What is cervical prolapse
Due to weakness or damage to the ligamentous apparatus, female organs move below the anatomical border.
In this case, discomfort, heaviness in the lower abdomen, and urinary disturbance appear. This is due to the fact that other nearby organs, such as the bladder and rectum, also change their location. In this case, lymph outflow is disrupted and tissue trophism changes. In severe cases, uterine prolapse may occur. The symptoms of this condition can no longer be ignored, since the body of the uterus, even at rest, comes out of the genital slit. This disease is very common, mainly affecting women after 40-50 years of age. Often the disease begins to develop in youth and progresses over time.
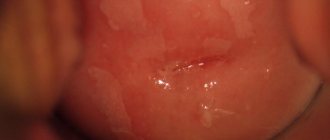
The photo shows how the uterus prolapses. When performing an ultrasound
it immediately becomes clear to the doctor that the uterus is below the physiological norm. In its normal state, it is equidistant from the walls of the pelvis and is located between the rectum and the bladder. The correct position of the uterus is facilitated by its tone, muscle and ligamentous apparatus, any violation of which leads to its prolapse and prolapse.
Uterine prolapse - causes
The disease occurs in women of any age, but if before the age of 30 the pathology is diagnosed in 10%, then after 50 years, signs of uterine prolapse appear in 50% of those examined.
Over time, the disease only progresses.
The main factor contributing to the manifestation of the anomaly is a weakening of the tone of the pelvic floor muscles. There are several other reasons for the development of the disease:
- injuries received during or after childbirth. This may include ruptures, the use of vacuum and forceps;
- surgeries on the genital organs. Often, when diseases such as cervical dysplasia, fibroids, cysts appear, various surgical interventions are prescribed, which cause tissue and muscle trauma;
- intense physical activity;
- congenital pelvic floor defects;
- some neurological diseases;
- numerous births;
- lifting weights;
- hormonal disorders, in particular lack of estrogen;
- the presence of constipation, obesity, tumors in the abdominal cavity. All this leads to increased intra-abdominal pressure and indirectly affects uterine prolapse;
- Connective tissue disorders and weaknesses are often hereditary.
Uterine prolapse after childbirth
During natural childbirth, the pelvic floor muscles are often injured. Pregnancy also has an impact, since at this time increased stress is applied to the ligaments. The photo shows the prolapse of the uterus after childbirth, it is noticeable how its position relative to the norm changes and the risk of prolapse gradually arises.
Today, after the first birth, women often face the problem of uterine prolapse. The risk of prolapse increases when the birth was difficult using a vacuum, forceps, there were severe tears, or the child weighed more than four kilograms.
Under favorable circumstances, if the woman does not lift heavy objects and does not have serious injuries, then the pathology is usually mild.
The main symptoms of uterine prolapse after childbirth will be painful discomfort during sexual intercourse and urination disorders; the photo shows how, due to weakness of the muscular system, the uterus moves down to the genital slit. A gynecologist will be able to identify the disease during an examination. For mild illness, he will prescribe special exercises for prolapse of the uterus or a bandage. The diagnosis cannot be ignored, as this can lead to prolapse and prolapse of other pelvic organs.
If a woman plans to have children in the future and the doctor approves of her decision, then surgical intervention after the first pregnancy is not indicated. Otherwise, the operation will be ineffective, due to the fact that after the second pregnancy and childbirth, all organs will return to their previous state.
Degrees of descent
Depending on the severity of the disease, the doctor will be able to tell the patient how to treat uterine prolapse. In total, there are four degrees of prolapse:
- 1st degree - the cervix is located in the vagina, but its canal descends below the narrowest part of the pelvic cavity. The omission is expressed slightly in this case;
- 2nd degree - the body of the uterus is located in the vagina; when straining, the cervix may appear from the genital slit. This degree is characterized as partial or incipient prolapse. During a gynecological examination, the doctor can see it without the use of gynecological instruments;
- 3rd degree - the cervix and part of the uterus protrude from the genital slit. Incomplete loss;
- 4th degree - all sections and walls of the vagina emerge from the genital slit. Complete loss.
