General information
Psittacosis is an infectious disease of the respiratory system transmitted by birds.
Also used to describe it are the following names: psittacosis, parrot fever, respiratory chlamydia. The disease is relatively rare. According to medical statistics, about 10 cases of psittacosis are recorded in the United States annually. Most cases are caused by contact with sick pet birds - cockatiels, macaws and other parrots.
The causative agent of psittacosis is the specific bacterium Chlamydia psittaci. It can be carried by over 150 species of various ornamental, agricultural and wild birds, including: parrots, canaries, ducks, chickens, turkeys, crows and pigeons.
Chlamydia psittaci. Photo: PHIL CDC
There are also other types of chlamydia that cause damage to the lungs (C. pneumoniae) and other organs and systems in humans (C. trachomatis), for example, the genitourinary system, joints, eyes, etc.
Medicines
Photo: zagranmaster.ru
Macrolides . Drugs of this group are able to penetrate into cells and create a high concentration there. Since psittacosis chlamydia is an intracellular pathogen, the use of drugs that have the above properties is effective. Macrolides have a low toxic effect, there are no cross-allergic reactions with Beta-lactam antibiotics (penicillins, cephalosporins, carbapenems, monobactams). This means that the likelihood of allergic reactions is extremely low. Macrolides do not cause destruction of bacteria, which prevents the release of intracellular toxins. Approved for use by children.
Fluoroquinolones . Synthetic antimicrobial drugs. There are forms for oral administration and parenteral administration (intravenously). Fluoroquinolones are capable of acting on both extracellular and intracellular microorganisms (including Chlamydia psittaci). Drugs of this group create high concentrations in the blood and penetrate well into various organ systems. The most common side effects are allergic reactions, vomiting, nausea, diarrhea, and insomnia. Fluoroquinolones disrupt the development of cartilage tissue, therefore quinolone derivatives are contraindicated for use in children under 18 years of age, pregnant and nursing mothers.
Tetracyclines have a wide spectrum of action against microorganisms, which include chlamydia. Able to penetrate and accumulate inside cells. Tetracyclines act bacteriostatically: they inhibit the functioning of the 30s ribosomal subunits and thereby stop the synthesis of vital bacterial proteins. Tetracyclines are divided into two groups according to the duration of their antibacterial action: short-acting tetracyclines (tetracycline, oxytetracycline) and long-acting tetracyclines (methacycline, doxycycline). The drugs of the first group act on bacteria for 6-8 hours, they are prescribed 3-4 times a day. The drugs of the second group retain their antibacterial effect for 12-24 hours, so it is enough to take them 1-2 times a day.
The most common side effects are allergic reactions (such as urticaria), tooth staining, and dyspeptic reactions from the gastrointestinal tract. Teeth discoloration occurs due to the ability of tetracyclines to bind to calcium ions and deposit in bones and teeth, giving them a gray color. Tetracyclines are not recommended for use in children under 12 years of age; they are contraindicated during pregnancy and breastfeeding. Tetracycline drugs have high hepatotoxicity, so taking tetracyclines is contraindicated in patients with liver diseases.
Causes of psittacosis
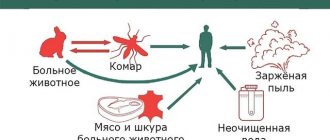
The leading cause of human infection is contact with sick birds. In this case, chlamydia can enter the human body in several ways. One of the most common is inhaling dust particles containing bird urine or feces contaminated with the bacteria. For example, when cleaning a cage or staying in a dovecote for a long time (Fig. 1).
Infection is also possible through direct interaction with a bird, its feathers, eggs, and so on. Examples: stroking a parrot, hand-feeding pigeons, biting, or even simple contact with a bird's beak. In this case, an important point is the contact of dirty hands with a person’s mouth and nose or a direct “kiss” of the bird on the beak.
Figure 1. How you can get psittacosis. Source: MedPortal
In rare cases, you can become infected from another sick person through close contact by inhaling chlamydia, which is released when you cough or sneeze.
Despite the fact that eating meat or eggs of sick birds is also a likely route of contracting psittacosis, there is no evidence of such a route of spread of the disease.
Who is at risk?
