Author
: Grachev Ilya Illarionovich
Editor
: Efremov Mikhail Mikhailovich
Date of publication: 05.13.2014 Date of update: 12.11.2020
Muscle pain, which can either intensify during movements or touches, or torment a person constantly, even at rest, is a reason to think about your health. Myalgia is the name of this common disease, and both older people and children suffer from it.
A large number of people around the world suffer from this disease, which negatively affects the quality of life, disrupting their usual routine. Myalgia is a disease that requires accuracy in diagnosis and correct, individual treatment. It has many manifestations and a variety of factors can trigger its development.
Myalgia does not go away on its own and has serious complications, so you should not delay treatment.
See how easily the disease can be cured in 10-12 sessions.
Causes of myalgia
It is very difficult to list all the causes of myalgia: the very lifestyle of a modern person is a negative factor that increases the chances of contracting this disease. The most common reasons include:
- Stress, prolonged emotional tension.
- Excessive physical activity overstrains the muscles, as a result of which myalgia develops, and a complete lack of exercise can also cause the disease.
- Infectious diseases such as influenza virus and ARVI. Spinal diseases, arthritis, radiculitis.
Exercise stress
“Body aches” after physical activity can occur both in untrained people and in professional athletes8. And the cause of discomfort is the accumulation of under-oxidized metabolic products in muscle cells; in particular, painful sensations are caused by an excessive amount of lactic acid (lactate)2. Less commonly, the cause is microtrauma, but this can only occur if the training rules are violated8.
Muscle soreness due to overwork does not occur immediately, but after a few hours or within 1-2 days after training or unusual physical activity and disappears within a week8.
Symptoms of myalgia
Basically, the symptoms of myalgia manifest themselves in the form of pain, and the pain can be of a different nature and concentrated in different areas. But not only the presence of pain indicates an illness. This disease is characterized by a number of other symptoms:
- Pain in muscles, joints, ligaments.
- Heaviness in the limbs.
- Hypertension, headaches.
- Dizziness, weakness, nausea and even vomiting.
What is POSSIBLE for diseases of the spine
What NOT to do for spinal diseases
List of sources
- Shostak N. A., Pravdyuk N. G., Novikov I. V., . Trofimov E. S. Myalgia in therapeutic practice – approaches to differential diagnosis, treatment // Attending physician. No. 3 p. 21-24.
- Ivanichev G.A. Pathogenetic aspects of the formation and manifestation of classical muscle pain syndromes. Manual therapy. 2009; 3 (35): 3–12.
- Busheneva S.N., Kadykov A.S., Piradov M.A. Myofascial syndrome: from theory to practice. Russian medical journal. 2005; 22. p. 57-62.
- Godzenko A.A., Badokin V.V. Local therapy of myofascial pain syndrome. RMJ. Rheumatology. 2007; 26: 1998–2003.
- Osipova N. A., Abuzarova G. R., Petrova V. V. Principles of using analgesics for acute and chronic pain. Clinical recommendations. M.: FSBI “MNIOI im. P. A. Herzen” Ministry of Health and Social Development of Russia, 2010. 67 p.
Treatment methods for myalgia
In our clinic, myalgia is treated using techniques that have stood the test of time for centuries. The wisdom of oriental healers and the achievements of modern medicine - this symbiosis allows you to comprehensively and effectively influence the existing problem, completely solving it. We offer the following treatment methods:
- Acupuncture. Using special needles, the impact on specific areas of the body allows you to quickly relieve muscle spasms and quickly relieve pain.
- Massage. Honey, acupressure or general massage allows you to quickly relax tense muscles and have a general relaxing effect on the entire body, due to which myalgia recedes. Pinched nerves are released, and metabolic processes improve.
- Hirudotherapy. The essence of the procedure is to stimulate bioactive points of the body through the bite of a medicinal leech. This method allows you to achieve an incredible reflex effect, since leeches not only mechanically affect the body, but also biologically.
- Stone therapy. The method is based on the healing power of heat; this heat not only relaxes overstrained muscles, but also has a positive effect on the blood circulation process, improving tissue nutrition and promoting their recovery.
- PRP therapy is the newest way to stimulate recovery processes. It is used to restore the functions of various organs after diseases and injuries, including to restore the function of the musculoskeletal system in case of myalgia.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating Myalgia
Treatment of myalgia at the Paramita clinic
The main advantage of our clinic is accurate diagnosis. The examination is carried out to identify muscle tension. Attention is paid to the patient's symptoms and history. Thanks to a careful examination, effective treatment for myalgia is prescribed. After the first sessions, patients note that the pain gradually recedes and how much their overall health improves.