Classification of the disease
The uterine body in the pelvic area is held in place by the ligamentous apparatus and muscular structures of the perineum. The characteristic position has a slight forward inclination, and the vagina and cervix form the opposite angle of inclination. The posterior wall of the uterus is in contact with the rectum, the anterior wall with the bladder. With pathological displacement, the reproductive organ is infringed, which leads to its being pushed out.
There are two types of uterine prolapse - complete and incomplete. In the first case, the organ does not leave the vulvar ring, in the second, the uterus almost completely extends beyond its limits.
The process of disease development occurs gradually:
- First, the cervix descends, but not further than the exit from the vagina.
- The position of the reproductive organ changes only when physical exertion occurs (constipation, coughing or lifting heavy objects).
- Part of the uterus begins to extend beyond the vagina.
- Complete prolapse of the uterine body occurs due to prolapse of the vaginal walls.
Depending on the area of the lesion, cystocele (prolapse of the anterior wall, which is characterized by urinary incontinence), and rectocele (protrusion of the posterior wall, which is accompanied by gas incontinence and constipation) are distinguished. There is also a mixed form of the disease, which is characterized by simultaneous protrusion of the posterior and anterior vaginal walls.
Make an appointment
Symptoms of uterine prolapse
In the early stages of the disease, treatment is easier and more effective, so it is important not only to know what cervical prolapse looks like in the photo, but also to study the signs of the disease. The problem with diagnosing the pathology is that women in the early stages attribute the manifestation of the disease to fatigue, menstruation, or an uncomfortable position. Many people tend to ignore problems until the signs of uterine prolapse leave no doubt. In these cases, uterine prolapse occurs and the only treatment left is surgical treatment.
When the uterus prolapses, the following symptoms may appear:
- nagging pain in the area of the ovaries, mild at first, then progresses. At first, symptoms appear only after sitting for a long time; in a supine position, the pain subsides. Over time, the pain syndrome intensifies; violation of defecation and urination;
- discomfort and pain during sexual intercourse;
- sensation of a foreign body in the vagina;
- menstruation becomes heavy and painful.
As it progresses, all existing symptoms intensify. Urinary incontinence may occur with the slightest exertion (sneezing, coughing) or, conversely, urination becomes difficult. The risk of infectious diseases of the genitourinary system increases. With severe prolapse or prolapse of the uterus, as in the photo, a woman can determine the formation herself. In severe cases of the disease, prolapse of the bladder and rectum is often detected. It is worth remembering that each woman exhibits symptoms of the disease individually, so it is important to respect your health and not ignore the initial symptoms.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
What complaints does pelvic organ prolapse cause?
In the case of pelvic organ prolapse, complaints are the determining factor in choosing the necessary treatment method. This may be a feeling of pressure in the pelvis, sometimes even pain; often the patient feels or can feel a formation protruding from the vagina, on which abrasions can form over a long period. If you experience urinary incontinence when coughing or laughing, a sudden urge to urinate, or after urinating you have to push the protrusion back into the vagina, prolapse may be to blame. When the intestine protrudes, defecation problems may occur. Usually, the stronger the prolapse, the more pronounced the complaints, which may intensify over time. When contacting a doctor, it is important to accurately describe your existing complaints so that the specialist can offer you the most suitable treatment method.
Diagnostics
Before prescribing treatment, the gynecologist notes the main symptoms of uterine prolapse and conducts additional diagnostics.
- The doctor examines the rectum and vagina, checking for displacement of the bladder and vaginal walls.
- A swab of the flora is taken and a bacterial culture is done.
- In case of urination problems, laboratory tests are required - microscopy, bacteriological examination of urine, Nechiporenko analysis.
