Materials and methods
The open prospective study included 98 women (mean age 68±9 years, mean duration of postmenopause 17±4 years) with postmenopausal AP, who were observed on an outpatient basis at the National Medical Research Center for Primary Care. In the anamnesis, a fracture of the proximal femur (PHB) was noted in 4, radius - in 8, compression fractures of the vertebrae - in 27. The median 10-year probability of major fractures according to FRAX in patients who had not previously received therapy was 14.9%, fracture femoral neck (FNC) - 3.7% (Table 1).
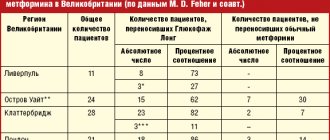
Table 1. Clinical and instrumental characteristics of the examined patients Note. Here and in the table. 2 NPs - those who had not previously taken anti-osteoporotic therapy; P - previously taken anti-osteoporotic therapy.
All patients received denosumab at a dose of 60 mg once every 6 months subcutaneously (in most cases in the abdominal area) for 12 months or more, as well as calcium and vitamin D supplements according to the instructions [12].
Before starting treatment with Prolia, the concentration of vitamin D (25 (OH)D) in the blood serum was measured. In order to increase the effectiveness and safety of therapy, vitamin D saturation was carried out (50,000 IU per week for 4 weeks) followed by a transition to maintenance intake (800-2000 IU/day) depending on the degree of vitamin D deficiency. The daily calcium intake was at least 1000-1200 mg [13].
Inclusion criteria: signed informed consent; duration of postmenopause (after natural or surgical menopause) ≥1 year; diagnosis of AP, according to WHO criteria: BMD ( T
-criterion) of lumbar vertebrae (LI—LIV) and/or PBC or SBC –2.5
SD
and below;
the presence of low-traumatic fractures of the vertebrae, the spinal vertebrae or the radius with a T
-criterion of –1.5
SD
or lower and a high 10-year risk of major fractures according to FRAX.
Exclusion criteria: other metabolic skeletal diseases; hypocalcemia; malignant neoplasms diagnosed within the last 5 years before the start of therapy; taking other drugs for the treatment of AP after inclusion in the study, except for calcium and vitamin D; taking replacement therapy with female sex hormones; inability to perform densitometry of at least two lumbar vertebrae.
Among the patients there were no persons systematically taking glucocorticosteroids. The following concomitant diseases were identified: type 2 diabetes mellitus - in 8, diseases of the gastrointestinal tract - in 20, hypothyroidism, which requires taking levothyroxine less than 100 mcg / day - in 8, hypertension - in 28, various disorders heart rhythm - in 8, coronary heart disease - in 16, kidney disease with a decrease in creatinine clearance to 27 ml/min - in 3, breast cancer and mastectomy more than 5 years before inclusion in the study - in 6; 3 patients were treated with aromatase inhibitors. Diseases such as diabetes mellitus, hypothyroidism with long-term use of replacement therapy, and a history of therapy for breast cancer could determine the mixed nature of AP.
The maximum observation period was 4 years: 48 people received treatment for 12 months, 29 for 24 months, 11 for 36 months, 10 for 48 months.
Adverse events were assessed after the first administration of the drug, then after 6, 12, 24, 36 and 48 months of treatment based on questionnaires given to patients. In addition, the convenience of the scheme and form of drug administration was assessed using a 4-point system: very convenient, fairly convenient, satisfactory, unsatisfactory.
The patients were divided into 2 groups: 1st - 26 people who had previously received treatment with anti-osteoporotic drugs (15 aminoBP, 6 strontium ranelate, 10 active metabolites of vitamin D), and were transferred to denosumab therapy after consultation at the National Medical Research Center for PM due to the ineffectiveness of the drugs or poor tolerability no earlier than 3 months after the end of previous therapy; 2nd - 72 patients who had not received anti-osteoporotic therapy before denosumab was prescribed.