The main risk group is formed by people who directly interact with birds:
- employees of veterinary clinics, pet stores and zoos,
- poultry farm workers,
- breeders,
- people involved in breeding poultry at home,
- owners of parrots and other ornamental birds living in cages.
Photo: anuta23 / freepik.com
Another risk group includes people with weakened immune systems, which increases susceptibility to chlamydia. A decrease in the body's defenses may be due to: HIV infection and AIDS, malignant tumors and their treatment (chemotherapy, radiation therapy), long-term use of glucocorticosteroids (for example, in the treatment of autoimmune diseases such as rheumatoid arthritis), as well as chronic diseases that are difficult to treat (severe heart failure, chronic pancreatitis).
Symptoms of psittacosis
Most people experience symptoms within 5 to 14 days of exposure to a sick bird. At the same time, signs of psittacosis can appear faster, just 2-3 days after chlamydia enters the body, or later - within 19 days.
The most typical manifestations of parrot fever:
- Increased body temperature to 39-40°C with chills.
- Pain and sensation of “soreness” in the throat.
- Runny nose, accompanied by nasal congestion and a moderate amount of mucous discharge.
- Dry cough, in some cases accompanied by expectoration of a small amount of sputum.
- Pain and aching sensation in joints and muscles.
- Nausea and vomiting.
- Diarrhea.
- Diffuse chest pain.
- General weakness, excessive fatigue, malaise.
- Nosebleeds.
- Conjunctivitis: redness of the mucous membrane of the eyes, increased lacrimation, sensitivity to light.
Folk remedies
Photo: krrot.net
In the absence of suitable antibacterial therapy, psittacosis is dangerous due to possible complications: without treatment, chlamydia spreads to other organ systems and causes their degenerative lesions. If similar symptoms appear, or if you come into contact with sick or wild birds, you should seek qualified medical help. After drug treatment, additional therapy with traditional medicine is possible. The use of folk remedies is permissible only after approval by the attending physician.
When treating psittacosis with folk remedies, you can relieve intoxication syndrome and stimulate the immune system with a large amount of vitamins. The following remedies can help in the treatment of psittacosis:
- Viburnum decoction . To prepare it, you need to take 50 g of berries or 100 g of viburnum leaves, add 1 liter of water and boil for about an hour. Then, together with the berries and leaves, the broth is infused in a thermos for 8 - 10 hours, filtered. An adult should drink at least 1 liter of drink per day.
- Rose hip decoction . To prepare a decoction, add 50 g of rose hips to 1 liter of water and boil for 3 hours. After boiling, infuse in a warm place, after 5 hours bring to a boil again and add 50 g of honey. You need to consume the resulting decoction 250 ml 2 times a day. Before use you need to strain.
- Herbal collection . To prepare the mixture, you should take equal quantities of chamomile petals, lungwort, oregano, plantain leaves, rose hips, and licorice root. They are crushed, then 2 tablespoons of the prepared mixture are poured into 500 ml of water and boiled for 10 minutes. After boiling, the broth is infused in a warm place for at least 2 hours. You need to take the resulting drink after filtering 1/3 glass three times a day.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Diagnostics
An infectious diseases specialist deals with the diagnosis and treatment of ornithosis in humans, if necessary, together with a therapist or pulmonologist. One of the key points when examining a patient is interviewing and identifying previous contact with birds, as well as his complaints and objective changes in health status. The final diagnosis is established upon receipt of the results of laboratory and instrumental tests that exclude other infections, for example, salmonellosis, paratyphoid fever, etc.
Laboratory confirmation of the disease is carried out using microscopic and bacteriological analysis of sputum, as well as specific tests:
- immunofluorescence reactions (RIF),
- enzyme immunoassay (ELISA),
- polymerase chain reaction (PCR), etc.
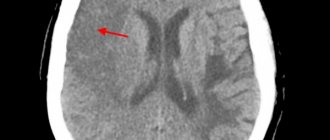
Lung damage (pneumonia) due to psittacosis is detected using chest x-ray, which, if necessary, is supplemented by computed tomography (CT).
Medical reference books
Psittacosis
ICD-10: A70
Ornithosis
– an acute infectious disease characterized by symptoms of intoxication, primary damage to the lungs, nervous system and hepatolienal syndrome.
