Causes
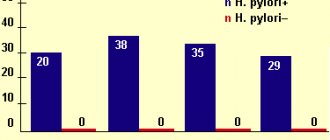
Helicobacter pylori. Duodenal ulcers in most cases develop against the background of damage to the body by the bacterium Helicobacter Pylori. Among the features of its vital processes are the production of substances that damage the mucous membrane of the stomach and duodenum, as well as the production of ammonia, leading to an increased secretion of hydrochloric acid.
Regular use of NSAIDs. The development of this disease can be caused by regular use of non-steroidal anti-inflammatory drugs, such as diclofenac, ibuprofen, acetylsalicylic acid (aspirin), etc. It is important to consider that these drugs in some cases pose a major threat to the duodenum.
Wrong lifestyle. Factors contributing to the development of duodenal ulcer include alcohol abuse, smoking, and poor diet.
Heredity. One of the possible causes of duodenal ulcer is heredity. Statistics indicate that the presence of an ulcer in one of the parents determines its occurrence in the child in the future by 40%.
Peptic ulcer of the stomach and duodenum
Which doctors should I contact?
If symptoms of gastric and duodenal ulcers appear, you should contact or. The doctor will draw up an individual examination and treatment plan, taking into account the clinical form of the disease, and, if necessary, prescribe consultations with specialists. Observation is often required to select rational diet therapy, drug treatment and prevention of exacerbations. In case of development of surgical complications of peptic ulcer, consultation is necessary. In the presence of concomitant diseases, such as diabetes mellitus and heart failure, participation in the selection of therapy will be required. If a peptic ulcer has developed against the background of severe psycho-emotional stress, consultation with a medical psychologist or psychiatrist is necessary.
Treatment of gastric and duodenal ulcers
Treatment of gastric and duodenal ulcers is complex and includes diet therapy, medical conservative and surgical treatment. With conservative drug therapy for peptic ulcer associated with H. pylori, two eradication treatment regimens (aimed at destroying the pathogenic microorganism) are possible: three-component and four-component therapy.
Triple standard therapy includes proton pump inhibitors and antibacterial drugs of two groups in different dosages. In addition to the proton pump inhibitor and antibacterial drugs of two groups, the four-component therapy for peptic ulcer includes bismuth preparations.
Choosing a treatment regimen and calculating dosages of antibacterial drugs is the responsibility of the doctor, who will tell you in detail about the duration of therapy, the frequency of drug administration, and how to check the effectiveness of the chosen treatment.
If these treatment regimens are ineffective, individual options are used, selected taking into account sensitivity to antibacterial drugs.
In the case of peptic ulcer not associated with H. pylori, proton pump inhibitors and h2-blockers are used to reduce the secretion of hydrochloric acid and reduce the impact of aggressive factors on the mucous membrane of the wall of the stomach and duodenum. Also, to relieve symptoms for a short time, the doctor may prescribe antacids; in case of gastrointestinal motility disorders, antispasmodics and prokinetics.
Surgical treatment of peptic ulcer is used when complications develop that cannot be suppressed by conservative treatment methods.
Complications of gastric and duodenal ulcers
Complications of gastric and duodenal ulcers are life-threatening conditions.
If symptoms of a complicated ulcer appear, you should urgently seek medical help. Bleeding
is one of the most dangerous and rapidly developing complications of peptic ulcer disease. Its sign is the presence of blood in the vomit (black or dark brown vomit, “coffee grounds”) and/or black tarry stool. The development of bleeding is accompanied by pain, which stops abruptly, but sudden weakness and dizziness occur, blood pressure decreases, the pulse quickens, and loss of consciousness is possible. With minor bleeding, blood is found in the stool.
Perforation of the organ wall
accompanied by “dagger” pain in the abdomen, severe weakness, dizziness, weak pulse, low blood pressure, nausea, and vomiting.
Ulcer penetration
into neighboring organs (penetration) is characterized by abdominal pain, which can radiate to the back, vomiting, which does not bring relief.
