Relevance
Fluconosole is an antifungal drug that inhibits cytochrome P451 (CYP51) in fungi, which plays a major role in ergosterol synthesis and fungal cell wall formation. In humans, CYP51 is required for the synthesis of cholesterol required for the formation of embryonic tissues.
Fluconazole is often prescribed as first-line therapy during pregnancy to treat fungal infections.
Researchers from Canada assessed the association between low- and high-dose fluconazole use during pregnancy and the risk of spontaneous abortion, major congenital malformations, and stillbirth.
pharmachologic effect
The abstract contains information that the drug acts as an antifungal agent, specifically inhibiting the synthesis of fungal sterols. Belongs to the class of triazole compounds.
There is a specific effect on fungal enzymes that depend on cytochrome P450. The active substance demonstrates activity against a variety of strains of Candida spp. (including effective against visceral candidiasis), Cryptococcus neoformans (including effective against intracranial infections), Trichophytum spp, Microsporum spp. The drug is also active against microorganisms that are causative agents of endemic mycoses: Coccidioides immitis, Hystoplasma capsulatum, Blastomyces dermatitidis.
The drug stops the conversion of fungal cells into lanosterol into ergosterol. Under its influence, the permeability of the cell membrane increases, the process of its growth and replication is inhibited. It is highly selective for cytochrome P450 of fungi, but in the human body it almost does not inhibit these enzymes. Does not demonstrate antiandrogenic activity.
Pharmacokinetics and pharmacodynamics
Wikipedia indicates that after oral administration, the drug is actively absorbed into the human gastrointestinal tract. In plasma, the concentration of the active substance is more than 90% of the level that is observed if intravenous administration is practiced. The absorption of the substance is not affected by food intake, so it does not matter how you take it, before or after meals. After taking the medicine orally, the highest concentration in the blood occurs after 0.5–1.5 hours. The half-life from the blood is 30 hours. That is, you can take the product once a day. For vaginal candidiasis, a single dose of the drug is sufficient, for which one tablet or another form of the drug is used.
11–12% of the active substance binds to blood plasma proteins. When the drug begins to work depends on the treatment regimen. If you take the medicine once daily, then a stable concentration of the active component in the human blood is observed on the fourth or fifth day (in 90% of people). If on the first day of treatment the patient is given a double daily dose, then this effect is observed already on the second day of treatment.
Penetrates into all fluids in the body. It is excreted from the body through the kidneys, approximately 80% is excreted unchanged.
Pharmacological properties of the drug Fluconazole
Antifungal agent of the class of triazole compounds. Fluconazole has a pronounced antifungal effect and specifically inhibits the synthesis of fungal sterols. It has a specific effect on fungal enzymes dependent on cytochrome P450. Active against various strains of Candida spp. (including visceral candidiasis), Cryptococcus neoformans (including intracranial infections), Microsporum spp. and Trichophytum spp. Fluconazole is also active against pathogens of endemic mycoses: Blastomyces dermatitidis, Coccidioides immitis (including intracranial infections), Hystoplasma capsulatum . After oral administration, it is well absorbed from the digestive tract; the concentration in the blood plasma exceeds 90% of the concentration level achieved with intravenous administration. Eating does not affect the absorption of fluconazole. The maximum concentration in blood plasma is achieved 0.5–1.5 hours after oral administration. The half-life of the drug from blood plasma is 30 hours, which allows the drug to be used once a day during a course of treatment with fluconazole and provides a therapeutic effect for vaginal candidiasis after a single dose of the drug. The concentration of the active substance in the blood plasma is directly proportional to the dose taken. 11–12% of fluconazole is bound to plasma proteins. With a single daily dose of fluconazole on days 4–5, a stable concentration in the blood plasma is achieved in 90% of patients. When a loading (twice daily) dose is administered on the 1st day of treatment, the above effect is achieved by the 2nd day of treatment. The pharmacokinetics of fluconazole when administered intravenously is similar to that when administered orally. Fluconazole penetrates well into all body fluids. In the cerebrospinal fluid, the concentration of fluconazole reaches 80% of its concentration in the blood plasma. Fluconazole is excreted from the body in the urine, 80% unchanged. Fluconazole clearance is directly proportional to creatinine clearance.
