A group of diseases caused by streptococci with infectious lesions of the skin is called streptoderma. Purulent inflammatory processes begin to develop in different layers of the skin, caused by pyogenic bacteria. Without timely treatment, the patient may develop serious complications that pose a serious threat to health.
Children are most often exposed to streptococcal skin diseases. At an early age, the body’s immunity is still weak and not as well developed as in adult patients. A minor abrasion or scratch will be enough for bacteria to enter the child’s delicate skin.
Classification of streptoderma
The disease is usually divided into several types, depending on the depth of the inflammatory process.
The surface type includes:
- paronychia;
- inflammation of an erysipelas nature;
- toxic shock caused by streptococcal syndrome;
- papulo-erosive and intertriginous streptoderma;
- crevice impetigo;
- acute diffuse disease.
With a deep form of development of pathology, cellulite and vulgar ecthyma are distinguished. Clinical forms are divided into several types, depending on the type of pathogen.
There are three main stages in total:
- Initial
. Characterized by small rashes with pus. Within 24 hours, red spots turn into small blisters with a purulent center. - Non-bullous.
The next stage occurs after severe damage to the skin; after the blisters burst, the formation of streptococcal ecthyma begins. Small ulcers appear at the site of acne, and after a few days they dry out completely. - Chronic.
The last form of the disease is often observed with improper therapy. When the body's protective properties decrease, regular rashes occur, causing discomfort and acute pain.
If you suspect the development of streptoderma, an urgent visit to a dermatologist is required. A timely examination helps to prescribe an effective course of treatment and minimize the possibility of subsequent complications or progression of the disease to the next stage.
What can streptoderma be confused with?
Pyoderma
With pyoderma, the sebaceous and sweat glands are damaged. The rash appears in certain areas of the skin - parts of the body, scalp.
Herpetic rash
Herpes is characterized by the presence of blisters with constant inflammatory processes. They burst and provoke development.
Thrush or candidiasis
Candidiasis is characterized by erythematous papules or reddened, wet plaques. In the pathology under consideration, the lesion, as a rule, occurs in the mucous membranes or fold areas.
Manifestations of allergies
An allergic rash continues to occur as long as the influence is the causative agent of the allergy.
Causes of streptoderma
The skin of any person is always covered with a large number of opportunistic bacteria that do not pose a threat to health. This position, on the contrary, strengthens the skin’s ability to fight pathogens, which include streptococci.
As long as the immune system is not weakened, the skin acts as a reliable barrier and bacteria are not capable of causing harm. But when the protective properties of the body are weakened, there is a threat of the formation of streptoderma.
Decreased immunity may occur for the following reasons:
- the presence of other chronic pathologies;
- regular stress, poor sleep, excessive physical activity;
- sudden hypothermia or, conversely, overheating of the body;
- helminthiasis;
- previously suffered viral diseases.
Failure to maintain personal hygiene or mechanical damage to the skin can also cause the formation of an infectious disease.
Risk factors are:
- poor working conditions, such as being too hot, humid or stuffy;
- changes in hormonal levels;
- being overweight;
- poor nutrition;
- diabetes and other endocrine diseases.
Sometimes the causative agent can be low-quality personal care products or cosmetics. Streptoderma can contribute to the development of other scratching diseases due to severe skin itching.
What it is?
Pyoderma is a pustular skin disease caused by pyogenic bacteria, the main of which are staphylococci and streptococci, and a little less frequently - Proteus vulgaris and Pseudomonas aeruginosa. Pyoderma is more common in childhood and among workers in certain types of industry and agriculture.
An increase in incidence is observed in the autumn-winter period - the cold and damp season. The humid climate of hot countries is the reason for a large number of patients with mycoses and pustular skin diseases.
Ways of infection of streptoderma
Regardless of the form in which the disease occurs, its infectious nature implies rapid transmission.