Stenosis of the pyloroduodenal zone
, or narrowing of the ulcer site. As a result of a decrease in the diameter of the outlet of the stomach and duodenum, food stagnation occurs in the stomach, bad breath appears, vomiting of “yesterday’s” food, pain and a feeling of heaviness in the abdomen.
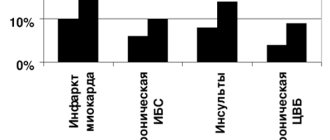
Peptic ulcer of the stomach and duodenum is a precancerous condition and increases the risk of developing stomach cancer
several times.
Prevention of gastric and duodenal ulcers.
Specific prevention of gastric and duodenal ulcers has not been developed.
The main measures to prevent ulcer formation include: normalizing the work and rest regime, giving up bad habits, eradicating H. pylori in infected individuals, limiting the use of painkillers (if long-term use of non-steroidal and steroidal anti-inflammatory drugs is necessary, they must be combined with antisecretory drugs).
An important component of the prevention of peptic ulcer disease and its relapse is adherence to the principles of proper nutrition.
Limit very hot and spicy dishes and alcohol. Long breaks between meals are unacceptable.
To prevent relapses of the disease, sanatorium-resort treatment is actively used. It is important for the patient to provide psycho-emotional peace and avoid stressful situations.
Sources:
- Peptic ulcer disease. Clinical recommendations of the Ministry of Health of the Russian Federation, 2021.
- Clinical guidelines of the Russian Gastroenterological Association for the diagnosis and treatment of peptic ulcers, 2016
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Symptoms
Pain in the upper abdomen. They are located slightly below the sternum. This symptom occurs in almost all patients. It usually appears during hunger and stops after eating. The pain syndrome can be characterized as severe, piercing or aching. The pain often radiates to the heart or back. Up to 80% of patients with duodenal ulcers experience nighttime abdominal pain.
Other symptoms
- Nausea.
- Flatulence.
- Belching.
- Bloating.
- Vomiting blood (a sign of an advanced ulcer).
Often the disease does not manifest itself in any way, which indicates its hidden course. This is most common in older people.
General information
About 10% of the population worldwide is affected by peptic ulcers, with men 2 times more likely than women. Medical statistics show that in the duodenum, compared to the stomach, ulcers form 4 times more often. Ulcers found in both the duodenum and stomach are called combined.
Pain and dyspeptic syndromes are the main manifestations of peptic ulcer disease. Up to 75% of patients experience pain in the upper half of the abdomen, manifestations of pain of minor intensity - in approximately 50% of patients, and severe pain - in about a third of patients.
Diagnostics
Endoscopy. The most common and reliable method of diagnosis is endoscopy. The procedure is quite unpleasant for the patient, but it allows the doctor to get a complete picture of the condition of the patient’s internal organs.
Tests. Special testing methods are used to determine the presence of Helicobacter Pylori bacteria. They involve the examination of blood, vomit and feces, as well as material obtained from a biopsy.
X-ray. An important role in the diagnosis of duodenal ulcers is played by x-ray examination, which allows you to complete the picture of the disease.
Palpation. Palpation of the corresponding areas of the abdomen is one of the main methods for diagnosing ulcers.
Publications in the media
Localization • Most duodenal ulcers are located in its initial part (in the bulb). Approximately 5% of ulcers are located postbulbar. The frequency of ulcers is the same on both the anterior and posterior walls.
Clinical manifestations • Pain is the predominant symptom in 75% of patients. Pain occurs 1.5–3 hours after eating (late), on an empty stomach (hungry) and at night (night). Subjectively, pain is perceived as a burning sensation in the epigastric region. Eating improves the condition (“seized pain”) • Vomiting at the height of pain brings relief (reduction of pain) • Vague dyspeptic complaints - belching, heartburn (early and most common manifestation), bloating, food intolerance • Frequent constipation • Pain is determined by palpation in the epigastric region, sometimes some resistance of the abdominal muscles • Asthenovegetative syndrome • Characterized by periods of remission and exacerbation, the latter lasting several weeks. There is a seasonality of the disease (spring and autumn).
