Chronic rhinosinusitis is a common disease in which a long-term inflammatory process of the nasal mucosa continues (12 weeks or more).
Author:
- Galkin Alexey Vladimirovich
ENT pathology expert
3.40 (Votes: 5)
Chronic rhinosinusitis is a common disease in which a long-term inflammatory process of the mucous membrane of the paranasal sinuses continues (12 weeks or more).
Differences between chronic and acute rhinosinusitis
Chronic rhinosinusitis is characterized by a long course and usually occurs without a pronounced increase in temperature. An acute condition is always accompanied by high fever, begins unexpectedly and has more pronounced painful symptoms.
The main symptoms of chronic rhinosinusitis:
- runny nose;
- impaired nasal breathing, feeling of swelling in the nose;
- postnasal drip (accumulation or drainage of mucus in the throat, the need to cough up mucus);
- swelling and swelling of the soft tissues of the cheeks, eyelids, nose, forehead;
- deterioration (absence) of smell and taste.
Also, with chronic inflammation, a cough may appear with radiating (radiating) pain in the ear, upper jaw, and teeth.
Other symptoms of chronic rhinosinusitis:
- otalgia (ear pain);
- pain spreading to the upper jaw and teeth;
- sore throat;
- cough (may get worse at night);
- halitosis (putrid odor);
- fatigue;
- nausea.
Case from practice
Patient P., 15 years old. A course of nasal irrigation (washing) No. 5 and centrotherapy (10 sessions) was carried out as part of a complex treatment (systemic and local antibacterial therapy, antihistamines and vasoconstrictors) for bilateral acute purulent sinusitis. Before this, for several years he suffered from bilateral sinusitis twice a year and ARVI up to 4-5 times a year. Over the next 2.5 years, I only suffered from mild acute respiratory viral infection three times, using only vasoconstrictor drops for a runny nose.
Causes of chronic inflammation
The main reason for the development of chronic inflammation of the maxillary sinuses is a violation of their normal drainage. This occurs due to prolonged infectious or non-infectious edema (allergy, drug-induced edema) in the area of the maxillary nasal anastomosis or impaired mucociliary clearance. Also, the background for the formation of chronic inflammation is anatomical obstacles in the nose that disrupt normal drainage (deviated septum, enlargement of the middle turbinates).
In summary, the main causes of chronic sinusitis are:
- prolonged allergic swelling of the nasal mucosa;
- frequent respiratory infections;
- septal deformation;
- hypertrophy of the middle turbinates;
- prolonged swelling of a non-allergic nature (medicinal rhinitis);
- chronic inflammatory process in the area of the upper teeth (periodontitis, odontogenic cysts);
- foreign bodies (filling material, sinus lift material, tooth roots, etc.);
- neoplasms in the nasal cavity or paranasal sinuses;
- other diseases: cystic fibrosis, gastroesophageal reflux, HIV infection, immunodeficiency conditions.
Clinical observation
Patient T., 18 years old. Complaints of difficulty in nasal breathing, congestion and purulent discharge from the nasal cavity. According to the patient, complaints appeared against the background of ARVI on the 6th day of illness. It is treated with vasoconstrictor drops and antipyretic drugs with a short-term positive effect. During endoscopy of the nasal cavity with a Karl Storz 0 g endoscope (Germany), inflamed and edematous mucosa, viscous mucopurulent discharge in moderate quantities, mainly in the area of the middle nasal passage on the right, were visualized, the nasal septum deviates to the right, in the nasopharynx and oropharynx, discharge of discharge into the oropharynx was noted with symptoms of pharyngitis.
It must be taken into account that endoscopic examination of the nasal cavity is carried out by an otolaryngologist. General practitioners and pediatricians should follow the diagnostic criteria for ARS.
The patient was prescribed complex topical therapy, which included rinsing the nasal cavity with a normalized solution of sea salt, Sinuforte, 1 injection 1 time per day into each half of the nose for 7 days. During the therapy, regression of symptoms and significant positive dynamics were noted when examined after 7 days (Fig. 2).
The patient's recovery occurred with monotherapy, without the use of antibacterial drugs.