Indications for use
The following indications for use of the drug are determined:
- infectious diseases caused by candida ( disseminated candidiasis , generalized candidiasis , other forms of invasive candidiasis ;
- candidiasis of the mucous membranes (including the pharynx, oral cavity, esophagus);
- candiduria;
- chronic atrophic and mucocutaneous candidiasis of the oral cavity (develops in people with dentures);
- non-invasive bronchopulmonary infections;
- genital candidiasis ( vaginal candidiasis in acute form and with relapses);
- prevention of recurrent manifestations of vaginal candidiasis (if the disease develops three times a year), candidal balanitis ;
- cryptococcal infection, cryptococcal meningitis;
- onychomycosis;
- dermatomycosis (including mycoses of the body, feet, groin area);
- pityriasis versicolor;
- endemic mycoses deep;
- prevention of the development of fungal infections in people who have undergone cytostatic or radiation therapy.
Nosological classification (ICD-10)
- B20.4 Disease caused by HIV, with manifestations of candidiasis
- B20.5 Disease caused by HIV, with manifestations of other mycoses
- B35.1 Mycosis of nails
- B35.3 Mycosis of the feet
- B35.4 Mycosis of the trunk
- B35.6 Athlete's foot
- B36.0 Tinea versicolor
- B37.0 Candidal stomatitis
- B37.1 Pulmonary candidiasis
- B37.2 Candidiasis of the skin and nails
- B37.3 Candidiasis of the vulva and vagina (N77.1*)
- B37.4 Candidiasis of other urogenital sites
- B37.6 Candidal endocarditis (I39.8*)
- B37.7 Candidal septicemia
- B37.8 Candidiasis of other sites
- B38 Coccidioidomycosis
- B39 Histoplasmosis
- B41 Paracoccidioidomycosis
- B42 Sporotrichosis
- B45 Cryptococcosis
- B45.0 Pulmonary cryptococcosis
- B45.1 Cerebral cryptococcosis
- B45.2 Cutaneous cryptococcosis
- N51.2 Balanitis in diseases classified elsewhere
- Y88.0 Consequences of adverse effects of drugs, medications and biological substances used for therapeutic purposes
- Z51.0 Radiotherapy course
- Z51.1 Chemotherapy for neoplasm
Contraindications
There are the following contraindications for the use of this medicine:
- manifestation of high sensitivity to fluconazole or to azole compounds, which are similar in chemical structure to fluconazole;
- concurrent use of terfenadine if the patient receives a dose of Fluconazole 400 mg per day or more;
- concomitant use of astemizole or any other drugs that increase the QT interval;
- age up to 4 years.
It should be taken with caution in case of liver failure, also kidney failure, when a rash appears in people suffering from a superficial fungal infection, in potentially pro-arrhythmogenic conditions in people with risk factors (organic heart disease, taking medications that provoke the development of arrhythmia , electrolyte imbalance). How to take Fluconazole in this case, you should definitely ask a specialist.
Side effects
When treated with the drug, the patient may develop the following side effects:
- abdominal pain, diarrhea ;
- headache;
- nausea , flatulence ;
- skin rash;
- hepatotoxic effects;
- anaphylactic reactions.
How to take the medicine when such effects occur, and whether it is worth continuing treatment, should be individually consulted with a doctor.
Instructions for use of Fluconazole (Method and dosage)
The drug is prescribed for oral administration (Fluconazole Stada capsules, Fluconazole Teva, tablets) or for intravenous administration. There are also other forms of medication, the active ingredient of which is fluconazole - suppositories, ointment.
The solution is infused at a rate not exceeding 10 ml per minute.
Fluconazole tablets, instructions for use
The dosage of the drug depends on the disease and its severity.
Patients with disseminated candidiasis and candidemia are prescribed 400 mg on the first day, then the dose should be reduced to 200 mg. For the treatment of generalized candidiasis, are advised to take 6–12 mg per 1 kg of weight per day.
For patients with oropharyngeal candidiasis , 50 mg to 100 mg of Fluconazole is indicated once a day, the treatment period is 1-2 weeks.
People suffering from atrophic candidiasis of the oral mucosa are advised to take 50 mg once a day. Treatment is combined with the use of local products for the treatment of prostheses. When treating other candidiasis infections of the mucous membranes, 50–100 mg per day is prescribed, the period of therapy is from 14 to 30 days.
In order to prevent the development of relapses of oropharyngeal candidiasis in people with AIDS , 150 mg once a week is indicated. If mucosal candidiasis develops in children, the dose should be taken at the rate of 3 mg of drugs per 1 kg of weight per day. On the first day, you can give your child a double dose.
