Etiology
Hyperthermia is a polyetiological secondary condition. The process of restructuring the work of the thermoregulation center begins with the appearance of pyrogenic substances in the body. They are divided into infectious or exogenous and non-infectious, called endogenous.
Thus, the reasons for the development of hectic fever can be divided into two large groups.
- Infectious, in the form of inflammatory diseases. For example, influenza, tuberculosis, sepsis of the blood or internal organs.
- Non-infectious. These include tissue necrosis, allergies and oncology, blood transfusions, and internal hemorrhages.
Symptoms
The patient is constantly thirsty.
Symptoms of hectic fever can be divided into general and specific. What happens with common:
- body temperature rises;
- heart rate and breathing increase;
- blood pressure drops below normal;
- the patient notes migraine attacks and a feeling of aching muscles and joints;
- the oral mucosa dries out, the patient feels constant thirst;
- daily diuresis is significantly reduced;
- appetite completely disappears.
Particular symptoms depend on the rate of temperature rise. A gradual rise is characterized by:
- redness of the skin;
- moderate chills;
- feeling of heat and stuffiness;
- increased sweating.
A rapid increase in temperature, in turn, is accompanied by symptoms such as:
- pale skin;
- severe and short-term attacks of chills;
- feeling cold;
- blueness of the nail plates.
Causes
LNG can be caused by infectious diseases, the development of an inflammatory or malignant process, or systemic connective tissue diseases.
The most common reasons:
- infectious diseases - malaria, tuberculosis, aspergillosis, herpes, borreliosis, tick-borne encephalitis, abdominal-pelvic abscesses, prostate abscess, cholecystitis, dental infections, endocarditis, osteomyelitis, sinusitis, cytomegalovirus, Epstein-Barr virus, HIV, genitourinary infections, opportunistic infections ;
- autoimmune diseases - inflammatory bowel disease, rheumatoid arthritis, adult Still's disease, polymyalgia rheumatica, Reiter's syndrome, vasculitis, systemic lupus erythematosus, rheumatic fever;
- malignant tumors - renal cell carcinoma, hepatoma, colon cancer, pancreatic cancer, sarcomas, lymphomas, chronic leukemia, metastatic cancer.
Other reasons include:
- drug-induced fever (hypersensitivity reaction to certain medications);
- hepatitis (granulomatous, lupus, alcoholic);
- complications of liver cirrhosis;
- deep vein thrombosis;
- gout;
- Behçet's disease;
- Felty's syndrome;
- sarcoidosis;
- thyroiditis, Crohn's disease, familial periodic fever, cyclic neutropenia (rare).
Types of fever and their characteristics
In official medicine, in addition to the causes of fever, several more criteria are identified that allow classifying this pathological process.
- With a total duration of up to 2 weeks, the body’s reaction is called acute. Up to a month and a half, adjust. Above – chronic.
- According to the temperature level within which it can increase or decrease. 41°C or more is called excessive fever. Around 39-40.9°C high. No more than 38-38.9°C febrile. And from 37 to 37.9°C subfebrile.
- Based on what temperature changes are observed during the day. There are constant, intermittent, laxative, wavy, recurrent, perverted, irregular or debilitating. The last type, which is otherwise called hectic fever, is the most severe and dangerous for the patient. It is characterized by sudden temperature fluctuations of 3°C or more.
Diagnostics
To prescribe the correct course of treatment, hectic fever and its genesis must be accurately diagnosed, since the symptoms may be similar to sunstroke, heatstroke and other fever-like conditions. In addition, patients often try to fake it.
First, blood and urine samples are taken for general analysis. They also take pictures of the patient’s chest using an X-ray machine and perform an ECG. If the data from these research methods is not enough, then more complex ones are resorted to. For example, a CT scan or a biopsy of certain tissues and body fluids.
Stages of fever
In the development of hectic fever, 3 stages can be observed:
- continuous increase in temperature;
- stopping and prolonged consolidation at high values;
- decrease in temperature level.