Infection can occur in one of the following ways:
- close contact with an infected patient, such as shaking hands, kissing or hugging;
- received injury to the skin in the form of an insect bite, burn or cut;
- contact with a surface on which there is a trace of contact with a sick patient, this could be door handles in public places, handrails in transport, cutlery or bath accessories;
- by airborne droplets from sneezing or coughing.
When a patient is in a large group, an outbreak of the disease can very quickly lead to a quarantine regime. Therefore, when primary signs of suspected streptoderma appear, the person must immediately be isolated from others. The incubation period can last up to two weeks. At the same time, people who were in direct contact with the sick patient are being monitored.
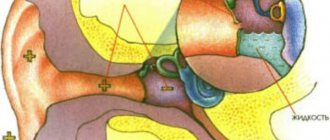
Superficial bacterial skin infections
Folliculitis
- inflammation of the hair follicle: abscess around the hair, redness of the surrounding area.
Pemphigus of newborns
- a severe contagious disease when inflammatory blisters cover the baby’s entire body, forming crusts and ulcers.
Impetigo
- against the background of redness, painless blisters with cloudy contents appear. Then the blisters shrink to yellowish crusts, leaving erosions.
Impetigo often occurs in children and young women. Localization: face, under the hair of the head, limbs. When staphylococcus attaches, the crusts become greenish or bloody. The disease spreads quickly in communities. If you suspect it, you need to isolate the child and bandage the wound.
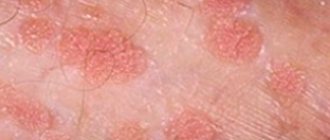
Symptoms of streptoderma
The disease does not appear immediately. In the first seven days, characteristic symptoms may be absent, and the first signs appear only in the second week:
- rashes appear that form in groups;
- oval-shaped spots with a reddish tint, covered with small scales, appear on the skin;
- in place of the spots, small pimples very quickly appear, similar to bubbles, filled with a cloudy white or yellow liquid;
- within 24 hours, pimples burst, and in their place a dried crust forms;
- after some time, the crusts peel off, and red skin becomes visible underneath;
- The affected areas of the skin return to normal over time.
Purulent lesions of an infectious nature are most often localized on the face and arms, less often on the legs, back and buttocks. Symptoms may vary, depending on the stage of the disease and its form. An important role is played by the patient’s immunity and the presence of other chronic pathologies that contribute to the weakening of the body’s protective properties.
General weakness and drowsiness may be added to the listed symptoms. Often the rashes are accompanied by nausea and aching pain in the muscles. The temperature may rise slightly and unbearable itching may appear in the areas where acne is located.
Diagnosis of streptoderma
If characteristic signs of a skin disease appear, an immediate visit to our Your Health clinic in Moscow is required.
At an appointment with a dermatologist, an initial examination will be carried out followed by the appointment of the necessary diagnostic measures, the purpose of which is to confirm the preliminary diagnosis:
- taking an anamnesis, during which the doctor will ask leading questions about the onset of symptoms, bad habits and other chronic pathologies;
- a survey will be conducted about the place of work and social and living conditions will be clarified;
- at the next stage, an examination of the affected areas of the skin is carried out, with an assessment of the localization, degree of prevalence and type of rash;
- referral for bacteriological culture to collect the contents of papules and ulcers;
- The test reveals the sensitivity of bacteria to various types of medications, which facilitates the correct selection of antibiotics for therapy.
Depending on the results of the study, additional tests may be prescribed in the form of biochemical blood sampling, determining the presence of syphilis and thyroid hormones. General analysis of urine and feces for worms.
Features of facial skin infections
The blood supply to the organs of the head, face, and membranes of the brain is closely connected. Incorrect treatment and squeezing of pimples is dangerous due to the spread of bacteria through the blood and lymph. You can achieve an increase in the area of the affected area, such dangerous complications as meningitis, abscesses and phlegmon, and inflammation of the eyes.
Before deciding on cosmetic procedures - cleansing, peeling, mesotherapy - undergo an examination by a dermatologist to determine the cause of the pustular rash and receive treatment.