Patients with cryptococcal infections and cryptococcal meningitis are usually prescribed 200–400 mg of drugs once a day. On the first day, 400 mg of the drug is indicated. The duration of treatment can be from 6 to 8 weeks. Children are prescribed a dose of 6–12 mg per 1 kg of weight per day.
People suffering from infectious skin diseases are recommended to prescribe 150 mg once a week or drink 50 mg of the drug once a day. Treatment should be continued for 2-4 weeks. For men and women with mycosis of the feet , longer therapy is sometimes required - up to 6 weeks.
Patients with pityriasis versicolor are recommended to take 300 mg once a week, the treatment period is 2 weeks. Depending on the intensity of your symptoms, your doctor may prescribe another dose of Fluconazole in the third week. It is possible to use another treatment regimen - 50 mg 1 time per day, the treatment period is two to four weeks.
Patients with onychomycosis are prescribed 150 mg once a week. Therapy should continue until a healthy nail grows in place of the diseased nail.
People suffering from deep endemic mycosis sometimes undergo a long course of treatment with the drug, which can last up to two years. The dose per day is 200–400 mg.
Instructions for the use of fluconazole for thrush stipulate that for vaginal candidiasis, a single dose of the drug is taken, its dose is 150 mg.
As a rule, Fluconazole for thrush is effective after a single dose. But your doctor will tell you more about how to take Fluconazole for thrush after an individual consultation. Before determining how to take any medicine for thrush if you have thrush, the specialist takes into account the causes of the disease and the individual characteristics of its course. For chronic thrush, Fluconazole Teva or other types of the drug are prescribed to prevent relapses at a dose of 150 mg once a month. The product should be used for 4-12 months. For the purpose of prevention, capsules are prescribed in a dose of 50–400 mg once a day, depending on how high the risk of the disease is. For children with thrush, Fluconazole tablets are prescribed at a dose of 3–12 mg of medication per 1 kg of weight per day. How much to drink depends on the severity of the infection.
For balanitis, the treatment regimen for men is as follows: the drug should be taken in a dose of 150 mg once.
Some patients are interested in whether it is possible to take pills or capsules during menstruation. According to experts, you can take Fluconazole at any time, regardless of your monthly cycle. How long it takes for the medicine to help depends on the intensity of the symptoms of the disease.
The use of fluconazole for the treatment of fungal infections in urology
Alyaev Yu.G., Grigoryan V.A., Sultanova E.A., Allenov S.N., Shpot E.V.
Infections caused by yeast-like fungi of the genus Candida (Candida spp.) are the most common of all fungal infections Candida is often the causative agent of nosocomial infections and extremely rarely of community-acquired infections in patients without urinary disorders. The increasing importance of infections caused by fungi of the genus Candida is associated with the widespread use of invasive diagnostic and treatment , immunosuppressive therapy and antimicrobial drugs with a broad spectrum of antibacterial activity [1–4].
Asymptomatic candiduria and candidal cystitis in women
The detection of candida in urine is called candiduria. Candiduria is rarely found in healthy people. Risk factors for candiduria include:
- Diabetes mellitus (DM). In patients with diabetes, the risk of uroinfections caused by fungi increases significantly. Diabetes is a predisposing factor for candiduria, since in patients with glucosuria, the intensity of fungal growth increases, resulting in active colonization of the women’s vagina by fungi of the genus Candida. Additional risk factors include decreased phagocytic activity and nonspecific resistance, as well as urinary retention in patients with a neurogenic bladder [5]. In addition, patients with diabetes are more often subjected to instrumental studies and receive antibacterial drugs.
- Antibacterial therapy. In 30% of healthy individuals, Candida colonizes the mucous membrane of the gastrointestinal tract. However, in patients receiving antibiotics, colonization rates can reach 100% [6]. There is no evidence that the administration of antibiotics directly leads to an increase in the proliferation or virulence of Candida, however, there is evidence indicating that suppression of the endogenous flora by antibiotics leads to Candida colonization of the intestines, genital tract, and urethra [6].
- Bladder catheterization. A catheter inserted into the bladder is the point of entry for microorganisms into the urine collection system. All long-standing catheters are necessarily colonized by flora [7].