- If pathology is detected, all women undergo colposcopy
. - An ultrasound examination of the pelvic organs
is prescribed . - If indicated, bladder examination and urodynamic studies are performed.
- , excretory urography
may be done . - When additional diseases are associated or there are hyperplastic processes of the endometrium, diagnostic curettage of the uterine cavity and hysterosalpingoscopy are prescribed.
- To clarify the condition of the pelvic organs, computed tomography
. - In case of complete or partial prolapse, the patient can be additionally examined by a surgeon, urologist, or proctologist. The condition of the sphincter of the rectum and bladder is examined to detect stress incontinence.
Early diagnosis of uterine prolapse is an opportunity for a woman to avoid surgery by using conservative treatment methods.
Operation
The main method of treatment is still surgical, since the supporting apparatus of the pelvis is not restored. Unfortunately, the most popular method, removal of the uterus, often does not help, since not only the uterus, but the pelvic organs (bladder, rectum) prolapse.
For this reason, this approach leads in 30-50% of cases to the development of prolapse of the vaginal stump.
Another problem with hysterectomy is posthysterectomy syndrome, which leads to impaired urination, defecation and decreased sexual function, including due to postoperative shortening of the vagina. Reconstructive operations performed through the vagina seem to be the most optimal and proven. On the one hand, they allow you to achieve a good anatomical result, on the other, a good cosmetic effect. One of the most modern techniques are hybrid operations, which allow the operation to be individualized for each specific patient, while maximizing the use of his own tissues, and, if necessary, supplementing them with a prosthesis only in the busiest places.
Treatment of prolapse and prolapse of the uterus
When symptoms of uterine prolapse appear, a woman should definitely go to the doctor to prescribe treatment. Before doing so, it is important not only to read reviews about the specialist, but also to completely trust him. Only in this case, if all recommendations are followed, will the patient be able to cope with the pathology. When choosing tactics and treatment methods, the doctor is guided by the patient’s age and the severity of the disease. For minor or mild cases, conservative methods are used; in severe forms, with complete or partial prolapse of the uterus, surgical intervention is recommended. Surgery for uterine prolapse is the correction of functional changes and its fixation. The type of intervention is determined individually. During the consultation, the doctor will definitely tell the woman what to do if the uterus prolapses and how best to carry out treatment.
The goal of both treatment methods is the same - restoration of the anatomical position of the uterus and diaphragm of the pelvic area.
Conservative methods
Treatment with conservative methods represents a whole series of therapeutic measures that must be carried out comprehensively.
Gymnastics
When the uterus prolapses, Kegel gymnastics is prescribed - this is one of the most well-known methods of strengthening the pelvic floor muscles. Professor of Medicine Dr. Arnold Kegel has developed a whole system of exercises to treat weakness of ligaments and muscles, their essence is to strengthen the muscles and increase blood flow. In his works, the doctor emphasized the importance of the following factors:
- regularity of independent work of intimate muscles;
- determination of results using a special perineometer device;
- use of elastic loading.
These exercises for uterine prolapse are considered simple and can be done independently.
At the very beginning, a woman needs to determine which muscles she will have to work with. To do this, for example, during urination, you can interrupt the stream of urine, then the technique will become clear. You can’t train like this all the time; this is done to master the basic movements.
You can start training by lying on your back, with your legs slightly spread and your knees bent. The heels should be on the floor, one hand should be placed under the buttocks, the other on the stomach.
- You need to squeeze your pelvic floor muscles, pulling them up. Hold time is 10 seconds.
- Then it is important to completely relax the muscles for 10 seconds.
- Exercise time: 5 minutes, three times a day.
It is considered incorrect to hold your breath during exercise, push your muscles down, and retract your navel.
Exercises can be done not only lying down, but in any other position, unnoticed by others. The result is felt within 5-6 weeks, but in some cases, with severe muscle weakness, up to three months of training may be required.
In addition to the well-known Kegel technique, you can perform therapeutic exercises according to Yunusov.
