Ringworm is a general name for a group of skin diseases that manifest as characteristic rashes that can be localized in different parts of the body.
Infections differ in pathogen, clinical manifestations, severity and treatment tactics. One of the fairly common types of lichen is Zhiber's pink lichen.
Zhiber's pityriasis rosea is an acute inflammatory dermatosis of unknown etiology that develops against a background of weakened immunity, for example, after an acute respiratory viral infection or influenza. Most often, the disease is diagnosed in adolescents and young adults, while it is rare in children and the elderly.
Doctors do not have a clear opinion about the causes of pityriasis rosea, but most dermatologists are inclined to believe that the causative agent of the infection is herpes virus types 6 and 7. The herpes virus remains in a latent state in the human body for a long time, but when the protective forces are weakened, it begins to actively develop and affects the upper layers of the skin with the formation of symptoms of pityriasis rosea.
Causes of pityriasis rosea
Currently, the exact cause of the pathology is not clear. Many representatives of the medical community believe that the development of pityriasis rosea occurs under the influence of the herpes virus, but this opinion has not yet been confirmed. It is believed that the disease can be triggered by taking certain medications.
Risk factors also include:
- Decreased immunity due to acute respiratory viral infections, sore throat, colds;
- Presence of chronic diseases;
- Stressful situations;
- Disruptions in the metabolic process;
- Illiterate skin care;
- Allergic manifestations;
- Hypovitaminosis;
- Injuries and damage to the skin, including insect bites.
Pityriasis rosea develops due to hypothermia or as a consequence of vaccination. Sometimes the cause is pathologies of the digestive system.
Make an appointment with a dermatologist by phone or by filling out the online form
| Select a clinic | Skin rash | Dermatologist at the clinic | Dermatologist at home |
Methods of infection and risk groups
At the moment, there is no reliable evidence of the transmission of this disease from a sick person to a healthy one. There are only infrequent cases when someone in the environment fell ill with lichen upon contact, but in all cases there were provoking factors. These include:
- presence of herpes virus in the body;
- weakened immune system;
- recently suffered viral and colds;
- frequent hypothermia of the body.
The risk group mainly includes women under 40 years of age and children. Men suffer from this disease much less frequently. Almost no cases of infection are detected in infants and people over 40 years of age. In order to reduce the risk of contracting Gibert's disease, it is worth strengthening your immune system. It is reliably known that in most cases the disease appeared against the background of a weakening of the body’s protective functions.
Symptoms of pityriasis rosea
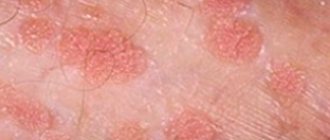
The beginning of pityriasis rosea is the formation of a maternal plaque - a single spot of a fairly large size and a round shape. Its diameter is from 2 cm, the color is pinkish, but gradually the central part of the spot turns yellow. Over time, peeling begins here.
After 7-10 days, multiple oval-shaped spots form on the surface of the skin. They are smaller than the maternal plaque - about 0.5-1 cm in diameter. For the most part, the rash spreads along the back and shoulders, covers the sides of the body, and runs along the lines of skin tension. In the center of all spots, the skin peels off, and a red border appears along the edges of the rash.
The spots that appear do not merge with each other. The pathology may be accompanied by itching. Sometimes the disease manifests itself in an atypical form - without the appearance of a maternal plaque. Pityriasis rosea lasts for several weeks, after which the rash goes away on its own. However, there is also a longer course – up to six months. Pityriasis rosea may be accompanied by weakness and malaise, drowsiness and fever.
Useful information on the topic:
- Calling a dermatologist to your home
- Fungal infections
- Rash on the body
- Sexually transmitted diseases
- How to get tested
- Wart removal
- Removal of condylomas
- Tests for STIs
- Removal of papillomas
- Skin rash
- Pyoderma
- Skin structure
- Mushroom tests
- Diagnosis of sexually transmitted infections
Dermatologists have known about Gibert's rosacea (RL; synonyms: lichen maculae and ringworm, scaly roseola, disseminated lichen) for more than 150 years (described by S. Gibert in 1860), but its etiology and pathogenesis remain unknown [1, 2]. This dermatosis is considered an inflammatory disease of unknown etiology [3]. In LV cancer, a certain causal role is noted for a number of background diseases and conditions of patients, in particular, neurotrophic and endocrine disorders, respiratory infections, visceral pathology, focal diseases, and intoxications [1, 2]. A viral etiology of LVH is suggested [4], and streptococcal genesis is also not ruled out [1, 5], but researchers are more inclined to the infectious-allergic nature of this disease [1, 3, 5].