- Other risk factors. Other risk factors for candiduria are older age, female gender [8], the use of immunosuppressive drugs, radiation therapy, the installation of intravenous catheters, obstruction of urine outflow, and tuberculosis of the genitourinary system [6].
Asymptomatic candiduria, as a rule, is discovered by chance, is not accompanied by clinical manifestations and does not require treatment , except for the presence of risk factors for generalization of infection .
At urological clinic, we treated asymptomatic candiduria in 15 patients: 9 patients suffered from diabetes (and their blood glucose levels were not sufficiently corrected); 2 patients had recently undergone chemotherapy for breast cancer, 4 patients were diagnosed with severe bladder dysfunction such as detrusor hypotension.
All patients were treated with fluconazole 150 mg orally, once.
As a rule, a single dose of the drug was sufficient to eliminate candiduria. Repeated use of fluconazole was required in only 1 patient suffering from diabetes. The absence of candiduria was confirmed by double bacteriological examination of urine performed at an interval of 2 weeks.
Candidal cystitis, in addition to candiduria, is accompanied by the usual signs of inflammation of the bladder: pain during urination of varying severity, pain in the suprapubic region, frequent urination in small portions, burning in the external genital area, terminal gross hematuria.
At urological clinic we examined 58 of the following patients:
- in 48 of them, cystitis had a mixed etiology (i.e., bacteria of the predominantly intestinal group were sown at a titer of >103 CFU/ml in combination with fungi of the genus Candida at a titer of >104 CFU/ml);
- In 10 patients, bacteriological examination of urine revealed only Candida fungi in a titer of 104 to 108 CFU/ml.
Patients in this latter group received long-term therapy with broad-spectrum antibiotics for chronic recurrent cystitis without sufficient antifungal prophylaxis.
All patients were treated taking into account the sensitivity of the microflora. Patients with cystitis of mixed etiology were prescribed an antibacterial drug in combination with fluconazole :
- antibacterial drug + fluconazole orally 100–200 mg/day. (depending on the Candida titer and duration of antibacterial therapy), 7–14 days.
Patients with candidal cystitis were prescribed fluconazole as monotherapy according to the regimen given above.
It should be noted that the treatment of candiduria turned out to be effective in 100% of cases, which is confirmed by the results of a double bacteriological examination of urine performed at an interval of 2 weeks.
Candidal balanoposthitis and urethritis in men
Candidal balanoposthitis is one of the most common mycotic infections of the penis [9]. In addition to independent damage and development of balanoposthitis, there is a secondary addition of candidiasis infection against the background of already existing balanoposthitis of a different etiology. The clinical picture of balanoposthitis caused by Candida fungi is manifested by the presence of patchy erythema, swelling of the skin, and the appearance of erosive and ulcerative elements, while the pathological process can spread to the skin of the scrotum. Data from microscopic and bacteriological studies allow us to establish the correct diagnosis [9].
One of the routes of infection for candidal balanoposthitis is sexual, but the presence of endocrinopathies (DM, thyroid disease, obesity, etc.), a decrease in the body’s immunological reactivity and other factors are of decisive importance.
The urological clinic has experience in treating 327 patients with candidiasis balanoposthitis.
Depending on the severity of the process, treatment was carried out with local or systemic drugs or a combination of both.
For mild forms of balanoposthitis, along with compliance with hygienic measures, the following was used:
clotrimazole, 1% cream, topically 2–3 times a day, 1–2 weeks. or econazole, cream or powder, topically 2 times a day, 1–2 weeks.
In the presence of risk factors for generalization of infection (for example, in patients with diabetes or patients with immunosuppression), as well as in cases of pronounced inflammatory changes, local therapy was supplemented with drugs for systemic use :
- fluconazole 150 mg orally, once or fluconazole 150 mg orally, on the 1st day, then 50 mg once a day, 7 days. or fluconazole 200 mg orally, on the 1st day, then 100 mg 1 time per day, 4 days.
This therapy was effective in 93–95% of patients, which was confirmed by the results of examination, microscopic and bacteriological examination. In 5–7% of cases, the course of treatment had to be repeated or prolonged.
Often, candidal balanoposthitis is combined with candidal urethritis [9]. In this case, patients experience pain when urinating, frequent urination, cheesy discharge from the urethra, and hyperemia of the urethral sponges.