Entire complexes of therapeutic exercises have been developed for uterine prolapse.
- You can perform the well-known “bicycle” exercise for at least 5 minutes.
- Starting from the starting position “birch tree”, the legs perform “scissors” movements.
- Lying on your back, you need to lean on your elbows, bend your legs, then raise your hips. You will get a half-bridge; in this position, pull in the perineum, count to 10 and return to the starting position.
- It is necessary to pump up the press. To do this, you need to raise your straight legs, connecting them together. Then, in weight, you need to bend your knees, straighten them and lower them to the floor. Repeat the exercise 10 times.
- An excellent exercise when you are sick is simply climbing stairs.
At your appointment, the doctor must tell you how to strengthen the pelvic floor muscles and share special gymnastic complexes. You need to do exercises daily, if possible several times a day, then the result will be positive and the muscles will strengthen faster.
Gynecological massage
In gynecological practice for the treatment of uterine prolapse, special massage can be used. The procedure develops ligaments and muscles, increases tone. With minor pathology, all organs return to their places and are firmly fixed by the ligamentous apparatus.
The massage is performed on a special table or on a regular gynecological chair. The duration of the procedure is about 15 minutes. The doctor tries to prevent severe pain during the massage, so the intensity increases gradually. After five procedures, the patient should be examined to determine the effectiveness of the chosen massage technique. In order to strengthen the positive result, it is important to lie on your stomach for about 20 minutes after the procedure.
Bandage
If a mild degree of pathology is diagnosed, the gynecologist may prescribe a bandage for uterine prolapse. Wearing such a product can make life easier for the patient; it fixes muscle tissue well, which reduces pain and discomfort. The use of a bandage is necessary during pregnancy in case of prolapse; wearing it reduces the pressure of the child on the organs and reduces the load on the spine.
Today there are several types of support structures - these are panties or belts. Such tightening products consist of natural fabrics with plastic inserts. Bandage panties can be worn directly on the naked body and washed if necessary. When it is necessary to constantly wear fixing bandages, it is recommended to buy several models at once to maintain hygiene.
The disadvantage of bandages is that they put pressure on internal organs, although modern models are very comfortable. They should not be worn more than twelve hours a day.
Tying up
As an auxiliary remedy for mild uterine prolapse, as in the photo, and the absence of severe symptoms, treatment can be carried out using cloth tying. This method is still mainly used for prevention, but it will not be superfluous after childbirth. Its difficulty lies in the technique of execution; when properly tied, unlike a bandage, the organs are not compressed, but simply fixed, and the condition of the pelvic muscles improves. For tying, a thick fabric is suitable - cotton or linen, approximately 3 meters long and 50 centimeters wide.
The action should only be carried out lying down, the fabric is placed at the waist and crossed behind the back, then brought forward again. In this case, you should get two layers, the wide one should fit the stomach, the narrow one should serve as support, and you need to tie a knot on the side. The fabric should not be pulled too tight; it should be comfortable and comfortable. Of course, the first time it is best to tie it under the supervision of a specialist or nurse.
Medications
In some cases, your doctor will prescribe medication to strengthen your muscles, usually estrogen-based medications. The hormone is responsible for stimulating the development of the uterus and the normal functioning of the muscle tissue of the pelvic organs. Not only drugs for internal use are prescribed, but also estrogen-based ointments that are inserted into the vagina. If, in addition to prolapse, inflammatory diseases appear, then antibacterial therapy is prescribed. For constipation, your doctor may recommend mild laxatives.
Use of pessaries
When the uterus prolapses, the use of a pessary is sometimes prescribed - this is a special rubber ring that is placed in the vagina and serves as support for the displaced organs. But this method has a number of limitations and can lead to inflammation and even bedsores. In modern practice, it is used quite rarely and is prescribed to older patients. The pessary must be disinfected daily and visited a gynecologist every two weeks to monitor the condition.