All patients underwent the following studies:
— examination and anthropometric study;
— dual-energy X-ray bone densitometry of the lumbar spine (LI-LIV) in the posteroanterior projection and POBC using Hologic Delpfi W (USA) and Lunar Expert (USA) devices. Dynamic measurements were carried out once a year on the same device. BMD indicators are unified and adjusted to the indicators used in the Hologic database using correction factors;
- laboratory tests: level of total calcium, creatinine, total alkaline phosphatase (TALP), C-terminal telopeptide of type I collagen (CTx, β-CrossCaps) in blood serum;
— survey about the presence of adverse events.
The 10-year probability of major osteoporotic fractures was assessed using the Russian FRAX model and bone resorption marker CTx once in 72 patients of group 2.
Statistical data processing was carried out using Microsoft Excel applications and the statistical data analysis package SPSS 20.0. Conventional methods of parametric and nonparametric analysis were used. Quantitative variables were described by the number of parameters, the arithmetic mean ( M
), standard deviation from the arithmetic mean (
σ
).
Qualitative variables were described in absolute and relative values (in percentages). Differences were considered statistically significant at p
<0.05. When comparing qualitative indicators, statistical analysis methods were used: Pearson's χ2 test, paired and unpaired Student's t-test. For parameters whose distribution differed from normal, nonparametric tests were used: when comparing two groups, paired Spearman correlation analysis was used to determine the two-sided significance of the indicators.
Results and discussion
During treatment with denosumab, a significant increase in BMD was observed in all measured skeletal areas (Fig. 1).
Rice.
1. Dynamics of BMD during treatment with denosumab. Here and in Fig. 2 * — p≤0.001. Thus, the increase in BMD in the lumbar spine after 12 months was 4.2%, after 24 months - 7.5%, after 36 months - 8.8%. In the ShBK there was an increase in BMD by 3.1, 3.9 and 5.3%, and in the entire PBC - by 2.8, 4.1 and 5%, in the forearm (1/3 of the radius) - by 0.9 , 1.4 and 2.6% respectively. The data obtained are consistent with the results of an axial phase III RCT assessing the effectiveness and safety of denosumab FREEDOM therapy. However, it should be noted that this study included women with T
-criterion of –2.5
SD
or less, but not less than –4
SD
, while in our study there were no restrictions and patients with a lower
T
-criterion were included.
Thus, in the first part of the FREEDOM study, which lasted for 3 years, BMD in the spine increased by 8.8%, in the BCD by 5.2%, and in the POB by 6.4% [14, 15]. The increase in radial bone BMD over 3 years of denosumab treatment was 3.5% ( p
≤0.0001) [7]. In addition, forearm BMD was measured in an extension study that included 115 patients in the FREEDOM placebo group who received calcium and vitamin D alone and subsequently switched to denosumab, which they received for 5 years in the FREEDOM extension study. Despite the decrease in BMD during the placebo period, at the end of the study there was an increase in BMD by 1.5%, which was important confirmation of the cessation of cortical bone loss [16]. Currently, denosumab is the only drug that increases BMD in the area of 1/3 of the forearm, indicating a clinically significant effect of the drug on cortical bone.
For a number of chronic non-infectious diseases and risk factors for their development, tactics are used to achieve target values of the studied indicators. For this purpose, biomarkers of the pathological process and their levels that must be achieved to prevent the development of complications have been identified. Thus, for a cerebral stroke, such a marker is the level of blood pressure, and its target level is 140/90 mmHg. [17]. Clinical guidelines for the treatment of AP currently do not identify special markers or define their target values. This is due to the fact that treatment with the most common antiresorptive drugs, BP, did not cause a constant and significant increase in bone mass, especially in the POBC, and the markers of bone turnover were characterized by very high variability. Currently, in the course of 5-, 6- and 10-year studies of FD, it has been shown that BMD increased maximally in the 3-4th year of treatment, and then remained at the same level or tended to decrease. This is probably due to the slowdown in bone mineralization during long-term use of BP, necessitating a temporary break in treatment [18, 19]. However, a meta-analysis of RCTs on the effectiveness and safety of various drugs for the treatment of AP has proven a statistically significant linear relationship between the increase in BMD in the vertebrae and femur and a decrease in the relative risk of fractures at a low level of injury [20]. The emergence of new antiresorptive (denosumab) drugs for the treatment of AP, which caused a continuous and significant increase in bone mass over 10 years, made it possible to consider BMD as a marker for achieving target values, i.e., transition from the “zone” of AP to the “zone” of osteopenia or overcoming the acceptable level of risk of fractures, which is T
-criterion –2.5
SD
.