The diagnosis is made based on the characteristics of the clinical picture and the results of laboratory methods:
- microscopic examination of a native or Gram-stained preparation allows not only to detect the presence of Candida with a predominance of vegetative forms of the fungus (mycelium and budding yeast cells), but also to assess the composition of the urethral microflora (pathogenic and conditionally pathogenic microorganisms) and the severity of the leukocyte reaction;
- Bacteriological examination makes it possible to determine the species of the isolated fungal culture and accompanying microorganisms, as well as to assess drug sensitivity. The growth of fungal colonies >104 CFU/ml is diagnostically significant [9].
In 55 of 327 patients with candidal balanoposthitis, candidal urethritis was also detected.
Treatment in this case necessarily included a systemic antifungal drug:
- fluconazole 150 mg orally on the 1st day, then 50 mg 1 time per day, 7 days. or fluconazole 200 mg orally on the 1st day, then 100 mg 1 time per day, 4 days.
Prevention of fungal infections
Experience in treating urological patients with various inflammatory diseases requiring the prescription of broad-spectrum antibiotics indicates that fluconazole is one of the main and most effective drugs used to prevent fungal superinfection. Depending on the duration of antibacterial therapy, the presence of concomitant diseases (especially diabetes and immunosuppressive conditions), the drug is prescribed once, repeatedly or in prolonged courses:
fluconazole 150 mg orally, once (if necessary, repeat after 1 week, or fluconazole 50 mg orally, 1 time per day, daily or every other day, 7–14 days.
Conclusion
Fluconazole is widely used in urological practice.
The drug has a wide spectrum of action, including most species of Candida, Cryptococcus neoformans, dermatophytes, Malassezia furfur and the “classical” dimorphic pathogens Histoplasma capsulatum, Blastomyces dermatitidis, Paracoccidioides brasiliensis, Coccidioides immitis.
Among the fungi of the genus Candida, the most sensitive to fluconazole are C. albicans, which are the causative agents of most fungal urological infections. Resistance in C. albicans strains rarely develops during treatment.
Fluconazole is soluble in water and is quickly and almost completely absorbed from the gastrointestinal tract. More than 90% of the dose taken orally enters the bloodstream. Simultaneous food intake, as well as gastric acidity, do not affect the absorption of the drug. Peak concentrations are created within 1–2 hours, equilibrium concentrations are achieved by days 4–6 with 1 dose daily. The pharmacokinetic properties of the drug are the same when administered orally or intravenously.
In blood plasma, no more than 12% of the drug is bound to proteins, the main amount is in free form. Therefore, fluconazole penetrates well into all body fluids.
Fluconazole is excreted by the kidneys, mainly in unchanged form. Very high – more than 100 mg/l – concentrations of the drug are created in the urine. Excretion of the drug depends on the glomerular filtration rate. Fluconazole is very poorly metabolized by the liver. The plasma half-life is approximately 30 hours; dosage and duration of therapy do not affect the half-life [10].
Thus, it is obvious that fluconazole can be considered the drug of choice for both the treatment and prevention of fungal infections in the majority of urological patients.
Literature
1. Storfer SP, Medoff G, Fraser VJ et al. Candiduria: retrospective review in hospitalized patients. Infect Dis Clin Pract 1994; 3:23–9.
2. Leu HS, Huang CT. Clearance of funguria with short–course antifungal regimens: a prospective, randomized, controlled study. Clin Infect Dis 1995; 20: 1152–7.
3. Jacobs LG, Skidmore EA, Freeman K et al. Oral fluconazole compared with bladder irrigation with amphotericin B for treatment of fungal urinary tract infections in elderly patients. Clin Infect Dis 1996; 22:30–5.
4. Lundstrom T, Sobel J. Nosocomial Candiduria: A Review. Clin Infect Dis 2001; 32:1602–7.
5. Goeke TM. Infectious complications of diabetes mellitus. In: Grieco MH, ed. Infections in the abnormal host. New York: Yorke Medical Books, 1980; 585–600.
6. Fischer JF, Chew WH, Shadomy S et al. Urinary tract infections due to Candida albicans. Rev Infect Dis 1982; 4: 1107–18.
7. Stamm WE. Catheter–associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med 1991; 91 (suppl. 3B): 65S–71S.
8. Kauffman CA, Vazquez JA, Sobel JD et al. Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis 2000; 30:14–8.
9. Rational pharmacotherapy of skin diseases and sexually transmitted infections (edited by A.A. Kubanova and V.I. Kisina). M.: Litterra, 2005.