Relevance. Historical data
The disease was first described by T. Jurgensen under the name atypical pneumonia (1876). In 1879, D. Ritter established its connection with infection from parrots. In 1892, an epidemic of severe pulmonary disease was observed in Paris: the source of infection were parrots imported from Buenos Aires. At the same time, the infection was named psittacosis (from psittakos - parrot). Later, when it was established that the reservoir and source of the pathogen were various species of wild synatropic, ornamental and domestic birds, the disease began to be called ornithosis (from the word ornis - bird). In a special study conducted in the 70s of the last century in various countries (France, USA, Germany, Holland, USSR), it was found that 10-20% of acute pneumonia have psittacosis etiology.
Etiology
Pathogen
– Chlamydia psittaci, belongs to the genus Chlamydia, family Chlamydiaceae. Chlamydia occupy an intermediate position between viruses and rickettsia, have a coccoid shape, a diameter of 0.30-0.45 microns and are obligate intracellular parasites. They contain DNA and RNA and have a complex development cycle that ends in 24-48 hours. They are cultivated on chicken embryos, as well as by infecting experimental animals. Unlike viruses, chlamydia is sensitive to some antibiotics (tetracyclines, chloramphenicol, erythromycin). Resistant to freezing, inactivated by heating and under the influence of various disinfectants.
Epidemiology
Reservoir and sources of infection
– domestic and wild birds.
Currently, the causative agent of psittacosis has been isolated in more than 150 species of birds, which causes the widespread distribution of this disease. A sick person does not pose an epidemiological danger. The most susceptible to the disease are people who are in constant contact with birds: workers in poultry farms, meat processing plants, etc. However, occupational diseases account for only 2-5% of the total number of cases. The transmission mechanism
of psittacosis is aerosol, the transmission route is airborne dust. A fecal-oral mechanism with foodborne transmission is possible (up to 10% of cases). Psittacosis is characterized by spring and autumn seasonality. Sporadic diseases can occur throughout the year. People's natural sensitivity is high. Post-infectious immunity is short-lived, repeated cases of the disease are possible with an interval of up to 2 years.
Pathogenesis
The entry point for infection is the mucous membrane of the upper respiratory tract. The pathogen penetrates the epithelium of small bronchi and bronchioles, and subsequently into the interstitial tissue, where it multiplies and accumulates. When the affected cells are destroyed, their decay products, as well as chlamydia, bacterial toxins and waste products enter the blood. Pneumonia develops against the background of catarrhal tracheobronchitis and hyperplasia of the peribronchial lymph nodes. Chlamydia is capable of long-term intracellular localization, which makes the disease recurrent.
Less commonly, the mucous membrane of the digestive tract – the small intestine – serves as the gateway to infection. In this case, the pathogen also enters the blood, causing intoxication and affecting a number of organs and systems, but secondary hematogenous pneumonia does not occur. As a result, the disease proceeds atypically - without damage to the lungs. In some cases, chlamydia penetrates the central nervous system and leads to the development of serous meningitis.
During pathological examination
They show signs of catarrhal tracheobronchitis and hyperplasia of the peribronchial lymph nodes, in the lungs there are areas of infiltration, interstitial changes and atelectasis. Morphologically, fluid exudation into the alveoli is detected. The exudate contains mononuclear cells and deflated epithelial cells. A significant number of mononuclear elements are found in the alveolar and interstitial tissue. When a secondary infection occurs, purulent tracheobronchitis and large-focal or lobar pneumonia develop. In other internal organs, plethora, edema, dystrophic changes, proliferation of cells of the macrophage system are observed, and sometimes focal necrosis occurs.
Clinical picture
The incubation period for psittacosis lasts from 5 to 30 days, most often 8-12 days. There is no generally accepted classification of psittacosis. The most complete is the clinical classification of A.P. Kazantseva (1973). A. Acute psittacosis: 1) typical (pneumonic) forms: mild, moderate, severe; 2) atypical forms: a) meningopneumonia; b) psittacosis meningitis; c) ornithosis without lung damage; 3) asymptomatic (inapparent) form. B. Chronic ornithosis: 1) chronic ornithosis pneumonia; 2) chronic ornithosis without lung damage. B. Post-thornitis nonspecific chronic pneumonia.