An individual approach, gentle but effective methods of influencing the problem and professionalism - these are the conditions due to which a quick and long-term result is achieved: myalgia recedes, and health problems cease to remind of themselves for a very long time!
Sign up for a free initial appointment
Classification
The classification is based on various criteria, according to which the following are distinguished:
- According to pathological changes in the muscular-ligamentous apparatus: fibromyalgia (primary/secondary), myositis (polymyositis), epidemic myalgia .
- According to the nature of the course: acute, chronic.
- According to the location of pain: localized, diffuse.
- According to the level of the CPK enzyme (creatine phosphokinase) in the blood: with an increase in CPK activity and without a change in the level of CPK.
Stages of the disease
- Sometimes the disease is preceded by a feeling of malaise and weakness.
- The pain may gradually increase or, conversely, suddenly manifest itself.
- A “myopathic syndrome” appears when climbing (from a sitting position, up stairs) and the pain intensifies.
- There is a feeling of stiffness and limited body mobility.
- There is a feeling of constant tension.
- If the cause of the disease is serious enough, the next stage may be pain in the joints and bones.
- Possible fever and chills.
Injuries
Severe pain can occur when muscle fibers and tendons are torn. This usually happens if the load is excessive and the muscles are not prepared for it1. But they can also be damaged by sudden movements3. Unlike “ache” due to muscle overwork, pain due to injury occurs immediately, at the peak of the load3.
It should be remembered that even a small, but untreated injury can cause an even more severe sprain3. Therefore, if you experience pain during physical activity, be sure to consult a doctor to rule out a serious injury.
to come back to the beginning
Diagnosis of myalgia
Many people do not attach importance to muscle pain, considering it a consequence of fatigue. But it should be understood that all processes in the human body are closely connected; damage to one of the systems can unpredictably affect the other. Therefore, it is better to use modern diagnostic methods:
- collecting the patient's medical history;
- Ultrasound of superficial muscles;
- MRI for muscle groups located deep in the body;
- taking samples for infections;
- Needle electroneuromyography is performed to assess muscle activity.
Muscle fatigue
In our technological age, many people are gradually forming a new “bad habit”. Spending most of the day in front of a computer screen or holding mobile gadgets in our hands, we may not even notice that we are sitting in a completely uncomfortable and unnatural position. It especially affects the muscles of the shoulder girdle, neck, back and right arm, which is constantly on the computer mouse of office workers1. Staying in one position for a long time or using stereotyped movements can lead to overstrain of the muscles involved, which we feel as soreness1.
TYPES OF MUSCLE DISEASES
Muscle diseases are divided into groups that have a similar occurrence, characteristic manifestations, course and treatment methods.
Diseases include:
- myasthenia gravis – muscle weakness due to autoimmune processes;
- myalgia – pain in muscle tissue due to cell spasm;
- myositis - inflammatory processes that occur against the background of infections, parasites, and other causes);
- Rhabdomyolysis is a serious disease that develops due to the destruction of skeletal muscle and the release of myoglobin (protein) into the blood.
Diseases of the spine and joints
Muscles react to disruption of the joints4 and vertebrae5 associated with them. Therefore, myalgia is one of the symptoms of diseases of the spine5,11 and joints of the limbs4. For example, with osteochondrosis or scoliosis (curvature of the spine), pain in the neck, chest or lower back is associated with overstrain of the paravertebral muscles5,11. And in advanced cases, when the vertebra compresses the nerve root emerging from the spinal cord, the pain can “radiate” to the arm or leg11.
Often myalgia with osteochondrosis is combined with a feeling of numbness or “crawling goosebumps”. At the moment of acute pain, a person freezes, taking a forced position11.
POLYMYALGIA RHEUMATIC
Polymyalgia rheumatica should be considered one of the difficult diagnoses. As a rule, this disease is not detected in a timely manner. Before polymyalgia rheumatica is recognized, patients are misdiagnosed for several weeks, and often years, because the main manifestation of the disease is pain.
Polymyalgia rheumatica is a systemic inflammatory disease of older people, characterized by pain and stiffness in the muscles of the shoulder and/or pelvic girdle.