10. Sergeev A.Yu., Sergeev Yu.V. Fungal infections. Guide for doctors. M.: BINOM-Press, 2003.
Interaction
Before starting treatment, it is important to know not only what Fluconazole in tablets and other forms helps with, but also about the interaction of drugs with other drugs.
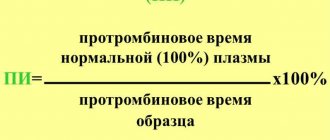
When taking Warfarin , the prothrombin time of fluconazole becomes longer.
With simultaneous administration of hypoglycemic oral agents belonging to the group of sulfonylurea derivatives, the half-life of Fluconazole increases. As a result, there is a possibility of hypoglycemia.
With simultaneous administration of phenytoin, a clinically significant increase in phenytoin concentrations is observed.
With simultaneous repeated use of hydrochlorothiazide, an increase in the concentration of fluconazole in the blood is observed. There is no need to change the dosage.
With simultaneous treatment with Rifampicin, AUC decreases by 25%. The half-life is also reduced by 20%. In some cases, the doctor decides to increase its dose.
When treating with Fluconazole, monitoring the concentration of cyclosporine in the blood is recommended.
If the patient simultaneously receives high doses of Theophylline , it is important to consider the possibility of Theophylline overdose.
It is contraindicated to take a dose of more than 400 mg per day in combination with terfenadine .
When taking cisapride , negative side effects from blood vessels and the heart may occur, in particular, paroxysms of ventricular tachycardia .
If Fluconazole and Zidovudine , the patient should be monitored by a doctor, as the side effects of Zidovudine may increase.
If treatment with Astemizole , cisapride , Tacrolimus , Rifabutin , or any other drug that is metabolized by the cytochrome P450 system is simultaneously prescribed, the concentration of these drugs in the blood may increase.
The absorption of Fluconazole is not affected by simultaneous administration of Cimetidine or antacids.
Pharmacokinetics
After oral administration, fluconazole is well absorbed; food intake does not affect the rate of absorption of fluconazole, its bioavailability is 90%.
The time to reach maximum concentration after oral administration of 150 mg of the drug on an empty stomach is 0.5–1.5 hours, Cmax is 90% of the plasma concentration when administered intravenously at a dose of 2.5–3.5 mg/l. T1/2 of fluconazole is 30 hours. Communication with plasma proteins is 11–12%. Plasma concentration is directly dependent on dose. A 90% level of equilibrium concentration is achieved by the 4th–5th day of treatment with the drug (when taken once a day).
Administration of a loading dose (on the first day), 2 times higher than the usual daily dose, allows one to achieve a concentration level corresponding to 90% of the equilibrium concentration by the second day.
Fluconazole penetrates well into all biological fluids of the body. Concentrations of the active substance in breast milk, joint fluid, saliva, sputum and peritoneal fluid are similar to its levels in plasma. Constant values in vaginal secretions are achieved 8 hours after oral administration and are maintained at this level for at least 24 hours. Fluconazole penetrates well into the cerebrospinal fluid (CSF) - with fungal meningitis, the concentration in the CSF is about 85% of its level in plasma. In sweat fluid, epidermis and stratum corneum (selective accumulation) concentrations exceeding serum levels are achieved. After oral administration of 150 mg on the 7th day, the concentration in the stratum corneum of the skin is 23.4 mcg/g, and 1 week after taking the second dose - 7.1 mcg/g; concentration in nails after 4 months of use at a dose of 150 mg once a week is 4.05 mcg/g in healthy and 1.8 mcg/g in affected nails. The volume of distribution approaches the total water content of the body.
It is an inhibitor of the CYP2C9 isoenzyme in the liver. It is excreted primarily by the kidneys (80% unchanged, 11% in the form of metabolites). Fluconazole clearance is proportional to creatinine clearance. No fluconazole metabolites were detected in peripheral blood.
The pharmacokinetics of fluconazole depends significantly on the functional state of the kidneys, and there is an inverse relationship between the half-life and creatinine clearance. After hemodialysis for 3 hours, the concentration of fluconazole in plasma decreases by 50%.
special instructions
If liver dysfunction is observed during treatment, constant monitoring by a physician is important. If signs of liver damage are observed, the medication should be discontinued.