LV cancer is included in the group of presumably infectious diseases [1, 2, 6]. The infectious nature of this dermatosis is indicated by the presence of mild prodromal symptoms, seasonal nature (usually occurs in spring and autumn), simultaneous disease of members of the same family (rarely observed), maternal plaque (primary focus) and generalized rash, paroxysmal efflorescence, slight enlargement of regional lymph nodes [ 2-4, 7]. Other representatives of this group are psoriasis, lichen planus, polymorphic exudative erythema.
The rash is preceded by a mild period of prodrome in the form of malaise, headache, myalgia, arthralgia, redness of the pharynx, and low-grade fever. After 7-10 days, a bright pink maternal plaque (reaching at least 5 cm in diameter) appears on the body in the form of a medallion, oval-round in outline. Its central part is yellowish, somewhat sunken, the edges are pink, slightly elevated. The elements of the rash are located randomly, discretely, but can touch and even merge, located on the torso, proximal areas of the skin of the extremities, in the axillary and inguinal folds, and rarely on the neck [1, 2, 8]. Itching is usually absent or mild, rarely severe [3, 8, 9]. The orientation of efflorescence along Langer lines is noted [3, 6]. In approximately 20% of patients, there is no maternal plaque, and in some cases there are several of them, which is regarded as an atypical manifestation [2, 8, 9].
In the clinical picture of LVH, one should note the peculiarity of the spots - their pink corolla and a collar of thin scales, in the center resembling crumpled (corrugated) tissue paper [8].
The diagnosis of LV cancer is based on characteristic clinical manifestations [2, 9], but in order to avoid diagnostic errors, one should remember about the atypical manifestations of dermatosis - papular, urticarial, hemorrhagic, vesiculobullous, pustular rashes, accompanied by intense itching [1, 2, 8, 10]. Sometimes, apart from the maternal plaque, there are no other rashes or they are located on the face and neck, and may also have a target-like appearance. Histological changes are not specific [1, 6].
The range for the differential diagnosis of RLZ includes a number of diseases: mycosis of smooth skin, seborrheic dermatitis, psoriasis, parapsoriasis, secondary syphilis, multiform exudative erythema, toxicoderma, Lyme disease, coin-shaped eczema, pityriasis versicolor, Devergie's disease.
RLZh compares favorably with many dermatoses by spontaneous recovery in 6-8 weeks, persistent immunity, as well as a pathognomonic feature - lacy collar folds and a bright pink corolla of spots and maternal plaque.
The prognosis of the disease is favorable. In most cases, treatment for patients with LV cancer is not required [2, 9]. However, for acute inflammatory, exudative phenomena and complicated forms, Presocial, antihistamines, sodium thiosulfate, and glucocorticosteroid drugs are used [9].
For severe rashes, antibacterial drugs are used (for example, erythromycin for 14 days), as well as ascorbic acid, calcium pantothenate, and suberythemal doses of ultraviolet radiation [10]. Externally, shaken mixtures, lorindene C, hyoxysone, and 10% methyluracil ointment are prescribed [1, 6].
It is recommended to avoid water procedures and wearing synthetic clothing; spicy, salty foods are excluded from the diet [1, 3]. It is recommended to limit the consumption of chocolate, citrus fruits and spices.
We present clinical observations of patients with LV cancer who were in City Clinical Hospital No. 14 named after. V.G. Korolenko (Fig. 1-7).
Figure 1. Patient Ts., 55 years old.
Figure 2. Patient R., 31 years old.
Figure 3. Patient S., 13 years old.
Figure 4. Patient K., 14 years old. a - front view; b — rear view.
Figure 5. Patient K., 10 years old. a - front view; b — rear view.
Figure 6. Patient Ts., 13 years old.
Figure 7. Patient Zh., 8 years old. a - front view; b — rear view.
Patient Ts., 55 years old (see Fig. 1)
, the “maternal” plaque in the back area was discovered a week before going to the doctor, daughter exanthemas began to appear 6 days after the appearance of the “maternal” plaque. There was no itching. No treatment was given.