Introduction
The history of the description of polymyalgia rheumatica dates back to 1957. Barber described 12 cases of this disease and proposed the term “polymyalgia rheumatica”. However, even in the literature of the 19th century one can find individual publications with clinical examples of this disease. In our country, the priority for describing polymyalgia rheumatica belongs to M. Astapenko, E. Agababova, S. Sidelnikova in 1976. The first case of temporal arteritis (without polymyalgia rheumatica) was described back in 1890 in England. Temporal arteritis, closely associated with polymyalgia rheumatica, was described in 1932 by B. T. Horton et al.
The epidemiology of polymyalgia rheumatica has only begun to be studied in the last 20-30 years. Thus, in the USA, only representatives of the white race aged 50 years and older become ill with a frequency of 53.7 per 100 thousand; in Sweden - 28.6 per 100 thousand; in Norway - 32.8 per 100 thousand, and in the Scandinavian countries the prevalence of temporal arteritis is noted, more than in other European countries and in the USA. Polymyalgia rheumatica also occurs in southern countries, for example, in Italy and Spain, and temporal arteritis, which was previously rare in these countries, has become significantly more common in recent years.
It is now generally accepted that polymyalgia rheumatica cannot be classified as a rare pathology. In the world, its frequency ranges from 28.6 to 133 per 100 thousand population over 50 years of age, with an age peak of 65-75 years. Polymyalgia rheumatica begins only in old age. It rarely affects younger people (45-49 years old). Temporal arteritis also occurs in young people. It is noteworthy that polymyalgia rheumatica develops almost exclusively in physically strong people without serious somatic disorders and is 2-3 times more likely in women than in men. The prevalence of temporal arteritis is currently 200 per 100 thousand people over 50 years of age.
Etiology
The etiology of the disease is unknown. The role of a viral or bacterial infection is suspected. An unsuccessful search for the infectious principle was carried out: the level of antibodies to various viruses was studied, but the search for antibodies did not lead to positive results. However, the disease is believed to be caused by certain types of pneumococcus and parvovirus infection. In Sweden in 1994, after an epidemic outbreak of parvovirus infection, there was a high increase in the incidence of polymyalgia rheumatica for 12 months after the epidemic. Viruses are known to promote an inflammatory response with giant cells similar to those found in temporal arteritis. In 40% of cases of arteritis, parainfluenza virus type 1 was detected in patients. In addition, with temporal arteritis, Chlamydia pneumoniae was found in the vascular wall of many patients, which made it possible to regard them as the causative agent of the disease. Stressful situations and hypothermia may play a role. Cases of polymyalgia rheumatica following influenza vaccination have been described. In recent years, great importance has been attached to the environmental factor. A hereditary predisposition to this disease has been proven.
Pathogenesis
The pathogenesis of polymyalgia rheumatica also remains a mystery. The involvement of the immune system is undoubted, although no persistent defects in the immune response or specific antibodies have been identified.
The pathomorphology of polymyalgia rheumatica is characterized by the absence of multiple organs, in contrast to other diffuse connective tissue diseases. With this systemic inflammatory disease of connective tissue, the connective tissue structures of only the periarticular tissues and synovial membrane are affected: muscle tendons at the points of attachment to the bones, joint capsule, connective tissue layers of muscles, fascia, etc. The development of bursitis is mandatory.
A biopsy of painful muscles usually does not reveal any significant changes; A biopsy of the inflamed joint reveals histological signs of mild nonspecific synovitis and changes (edema, focal accumulations of lymphocytes) in the connective tissue periarticular structures. It is believed that the symptoms of polymyalgia are caused by arteritis. The peculiarity of arteritis lies in the fact that giant multinucleated cells are observed in the granulation tissue of inflamed arteries. Giant cell arteritis mainly affects the wall of the aorta and its branches, especially the large branches of the carotid artery and temporal arteries.
Clinic
The disease develops acutely. Often, patients can name the day and hour when intense pain in the muscles of a jerking, cutting, pulling nature suddenly and for no apparent reason appears. At the height of the disease, the localization and nature of pain are stereotypical: the area of the shoulder girdle, neck, pelvic girdle. In 100% of cases, the lesions are symmetrical, although at the very beginning the lesion may be one-sided. At the same time, pain is observed in at least two of these three areas. Constant pain of a cutting, pulling, tearing nature sharply intensifies with movement. Morning stiffness is typical. In addition, a feeling of stiffness appears after any period of immobility.