When using the medicine topically for men and women, it should be taken into account that people with AIDS are more likely to develop a variety of skin reactions.
It is necessary to take into account not only how long it takes for Fluconazole to act, but also the fact that if treatment is stopped prematurely, relapses may develop. Therefore, it is important to completely complete the prescribed treatment regimen. It is important to take this into account when using Fluconazole for nail fungus, since reviews for nail fungus indicate that if treatment is stopped prematurely, a relapse of the disease may occur.
Many patients have a question about whether Fluconazole is an antibiotic or not? Please note that this is an antifungal agent, not an antibiotic.
Whether men can take this drug depends on the diagnosis. Fluconazole for men is prescribed for fungal infections; it must be taken exactly as prescribed.
Special instructions for the use of the drug Fluconazole
Patients whose liver function tests are impaired during treatment with fluconazole should be under medical supervision. If clinical signs of liver damage appear, fluconazole should be discontinued. People with AIDS are more likely to develop severe skin reactions when taking many drugs. If a rash, possibly caused by the use of fluconazole, appears in a patient receiving treatment for a superficial fungal infection, the drug should be discontinued. If a rash appears in patients with invasive/systemic fungal infections, their condition should be monitored; if bullous lesions or erythema multiforme develop, fluconazole should be discontinued. The use of fluconazole should be avoided in pregnant women, except in cases of severe and potentially life-threatening fungal infections when the expected benefit to the woman outweighs the potential risk to the fetus. Fluconazole is detected in breast milk at the same concentration as in the blood, so its use during breastfeeding is not recommended.
Fluconazole analogs
Level 4 ATC code matches:
Medoflucon
Vfend
Itracon
Mikosist
Irunin
Mikomax
Orungal
Mycoflucan
Sporagal
Orungamin
Flucostat
Difluzol
Rumicosis
Futsis
Vero-Fluconazole
Kandizol
Kanditral
Itraconazole
Diflazon
Fluconazole analogues are products with a similar active ingredient. The price of analogues depends on the manufacturer and the form of release of the drug. There are a number of analogues of this drug:
- Diflazon
- Diflucan
- Vero-Fluconazole
- Mikomax
- Flucostat
Which is better: Fluconazole or Diflucan?
Often patients compare two drugs with antifungal action - Fluconazole and Diflucan . What is the difference between these medicines? Both drugs are based on the active substance fluconazole. Diflucan is available in tablets of 50 mg, 100 mg, 150 mg, and other forms. But the price of Diflucan is much higher.
Flucostat or Fluconazole - which is better?
Speaking about how Flucostat from Fluconazole, it should be noted that both drugs contain the same active substance. Flucostat is a more expensive medicine. What is the difference between these medications, and which one is best prescribed in a particular case, is determined by a specialist. As a rule, Fluconazole is more often prescribed when prophylaxis is necessary for cancer patients after radiation and chemotherapy.
Fluconazole or Nystatin - which is better?
Nystatin is an antifungal drug, an antibiotic, active against candida bacteria. Under the influence of Nystatin, the permeability of the membrane of fungal cells is disrupted, which contributes to disruption of their growth and reproduction. Which drug is preferred in a particular case depends on the diagnosis and the doctor’s prescription.
Seborrheic dermatitis. Terminology
Seborrheic dermatitis
- a chronic inflammatory skin disease associated with an increase in the quantity and change in the quality of sebum, as well as with the influence of skin microflora.
The composition of sebum includes glycerides (more than 40%), free fatty acids (16%), wax esters (up to 25%) and cholesterol, squalene (12%) and cholesterol. Triglycerides in sebum are broken down into free fatty acids by bacteria. Some of them form volatile fatty acids that impart odor to the skin. Sebum itself has no odor.
The wide prevalence and constant increase in incidence determines various approaches to treatment, the main goal of which is to achieve a long-term positive result.
Manifestation of seborrheic dermatitis:
1) thickening of the stratum corneum, peeling;
2) oily sheen, seborrhea, sebostasis (stagnation of sebaceous secretion at the mouth of the hair follicle);
3) inflammation of the skin;
4) itching.
Seborrheic dermatitis affects those areas of the scalp and body where the sebaceous glands are most developed:
- scalp,
- anterior chest area and interscapular area,
- area of the ears,
- forehead,
- nasolabial triangle.