Operative methods
The method of surgical treatment depends on many factors of the disease: the degree of prolapse, the woman’s age, general condition, sex life. Sexual relationships play an important role when choosing a surgical method. If a woman is firmly convinced that further sexual activity is not envisaged, for example, in old age, then this simplifies and increases the effectiveness of treatment. In this case, doctors recommend median colporrhaphy; the surgeon stitches the back and front walls of the vagina.
Among the popular methods of surgical treatment:
- plication of the uterine cross ligaments;
- facilitated laparoscopic protofixation;
- mesh sacrovaginopexy.
Treatment using special meshes that strengthen the pelvic floor is considered the most effective. These methods are characterized by a relatively easy and short recovery period.
During treatment of the disease, it is necessary to abstain from sexual activity, bad habits and physical activity. Depending on the surgical technique, you can usually return to sexual activity after a month and a half.
Folk remedies
In the treatment of pathology, traditional methods are often used; herbs and herbs have an analgesic effect and increase the tone of the uterus. Before using medicinal herbs and tinctures, you should always consult your doctor to identify contraindications.
- Elecampane. One tablespoon of the root of a dry plant is poured with 500 ml of vodka and left for 10 days. The tincture should be taken once a day on an empty stomach in the morning.
- Dymyanka. Two teaspoons of the herb should be poured into 500 ml of boiled cold water. Leave for 8 hours, then strain. Take half a glass of smoke half an hour before meals.
- Melissa. 2 tablespoons of raw materials should be poured with two glasses of boiling water. Leave in a thermos overnight. Take two-thirds of a glass one hour before meals.
- A decoction of birch and alder bark should be drunk as tea, half a glass twice a day after meals.
- White lily decoction. Two tablespoons of crushed root are poured into two glasses of boiling water and left in a thermos overnight. The decoction should be consumed before meals 3 times a day.
- Gentian decoction. Pour 2 tablespoons of raw material into a liter of water and heat in a steam bath, then the broth should sit for about an hour. Drink the strained product 100 ml three times a day.
- Eggshells with lemons. Dry shells from five eggs are mixed with nine finely chopped lemons. Leave the mixture for four days, stirring occasionally, then add 500 ml of vodka and let it brew for another five days. Strain the mixture and squeeze out. You need to take 50 grams in the morning and evening until the tincture runs out. The course of treatment is 3 times with breaks of one month.
Prevention and additional recommendations
To prevent uterine prolapse or relapses after treatment, it is necessary to begin training the pelvic floor muscles as early as possible. The most effective are vaginal exercisers and Kegel exercises. Birth trauma plays a big role. That is why it is recommended to select the best clinics to ensure a less traumatic birth process. Obstetricians-gynecologists with extensive experience are able to ideally restore the anatomy of the pelvic floor if ruptures occur.
Additional tips:
- Uterine prolapse is easier to prevent. The earlier preventive measures are started, the greater the chances of preventing the disease. You need to do strengthening procedures constantly, even after menopause.
- Don't forget about self-diagnosis. It is enough to strain while washing. If at the same time the walls of the vagina descend, then the problem already exists. The sooner you take action, the shorter the treatment will be.
- We manage without surgery. If you start sounding the alarm when primary symptoms appear, then surgical intervention can be avoided.
- We adhere to the specialist’s recommendations. Exercises to strengthen the pelvic floor muscles should be done daily or with breaks of one day. Efficiency can be increased using hardware techniques.
Every woman is at risk. The likelihood of the problem increasing after natural childbirth, heavy physical labor and constipation. At the beginning of the progression of pathological disorders, conservative treatment can be managed.
The problem is the difficulty of diagnosis. Only a gynecologist can determine the primary changes occurring. In this regard, it is recommended to visit a female doctor at least once a year. In the primary stages of prolapse, it is enough to use hardware techniques and specialized vaginal simulators. Thanks to timely measures, it is possible to eliminate complications such as sexual dysfunction and urinary incontinence.
Prevention of uterine prolapse
- Regular moderate physical activity.