Acute ornithosis Pneumonic form of ornithosis The course of the disease can be divided into the following periods: - incubation, which often lasts 8-12 days; - initial (before changes appear in the lungs) lasting 2-4 days; - peak period lasting 6-12 days; - a period of convalescence lasting up to 1.5-2 months.
The prodromal period is not expressed. The disease begins acutely, with an increase in temperature to 38-39 °C, often up to 40 °C. Fever is accompanied by chills, increased sweating, muscle and joint pain, headache, insomnia, lethargy, and nausea. The temperature curve is wavy in nature. The duration of fever depends on the severity of the disease and can range from 2 days to 1 month or more. During examination, some patients are found to have conjunctivitis. On the 2-4th day of illness, signs of lung damage appear: dry cough, sometimes stabbing chest pain (in approximately 50% of patients), after 1-3 days a small amount of mucous or mucopurulent sputum begins to be released, sometimes (in 15% of patients patients) mixed with blood.
An objective examination reveals pallor of the skin, absence of pronounced lesions of the upper respiratory tract, bradycardia, decreased blood pressure, and muffled heart sounds. When examining the lungs, percussion changes are quite scanty. Only when the focus of inflammation is localized closer to the periphery of the lungs or when it is massive is a dullness of the percussion sound clearly audible. Auscultation reveals hard breathing, scattered dry rales and, in a limited area, moist fine bubbling rales. Pneumonia is usually unilateral and is detected in the lower lobes. It is interstitial, less often focal or sublobar in nature. X-ray can detect interstitial changes or foci of infiltration, usually located in the lower parts of the lungs, as well as expansion of the pulmonary roots, increased pulmonary pattern, and sometimes enlarged hilar lymph nodes. Sometimes infiltrates are cloud-like in nature. Infiltrative changes disappear by the 15-18th day of illness, and interstitial changes persist until the 23rd and even 35th day of illness. However, in 10-30% of patients, radiographic changes in the lungs may be absent.
Damage to the gastrointestinal tract is manifested by decreased appetite, sometimes complete anorexia, constipation or diarrhea. The tongue is thickened, covered with a gray coating, the edges of the tongue are clean, and teeth marks are visible. By the end of the 1st week, half of the patients have an enlarged liver, and every third one has an enlarged spleen. Resorption of foci of pneumonia occurs slowly, and asthenia persists for a long time. Sometimes complete recovery occurs after 10-15 days; in severe and moderate forms of ornithosis, full recovery occurs only after 2-3 months. In some cases, the disease becomes remitting, with subsequent relapses. Early relapses develop after 2-4 weeks. after the acute phase, late – after 3-4 months. In some patients, ornithosis takes a chronic course. Atypical forms of ornithosis occur like meningopneumonia, ornithosis meningitis and ornithosis infection without lung damage. With meningopneumonia, patients, along with pneumonia, exhibit signs of central nervous system damage in the form of severe headache, vomiting, neck stiffness, and positive Kernig-Brudzinski symptoms.
Ornithosis meningitis
– one of the atypical forms of acute ornithosis, it is rare. It begins acutely with an increase in body temperature and the appearance of symptoms of intoxication. Over the next 2-4 days, meningeal symptoms appear (severe headache, stiff neck, positive Kernig, Brudzinsky, etc. symptoms). There are no changes in the lungs. Psittacosis meningitis is usually serous. In the cerebrospinal fluid, slight pleocytosis and a moderate increase in the amount of protein are detected. There are known cases of ornithosis meningoencephalitis, in which meningeal phenomena are accompanied by focal symptoms, paresis and paralysis. All these forms are extremely rare. Ornithosis without lung damage occurs with moderate fever, sore throat, muscle pain, enlarged liver and spleen. It is observed in 3-5% of patients.
Asymptomatic
(innaparent) form of acute psittacosis is detected only during epidemic outbreaks in the source of infection during laboratory examination. This form of the disease is more often observed in young people with good body reactivity.
Chronic forms of ornithosis.