Patient R., 31 years old, a plaque with a diameter of 2 cm of oval-round outline appeared on the skin of the left breast near the areola (see Fig. 2)
. The edges of the lesion, 2 cm wide, are pink-red, the central part is yellowish with thin scales. A similar rash appeared on the skin of the right breast after 4-5 days and on the skin of the torso (spots up to 1 cm in diameter). No treatment was given.
Patient S., 13 years old, was admitted to the DCVO on March 30, 2013 with a diagnosis of psoriasis (see Fig. 3)
. The duration of the disease was 1.5 months, it began with the appearance of a pink plaque with peeling on the thigh. The rash subsequently spread to the torso and limbs. There was no itching. Concomitant diseases: juvenile gynecomastia. Treatment: calcium gluconate, oxacillin, nystatin, mezim-forte, antihistamines; externally - zinc-oil and zinc-water talker. Full resolution of efflorescence.
Patient K., 14 years old (see Fig. 4)
. He had been ill since December and was sent to the hospital with presumptive diagnoses of psoriasis and parapsoriasis. He was treated at the DKVO from 05/23/13 to 06/21/13.
Dermatosis began with rashes on the skin of the chest, then the process spread to the torso and limbs. He was treated as an outpatient with naphtoderm, sulfur-salicylic ointment, radevit, elocom S. He took a bath every other day, and a hygienic shower every day.
Upon admission to the hospital, the acute inflammatory process is represented by spots, papules of bright pink color with oval outlines, the elements of the rash are swollen, covered with crusty scales. Moderate itching was noted. Treatment: intravenous infusion of saline with 30% sodium thiosulfate solution, calcium gluconate, antihistamines, diprospan 1.0 No. 1, cefazolin (intramuscular), enterosgel, delagil (1 tablet per day), Essentiale Forte, Sonopax, external zinc-oil and naphthalan mash, elocom cream, 2% naphthalan paste, 1% methylene blue solution. The rashes have regressed.
Patient K., 10 years old (see Fig. 5)
, was sent for treatment to City Clinical Hospital No. 14 named after. V.G. Korolenko with a diagnosis of guttate parapsoriasis. Disease duration - 2 weeks. First, a pink plaque with peeling appeared on the skin of the abdomen. Soon similar spots of smaller sizes were found on the torso and limbs, in the inguinal folds. The “maternal” plaque is 3.5 cm in diameter, edematous erythematous scaly spots up to 1 cm in size, without itching. According to laboratory and instrumental examinations, as well as consultations with specialists, no pathology was identified. Diagnosis: LV. Treatment: sodium hyposulfite, enterosgel, tavegil, macropen; zinc-oil mash, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
Patient Ts., 13 years old (see Fig. 6)
, 1.5 months was treated as an outpatient for psoriasis (white salik externally). The DCVO confirmed LVH. Treatment: oxacillin, calcium gluconate, enzistal, antihistamines, 2% naphthalan paste, 1% salicylic cream, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
Patient Zh., 8 years old (see Fig. 7)
, received external laticort and zinc paste for 2 weeks as an outpatient. Water procedures. The itching didn't bother me. Upon admission to the DCVO, a multiple rash of pink, swollen spots was observed; some of the elements in the central part had a collar of thin scales, reminiscent of crumpled tissue paper. Elements of the rash on the trunk and limbs with a diameter of 0.5-0.7 cm, on the neck - 1.5-2 cm. There was a tendency towards peripheral growth of efflorescence and merging into larger lesions. Treatment: oxacillin, calcium gluconate, enzistal, antihistamines, 2% naphthalan paste, 1% salicylic cream, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
At first glance, LVRD does not represent a pressing dermatological problem. The main thing is timely recognition and refusal of water procedures, which ensures spontaneous regression of the pathological process within 6-8 weeks. Unfortunately, at present, patients with pityriasis rosea are admitted to hospital treatment due to inadequate treatment and care due to erroneous diagnosis. Intense insolation also plays a negative role. With irrational therapy, complications are observed in the form of eczematization, impetiginization, which leads to an increase in recovery time to 2-3 months.
Pityriasis rosea in children
In childhood, pityriasis rosea manifests itself mainly after acute respiratory viral infection. The scales on the rash are usually sparse or absent altogether. The spots most often form in the inguinal folds and armpits. With this disease, the child can continue to live a normal life, the only limitation concerns water procedures. Do not use washcloths or rub the skin with hard towels. During the period of exacerbation of the disease, excessive sweating should be prevented, so physical activity will have to be limited.