Among 98 patients, according to the results of spinal densitometry, BMD according to T
-criterion below –2.5
SD
were detected in 79, the median
T
-criterion was –2.8
SD
.
After 12 months of therapy, this indicator increased in 23 (29%) women, and the median T
-score was –2.4
SD
, which corresponds to osteopenia.
In 56 patients, the T
-criterion for the spine area was low before the start of therapy, the median
T
-criterion was –3.4
SD
, and after 12 months of treatment it increased to a value of –2.9
SD
, but did not enter the “zone” of osteopenia. After 24 months, 25 people showed a transition from the “zone” of AP to the “zone” of osteopenia.
When analyzing the dynamics of BMD of the SBK, out of 47 people with identified AP in this skeletal area, 12 moved into the “zone” of osteopenia after 12 months of treatment. In the remaining 35 patients with the lowest BMD before treatment, median T
-criterion was –3.0
SD
, and after 12 months of therapy –2.8
SD
, which was also regarded as positive dynamics.
The study included 11 patients who at the first visit, according to densitometry, had osteopenia, but had a history of low-energy fractures, as well as a high risk of major fractures according to FRAX. Among them, 5 people had previously received anti-osteoporotic therapy and were switched to denosumab treatment. In 6 patients who had not previously received treatment, median T
-criteria before the start of the study was –1.5
SD
, –1.4
SD
, and after a year of therapy this indicator at both points was –1.2
SD
.
Achievement of target BMD was assessed over an 8-year period of treatment with denosumab in the FREEDOM study and concluded that many women with AP achieved non-osteoporotic T
-criteria (from 11 to 82%). Based on the results obtained, the authors called for the use of tactics to achieve target values in the treatment of AP [21].
An assessment of the dynamics of BMD after 12 months of therapy in 26 women who had previously taken anti-osteoporotic therapy showed a similar increase in bone mass as in the group of untreated patients, i.e., an additional positive effect was obtained when switching to denosumab (Table 2).
Table 2. Dynamics of BMD in 72 patients who did not receive and 26 who received anti-osteoporotic therapy before the start of the study. The data obtained confirm the results of studies that showed a more significant increase in BMD when patients were transferred from tablet BP or anabolic therapy with teriparatide to denosumab [22, 23].
A significant decrease in serum CTx concentration was noted 6 months after the start of denosumab therapy by 54% ( p
<0.001) and after 12 months - by 72% (
p
<0.001). Subsequently, when monitoring the CTx concentration once a year for 48 months, this level was maintained. These data are consistent with the results of the FREEDOM studies, in which the reduction in CTx concentrations reached 86 and 72% (after 1 and 36 months, respectively) and DECIDE (74% after 1 year of treatment) [8, 11] (Fig. 2).
Rice.