Develops in 10-15% of patients with acute psittacosis. In the absence of etiotropic therapy or improper treatment of ornithosis pneumonia (sulfonamides, streptomycin, penicillin), recovery does not occur, and the disease becomes chronic, characterized by a sluggish, long-term course with alternating exacerbations and remissions. The disease occurs in the form of chronic pneumonia with symptoms of bronchitis. Body temperature does not exceed 38 degrees, while intoxication remains (weakness, fatigue). The disease can last 3-5 years or more. Chronic psittacosis can occur without lung damage. Manifests itself in the form of a prolonged increase in body temperature not exceeding 38 degrees, symptoms of chronic intoxication, vegetative-vascular disorders, enlarged liver and spleen. May last for years. In some cases, long-term persistence of the pathogen in the body may not manifest itself in any way, causing a latent infection.
Complications
Complications with psittacosis can be caused by layered infection and the pathogen itself. Among them: myocarditis, thrombophlebitis, hepatitis, purulent otitis, neuritis.
Diagnostics
In case of group occupational diseases, the diagnosis of psittacosis is not difficult. The diagnosis is made on the basis of the most important clinical signs of ornithosis: acute onset of the disease, fever, excessive sweating, pulmonary syndrome, damage to the nervous system, liver, and spleen. Epidemiological history greatly facilitates diagnosis. The hemogram determines leukopenia or normocytosis, relative lymphocytosis and aneosinophilia, ESR is increased or normal. The diagnosis of psittacosis is confirmed by laboratory tests. Isolation of the pathogen from blood and sputum is carried out on chicken embryos, tissue cultures or by infecting animals. However, these studies are complex and not always available. The basis is serological methods - RSK and RTGA with reactions in paired sera, as well as ELISA. The diagnostic titer for RSC is 1:16-1:64; for RTGA 1:512 and higher or an increase in antibody titer by 4 times or more when studying paired sera. DNA diagnostics of chlamydia using polymerase chain reaction (PCR) has been developed. For early and retrospective diagnosis of ornithosis, an intradermal test has been proposed. The antigen is injected intradermally in a dose of 0.1 ml into the area of the inner surface of the forearm. The severity of the reaction is assessed by the size of the infiltrate and hyperemia. With psittacosis, the allergy test is positive in almost all patients and can persist for 2-3 years after recovery.
Differential diagnosis
It is carried out with influenza and other acute respiratory diseases, pneumonia of various etiologies, Q fever, mycoplasmosis, infectious mononucleosis, brucellosis, pulmonary tuberculosis, and in the meningeal form of the disease - with serous meningitis of other etiologies.
Treatment
Antibiotics are used as etiotropic drugs. The most effective etiotropic drugs in the treatment of psittacosis and generalized forms of chlamydia are tetracycline (0.3-0.5 g 4 times) or doxycycline (0.2 g once a day) during the entire febrile period and 5-7 days after normalization temperature. The use of azithromycin (0.5 g once a day for 5 days) or erythromycin (0.25 g every 6 hours for 5-10 days from the time body temperature normalizes) is also effective. In severe cases, antibiotics are used parenterally. Long-term antibiotic therapy prevents relapses and the transition of the disease to chronic forms. Premature withdrawal of antibiotics and inadequate therapy contribute to the occurrence of relapses and chronicity of the process. Penicillin, streptomycin and sulfonamides (Biseptol) are not effective for psittacosis. Along with this, detoxification therapy is carried out, including intravenous administration of crystalloid and colloid solutions. In some cases, glucocorticosteroids are indicated. Important components of pathogenetic therapy are oxygen therapy and bronchodilators. Symptomatic remedies are widely used. In the treatment of psittacosis meningitis, in addition, saluretics (furosemide, or Lasix, ethacrynic acid, or uregit) and osmotic diuretics (mannitol, or mannitol) are used for dehydration. In the chronic course of the disease, vitamin therapy, restoratives, and physical therapy (breathing exercises) are recommended. After discharge from the hospital, the convalescent must be under the dispensary supervision of a doctor at the infectious diseases office for 6 months.
Forecast
The prognosis is favorable. With modern treatment methods, the mortality rate is less than 1%. Relapses and chronicity of the process are possible.
Prevention
Combating ornithosis among poultry, regulating the number of pigeons, limiting contact with them. An important point is compliance with veterinary and sanitary rules when importing birds from abroad, transporting and keeping birds in poultry farms and zoos. Sick birds are destroyed and the premises are disinfected. The staff is provided with special clothing and disinfectants. Specific prevention has not been developed.