It is important to follow all doctor's recommendations. As a rule, drug treatment is not required, but special attention should be paid to restoring the body's immune defenses. In this regard, a balanced diet, room ventilation, and adherence to general hygiene rules play an important role. If there is itching or an atypical course of the pathology, the doctor prescribes medications. But it is not recommended to use folk remedies.
Description of the disease
Depending on the type of lichen, the rash may be dry or weeping, pale pink or bright red.
Most often, the disease affects the back, face and chest of the child (it is in these areas that the largest number of sweat glands are located). The disease is infectious in origin and is caused by viruses or fungi. The disease most often manifests itself in the spring-summer season, when it is warm and humid outside. At the moment, a large number of varieties of lichen are known. Many of them are highly contagious and potentially dangerous to the child’s immediate environment. That is why, if there is any suspicion of an infectious disease, it is necessary to immediately show the patient to a qualified specialist.
Pityriasis rosea in pregnant women
In pregnant women, pityriasis rosea can develop due to hormonal changes in the body (deficiency of female sex hormones) or a weakening of the immune system due to toxicosis. The disease does not affect the condition of the fetus and does not cause pathologies. However, it is necessary to identify the causes of the disease and eliminate them, since the health of the mother depends on the health of her baby.
The main treatment in such circumstances will be restorative methods. Doctors categorically prohibit the ingestion of decoctions of medicinal herbs, especially St. John's wort, sage, and oregano. Interferons are used to strengthen the immune system, but they should be taken with caution so that your own protective functions do not decrease even further. Multivitamin complexes are often prescribed.
When the disease develops, pregnant women should pay attention to their diet and do special gymnastic exercises. For those who are concerned about itching, doctors recommend treating the rash with vegetable oil, chamomile infusion, and calendula decoction. It is very important to avoid stress, which has an extremely negative effect on the body, including causing pityriasis rosea.
Prevention of pityriasis rosea
Simple preventive measures can prevent the development of the disease. To protect your body from pityriasis rosea, you need:
- Observe the rules of personal hygiene;
- Avoid synthetic and woolen clothing;
- Carefully select cosmetics, paying attention to their composition, quality, expiration dates;
- Adjust your diet so that your diet contains all the necessary substances;
- Avoid products with artificial colors and additives;
- Forget about bad habits;
- Temper yourself;
- Take vitamins as prescribed by your doctor.
It is advisable not to indulge in strong tea and coffee, fatty and fried foods. At the first manifestations of pityriasis rosea, you need to protect the areas of skin with rashes from direct sunlight and consult a doctor.
Diagnosis of pityriasis rosea
Diagnosis of the disease is not difficult, since the manifestations of the pathology are quite typical. But the doctor must make sure that the rash is caused by pityriasis rosea, and not by eczema, syphilis, psoriasis or fungal infection of the skin - mycosis.
In addition, the disease can occur in an atypical form, so special studies and tests are carried out to confirm the diagnosis.
| Appointment with a dermatologist at the clinic. Call a dermatologist at home. | Reception is strictly by appointment, make an appointment by phone: +7 | Prices for services | Reviews about the clinic |
Clinical picture
Most patients do not have severe symptoms of the disease; in some cases they complain of mild or severe itching. The problem occurs in emotional people or patients with skin allergies that react inadequately to external stimuli.
The first sign of pathology is the formation of a “mother spot” - a large pink area of dermis with pronounced peeling. After the scales are torn off, the spot acquires a brown tint and clear boundaries. It does not exceed 2-5 cm in diameter. Initially, a single focus of pityriasis rosea is registered, later several additional ones appear on the body.
Secondary spotting forms a few days after the appearance of the mother spot. Changes are recorded on the arms and legs, back, and abdomen. Secondary rashes have a similar shape, with a reddish or pinkish tint. They rarely occur in the neck or face. The appearance of the first spots requires immediate consultation with a doctor and treatment prescribed by a specialist.
Treatment methods for pityriasis rosea
In the typical course of the disease, treatment may not be required, but only a doctor can make such conclusions based on the examination results. In such situations, the patient is recommended to:
- Hypoallergenic diet;
- Limiting water treatments (shower instead of bath), using a soft washcloth;
- Wearing clothes made from natural fabrics;
- Avoiding activities that cause excessive sweating.