Streptoderma in children
According to statistics, children are much more likely to develop streptoderma than adult patients. This is due to more delicate skin and not fully strengthened immunity.
The disease in young patients occurs with some distinctive features:
- body temperature rises;
- most often papulo-erosive streptoderma and streptococcal impetigo are determined by type;
- lymph nodes increase in size;
- general intoxication of the body begins;
- The localization of rashes is most often observed on the thighs, scrotum and buttocks.
The presence of blue-red pimples with a liquid center indicates papulo-erosive streptoderma. The skin around the rash becomes very inflamed and red. When the bubbles burst, weeping crusts form.
Streptococcal impetigo is one of the most contagious skin infections. If one of the children in a kindergarten or school class gets sick, all the other children who are in contact with the sick child will most likely become infected.
Purulent rashes appear on the wings of the nose, mouth and face. The disease may be accompanied by a complication in the form of inflammation of the lymph nodes.
Pathology in children is determined by microscopy of smears taken from infected areas of the skin and subsequent bacteriological analysis. Based on the results obtained, therapy is prescribed. The selection of medications is done very carefully; the doctor in our clinic takes into account the general condition and individual characteristics of the child.
If a child has an infectious skin lesion, parents should follow the recommendations given by the dermatologist:
- limit contact with water, which contributes to the development of infection;
- explain to the child that wounds should not be scratched;
- exclude flour dishes and sweets from the diet;
- use underwear made from natural fabrics and change it every day.
Until complete recovery, the child is prohibited from being allowed into the children's group. If you follow all the doctor’s instructions, the course of treatment will go quickly and without serious complications.
Therapy and drugs
Throughout the spread of the disease, basic hygiene rules should be observed: in the first days, it is forbidden to take baths and wet impetigo, and it is forbidden to comb the affected areas.
Therapy for this disease is aimed at destroying the pathogen and strengthening the protective functions of the immune system. As a complex treatment, antibacterial drugs of the category of cephalosporins, macrolides and penicillins are prescribed. If you have bullous streptoderma, you should stop taking medications. As an immunocorrective treatment, the drugs “Likopida”, “Amiksin” and their analogues are effective. Treatment with drugs for . Restoration of microflora in the intestines occurs with the help of probiotics and prebiotics. Appropriate antihistamines will help get rid of scabies.
Means that increase the body’s resistance to infections in the form of solutions - “Eleutherococcus”, “Echinacea”, “Leuzea”, etc.
Sets of vitamin nutrients should also be taken in accordance with the instructions.
Local treatment includes antiseptic drugs that prevent the spread of putrefactive bacteria. Such medications include various alcohols, brilliant green, as well as their analogues - “Fukartsin”, “Chlorhexidine”, “Miramistin”, “Rivanol” or the cauterizing agent “Resorcinol”.
The use of a huge number of zinc-based pastes, preparations and ointments for streptoderma in children with intense scabies.
Calling a dermatologist to your home to treat streptoderma
Our clinic Your Health in Moscow offers all patients the paid service of calling a dermatologist to your home. To do this, you need to call the specified phone number specifying the reason for the request. The doctor will arrive at your place of residence on the day of your visit. An appointment in a comfortable home environment will allow you to receive qualified assistance with significant savings in free time.
Other advantages of calling a dermatologist at home include:
- the opportunity to take most of the required tests without leaving home;
- arrival of the dermatologist at the pre-agreed time without delay;
- absence of distractions that arise during a personal visit to the clinic;
- a preliminary diagnosis is made already at the first visit;
- no risk of infecting others through airborne droplets.
The service will be most relevant for people with a lack of time, parents of small children, elderly patients who have difficulty moving and patients with limited physical capabilities.