Treatment of psittacosis
Treatment is based on antibacterial therapy - antibiotics from the group of tetracyclines, macrolides, and fluoroquinolones. The duration of their use, as a rule, is from 10 to 14 days after normalization of body temperature. After receiving the results of a laboratory test of sputum, the antibiotics used may change in accordance with the sensitivity of chlamydia to them. In case of a protracted, chronic course, it is possible to carry out 2-3 courses of antibacterial treatment with an interval of about 7 days.
To combat individual symptoms and manifestations of psittacosis, it is possible to prescribe antipyretic drugs, mucolytics and antitussives, as well as intravenous drip therapy with plasma substitutes. In the presence of concomitant disorders of the immune system, under the supervision of an immunologist, it is possible to use immunomodulators and immunostimulants.
Sources
- Medical microbiology Pozdeev O.K. / Ed. acad. RAMS V.I. Pokrovsky. – M.: GEOTAR-MED, 2002.- 768 p.
- Chronic chlamydial infection as a cause of demyelination and vasculitis of the central nervous system: some aspects of diagnosis / Yu. I. Vainshenker, I. M. Ivchenko1, I. V. Nuralova2, V. A. Tsinzerling, A. V. Sozina, L. B. Kulyashova, L. A. Berezina, O. V. Narvskaya
- Journal of Infectology. Features of the clinical picture of ornithosis and respiratory mycoplasma infection during the 2012 outbreak L.V. Voloshchuk, A.L. Mushkatina, E.G. Rozhkova, P.V. Zarishnyuk, T.L. Tumina, G.L. Dneprovskaya, M.I. Sadikhova
- Bezdenezhnykh I.S. Ornithosis. Epidemiology, clinic. / I.S. Without money. – M.: Medicine, 1959. – 211 p.
- Bilibin A.F. Epidemiology and clinic of ornithosis / A.F. Bilibin // Klin. Medicine. – 1962. – No. 3. – pp. 34-38.
Forecast
As a rule, with timely and correct treatment, complete recovery occurs.
In rare cases, the disease can cause inflammation of various internal organs: the brain and its membranes (encephalitis and meningitis), the liver (hepatitis) and the inner lining of the heart (endocarditis). It is also possible to develop acute respiratory and/or heart failure syndrome.
Fatal complications occur with a frequency of less than 1:100 cases, that is, less than 1% of cases. The main causes are acute respiratory and heart failure, caused by damage to the lungs and heart, respectively.
Prevention
Prevention of psittacosis is aimed at preventing the transmission of chlamydia from birds to humans. It includes the following recommendations:
- Clean your poultry cage daily and ventilate the area in which they are housed.
- Wash your hands regularly after handling the bird, its feathers or eggs.
- Avoid contact with the bird’s beak, including so-called “kisses.”
- Follow all veterinary recommendations and safety rules when working in poultry farms, farms and zoos.
- Buy domestic and ornamental birds only in specialized stores and from trusted breeders. At the same time, immediately after purchasing an animal, you should take it to a veterinarian for examination.
Psittacosis in parrots
If you keep a parrot, you should carefully monitor its health. Psittacosis in birds is easy to recognize; in sick parrots, the eyes and sinuses suffer, and paralysis of the paws may develop (Fig. 2).
Figure 2. Psittacosis in parrots. Source: MedPortal
A sick animal should be isolated from other birds and contact a veterinarian as soon as possible. Psittacosis in parrots, like in humans, is treated with antibiotics (Fig. 3). You can reduce the risk of developing psittacosis in parrots by changing the water on time and regularly cleaning the cages. New birds should be kept in quarantine for some time before being placed with other pets.
Figure 3. Treatment and prevention of psittacosis in parrots. Source: MedPortal
Experts recommend
Faina Nikolaevna Ryabchuk, Ph.D., Associate Professor of the Department of Pediatrics 2 MAPL (St. Petersburg) recommends the drug Bifidum BAG for chlamydial infection to accompany antibiotic therapy and to strengthen local immunity on the mucous membranes for a course of 2-3 weeks. The species composition of bifidobacteria Bifidum BAG is antagonistically active against chlamydial infection. Mandatory time spacing with taking an antibiotic for 3-4 hours.
“It is the film of beneficial lactobacilli and bifidobacteria on the surface of the mucous membranes that protects against the action of pathogens, maintains health, and allows survival.”
Professor K. Rusch (Germany)