Laboratory tests • Analysis of peripheral blood in uncomplicated cases - unchanged • Analysis of feces for occult blood - Gregersen's reaction. A positive reaction can serve as one of the indirect signs of exacerbation of the process • The level of serum gastrin should be determined in patients with recurrent ulcers, in case of failure of conservative treatment and in cases of suspected endocrine disorders (for example, Zollinger-Ellison syndrome). The normal level of serum gastrin is less than 200 pg/ml.
Special studies
• Detection of H. pylori - see Chronic gastritis.
• Study of gastric secretion - increasing the pH of gastric juice on an empty stomach, with the use of specific irritants (cabbage broth, histamine), increasing the content of pepsin (1.5-2 times compared to the norm).
• X-ray examination with barium suspension; for greater accuracy, use the double contrast method - barium suspension + air •• Direct signs ••• "niche" symptom with radial convergence of folds ••• It is necessary to note the duration of evacuation of barium suspension from the stomach to determine the degree of stenosis (up to 6 hours, 6– 24 hours, more than 24 hours) ••• Typical deformation of the bulb - may complicate the interpretation of radiographs during the period of relapse of the disease •• Indirect signs ••• Pyloric spasm ••• Dyskinesia of the duodenal bulb ••• Jaggedness of the contours of the mucous membrane of the bulb ••• Hypersecretion stomach • Endoscopic examination is the most reliable method for diagnosing peptic ulcer disease; indicated for patients with a typical clinical picture, when fluoroscopy does not reveal a duodenal ulcer (accuracy >95%); allows you to detect a picture of type B gastritis, which often accompanies this type of ulcer • Ultrasound allows you to determine the fluid in the stomach cavity, differentiate the disease from chronic cholecystitis and cholelithiasis.
Concomitant pathology • Familial polyendocrine adenomatosis type I (SPEA I) is often accompanied by the development of gastrin-secreting tumors with the formation of ulcers • Liver cirrhosis and chronic renal failure are often complicated by duodenal ulcers • Zollinger-Ellison syndrome • Lesions of the gastrointestinal tract - chronic cholecystitis (25.6%), reactive pancreatitis, etc.
ICD-10. K26 Duodenal ulcer.
Treatment
Treatment of duodenal ulcers is determined comprehensively depending on the general condition of the patient, the results of laboratory tests and a number of other conditions. It should be noted that the surgical method, which was popular earlier, is now used less frequently, only in cases of bleeding or perforated ulcers. Pharmacological therapy consists of destroying the Helicobacter Pylori bacterium, restoring the mucous membrane of the affected organ and preventing complications caused by the ulcer.
To make an appointment at the ABC-Medicine clinic for the diagnosis and treatment of duodenal ulcers, call +7 (495) 223-38-83.
Causes of duodenal ulcer
Duodenal ulcers are usually caused by a person becoming infected with the bacterium Helicobacter Pylori. In addition to the bacterial form of the disease, an ulcer can develop due to increased acidity. Acid causes transformation of the duodenal mucosa, violating its integrity. In any case, for diagnosis it is necessary to undergo FGS with a biopsy in order to get an accurate answer about the reasons for the development of the ulcer.
Also, ulcerative processes can begin with regular use of non-steroidal anti-inflammatory drugs (for example, aspirin, ibuprofen, diclofenac, etc.). Many people take anti-inflammatory drugs for arthritis, muscle pain, etc. Aspirin is also used to protect against the formation of blood clots in the blood vessels. However, these drugs can sometimes have a destructive effect on the duodenal mucosa.
Smoking, drinking alcohol and poor diet contribute to the development of ulcers. Scientists have also proven that when working night shifts, the risk increases by 50%
Types of stomach ulcers
There are several types of stomach and duodenal ulcers. These include the following varieties:
- Perforated. With this type, a through hole appears in the wall of the organ. A communication is formed between the stomach and the abdominal cavity. Remains of food mixed with acid enter the abdominal cavity. They provoke inflammation in these tissues.