2. Dynamics of CTx levels during treatment with denosumab. In addition, a decrease in the level of total calcium in the blood was recorded after 6 months by 3.6% and after 12 months by 7.6% ( p
≤0.001). It should be noted that when assessing calcium metabolism before the start of therapy, 12 people showed slight and clinically insignificant hypercalcemia, which was not detected after 12 months of treatment. Subsequently, throughout the entire period of treatment, total calcium levels remained within normal limits. The hypocalcemic effect of denosumab in this case may indicate the manifestation of its pronounced antiresorptive effect. The decrease in the level of TAP in the blood did not reach statistical significance throughout the treatment. This is apparently due to the fact that ALP includes several isoenzymes, in addition to bone, reflecting the rate of bone remodeling. The average creatinine level did not change throughout treatment. In patients with reduced glomerular filtration of the kidneys, there was no increase in creatinine concentration in the blood. Currently, Prolia is the only drug for the treatment of AP approved for use in patients even with severe renal impairment. Due to its unique targeted mechanism of action, Prolia is not excreted in the urine and does not necessitate dose adjustment in chronic kidney disease. Special studies have shown that the degree of renal failure does not affect the pharmacokinetics and pharmacodynamics of the drug, and this provides an advantage to prescribing Prolia in this population [24].
Among the 98 patients who received the first injection of Prolia, no independent refusal to continue treatment was noted. The different number of patients after 24 months or more is associated with the period of analysis of the material, and not with the cessation of therapy, therefore in this article we do not draw conclusions about patients’ compliance with the prescribed treatment regimen.
The adverse events encountered were assessed as mild to moderate in severity. They are mainly associated with the musculoskeletal system: arthralgia was noted in 3 patients, the appearance or intensification of back pain - in 16, pain in the bones of the extremities - in 7. It should be noted that similar pain sensations in these patients were periodically observed before the start of therapy and Upon detailed questioning, women could not with complete confidence associate these manifestations with taking denosumab. In 2 patients, dermatitis was observed at a distance from the injection site 1 and 3 months after the first injection of denosumab, which resolved spontaneously. Both patients did not have a history of allergies and the cause of dermatitis could not be identified. All noted adverse events did not require discontinuation of the drug. During the observation period, 3 patients had fractures: one had a fracture of the radius in a typical place 2 months after the first injection, the second had a fracture of the ankle 3.5 months after the first injection, the third had deformities of 2 vertebrae 46 months after the start. treatment with denosumab. All patients were diagnosed with severe AP with a history of fractures, and new fractures were associated with low bone strength, and not with insufficient effect of the drug.
According to the survey, 86 patients found the drug administration regimen very convenient, 8 – quite convenient, 6 – satisfactory.
Prolia® (Prolia)
Calcium and vitamin D supplements
All patients are recommended to take calcium and vitamin D supplements in adequate doses during therapy with Prolia®.
Precautions for use
Hypocalcemia
It is important to identify patients at risk of developing hypocalcemia. Hypocalcemia should be corrected by taking calcium and vitamin D supplements in adequate doses before starting therapy. It is recommended to monitor calcium concentrations before each dose in patients predisposed to developing hypocalcemia for 2 weeks after the first dose. If symptoms of hypocalcemia develop during the course of therapy (see section “Side effects” for symptoms), it is necessary to evaluate the concentration of calcium in the blood. Patients should be warned to report symptoms suggestive of hypocalcemia.
In post-marketing studies, cases of severe symptomatic hypocalcemia (including death) were observed (see section "Side effects"), which were most often recorded during the first weeks after the start of therapy, but their development is possible at a later date.
Concomitant therapy with glucocorticoids is an additional risk factor for hypocalcemia.
Kidney failure
Patients with severe renal impairment (creatinine clearance <30 ml/min) or receiving dialysis are at increased risk of developing hypocalcemia. The risk of developing hypocalcemia and concomitant increases in parathyroid hormone levels increases with the severity of renal dysfunction. It is especially important for these patients to take calcium and vitamin D supplements in adequate doses, as well as regular monitoring of calcium concentrations in the blood (see above).
Skin infections
Patients receiving Prolia® may develop skin infections (mainly inflammation of the subcutaneous fat) requiring hospitalization (see section “Side Effects”). Patients should be advised to seek immediate medical attention if signs or symptoms of subcutaneous fat inflammation occur.
Osteonecrosis of the jaw (ONJ)
Rare cases of ONJ have been reported in patients receiving Prolia® for the treatment of osteoporosis (see section "Side effects").