The intensity of pain is clearly related to the activity of the disease. Because of the pain, movements are limited: it is difficult for patients to stand up, sit down, raise their arms, put them behind their backs, it is impossible to enter a vehicle without help, etc. It is important to observe how the patient gets out of bed: first slowly, wincing in pain, turns on his side, pulls his legs to his stomach, lowers them from the bed, leaning on his hands, sits down with difficulty, and only then, also with the help of his hands, gets up. Pain can also occur in other areas of the musculoskeletal system (hips, legs, buttocks, back, even forearms), but not as naturally. With rest, the pain usually subsides, although in 25-30% of cases it persists. I often experience night pain, which intensifies under the influence of body weight and pressure. Because of this, sleep becomes intermittent and rest is disrupted.
The symptoms of the disease gradually increase and reach a peak after 2-6 weeks, while objective changes are small. When palpating the muscles, there is little or no pain. There are no atrophies or infiltrations in the muscles of the shoulder and pelvic girdle. When palpating the periarticular tissues of the shoulder joint in the area of the greater tubercle of the head of the humerus or in the area of the acromial clavicular joints, the tendon-ligamentous apparatus and muscles are painful. Although patients complain of great weakness, skeletal muscle strength is preserved.
The general condition of the patients worsens. Appetite decreases, weight loss appears. Persistent low-grade fever is possible. Depression often occurs, especially if the patient does not find understanding in the doctor, and the prescribed therapy does not bring relief.
Arthritis in polymyalgia rheumatica usually appears several months after the onset of muscle pain: it is a remitting seronegative symmetrical synovitis with slight swelling - a sign of exacerbation of polymyalgia rheumatica. Very rarely, pain in the hands, synovitis, inflammation of the ligaments of the hands, tendovaginitis, etc. manifest the disease (the so-called distal musculoskeletal manifestation of polymyalgia rheumatica). The following features of articular syndrome can be noted:
- a small number of affected joints in one patient;
- mild signs of local inflammation;
- rapid subsidence of arthritis during treatment with prednisone;
- absence of radiological changes in the joints.
In many cases, patients, preoccupied with muscle pain, do not notice arthritis, and changes in the joints are revealed only upon careful examination: swelling of the joints, tenderness on palpation and pain with passive movements are visible. The process can be either bilateral or unilateral. It may be impossible to determine how old arthritis is. Arthritis may develop before glucocorticoid therapy or during a forced reduction in the dose of prednisolone. The most common localization of arthritis is the wrist, knee, shoulder, and hand joints. Exudative processes occur in the knee joints: with puncture it is sometimes possible to obtain up to 150 ml of synovial fluid, the changes of which are of a moderately inflammatory nature: neutrophil leukocytes up to 15,000 per 1 mm3, decreased viscosity. Over time, contracture may develop in the shoulder joint involving the capsule, which leads to limitation of active and passive movements and muscle atrophy. Arthritis of the wrist joints can be accompanied by unilateral or bilateral carpal tunnel syndrome, the manifestation of which can be paresthesia, chilliness and numbness of the 1st-4th fingers, worse at night, with stress and provocative tests, for example, compression of the carpal tunnel area, diffuse painless swelling of the hands is possible. In addition, with polymyalgia rheumatica, unilateral or bilateral palmar aponeurositis, tenosynovitis of the flexor tendons of the fingers often develop, and slight flexion contractures of the fingers are observed.
Temporal arteritis can occur simultaneously with polymyalgia rheumatica, but can precede it or (more often!) join much later. Polymyalgia rheumatica in many cases occurs without arteritis, but patients always represent a risk group, since it is impossible to predict whether arteritis will complicate polymyalgia and when this will happen. Sometimes it occurs even during prednisone therapy. In 50% of cases, temporal arteritis occurs in isolation without polymyalgia rheumatica. There may be a latent course of arteritis, which is detected by biopsy of the temporal or other arteries. In such cases, it is impossible to determine its duration. As a rule, the process is bilateral, but unilateral damage to the arteries of the head and neck also occurs. Temporal arteritis is accompanied by an increase in temperature to febrile levels (temperature suppositories are not typical for polymyalgia rheumatica, if there is no arteritis!). Headaches appear mainly in the temporal areas, less often in the forehead. Headache may be the first symptom of the disease. Characterized by intense night and morning cephalgia. On palpation, pain in the vascular wall is possible; the arteries are tortuous, their walls are compacted. Syncope may occur, which is usually mistakenly interpreted as epileptiform syndrome due to cerebrovascular disease in the elderly. Soreness of the scalp, hyperesthesia, hair loss, pain in the tongue, difficulty and pain when speaking, chewing and swallowing appear. Patients may complain of decreased vision. Sometimes blindness develops suddenly.