- Stressful. The main reason for its development is activation of the hypothalamus. The body produces adrenocorticotropic hormone. It helps reduce the production of mucus in the stomach and reduce its quality. These substances block the restoration of the mucosa and cause an increase in histamine levels. They provoke a deterioration in the blood supply to the mucous membrane. The acid-peptic balance is disrupted due to increased influence of the vagus nerve.
- Antral. They are detected in young people. It occurs in the stomach at the border with the duodenum. It is manifested by frequent vomiting with a sour taste, heartburn, paroxysmal pain, heaviness in the abdomen.
- Cardiac. This disease is rarely detected in patients. It causes pain after eating. Worries about a bitter taste in the mouth, frequent belching, a feeling of heaviness in the stomach when the stomach is empty. With this pathology, plaque appears on the tongue, as well as left-sided pleurisy. Most often it is detected in men. Severe forms of the disease are treated only surgically.
- Medicinal. The formation appears during treatment with certain drugs - corticosteroids, salicylates, anti-inflammatory drugs. With long-term use of these medications, ulcers and erosions form. These ulcers cause bleeding and severe pain.
- Chronic. This type of disease occurs with a slow, long-term course. This form is registered in a third of ulcer patients. Its main symptoms include severe heartburn, dyspeptic disorders, nausea and vomiting after eating, heaviness, and severe pain. Seasonal exacerbations are typical for the disease.
- Calleznaya. It often degenerates into stomach cancer and is localized on the lesser curvature. It is open for a long time, there are no signs of scarring. Arises from a chronic ulcer. Its main manifestations are severe pain, nausea and vomiting. It is treated primarily through surgery.
- Peptic. It is located on the lower part of the stomach. Occurs as a postoperative complication. The main role in the formation of the defect is played by Helicobacter infection and treatment with certain drugs. The main symptoms are intense pain that occurs on an empty stomach, nausea, vomiting with blood clots, diarrhea with blood, weight loss, loss of appetite.
- Mirror. The defect forms at the site of existing inflammation, most often in the lower part of the stomach. It deepens under the influence of gastric juice. It captures several layers of the stomach wall at once. With this form, severe pain does not stop for a long time. These injuries are difficult to heal.
- Endocrine. It is formed when there is a sharp increase in gastric secretion, which occurs due to an increased level of gastritis. The lesion has symptoms typical of an ulcer. The defeat appears suddenly and acutely. Difficult to respond to all types of treatment.
Often ulcerative lesions occur against the background of other somatic diseases: cirrhosis, renal failure, hepatitis, pathologies of the pancreas, as well as the cardiovascular system.
Symptoms of a stomach ulcer
The pain syndrome with a stomach ulcer, in contrast to ulcerative lesions of the duodenum, is more intense. Pain from a stomach ulcer occurs and intensifies immediately after eating. It occurs in the upper half of the abdomen. Most often, the pain is localized in the epigastric zone, occasionally radiating to the left hypochondrium.
The patient associates its appearance with food consumption. Usually the pain starts half an hour or an hour after he eats and stops after two hours. This is explained by gastric emptying. Pain occurs with an ulcer due to irritation of the surface of the defect with food. It stops when taking antacids. In addition, the patient is also worried about other symptoms of a stomach ulcer:
- Heartburn. It occurs when gastric contents, which have an acidic environment, reflux into the lower esophagus. It occurs synchronously with the appearance of epigastric pain.
- Nausea and vomiting. They occur at the same time the pain begins. Vomiting relieves the patient.
- Flatulence. The patient experiences bloating and heaviness of the intestines due to insufficient processing of food with enzymes.
- Signs of high acidity. The patient experiences sour belching and constipation.
A patient with an acute ulcer experiences a sharp decrease in body weight. This is due to the fear of eating, which precedes the onset of pain.