When the skin of the scalp is affected, thinning and thinning of the hair is observed. In severe cases, seborrheic dermatitis can have the character of a widespread exfoliative process up to erythroderma.
| Dandruff = seborrheic dermatitis | Brightness of blood vessels - inflammation |
Reviews about Fluconazole
Due to the high fungicidal activity of this drug, patient reviews and doctors' reviews of Fluconazole are mostly positive. Patients, leaving reviews about Fluconazole Teva, as well as reviews about Fluconazole Stada on the forums, write that the drug helps to quickly and effectively eliminate the symptoms of fungal diseases. Users mention that the tablets are relatively inexpensive, but at the same time they allow you to completely get rid of nail fungus and other unpleasant diseases. In some cases, it is enough to take Fluconazole 150 mg once to completely overcome the symptoms of the disease.
Very often, women write positive reviews about Fluconazole for thrush . It is noted that the medicine not only relieves thrush, but also helps prevent relapses of the disease.
Fluconazole price, where to buy
The price of Fluconazole tablets depends on the packaging and manufacturer. You can buy Fluconazole in Moscow at prices ranging from 40 to 140 rubles. Capsules 150 mg (1 piece in a package) can be purchased for 140 rubles. Capsules 50 mg can be purchased for 60 rubles (pack of 7 pieces)
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Fluconazole-Obl caps.
150 mg 2 pcs. JSC Alium 72 rub. order - Fluconazole-Obl caps. 150 mg 1 pc. JSC Obolenskoe farm. company
39 RUR order
- Fluconazole capsules 150 mg 4 pcs. OzonOzon LLC/Ozone Pharm LLC
101 rub. order
- Fluconazole capsules 150 mg 2 pcs. Ozon LLC
51 RUR order
- Fluconazole capsules 150 mg 1 pc. KanonpharmaZAO Kanonpharma Production
45 rub. order
Pharmacy Dialogue
- Fluconazole (caps. 150 mg No. 2) Ozon LLC
47 RUR order
- Fluconazole-Teva (caps. 50 mg No. 7)Teva Pharmaceutical Works Private Co.
RUB 286 order
- Fluconazole-Teva capsules 50 mg No. 7Teva
280 rub. order
- Fluconazole Stada (caps. 150 mg No. 1) Hemofarm LLC
65 rub. order
- Fluconazole-OVL capsules 150 mg No. 2Obolenskoye pharmaceutical pred.
66 RUR order
show more
Pharmacy24
- Fluconazole-Darnitsa 0.15g N2 capsules PrAT" Pharmaceutical company "Darnitsa", Ukraine
28 UAH. order - Fluconazole-KR 50 mg No. 7 capsules PAT"Khimpharmzavod"Chervona Zirka", Kharkov, Ukraine
15 UAH order
- Fluconazole-Darnitsa 150 mg No. 3 capsules PrAT" Pharmaceutical company "Darnitsa", Ukraine
40 UAH order
- Fluconazole 200 mg 100 ml No. 1 solution Eurolife Healthcare Pvt. Ltd., India
83 UAH order
- Fluconazole 100 mg N10 tablets PrAT "Technolog", Uman, Cherkasy region, Ukraine
32 UAH order
PaniPharmacy
- FLUCONAZOL capsule Fluconazole capsules 0.15g No. 2 Ukraine, Zdorovye LLC
33 UAH order
- Fluconazole caps. 150mg №2
31 UAH order
- FLUCONAZOL tablets Fluconazole tablets 150 mg No. 2 Ukraine, Tekhnolog ChAO
29 UAH order
- FLUCONAZOLE capsule Fluconazole forte caps. 200 mg No. 2 Ukraine, Health LLC
47 UAH order
- FLUCONAZOL capsule Fluconazole capsules 0.05g No. 10 Ukraine, Darnitsa ChAO
28 UAH order
show more
Composition and release form
| Capsules | 1 caps. |
| fluconazole | 50 mg |
| 150 mg | |
| excipients: lactose monohydrate; pregelatinized starch; colloidal anhydrous silicon dioxide; magnesium stearate; sodium lauryl sulfate capsule shell composition for 50 mg: titanium dioxide E-171; dye “Sunset” yellow E-110; gelatin capsule shell composition for 150 mg: titanium dioxide E-171; dye “Sunset” yellow T-110; dye "Ponceau-4R" E-124; gelatin |
in a blister 7 (50 mg) or 1 (150 mg) pcs.; 1 blister in a cardboard pack.