The localization of affected vessels is not limited to temporal arteritis. The facial, orbital arteries, vessels of the neck, upper and rarely lower extremities may be affected; there is a tendency to involve the aorta and its large branches (as in Takayasu's disease). In the vast majority of patients, arteritis occurs in three or more arteries. On palpation along the affected large arterial trunks, pain and hardening, weakening and asymmetry of the pulse are noted. This is especially true for temporal arteritis. Patients with temporal arteritis tend to be primarily ophthalmology patients because of the presence of ischemic optic neuropathy, or neuroretinitis, and decreased vision. Possible pain in the eyeballs, paresis of the eye muscles, strabismus, ptosis of the eyelids, diplopia. It is important to note once again that temporal arteritis also occurs in young people.
When the aorta and large arteries are damaged, systolic murmurs appear, and asymmetry of blood pressure in the peripheral arteries of the extremities is possible. It should be emphasized that changes in the arteries of internal organs are rare. In many cases, arteritis affects the pain syndrome; due to ischemia, the localization of pain expands: it spreads to the back, chest, and limbs.
Fever in different patients can be febrile, subfebrile, and polymyalgia rheumatica can occur without fever. In some patients, prolonged fever (weeks or even months) may be the main or only manifestation of the disease, especially when it begins with temporal arteritis.
Variants of the course of polymyalgia rheumatica:
-classical, when polymyalgia is combined with arthritis and temporal arteritis;
-isolated, that is, without temporal arteritis and without joint damage;
-steroid-independent, in which all typical clinical manifestations of the disease are relieved by NSAIDs;
- torpid, when a standard dose of prednisolone does not lead to complete elimination of myalgia, although it noticeably reduces their severity; increasing the dose of the drug to 25 mg gives a positive, but incomplete effect;
- the “silent” variant is characterized by the absence of myalgic syndrome and is manifested by asthenia, depression, and laboratory findings.
Diagnostics
Clinical signs of polymyalgia rheumatica (pain syndrome) are very important for diagnosis, but you cannot focus only on the clinic: gross diagnostic errors are possible! Also, temporal arteritis is often untimely diagnosed: the course of vasculitis is often asymptomatic, hidden, so that it is revealed only with targeted questioning and examination. The most characteristic sign of the disease is a sharp and persistent acceleration of ESR: 50-70 mm/hour and above. This is not only an important diagnostic sign: it is the dynamics of ESR that should be focused on when carrying out treatment. Other laboratory criteria of inflammation are also revealed: CRP, high fibrinogen, acute phase proteins (β2-, β-globulins) increase, as well as the level of sialic acids and seromucoid. The content of hemoglobin and red blood cells in the blood may decrease.
Back in 1972, V. Hamrin proposed diagnostic criteria for polymyalgia rheumatica:
1. The patient’s age is over 50 years;
2. The presence of muscle pain in at least two of three areas (neck, shoulder and pelvic girdle);
3. Bilateral localization of pain;
4. The predominance of the specified localization of pain during the active phase of the disease;
5. ESR more than 35 mm/hour;
6. The duration of symptoms of the disease is at least 2 months;
7. Limitation of movements in the cervical spine, shoulder and hip joints;
8. General weakness, increased fatigue, anorexia, weight loss, fever, anemia.
The first 5 criteria are considered mandatory, the rest are optional. Recently, the criteria are presented in the form of the acronym SECRET:
- S - Stiffniss and pain - stiffness and pain;
— E — Elderly individuals — elderly patients;
— C — Constitutional symptoms — general constitutional symptoms;
- R - Arthritis (rheumatism) - arthritis;
— E — Elevated erythrocyte sedimentation rate (ESR) — increased ESR;
- T - Temporal arteritis - temporal arteritis.