It is necessary to delay the initiation of therapy/conducting a new course of therapy in patients with unhealed open injuries to the soft tissues of the oral cavity. Before initiating denosumab therapy in patients with concomitant risk factors, it is necessary to conduct a dental examination and preventive dental measures, as well as an individual assessment of the benefit-risk ratio of denosumab therapy.
When assessing a patient's individual risk of developing ONJ, the following risk factors should be taken into account:
- the activity of the drug that inhibits bone resorption (increased risk for potent drugs), route of administration (increased risk with parenteral administration) and total dose of antiresorptive therapy;
- malignant tumors, concomitant pathologies (for example, anemia, coagulopathies, infections), smoking;
- concomitant therapy (corticosteroids, chemotherapy, angiogenesis inhibitors, radiation therapy to the head and neck area);
- poor oral hygiene, periodontal disease, ill-fitting dentures, a history of dental disease, invasive dental procedures (for example, tooth extractions).
During treatment with denosumab, all patients should maintain good oral hygiene, undergo regular dental examinations, and promptly report any adverse oral symptoms such as tooth mobility, pain, swelling, non-healing mucosal lesions, or discharge. During therapy, invasive dental procedures should only be performed after careful evaluation; It is necessary to avoid performing these procedures immediately before and/or immediately after administration of Prolia®.
A treatment plan for patients with ONJ should be developed in collaboration with the attending physician and a dentist or oral surgeon with experience in treating this pathology. Temporary discontinuation of therapy should be considered until the condition resolves and risk factors are eliminated whenever possible.
Osteonecrosis of the external auditory canal
Cases of osteonecrosis of the external auditory canal have been reported during denosumab therapy. Possible risk factors for this condition include steroid use and chemotherapy, and/or local risk factors such as infection or trauma. The possibility of osteonecrosis of the external auditory canal should be considered in patients taking denosumab who have ear symptoms, including chronic ear infections
Atypical hip fractures
Atypical femur fractures have been reported in patients taking Prolia (see Side Effects section). Atypical femoral fractures may occur with little or no trauma to the subtrochanteric or proximal diaphyseal portion of the femur. On x-rays, these fractures usually have a characteristic appearance. Atypical femoral fractures have also been reported in patients with certain underlying diseases and conditions (eg, vitamin D deficiency, rheumatoid arthritis, hypophosphatasia) and in patients receiving certain therapies (eg, bisphosphonates, corticosteroids, proton pump inhibitors). These cases have also been observed in the absence of antiresorptive therapy.
These bisphosphonate-related fractures are often bilateral; Therefore, in patients receiving denosumab therapy, if a femoral fracture is detected, examination of the hip on the opposite side is necessary.
Discontinuation of treatment with Prolia should be considered in patients with suspected atypical hip fracture, taking into account an individual assessment of the benefit-risk ratio. During treatment with Prolia®, patients should be advised to report new or unusual pain in the femur, hip or groin area. Patients who experience these symptoms should be evaluated for incomplete femoral fractures.
Multiple vertebral fractures (MVF) due to discontinuation of treatment with Prolia®, especially in patients with a history of vertebral fractures
Patients should be instructed not to interrupt therapy with Prolia without consulting their prescriber. Before discontinuing treatment with Prolia®, it is necessary to conduct an individual assessment of the benefit/risk ratio.
If treatment with Prolia is discontinued, a transfer to an alternative antiresorptive therapy should be considered.
Long-term antiresorptive therapy
Long-term antiresorptive therapy (both denosumab and bisphosphonates) may increase the risk of complications such as osteonecrosis of the jaw and atypical hip fractures due to pronounced suppression of bone remodeling processes (see section "Dosage and Administration").
Concomitant use of other medicinal products containing denosumab
Patients receiving therapy with Prolia should not receive other medicinal products containing denosumab at the same time (for the prevention of bone complications in adults with solid tumors metastasizing to the bone).