Complications of chronic rhinosinusitis
Prolonged inflammation carries many dangers, since the sinuses are close to such important structures as the eyes and brain:
- Meningitis (inflammation of the membranes of the brain and spinal cord);
- Sepsis. Generalized infection;
- Other infectious complications. Sometimes the inflammation spreads to the bones (osteomyelitis) or skin (cellulitis);
- Orbital complications. If the infection enters the eye socket, it can cause decreased vision or permanent blindness.
- Partial (or complete) loss of smell. The difficulty of odorants entering the olfactory cleft and inflammation of the olfactory nerve can lead to temporary or permanent loss of odor perception.
Description
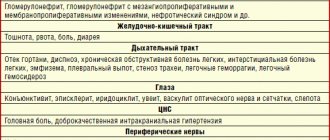
Allergic rhinosinusopathy (or rhinosinusitis) refers to a type of pathological condition. The disease manifests itself in the form of damage to the nasal mucosa and its paranasal sinuses. The development of the disease occurs due to disturbances in reactivity processes (in particular, the immune system). Damage to the nasal mucous membranes is almost never isolated, but additionally affects the skin, larynx, bronchi, lungs and mucous membranes of the eyes.
Rhinosinusopathy is determined by duration:
- episodic acute (inflammation of the nasopharyngeal mucosa goes away quickly when contact with inhaled allergens, as well as animal hair or bird feathers is avoided);
- seasonal (characterized by damage to mucous membranes only during the flowering period of plants);
- year-round or persistent (observed for at least nine months a year).
According to statistics, allergic rhinosinusopathy occurs in 20% of the total world population.
Diagnostics
To identify a chronic form of rhinosinusitis, the doctor will need to interview you, conduct a physical examination, and rhinoscopy (examination using a nasal speculum). But additional research will be required to determine treatment tactics.
Additional diagnostic methods:
- Endoscopy. A flexible, soft tube (endoscope) with fiberoptic light allows the doctor to see your nasal passages, the sinus area, and sometimes the inside of your sinuses.
- X-ray tomography. Images taken by a computed tomography (CT) scanner can show details of your maxillary sinuses and nasal area. The doctor will determine the volume and nature of the sinus lesions and assess the patency of sinus-nasal communications.
- Sowing from the mucous membrane for flora. Allows you to find out the infectious cause (if any) of sinus inflammation (fungi, bacteria) and prescribe the necessary treatment.
- Allergy testing. If your doctor suspects that the condition is caused by an allergy, you will need to undergo allergy testing (rhinocytogram, blood IgE, eosinophil cationic protein).
Establishing diagnosis
If you suspect rhinosinusitis, you should make an appointment with an otolaryngologist and an allergist or immunologist. After collecting a history of the disease, specialists will prescribe the following diagnostic methods:
- tests for allergic reactions;
- rhinoscopy;
- radiography.
The purpose of these research methods is to determine the characteristics of the washing fluid and study it for the presence of pus. In addition, during the diagnosis, the allergen-irritant is identified, the causes of the development of the disease are established (the origin may be bacterial or viral). Studies are also necessary to confirm or exclude vasomotor rhinitis.
Treatment of chronic rhinosinusitis
The goal of treatment is to reduce the number of exacerbations of sinusitis and reduce or disappear the symptoms of the disease. The main therapy is aimed at improving the drainage of the paranasal sinuses, as well as improving the functioning of the local immunity of the mucous membranes. To do this, it is necessary to eliminate the blockage of the sinus-nasal anastomosis, reduce the viscosity of the mucous secretion, and carry out immunotherapy. Sometimes surgery is required to clear the sinuses.
Drug therapy
The first stage of treatment for chronic rhinosinusitis is conservative therapy.
It includes:
- Regular cleansing of the nasal cavity and sinuses with isotonic sodium chloride solution (sterile saline solution).
- Nasal topical corticosteroids. These are nasal sprays that help reduce inflammation and swelling in the area of sinus anastomosis and improve drainage (mometasone, fluticasone, beclomethasone).
- Inhalation administration of a solution of antibiotics, corticosteroids, mucolytics into the sinuses. The use of sinus inhalers (Pari inhalers) allows medications to be administered precisely into the sinuses.
- Systemic administration of corticosteroids gives a strong anti-edematous, anti-inflammatory effect, reduces nasal polyps, improves drainage, but has serious side effects with long-term use of the drugs.