Constitutional symptoms mean not only the occurrence of the disease in people of the white race, but more frequent than in the population belonging to the HLA DR4 genotype. It is no coincidence that cases of the disease occurring in elderly patients with type 1 diabetes have been described, by the way, with satisfactory compensation of carbohydrate metabolism. While working in endocrinology, we have recently encountered such patients, and in all of them the symptoms of polymyalgia rheumatica were interpreted as a manifestation of diabetic sensory polyneuropathy, the disease was detected late (in some cases after many years), and treatment with prednisolone in all patients without exception caused a labile course of diabetes. Polymyalgia rheumatica can also be combined with type 2 diabetes mellitus (due to its high frequency in the elderly). All manifestations of a systemic disease are usually also regarded as complications of diabetes, so the diagnosis is not made in a timely manner.
Despite the clear signs of the disease, the diagnosis of polymyalgia rheumatica remains difficult. To diagnose it, additional examination is required: checking rheumatoid factor, LE cells, CK levels, AST, alkaline phosphatase, calcium, phosphorus, uric acid in the blood, creatinuria, electromyography, radiography of joints, biopsy of muscles and/or temporal and other arteries, color duplex scanning of large vessels, and often a full oncological examination, in particular, to exclude multiple myeloma (a sternal puncture has to be performed).
When biopsy of the temporal arteries, the diagnosis is based on giant cell granulomatous inflammation. However, the diagnosis of temporal arteritis cannot be removed if giant cells are not found in the biopsy specimen; it is important to evaluate perivascular signs of inflammation. In recent years, cerebral angiography has become widely used, which gives a complete picture of which arteries are affected, the degree of their obliteration, the risk of blindness, stroke and other vascular complications.
An important role is played by MRI and ultrasound to identify bursitis of the subacromeal, subdeltoid, in the area of the iliopsoas muscle, tenosynovitis of the biceps muscles (very often!): these are new diagnostic criteria for polymyalgia rheumatica, allowing diagnosis in patients with polymyalgia rheumatica with normal ESR.
Examination of synovial fluid in the presence of arthritis shows inflammatory changes; The culture results and the presence of crystals in this disease are negative.
Features of the immune status in polymyalgia rheumatica are characterized by a persistent decrease in the absolute and relative number of CD8+ lymphocytes (suppressor-cytotoxic T-lymphocytes) in the absence of signs of hyperactivity of the B-cell component of immunity, frequent detection of markers of damage to the vascular wall (Von Willibrand factor, antibodies to cardiolipin). Assessing the circulation of CD8+ lymphocytes is not only a diagnostic criterion for polymyalgia rheumatica, but also a criterion for the effectiveness of treatment. No specific antibodies have been detected for this disease. An increase in plasma von Willibrand factor persists even during corticosteroid therapy and contributes to sudden vascular accidents.
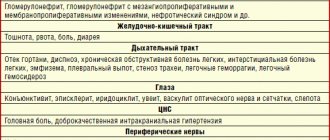
Differential diagnosis of polymyalgia rheumatica is carried out primarily with tumor processes of various localizations. (see table)
Table. Differential diagnosis of polymyalgia rheumatica
| Disease | Similarity of features | Main differences from polymyalgia rheumatica |
| Bilateral glenohumeral periarthritis | Pain in the shoulder girdle and painful restrictions of movement | No increase in ESR, no effect of prednisolone |
| Rheumatoid arthritis | Often in the elderly, the shoulder joints are affected, widespread myalgia and fever occur. | Polyarticularity, early involvement of small joints of the hands and feet, persistent inflammation; presence of RF, x-ray changes in the joints of the hands and feet; prednisolone in a daily dose of 10-15 mg does not lead to remission |
| Polymyositis | Myalgia and weakness mainly in the muscles of the shoulder and pelvic girdle | Muscle weakness rather than pain predominates; characteristic electromyographic changes are always detected; CK, AST are increased. Typical muscle pathology on biopsy. Prednisolone in small doses without effect. |
| Polyarteritis nodosa | Damage to large arteries, muscle pain syndrome | Hypertension, often malignant; renal syndrome such as glomerulonephritis; asymmetric peripheral neuritis; abdominal pain syndrome |
| Oncological diseases | Paraneoplastic process in the form of polymyalgia rheumatica | Treatment with prednisolone for 2-3 weeks without effect |
| Myeloma | Increased ESR | No effect from 10-15 mg of prednisolone per day |
| Nonspecific ulcerative colitis | Fever, arthritis, increased ESR, asthenia, weight loss | Diarrhea with blood |
In some cases, with high fever, polymyalgia rheumatica must be differentiated from sepsis or tuberculosis; for articular syndrome - with brucellosis, toxoplasmosis, arthritis of the jaw joint, maxillofacial neuralgia.