Complications of streptoderma
The disease can cause serious harm to the health of patients suffering from immunodeficiency and people prone to frequent allergies. If, when the characteristic symptoms of streptoderma appear, the patient does not seek help in time, then the risk of developing complications increases significantly, which include:
- when an infection enters the bloodstream, sepsis may form or blood poisoning may begin;
- the appearance of deep wounds from non-healing ulcers;
- damage to internal organs by staphylococci, rheumatism and nephritis may develop;
- dangerous increase in body temperature;
- intestinal dysbiosis;
- damage to the fetus during childbirth if the mother has infectious rashes on her body;
- the appearance of thrombophlebitis.
Quite often, after severe stages of skin damage, scars form that remain forever. A cosmetic defect subsequently requires additional expensive procedures to smooth out the outer layer of the skin.
Why should you contact our clinic?
Dermatologists of the highest category
Experienced dermatologists in Moscow. Experience of specialists from 15 years.
Modern equipment
Modern equipment from the world's best manufacturers.
Expert class equipment
Ultrasound is performed using expert-class equipment manufactured by General Electric, SONY, Mindray.
Tests and ultrasound on the day of treatment
Tests, x-rays, ultrasound with interpretation, dressings on the day of treatment in Moscow.
Consultations for adults and children
A network of dermatological clinics in Moscow. Clinics near the metro.
Experienced doctors
Our experienced doctors with over 15 years of experience. Candidates of Medical Sciences.
Prevention of streptoderma
A person at any age can be affected by an infectious skin disease. There is no guaranteed protection against this pathology, but there are a number of preventive measures, the observance of which helps reduce the risk of infection:
- rejection of bad habits;
- healthy lifestyle;
- correct rest regime;
- compliance with all generally accepted hygiene standards and sanitary rules;
- good nutrition;
- daily water treatments with shower;
- use of tar or resorcinol soap;
- timely change of underwear.
Exercising and frequent exposure to fresh air helps strengthen the immune system. In case of accidental damage to the skin, it is recommended to immediately treat the wound with iodine or hydrogen peroxide. You should try not to trigger chronic diseases if they are present and monitor the current state of the body, preventing possible exacerbations.
Types of streptoderma
The disease can occur in acute and chronic form. The first is distinguished by aggressive symptoms and clear manifestations in the form of rashes. The chronic form is characterized by regular exacerbations during a period of decreased immunity.
Streptoderma is divided into several types:
- intertriginous, when a rash forms in the skin folds and is accompanied by severe itching with a desire to scratch the affected areas, often observed in infants;
- dry, with the appearance of white or pink spots up to 5 centimeters in diameter, localized on the neck, arms and legs, after healing, scars often remain;
- the most common form of rash on the face, accompanied by rashes in the form of small blisters, the contents of which quickly flow out and a yellowish crust forms in their place.
The manifestation of characteristic symptoms, accompanied by rashes of various locations, indicates an infectious skin lesion. In such situations, an urgent visit to a dermatologist is required. If treatment is not started promptly, the disease can become chronic.
How to treat streptoderma at home?
First of all, a hypoallergenic diet is prescribed at home with a limit on sweets, spicy and fatty foods. It is important to avoid wearing clothes made of synthetics and wool, as this provokes sweating and contributes to the increase and spread of lesions. Patients are strongly recommended to give preference to natural fabrics.
Also, during the period of treatment of streptoderma, water treatments (bath, shower) are prohibited in order to prevent the spread of the disease. It is recommended to wipe healthy skin with chamomile decoction.
Drug treatment of streptoderma involves the use of multidirectional means. With their use, the manifestations of symptoms reduce their intensity already in the first days of treatment. Remission occurs within 7-10 days from the start of therapy.
- Salicylic alcohol is used to cleanse the affected skin surface and disinfect it. It is possible to perform disinfection using an aqueous solution of boric acid.
- Tetracycline or streptocide ointment is applied topically. It is used on damaged areas of the skin under a bandage. It is recommended to change dressings with ointment every 12 hours. When applied without a bandage, the ointment layer must also be renewed every 12 hours. When applying a new layer of ointment, you need to carefully remove the remnants of the old product from the surface of the skin using a napkin with an antiseptic solution.