- Local and systemic use of antibacterial and antifungal agents. The use of antimicrobial agents for infectious chronic rhinosinusitis allows one to cope with exacerbation of the disease.
- Immunotherapy - Your allergist-immunologist may add immune-boosting or allergy-regulating medications to your sinusitis treatment.
Surgery
With low effectiveness of conservative therapy, surgical treatment of chronic rhinosinusitis is indicated. It is aimed at eliminating the mechanical obstacle to sinus drainage (enlarged turbinate, deformed nasal septum, anatomical narrowing of the sinus anastomosis area, polyp in the anastomosis area, etc.), as well as cleansing the sinuses of foreign inclusions (fungal bodies, tooth roots, filling material, material for sinus lifting), cysts, polyps.
Endoscopic sinus surgery
For this procedure, the doctor uses an optical system consisting of a thin tube with magnifying lenses and a camera that transfers the image to a screen. Good visualization of the operated area, the ability to change the viewing angle ensures delicate and safe removal of obstacles at the exit from the sinus, and also allows you to clear it of foreign inclusions.
The surgical treatment performed only creates conditions for improving drainage and cleaning, so it is necessary to continue postoperative treatment to achieve a lasting effect.
Laboratory research methods
Bacteriological research
This is a study designed to isolate bacteria and study their properties in order to make a microbiological diagnosis. The material for the study can be obtained from the nasal cavity or from the affected sinus during puncture. When collecting material, there is a high probability of “traveling” microflora entering.
Study of mucociliary transport
Allows you to assess the condition of the mucociliary apparatus of the mucous membrane, that is, to identify one of the most important pathogenetic disorders in rhinosinusitis.
In clinical practice, the measurement of transport time is most widely used. One of the variations of this method is to measure the time during which a marker (charcoal, carmine, ink, foam, etc.) moves from the anterior parts of the nasal cavity to the nasopharynx. Due to its simplicity, the saccharin test has become more widespread.
Its principle is to measure the time it takes a particle to travel a conventional distance - from the anterior parts of the nasal cavity to the taste buds in the pharynx. Saccharin time in healthy people can range from 1 to 20 minutes, averaging 6 minutes. However, these indicators are very conditional.
Prevention
Follow these steps to reduce your risk of chronic rhinosinusitis:
- avoid upper respiratory tract infections;
- reduce contact with people suffering from respiratory diseases (colds, ARVI);
- if cold symptoms persist (7 days or more), do not delay going to the doctor;
- manage your allergies. Work with your doctor to keep your symptoms under control;
- avoid tobacco smoke and polluted air, replace filters in your car on time, and clean the air conditioner in a timely manner;
- humidify the air in the house at low humidity;
- avoid hypothermia.
Centrotherapy in combination with the “Light Breathing” irrigation technique for acute sinusitis
The combination of techniques gives a quick healing effect. As a rule, about 5 sinus lavage procedures and 10 centrotherapy sessions 2-3 times a week are required. Centrotherapy sessions are carried out from the first days of treatment, after the washing procedure, which enhances the therapeutic effect. In some cases, it is possible to shorten the course of antibiotic therapy.
*terminology of the founder of centrotherapy P. Bonnier
See the articles “Protracted runny nose in children and adults”, “Frequent colds in children and adults. Immune problems?
Signs
The first symptoms of allergic rhinosinusopathy are:
- difficulty breathing through the nose;
- periodic profuse mucous-watery discharge from the nose;
- paroxysmal sneezing;
- increased nasal congestion after a sneeze;
- a feeling of heaviness in the paranasal region and bridge of the nose;
- the appearance of a feeling of “heavy head”;
- intensification of this “heavy” feeling when tilting the head down (usually occurs with the development of the chronic form).
In case of infectious damage to the mucous membranes, a transition of infection from the maxillary sinus to the cellular system of the ethmoidal labyrinth is most often observed. A similar factor provokes the development of:
- chills;
- increased body temperature;
- weaknesses;
- sleep disorders;
- decreased appetite;
- irritability;
- frequent unexplained mood swings.
Even with a minimal allergic reaction, foci of negative manifestations can be observed in other tissues:
- bronchopulmonary system (manifested by cough, heavy sputum discharge, feeling of lack of air, possible attack of suffocation);
- on the skin (manifests as urticaria or atopic dermatitis).