The most common diagnostic errors
Sharply disturbed health, weight loss, lack of appetite, a significant increase in ESR, high temperature, and objective changes are small - all this makes one suspect a tumor process of various localizations, and often the oncological search is delayed, accompanied by numerous, sometimes burdensome for the patient, studies (FGS, sigmoidoscopy, colonoscopy, CTG of the abdominal organs, etc.). The absence of changes in internal organs with persistent, often increasing symptoms negatively affects the patient’s psyche and his relationship with the doctor. It is often necessary to resort to ex juvantibus prednisolone therapy for diagnostic purposes: if there is no effect from glucocorticoids, then it is necessary to look for another disease.
Treatment
Polymyalgia rheumatica is treated with prednisone. Patients “come to life” the very next day after taking small doses of prednisolone, and after 2-4 weeks clinical and laboratory remission of the disease occurs. The standard dose of prednisolone is 15 mg/day, and it should be distributed evenly over 5 mg 3 times a day. An alternative regimen (taken every other day) is not suitable for the treatment of this disease (no effect). The prescription of prednisolone is mandatory and should be carried out immediately upon diagnosis, which will reduce the risk of temporal arteritis. In the presence of temporal arteritis, significantly larger doses of corticosteroids are required. Other drugs are not needed, except those that prevent complications of glucocorticoid therapy - hypokalemia, osteoporosis, arterial hypertension, steroid gastric ulcers, steroid myopathy, diabetes mellitus, cataracts, etc. Calcium supplements and vitamin D3 should be prescribed immediately when planning glucocorticoid therapy. Remission can be achieved after 2-3 weeks, and then the selected dose should be maintained for another month. Achieving remission is the first stage of treatment.
The second stage of treatment - a gradual reduction in the dose of prednisolone - is done very slowly (!), by 1/4 tablets with an interval of approximately 14 days under the control of ESR. The slightest signs of exacerbation of polymyalgia rheumatica force you to return to the previous dose of the hormone, that is, the rate of dose reduction should be individual
(the selection of maintenance therapy for polymyalgia rheumatica with corticosteroids is called an art). Glucocorticoids are also used topically in the form of injections or phonophoresis in the presence of arthritis, or aponeurositis, carpal tunnel syndrome, and in the torpid course of the disease, and the effect is usually positive.
Cancellation of glucocorticoids is possible after an average of a year, rarely after 6 months, if no exacerbations have occurred. However, some patients are forced to take prednisolone for up to 3-10 years. The optimal maintenance dose is 5 mg/day. (complications are minimal). Factors delaying drug withdrawal were studied: female gender, younger age (less than 65 years), refractoriness to the initial dose of prednisolone 10 mg, development of the first exacerbation at a dose of more than 5 mg/day. Patient education plays an important role in the treatment of the disease. Doctors use NSAID treatment more often than they should in order to relieve pain in an elderly patient. However, NSAIDs do not eliminate pain; they can be used only for moderate manifestations of polymyalgia rheumatica and must be combined with prednisone therapy: this allows the use of smaller doses of the latter, which is important for signs of steroid myopathy (weakness appears in the legs when walking, especially up stairs, squatting). In recent years, aminoquinoline drugs such as hydroxychloroquine and methotrexate have been successfully used for the treatment of polymyalgia rheumatica, especially in the presence of contraindications to glucocorticoid therapy and refractoriness to prednisolone. Experience has been gained in the combined use of prednisolone and methotrexate: with smaller doses of both drugs it is possible to achieve stable remission and avoid complications inherent in glucocorticoids and cytostatics.
Therapy of temporal arteritis with glucocorticoids brings significantly less satisfaction than the treatment of polymyalgia rheumatica, is often accompanied by complications and is difficult due to the lack of reliable laboratory or instrumental indicators of vasculitis activity. Glucocorticoids can only eliminate exudative manifestations of inflammation and prevent the development of new vascular lesions. Ischemic changes in the optic nerves cannot be eliminated with prednisolone. The initial dose of prednisolone, according to many experts, should reach 60-80 mg/day, and with damage to large arterial trunks (the prognosis is worse), the dose of glucocorticoids is higher, and its decrease is slower. There has been encouraging experience in the treatment of temporal arteritis and polymyalgia rheumatica with cytostatics and FNOβ inhibitors.