- Treatment can include dressings soaked in an aqueous solution of silver nitrate at a concentration of 0.25%. It is also possible to use a solution of resocin (2%).
- Erythromycin ointment or 3% rivanol is applied to the surface of the crusts to soften and for disinfection purposes.
- In case of a generalized form of streptoderma or immunodeficiency conditions, steroid drugs for topical use may be prescribed. They are prescribed only by the attending physician.
Streptoderma in pregnant women
In the process of bearing a child, a woman undergoes a significant restructuring of her hormonal levels and a decrease in immunity. The body uses all resources for the development of the fetus. It is at this moment that the expectant mother is most vulnerable to the possibility of streptoderma.
The disease does not harm the health of the unborn baby; infection can only occur when streptococcus enters the bloodstream. Infection can get on the baby's skin during childbirth if there are infectious rashes on the woman's body. In this case, the disease can cause serious complications and threaten the child’s health.
Timely treatment will reduce all risks of infection during childbirth. Doctors will select the most gentle therapeutic course. All prescribed medications will not be dangerous for the baby. Most often, special creams and ointments are prescribed.
Preventive measures and prognosis
Due to the high risk of infection, sick children should keep their distance for some time and not contact other people. Quarantine is provided for up to 10 days. For the entire period of therapy, it is necessary to follow the rules of hygiene.
To prevent the development of the disease, it is necessary to disinfect the child’s personal belongings. Sick children should have a proper diet rich in nutrients. To improve the quality of the immune system, certain measures should be taken.
streptoderma treatment
As a rule, streptoderma ICD 10 in children is cured without any problems. Exacerbation of the disease and re-infection are observed mainly in children from disadvantaged families or in children with weak immunity. With timely treatment, symptoms disappear within one week. If you do not attach any importance to this, the disease can develop into a more severe form. In the worst case, the disease can lead to blood poisoning. For streptoderma, treatment with ointments and antibacterial agents is mandatory.
Treatment of streptoderma
The course of therapy involves the complex use of antiseptics, antibiotics, the choice of which depends on the type of pathogen, and special ointments. In some cases, additional medications may be prescribed in the form of tablets and injections. Skin itching is relieved with suprastin and telfast. To strengthen the immune system, take vitamins A, B and C.
Depending on the stage of development of the disease, opening of purulent rashes may be required. All related manipulations are carried out in a sterile operating room; operations at home are allowed. After successful opening of the abscesses, the resulting wounds are treated with aniline dyes twice a day. This will help prevent infection.
To speed up the healing process, you need to follow your doctor's recommendations:
- provide your own cutlery and dishes, exclude contact with household members;
- stop taking baths and showers;
- try to change bed linen more often and then wash thoroughly;
- Avoid visiting crowded places; it is advisable not to leave home at all until complete recovery.
It is allowed to use folk remedies, which include tinctures of Eleutheroccus, Echinacea and Leuzea. Admission should be carried out only after prior agreement with the attending physician. The effectiveness of treatment will depend on the individual characteristics of the body, age and current condition of the patient.
Elimination of skin lesions
If the disease has not become severe, treatment of streptoderma is carried out on an outpatient basis. If there are severe symptoms - deep erosion and necrotization of tissue, inflammation of the lymph nodes, etc. - the patient is admitted to a dermatological hospital. Therapy consists of:
- proper skin care, excluding washing with soap and water, to avoid spreading the disease to other areas;
- external treatment of affected areas with aniline dyes, application of ointments with antibiotics and keratolytic compounds;
- taking antibiotics in case of lymphangitis and severe intoxication;
- specific immunotherapy aimed at combating staphylococcal infection.
In addition, complex vitamins may be additionally prescribed, and at the end of the course of antibiotics, probiotic preparations may be prescribed to restore the intestinal microflora.