- Preventive examination by a gynecologist every six months.
- Refusal to lift weights.
- Special physical exercises during pregnancy and after childbirth.
- Rational management of childbirth.
- Proper nutrition to prevent constipation.
- Posture control.
- During menopause, hormone replacement therapy is possible.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Is it possible to slow down the formation of prolapse?
To reduce minor prolapse or reduce the risk of one, you can train the muscles that keep your organs in the right place by doing Kegel exercises.
They are based on repeated tension and relaxation of muscles. To understand which muscles need to be tensed, imagine that you are sitting on a ball and trying to lift it by tensing your muscles. This can be done in any position - sitting, standing or lying down. The goal of the workout is to hold the muscles under tension for approximately 10 seconds and repeat this exercise 8-10 times in one approach. You need to train 3 times a day at least 4 times a week. Follow this regimen for at least 16 weeks. To maintain the effect, this task must be performed over a long period of time, like any muscle training. Over time, you can try to tense your muscles more and hold them in this state for longer. If you are unsure if you are doing these exercises correctly, you may want to see a physical therapist.
Questions and answers
Question: What is the difference between program 2 and program 7? M.Sh., Nalchik. Answer: Programs 2 and 7 differ in goals: the goals of program No. 2 (treatment of urinary incontinence, treatment of uterine and vaginal prolapse) are to “straighten” the bend, reposition and FIX the UTERUS in the correct position, eliminate urinary incontinence during sexual intercourse, physical activity, stress and etc., i.e. mainly medicinal. The goals of program No. 7 (recovery after childbirth and narrowing of the vagina) are to improve the quality of life and develop the uniqueness of the feminine. Depending on the condition of the muscles and the level of training, various techniques are used.
Question: I have developed URINary INCONTINENCE WHEN COUGHING and RAISING BAGS. A friend who was treated by you said that it was prolapse of the uterus. I’m embarrassed to go out in public, I can’t go to the market, I started to feel ashamed of myself. An inferiority complex will soon form. But I'm only 54 years old. I HAVE HEARD A LOT OF GOOD THINGS ABOUT YOUR CLINIC. How can I get treatment? With uv., F.D., Makhachkala. Answer: Judging by the complaints, uterine prolapse is very likely. You should not lift more than 3 kg. Reception for examination and treatment by appointment by phone 8 (calls within Russia are free) or.
Question: I was treated for uterine prolapse in your clinic a couple of years ago. I've been working a lot lately and I'm starting to notice that it feels like I'm feeling it again. Is a relapse possible, what should I do? L.A., St. Petersburg. Answer: If you continue heavy physical activity with straining, lack of regular training of the muscles of the vagina and perineum, and failure to comply with preventive measures, RECURRENCE OF UTERUS AND VAGINAL PROPRESSION, uterine and vaginal prolapse, and urinary incontinence is possible.
Question: I was diagnosed with Uterine Prolapse. But I myself DO NOT FEEL ANYTHING, I do not experience any health problems. Could this be possible? A.M., Baksan. Answer: Very often, hardworking and patient women do not pay attention and do not consider the “minor symptoms” of uterine prolapse to be a problem: rapid fatigue of the “lower back”, periodic pain in the lower abdomen and groin areas in the evening and after physical activity, rapid filling and the feeling of incomplete emptying of the bladder , drip urinary incontinence when coughing, laughing, fast walking, straining, discomfort and pain during intimacy, etc. THE HABIT OF “ENDURING”, everyday life and bustle do not allow you to stop and look at yourself in a new way...
Question: Today is the 22nd day after giving birth. THE CERVIX IS VISIBLE IN THE VAGINA. Please tell me, is this the norm? Will she rise? Answer: Prolapse of the cervix extremely RARELY stops (disappears) on its own. It is DESIRABLE after the end of lochia (bloody discharge from the genital tract after childbirth) to REPOSITION THE UTERUS (return the uterus to the correct anatomical position). At the Resort WOMEN'S HEALTH CLINIC, this treatment is carried out within 7 DAYS.