In case of protracted course of pityriasis rosea, antiviral medications, treatment of rashes with salicylic alcohol, and topical antibacterial agents - ointments, can be prescribed. Antihistamine medications are used to reduce itching and can also prevent the spread of rashes. In some cases, treatment with antibiotics is required.
Ointments used for pityriasis rosea
For severe, disturbing itching, anti-inflammatory and antiallergic creams and formulations are prescribed. Ointments are used to treat the disease:
- Hydrocortisone – has an anti-inflammatory effect, relieves itching;
- Olettrinovaya is an antibacterial drug;
- Prednisolone - a composition with healing properties that can relieve inflammation;
- Loriden A - ointment with antipruritic, anti-parotid, anti-edematous effects;
- Sinalar – eliminates inflammation due to antibacterial properties;
- Lassara paste is an antiseptic that discolors stains;
- Rioloxol - antibacterial and anti-inflammatory;
- Flucinar – effectively relieves itching, eliminates flaking and inflammation;
- Sulfur – inhibits the inflammatory process.
Tsindol suspension also helps dry the skin, eliminate inflammation and itching. Ointments are applied to the pink plaques in a thin layer in accordance with the instructions and directions of the doctor. The treatment course is 2-3 weeks, the frequency of use of each drug is determined individually. At the same time as using medications, you should be careful with the affected skin.
However, any ointments, like all other medications, should be used exclusively as prescribed by a doctor, so as not to aggravate the situation. In addition, the effectiveness of each of the listed external remedies greatly depends on the patient’s age, the state of his immunity, the degree of spread of lichen, the presence of chronic pathologies and other characteristics of the body.
Ointments for ringworm
Ringworm can appear on the scalp and areas of the body where hair does not grow. Treatment of such forms of pathology involves the use of various means.
If ringworm is detected on the head, it is recommended to disinfect the hair before starting therapy. The list of good remedies includes alcohol or iodine solutions: Vocadin, Yoddicerin, Nitrofungin, sulfur ointment.
Treatment is not limited to the use of external agents; in addition, antifungal tablets are taken.
Vokadin
Vocadine is made on the basis of iodine tincture and provides anti-inflammatory and antimicrobial effects. The drug is applied to the affected areas according to the instructions for use. Treatment cannot be carried out for the following conditions:
- pathologies of the thyroid gland;
- pregnancy of any stage;
- children under 6 years of age.
Nitrofungin
This solution is a complete medicine against fungal infection. It can be used as an independent remedy or supplemented with other ointments against lichen.
During the day, infected areas of the body are treated at least 3-4 times, the optimal course of treatment is from 4 to 6 weeks. You should consult your doctor regarding possible adverse reactions.
Lamisil
Ringworm ointment Lamisil is made on the basis of the substance terbinafine, it works well against ringworm, red and other types of lichen in humans. It is necessary to carefully monitor the dosage of the medication and avoid excessive application.
Sulfuric ointment
A cheap and accessible product, it has a disinfecting effect and effectively fights lichen. Ointment:
- has no contraindications;
- does not cause adverse reactions in the body.
Before use, the affected area is treated with iodine solution.
Exifin
Cream against fungal infection, can be used during pregnancy. Application is carried out on cleansed skin, it is recommended to apply twice a day, in a thin layer. There are no contraindications, but before treating small children it is imperative to consult a pediatrician or dermatologist.
Calling a dermatologist to your home for pityriasis rosea
When the first signs of pityriasis rosea appear, you should consult a doctor. Today there is a convenient service for calling a doctor to your home, which provides many advantages:
- Saving time - no need to go to a medical facility or wait for your turn at the office door. You can simply arrange a doctor’s visit at a time convenient for you;
- Comfort – communicating with a doctor at home is much easier, because the doctor is not distracted by other patients and clinic staff, he can spend as much time as necessary on examination and consultation;
- Calmness – for children of all ages, a visit to a medical facility is often stressful, which plays a negative role in the development of many diseases, including pityriasis rosea. A doctor’s home visit will save the child from unnecessary worries;
- No risk – the development of pityriasis rosea often occurs against the background of weakened immunity. In such circumstances, contact with other patients is undesirable, but it is almost impossible to avoid it in the corridors of the clinic, as well as in public transport on the way to the medical facility. At home, such a risk is eliminated;
- If the disease is accompanied by fever, calling a doctor at home will be the best solution;
- Examination at home is the most convenient option for older people, mothers with small children, and patients with disabilities.