Prevention of streptoderma involves frequently washing the skin with soap and water. Research shows that soap solution destroys up to 95% of streptococci on the surface of the skin. Compliance with hygiene rules is especially important after contact with a person suffering from a pustular rash.
Diet for streptoderma
During the acute form of the disease, in addition to treatment with antiseptic agents and antibacterial treatment, it is required to adhere to a diet. The following foods should be included in your daily diet:
- legumes and nuts;
- lean meat, fish, eggs and a small amount of fresh cottage cheese;
- porridge;
- soups cooked in low-fat broth;
- fruits and vegetables;
- unsweetened compotes, decoctions and other drinks with low sugar content.
There are no strict restrictions on foods for patients with streptoderma, but doctors advise to refrain from eating fried foods, sausages, butter and hot seasonings. It is advisable to temporarily exclude from the daily diet all products that contain dyes and flavor enhancers.
How to treat with folk remedies?
To speed up recovery, auxiliary treatment with folk remedies is allowed for streptoderma in adults. These include:
- overheating of the skin and increased sweating should be avoided;
- following a diet that excludes sweet, fatty, and spicy foods from the diet;
- clothing should be made from “breathable”, natural materials;
- dressings soaked in herbal decoctions that have drying properties and are not allergens: chamomile and oak bark;
- Since you cannot shower or bathe during illness, it is recommended to wipe healthy skin with napkins soaked in chamomile decoction.
Any treatment, even with the most proven methods, must be accompanied by permission and supervision of a doctor. Otherwise, complications may arise that are difficult to correct.
Streptoderma and similar diseases
Based on external manifestations and test results, not only a diagnosis of streptoderma, but other pathologies of the skin can be established.
In terms of external signs, the diseases are similar to each other, but the treatment regimen is completely different:
- allergic dermatitis, characterized by severe itching not only in areas of the rash;
- lichen and herpes, viral manifestations with rashes localized in the waist and abdomen, accompanied by elevated body temperature;
- eczema, appears upon direct contact with an allergen or as a complication of chronic streptoderma;
- staphylococcal pyoderma, destroys the sebaceous glands, and in severe form can cause furunculosis;
- chickenpox, a viral pathology accompanied by rashes on various parts of the body;
- pityriasis versicolor, characterized by the appearance of brown or reddish spots, the skin in the affected areas begins to peel off.
To accurately establish the disease, it is necessary to undergo a detailed examination and pass the necessary tests. Based on the results, the pathogen will be identified and an accurate diagnosis will be made.
Causes of complications and re-infection
The reason for re-infection may be incorrect therapy when, for example, if you have primary criteria for improvement, you decide to stop therapy. The most important thing is to remember that you need to unquestioningly follow the advice and instructions of your doctor.
streptoderma complications
Prognosis for streptoderma
The disease responds well to treatment and if the patient follows the doctor’s recommendations, the therapy will be successful and without complications. The main thing is not to try to get rid of rashes on your own, this can only cause harm.
Modern medications are highly effective and fight streptococcal infections well, which in turn allows you to quickly relieve the inflammatory process and overcome the disease.
If you do not take any measures and ignore the characteristic symptoms, the disease can develop into a chronic form, which carries with it serious complications, infection of internal organs and even blood poisoning, which is especially susceptible to patients with weakened immune systems. Timely treatment eliminates all symptoms of streptoderma within a week.
Publication date: 2020-06-30
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Treatment of bacterial skin infections
It should start from the early stages and be carried out under the supervision of a specialist. In some cases, local treatment with antibacterial ointments and wiping with antiseptics is sufficient. Widespread rashes, deep pyoderma, require the prescription of systemic antibiotics. In chronic cases, the doctor may recommend autohemotherapy and immune drugs.
Surgical treatment is carried out if the abscess does not open on its own or if a rough scar must be avoided. Laser coagulation and physiotherapy are used to restore tissue.
It is important to identify and treat concomitant diseases, eliminate adverse external effects on the skin, and select nutrition.