Course and prognosis
In the classic course of the disease, glucocorticoids help suppress the inflammatory process and after 6-12 months, sometimes later, achieve complete recovery. Spontaneous remissions and even recovery from this disease are also known. An undulating course of polymyalgia rheumatica has been described if prednisolone is discontinued as soon as the muscle pain has stopped, or with a forced reduction in the dose of the drug, and the localization of pain changes, new symptoms of the disease appear (arthritis, aponeurositis, etc., including the temporal arteritis, if it did not exist before).
N. Bunchuk and M. Rytikova, who have the largest number of clinical observations of polymyalgia rheumatica, identified in 1991 the torpid course of the disease, in which a standard dose of prednisolone does not lead to the complete elimination of polymyalgia, although their severity may noticeably decrease. The ESR in these patients decreases and even returns to normal, but painful or painless restrictions of movement remain, mainly in the shoulder joints, usually more pronounced on one side. In this case, signs characteristic of an isolated lesion of one or another periarticular structure are determined, more often - simple tendinitis of the supraspinatus muscle or the long head of the biceps brachii muscle. Such patients required large doses of prednisolone (a dose of 25 mg/day is not always sufficient). Injections of glucocorticoids into the area of the affected muscle-tendon structure are necessary. Some patients experience stable remission, while others experience a relapsing course.
With isolated polymyalgia rheumatica (without vasculitis), the prognosis for life is favorable; in the presence of temporal vasculitis, the prognosis is always questionable. When the dose of prednisolone is reduced, relapses of arteritis with the onset of blindness are possible; vasculitis can lead to sudden death due to stenosis and occlusion of the cerebral, coronary arteries, and aortic aneurysm. In some cases, temporal arteritis, although it has a long course, ends in recovery.
Conclusion
Despite the well-studied clinical picture and course of polymyalgia rheumatica, it remains unclear why the disease affects only older people, why the arteries of the head and neck are affected, and not the internal organs, and most importantly, the causes of the disease are still not clear. This means that etiotropic therapy is impossible.
Irina TERESCHENKO,
Professor.
Perm State Medical Academy.
Rhabdomyolysis
With muscle injuries (more common in athletes), gradual destruction of tissue occurs, this condition is called rhabdomyolysis. This process ultimately ends with the death (necrosis) of cells and the release of toxins into the circulatory system. This disease can cause serious complications and lead to kidney failure. If qualified assistance is not provided, it can result in death.
Possible reasons:
1. Bodily injuries (injuries, beatings, accidents, accidents).
2. Stage 3 and 4 burns.
3. Long surgical operations (more than 8–10 hours).
4. Long-term compression of tissues with impaired blood supply.
5. Electric shocks.
The development can be provoked by: increased loads during training, epileptic seizures, severe muscle spasms, delirium tremens.
It is very difficult to recognize the disease; the manifestations are similar to the symptoms of many diseases; sometimes rhabdomyolysis occurs secretly. Often the correct diagnosis can only be made based on the results of a blood test. In an advanced form, the patient may fall into a coma and die.
PREVENTION OF MUSCLE DISEASES
Preventive measures include a number of simple rules:
- avoid hypothermia, wear seasonal clothing;
- carefully follow all doctor’s orders for any disease;
- do not self-medicate;
- practice a healthy lifestyle;
- use regular exercise.
It is best to practice under the guidance of experienced instructors who will select an individual rehabilitation program and help you achieve a quick and high-quality recovery. This is the approach that the specialists at the Center for Restorative Medicine follow. The cost of admission and other details can be found on the Center’s website or by calling.
MYASTHENIAS
A disease of the autoimmune system that causes muscle weakness due to interruptions in neuromuscular transmission is called myasthenia gravis. The activity of the ocular, facial and masticatory muscles is usually impaired; the muscles of the respiratory organs are less commonly affected. Characteristic manifestations: drooping of the lower eyelid, disturbances in vocal function (nasal sound, hoarseness, hoarseness or weakness), disturbances in swallowing and chewing.
The word "myasthenia" means impotence, muscle weakness. This is a pathological process, which is based on the self-destruction of body cells. The normal immune response changes direction and begins to destroy its own cells instead of foreign ones, which leads to the destruction of organs and tissues of the body.
Possible reasons:
- genetic predisposition;
- benign or malignant tumors;
- systemic diseases;
- damage to the nervous system;
- hyperthyroidism, sleeping sickness.