Dry natural rubber
The needle cap of the pre-filled syringe contains dry natural rubber (a derivative of latex), which may cause allergic reactions.
Excipient Warnings
This drug contains 47 mg of sorbitol per 1 ml of solution. The additive effect of the simultaneous use of drugs containing sorbitol (or fructose), as well as the intake of sorbitol (or fructose) from food, should be taken into account.
This medicine contains less than 1 mmol sodium (23 mg) per 60 mg dose, i.e. can be regarded as practically sodium-free.
Special precautions for use and disposal
- Before administration, the solution should be assessed for inclusions or color changes. The solution should not be used if it becomes cloudy, has suspended particles or changes color.
- Do not shake.
- To avoid discomfort at the injection site, the drug should be brought to room temperature (up to 25 ° C) before injection, and then the entire contents of the pre-filled syringe should be slowly injected.
Any unused drug or unused materials must be disposed of properly.
Read these instructions carefully before using the drug.
Prolia® in a pre-filled syringe with needle guard:
— It is very important that before you start self-injecting, your doctor or nurse has given you detailed instructions on how to perform the injection.
— Prolia® is administered subcutaneously (subcutaneous injection).
— Tell your doctor if you have an allergy to latex (the needle cap of the pre-filled syringe consists of a latex derivative).
— Do not remove the gray cap from the needle of a prefilled syringe until you are ready to inject.
— Do not use a prefilled syringe if it has been dropped on a hard surface. Use a new prefilled syringe and tell your doctor or nurse.
— Do not attempt to activate the safety device of a pre-filled syringe before injection.
— Do not attempt to remove the clear guard from a pre-filled syringe before injection.
If you have any questions, please contact your doctor or nurse.
Step 1: Preparation
A. Remove the blister pack with prefilled syringe from the packaging and prepare everything needed for injection: alcohol wipes, cotton swab or gauze pad, tape and sharps container (not included in the packaging).
For a more comfortable injection, leave the prefilled syringe at room temperature for about 30 minutes before injecting. Wash your hands thoroughly with soap.
Place the prefilled syringe and other necessary supplies on a clean, well-lit surface.
— Do not attempt to heat the syringe in hot water or a microwave oven.
— Do not leave the prefilled syringe in direct sunlight.
— Do not shake the prefilled syringe.
— Keep the prefilled syringe out of the reach of children.
B. Open the blister pack by pulling the label. To remove the prefilled syringe from the blister pack, grasp the safety device.
Take the syringe as shown in the picture
For security:
— Do not touch the plunger.
— Do not touch the gray needle cap.
C. Check the drug and the prefilled syringe.
— Do not use a prefilled syringe if:
- The drug is cloudy or contains foreign particles. The solution should be clear, colorless or light yellow.
- Any of the parts are damaged or broken.
- The gray needle cap is missing or loose.
- The last day of the month of expiration indicated on the label has expired.
Tell your doctor or nurse about all of the above.
Step 2: Preparing the injection site
A. Wash your hands thoroughly. Prepare and clean the injection site.
You can use:
- Upper thigh.
- Abdomen, excluding the area around the navel, approximately 5 cm.
- The outer surface of the shoulder (only if someone else is giving you the injection). Clean the injection site with a swab soaked in alcohol. Let the skin dry.
—
Do not touch the injection site before injecting.
! Do not inject in areas where the skin is thin, bruised, red, or hard. Avoid injecting into areas with scars or stretch marks.
B. Gently pull the gray cap off the needle, without twisting, away from the syringe body.
C. Pinch the injection site to create a firm surface.
! It is important to keep the skin pinched while injecting.
Step 3: Introduction
A. Pinch the skin. INSERT the needle into the skin.
— Do not touch the treated injection area.
C. Slowly and smoothly PRESS the plunger until you feel or hear a “click.” Press the piston until it clicks.
! It is important to press the plunger until it clicks to deliver the entire dose.