At the first stage, the body’s thermoregulation center begins to function in a manner similar to situations when the surrounding temperature is low. Cellular oxidative processes increase heat generation. Muscle tone increases and turns into thermogenesis. The skin becomes dry and pale, the upper and lower extremities begin to get cold. Chills and a desire to warm up increase.
An increase in temperature often occurs due to a decrease in heat transfer from the body at this stage. But its growth is also possible along with heat generation, but not simultaneously.
The second stage is established when equilibrium is reached between the formation of heat in the body and its release, but at a temperature level shifted compared to the norm. The subcutaneous vessels dilate, giving it a red tint and heat. The patient's breathing becomes rapid. Thermogenesis and chills disappear. An increase in temperature in the evening and a slight decrease in the morning are noted.
At the last stage, a decrease in the level of pyrogenic substances in the body is recorded. They no longer affect the functioning of the thermoregulation center, and the body strives to increase heat output and reduce its formation due to profuse sweating.
Under such conditions, the temperature can decrease at a critically rapid rate or lytically. The first option is accompanied by disturbances in water-salt balance, hypotension, dehydration and, in severe cases, collapse. The lytic drop in temperature is gradual and does not pose a danger to humans.
Fever in a child: how to bring down the temperature
Why does the temperature rise during illness?
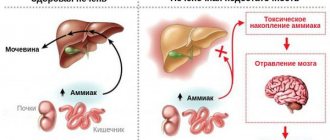
The body has its own “climate control” system, which is responsible for the constancy of body temperature. During inflammation, substances are produced that change the settings of the thermoregulation center, and the temperature begins to be maintained at a higher level. This makes a certain sense: in conditions of elevated temperature, bacteria and viruses feel less comfortable, and the immune system, on the contrary, begins to work more actively. This is a fever - with its help the body fights infection. Fever should be distinguished from heatstroke - there is no protective meaning in it, and the temperature rises due to the fact that the body simply does not have time to cool down (usually due to heat, physical stress and lack of water).
What temperature is considered normal?
Body temperature is very variable and depends on age (the younger the child, the higher his temperature), time of day (usually higher in the evening), physical activity, and also on the method of measurement - thus, the 36.6 ° C familiar to everyone is very arbitrary and There is simply no single standard.
How to measure temperature?
We are accustomed to measuring temperature under the armpit; in many countries, measurements are taken in the mouth or rectum (these indicators are higher). Electronic thermometers are preferable to mercury thermometers - but it must be borne in mind that in order to get an accurate result after the sound signal, you need to leave the thermometer for a few more minutes. Not everyone does this, and therefore the indicators of an electronic thermometer are sometimes unfairly considered to be underestimated. There are also ear and non-contact infrared thermometers, but their readings are not highly accurate.
When should the temperature be lowered?
In itself, high temperatures up to 41 ° C are not life-threatening. The temperature needs to be brought down if the child feels unwell, and the numbers on the thermometer are of secondary importance. If a child has chronic diseases, then it is worth discussing this issue with the attending physician in advance, and if a high temperature appears in a baby under three months old, this is a reason to call an ambulance. In all other cases, you should focus on the child’s well-being: if he is lethargic, complains of a headache and general malaise already at 37.9 ° C, you have the right to give an antipyretic drug. And if a child can barely sit still with a thermometer, you should not run after him with medicine, even if the thermometer reads almost 39 °C.
Many people think that the higher the child’s temperature, the more dangerous and severe the infection he faces, but this is not entirely true. The immune system has not yet fully formed and attacks any infections with all its might. This is why a child’s temperature can rise significantly with a banal ARVI, while this usually does not happen in adults.
How to lower the temperature correctly?
First of all, you need to make sure that the child drinks a lot and does not overheat additionally - to do this, you need to remove excess clothes and blankets from him and open the window slightly so that the room is not stuffy. You can wipe with warm (not cold) water - the cooling effect is achieved due to the evaporation of water from the surface of the skin. And finally, if you feel unwell, you can give an antipyretic drug - it will return the thermoregulation center to maintaining the original, normal temperature. The most effective method is to give an antipyretic, and after half an hour, wipe the child with water.