The quality of medical care at home is no different from that provided in a medical facility. The doctor gives the necessary recommendations, provides full consultation, diagnoses the disease and prescribes adequate treatment.
Common symptoms and manipulations in dermatology:
- Skin rashes
- Calling a dermatologist to your home
- Itching in the urethra
- Itchy skin
- Skin rash
- Prevention of casual sex
- Skin neoplasms
- Pyoderma
- Pityriasis rosea
- Streptoderma
- Scabies
- Peeling skin
- Fungal infections
- Skin infection
- Pus on the skin
- Blisters on the skin
- Papillomas on the foreskin
- Sexually transmitted diseases
- Skin structure
The causes of the disease are deprived
The etiology of individual forms of day deprivation has not been identified, but certain factors that provoke their appearance and relapse have been identified:
- genetic predisposition;
- allergic reactions;
- stress;
- hypothermia;
- transferred viral disease.
Weakening of the immune system due to various diseases in some cases provokes the occurrence of pityriasis versicolor or versicolor (its second name) lichen.
What does lichen look like on human skin?
This disease most often occurs in people over 30-35 years of age. But in recent years, doctors have noted that cases of lichen in younger people of different sexes have become more frequent. The possibility of infection with various types of lichen persists up to 70 years.
Where to go with pityriasis rosea
Diagnosis and treatment of pityriasis rosea is carried out by a dermatologist. There are at least two important reasons to see a doctor rather than self-medicate. The first is the need to define the disease. Often, pityriasis rosea has some similarities with other skin pathologies such as fungal infections, psoriasis, mycosis of smooth skin or syphilis.
The second reason is to prevent complications. Despite the fact that the disease usually goes away on its own, sometimes lack of treatment or incorrect selection of drugs creates a serious risk of complications. They consist in the spread of rashes, the appearance of prolonged severe itching, and skin pigmentation after recovery.
With a strong decrease in immunity, a complicated course of the disease with an increase in temperature is possible. In people with blood pathologies or cancer who have undergone chemotherapy, the disease can develop again. The use of folk recipes and all kinds of folk remedies can cause contact dermatitis and even chemical burns. When using dyes, for example, celandine, diagnosing the disease is difficult, and a bacterial infection enters the body.
Symptoms
The disease manifests itself in the form of spots on the skin.
First, several so-called maternal formations about 5 cm in size appear. Then, over the course of a week, a large number of similar spots of smaller sizes scatter throughout the body. The most vulnerable areas are the abdomen, shoulders and hips. Rashes are rare on the face and neck. All spots, both maternal and “baby” ones, have the same appearance: pink or with a yellowish tint, round in shape, flaky inside with a smooth rim. Often, apart from spots, this disease does not manifest itself in any way. Therefore, as soon as any characteristic formations are discovered on the body, you should immediately contact a special clinic to diagnose pityriasis rosea. Sometimes itching appears in the affected areas, and the lymph nodes on the neck and chin become enlarged. If a person’s immunity is severely weakened, severe fatigue, fever or general intoxication of the whole body appears. There are cases when the external manifestation differs from the usual: blisters or white nodules appear on the skin.
What tests need to be taken for pityriasis rosea?
The diagnostic method and set of necessary studies are determined by a dermatologist. Typically, the patient takes a blood test to study general indicators. Tests are often ordered to detect antibodies to viral agents, including syphilis and herpes. To exclude fungal damage to the skin, microscopic examination of scrapings from the site of the lesion is carried out.
Additionally, the doctor may prescribe an immunogram if there is a suspicion of a significant decrease in the body's defenses. The cause of pityriasis rosea is an allergic reaction, so testing for allergens is possible. If necessary, the doctor prescribes additional examinations and consultations with specialists. Typically, such measures are taken in case of protracted or atypical course of the pathology.
Diagnosis of the disease
Determining the correct diagnosis is sometimes difficult due to the absence of a pathogen. The disease can be confused with other lichen and toxicoderma.
The examination is a visual inspection. A qualified dermatovenerologist will take into account the characteristic placement of spots on the body, their appearance, shape, and based on this will make a diagnosis.
Tests that may also be prescribed:
- general urine and blood tests;
- microprecipitation reaction (diagnosis of syphilis);
- scraping from affected areas.
After diagnosis, the specialist will determine how to treat pityriasis rosea and will advise the patient in detail regarding lifestyle.
Make an appointment