C. RELEASE your thumb. Then REMOVE the syringe from the skin.
Once you release the plunger, the prefilled syringe guard will cover the needle.
—
Do not put the gray needle cap back on the prefilled syringe.
Step 4: Finish
A. Dispose of the used prefilled syringe and other associated materials in a sharps container.
Medicines must be disposed of in accordance with proper regulations. Ask your doctor or pharmacist how to discard the medicine when it is no longer needed. These measures will help protect the environment.
Keep syringes and related materials out of the reach of children.
— Do not reuse a prefilled syringe.
— Do not recycle the prefilled syringe or throw it away in household waste.
B. Examine the injection site.
If blood appears at the injection site, apply pressure with a cotton swab or bandage. Do not rub the injection site. If necessary, cover the injection site with a bandage.
Instructions for administering Prolia® in a pre-filled syringe
This section provides information on how to properly administer a prefilled syringe injection. It is very important that before you begin self-injections, your attending physician or nurse instruct you in detail on the technique of performing the injection. Wash your hands thoroughly before giving the injection. If you have any questions about the injection technique, please contact your doctor or nurse.
Before starting the injection:
Read all instructions carefully before using the prefilled syringe.
DO NOT use the PZS if the cap has been removed.
How to use a pre-filled syringe?
Your doctor has given you Prolia® in a prefilled hypodermic syringe. You should inject the entire contents of a prefilled Prolia® syringe (1 ml) once and repeat the injection after 6 months as directed by your healthcare professional.
Equipment:
For self-injection you will need:
1. a new pre-filled syringe with Prolia®;
2. alcohol wipes or similar materials.
What should you do before self-administering Prolia® subcutaneously?
1. Remove the syringe from the refrigerator. DO NOT pick up a pre-filled syringe by the plunger or protective cap as this may damage the device.
2. The pre-filled syringe can be left outside the refrigerator to reach room temperature.
This will make the injection more comfortable.
DO NOT heat the prefilled syringe in any other way (such as in a microwave or hot water).
DO NOT leave the syringe in direct sunlight.
3. DO NOT shake the pre-filled syringe.
4. DO NOT remove the cap from the prefilled syringe until you are ready to inject.
5. Check the expiration date of the pre-filled syringe on the packaging.
DO NOT use a prefilled syringe if the last day of the expiration month stated on the label has passed.
6. Check the appearance of Prolia®. The solution should be clear, colorless or light yellow. If the solution becomes cloudy or has a different color, the drug should not be used.
7. Choose a comfortable, well-lit place and a clean surface where you can conveniently place all the necessary materials.
8. Wash your hands thoroughly.
How to choose the right injection site?
It is best to inject into the upper thigh and abdomen. If someone else is giving you the injections, you can use the outside of your upper arm.
How to give an injection correctly?
1. Disinfect the injection site with an alcohol wipe.
2. To avoid bending the needle, gently pull the needle cap straight away without twisting, as shown in Figures 1 and 2.
DO NOT touch the needle or press the plunger.
3. If small air bubbles are visible inside the pre-filled syringe, there is no need to remove them before injection.
Injecting the solution with air bubbles is safe.
4. Pinch the skin (without squeezing) between your thumb and forefinger. Insert the needle completely into the skin as your doctor or nurse showed you.
5. Slowly and smoothly press the plunger while holding the skin fold. Press down on the plunger until the syringe is empty.
6. Remove the needle from the skin and release the skin fold.
7. If blood appears at the injection puncture site, carefully wipe it off with a cotton swab or napkin. Do not rub the injection site. If necessary, cover the injection site with a bandage.
8. Use one PZZ for one injection only. DO NOT use any remaining medication in the syringe.
Remember
: If you have problems, seek help or advice from your doctor or nurse.
Disposal of used syringes
- DO NOT put the cap back on a used syringe.
— Keep the used syringe out of the reach of children.
— The used syringe must be disposed of properly. Ask your doctor or pharmacist how to discard the medicine when it is no longer needed. These measures will help protect the environment.