is usually prescribed by an infectious disease specialist, depending on the type of disorder - intestinal, nephrological, hepatobiliary, etc. Most often, the diet meets the standards of a complete balanced diet and is rich in vitamins .
Patients can be offered Table 13 , which helps maintain general strength and increase resistance to infections, reduce intoxication, and also has a beneficial effect on the digestive organs during fever and bed rest. This menu usually consists of:
- milk porridges;
- natural compotes and decoctions;
- pureed vegetable soups and meat broths;
- easily digestible proteins - boiled meat, steamed cutlets, omelettes and fish;
- fermented milk drinks.
Treatment
The treatment of tularemia is based on antibiotic therapy. To defeat a disease, it is necessary to destroy its source - the bacterium.
Drug therapy aimed at combating the infectious agent
The generally accepted standard of treatment for tularemia is antibiotics from the aminoglycoside and tetracycline groups. Third-generation cephalosporins and fluoroquinolones are used as second-line drugs.
The course duration is usually two weeks. In the event of a relapse of the disease, a drug that was not used during the first wave of the disease is chosen to continue treatment, since the bacteria could have acquired resistance to the previously used antibiotics.
Symptomatic treatment
Patients with symptoms are recommended bed rest and a balanced diet rich in vitamins. The ward is disinfected daily.
As symptomatic treatment, drugs are used to reduce the harmful effects of intoxication, allergic reactions and inflammation. Vitamins and medications may be prescribed to support the cardiovascular system. In case of eye damage, they are washed and instilled with a 20-30% solution of sodium sulfacyl 2-3 times a day. For tularemic sore throat, gargling is prescribed.
Treatment of ulcers
To treat ulcers and speed up the resorption of buboes, compresses and bandages with ointment are used. Physiotherapy procedures may be indicated: exposure to heat, blue light, laser irradiation, etc.
If the bubo has festered, it is opened and cleaned.
Possible complications
The vast majority of patients with tularemia can be cured without consequences. But in approximately 1-2% of cases of the disease, complications are observed, mainly related to the generalized form of tularemia.
Common complications include:
- meningitis and meningoencephalitis,
- secondary pneumonia,
- infectious psychosis after tularemia,
- chronic joint damage - polyarthritis,
- progressive heart disease - myocardial dystrophy,
- chronic course with frequent relapses.
Mortality with tularemia is less than 3%, with a generalized form - 30-60%.
Prevention
To protect yourself from infection, you should remember to take precautions while being in nature, when contacting animals, and eating meat and animal products. Vaccination remains the most effective method of prevention.
Is there a vaccine? Is it effective?
The most reliable way to protect yourself from infection is to get vaccinated. The effectiveness of vaccination against tularemia exceeds 90%; in Russia it is recommended for adults and children over 7 years old living in dangerous regions.
To protect against infection, a live vaccine containing weakened bacteria that cannot cause disease is used. On days 5–7 and 12–15 after vaccination, the strength of immunity is assessed. If immunity is not formed, re-vaccination is carried out. The state of immunity of vaccinated people is checked 5 years after vaccination and subsequently every 2 years.
Emergency unscheduled preventive vaccination is carried out in the presence of epidemiological indications:
- in case of illness of people in this territory,
- with intensive reproduction of rodents,
- with widespread carriage of tularemia among one or more animal species over a large territory.
Precautions in nature
Measures to reduce morbidity include controlling the spread of infection, carrying out deratization measures and disinsection of hazardous areas.
In case of a water outbreak, it is forbidden to drink unboiled water, as well as to swim. To reduce the risk of infection from tick and mosquito bites, it is recommended to use repellents, wear closed clothing, and limit the entry of unvaccinated people into disadvantaged areas.
To prevent commercial infections, it is advisable to use gloves when removing skins from killed rodents and to disinfect your hands.
It is necessary to carry out sanitary education work among the population of areas disadvantaged by tularemia. Persons who have been in contact with the patient are not isolated, since the sick are not contagious. The patient's home is disinfected.
Classification
Depending on the course and form, tularemia can be ulcerative-bubonic, conjunctival-bubonic, anginal-bubonic, abdominal (intestinal), broncho-pneumonic with a bronchilitic and pneumonic type of course, generalized (primary septic).
Depending on the area of distribution, the infection can be of different types:
- A - Nearctic, widespread in North America, is highly pathogenic for the human population, as well as rabbits, bacteria are capable of fermenting glycerol and producing citrulline ureidase ;
- B - Holarctic, was registered in Europe and Asia, has moderate pathogenicity for humans and various rodents, bacteria are not capable of fermenting glycerol, there is no citrulline ureidase in the structure, it can be isolated from water or its inhabitants, this type is most typical for areas of the Russian Federation;
- C - Central Asian - the infection is low-pathogenic for rabbits; bacteria are capable of fermenting glycerol and citrulline .