The only two medications allowed for children with fever are ibuprofen and paracetamol (acetaminophen). They are available in the form of suppositories and syrups under different trade names.
The dose is calculated by weight, not by age of the child.
Ibuprofen: single dose - 10 mg per 1 kg of child's weight. Can be given every 6 hours no more than 4 times a day.
Paracetamol: single dose - 10-15 mg per 1 kg of child's weight. Can be given every 4-6 hours, but no more than 4 times a day.
The drugs begin to act 30-60 minutes after administration and reduce the temperature by about 1-2 °C (and not up to 36.6 °C), while improving well-being. If more than 3 hours have passed after taking one of them, and there is no effect, you can change the drug and start using another, but do not alternate them each time.
When to call an ambulance?
Fever itself is not a reason to panic. It is better to seek emergency medical help if there are so-called red flags:
- disturbance of consciousness, convulsions;
- dehydration (lack of urination, tears when crying, dry mucous membranes);
- breathing problems (sharp increase in frequency, difficulty breathing, appearance of uncharacteristic sounds);
- the appearance of a rash that does not fade when pressed (if you press a glass glass tightly to the site of the rash, the rash remains bright);
- severe headache even after taking antipyretics;
- incessant vomiting;
- persistence of poor health and fever of more than 40 ° C after taking antipyretics;
- acute abdominal pain;
- age up to 3 months.
All other situations most likely do not require emergency assistance. So, if ear pain appears, you can give your child a painkiller (the same ibuprofen) and calmly wait for the pediatrician. But if you think that something is wrong with your child and he is behaving unusually, you should take your child to the doctor as soon as possible.
What not to do?
It is strictly forbidden to use aspirin as an antipyretic in children due to the risk of a fatal complication - Reye's syndrome. In addition, you cannot:
- give analgin and soluble combination drugs “against colds” (like Theraflu) as an antipyretic;
- rub with alcohol and vinegar due to the risk of poisoning (the permeability of children's skin is higher than that of adults);
- wrap the child up and wait for him to sweat;
- use mustard plasters due to the risk of burns;
- take antibiotics on the third day of fever. There are many viral infections in which the temperature lasts longer than 5 days. If the fever persists, you need to see a pediatrician rather than take antibiotics.
Don’t just take your child’s temperature, just in case he’s healthy. If something is wrong with your child, you will notice it without a thermometer. Believe me, it is very easy to see that a healthy child’s temperature is above 37 °C. Coping with your anxiety and making sure that this temperature is normal for him is much more difficult.
And finally, there is no need to panic. Fever is an everyday thing. A sick child needs a calm mother who will give him something to drink if necessary, give him medicine, wipe him off with a damp towel and just be there.
Treatment
Treatment for hectic fever should serve two purposes. Support the functioning of internal organ systems, primarily the respiratory, cardiac and excretory systems. And also fight hyperthermia. To do this, you can use not only medications, but also physical effects on the body.
The patient is freed from clothes and put to bed, his head slightly raised. Cold compresses from moistened bandages or ice packs are applied to the head and wrists. The body is wiped with a solution of vinegar at a concentration of 3%, alcohol or simply cool water. Additionally, you can use a fan or air conditioner for cooling.
In a hospital setting, the patient undergoes gastric lavage and water enemas. All infusion solutions for intravenous use are also refrigerated. At this stage, it is important to ensure that the body temperature reaches a maximum of 37.5 ° C, since under the influence of the above measures the body itself will continue to reduce it.
Antipyretic and antiallergic medications are prescribed in the form of intramuscular injections. This may be brufen and its analogues, acetylsalicylic acid and solutions of analgin with diphenhydramine or suprastin. For increased excitability, aminazine or lytic mixtures are prescribed.
In case of respiratory failure or cardiac arrest, resuscitation measures are carried out. If there is a threat of cerebral edema, then magnesium sulfate is used. For hypotension, prednisolone is used, and seduxen is used to combat seizures.