Question: Before pregnancy, the uterus was bent backwards; after a complicated birth and curettage, a forward bend formed on the seventh day after birth. Now, when the pelvis is raised and, sometimes, DURING SEXUAL INTERACT, AIR gets in and comes out with a “fart.” Is this related to the curvature of the uterus and what can be done about it (it is impossible to play sports because of this “farting”)? Answer: The release of air from the vagina is associated with weakness (insufficiency) of the perineal muscles and an increase in the capacity (volume) of the vagina. WITH THE PURPOSE OF SOLVING this problem, the Clinic has developed Program No. 7 Recovery after childbirth and narrowing of the vagina. WE ARE READY TO RECEIVE YOU.
| ONLINE to an experienced doctor can be found here. REGISTER ONLINE for treatment here. REGISTER online for treatment |
Sign up
Question: WHAT DOCUMENTS ARE REQUIRED for vaginal reduction and treatment in your clinic? Answer: It is advisable to have copies of the results of a previously conducted clinical and laboratory examination (copies of ultrasound, laboratory and other studies), copies of epicrisis (conclusions) of surgical and conservative treatment. In other words, the most complete amount of medical information about your health status. If necessary or desired, it is possible to perform a clinical and laboratory examination in our Clinic.
Question: Is it possible to issue a sick leave certificate at the Clinic for the period of vaginal reduction and treatment? Answer: At the Women's Health Resort Clinic, sick leave (sick leave) is not issued.
Question: How to get to the Clinic UNDER THE POLICY? What is needed for this: a referral from a gynecologist, or is just desire and an insurance policy enough? Answer: You should contact your insurance company to obtain a cover letter. If you have a covering letter, you will be able to carry out the necessary examination and treatment in our Clinic. At the appointment you must have your passport and insurance policy with you. Sincerely, Chief Accountant of the Women's Health Resort Clinic.
Question: Do you provide documents to obtain a tax deduction for the treatment of uterine prolapse? Answer: The Women's Health Resort Clinic provides documents to obtain a tax deduction for the treatment of uterine prolapse (13% tax refund).
We work WITHOUT WEEKENDS and holidays:
Monday - Friday from 8.00 to 20.00, Saturday, Sunday, holidays from 8.00 to 17.00.
Treatment in Pyatigorsk by appointment by multi-channel phone 8 (800) 500-52-74 (calls within Russia are free) or +7.
The cost of treatment for uterine prolapse is 17,150 rubles.
The cost of vaginal reduction with vaginal threads is 55,000 rubles.
| ONLINE to an experienced doctor can be found here. REGISTER ONLINE for treatment here. REGISTER online for treatment |
Sign up
Subsections
- Program No. 1. Treatment of inflammatory and infectious processes of the pelvis
- Program No. 2. Treatment of urinary incontinence, treatment of uterine and vaginal prolapse
- Program No. 3. Treatment of female infertility
- Program No. 4. Cervical treatment
- Program No. 5. Treatment of uterine fibroids
- Program No. 6. Treatment of cervicitis and endocervicitis
- Program No. 7. Recovery after childbirth and narrowing of the vagina
- Program No. 8. Treatment of chronic cystitis
- Program No. 9. Treatment of menopause
- Program No. 10. Treatment of mastopathy
- Program No. 11. Treatment of endometriosis
- Program No. 12. Treatment of hydrosalpinx
- Program No. 14. Treatment of polycystic ovary syndrome
- Program No. 15. Preparation for IVF, ICSI, artificial insemination
- Program No. 16. How to remove belly fat
- Program No. 17. Treatment of kraurosis
- Program No. 18. Treatment of vulvar leukoplakia
- Program No. 19. Prevention of mastopathy
- Appointment with a gynecologist to “check for EVERYTHING”
Consultation with other specialists
Consultations with specialists regarding prolapse and prolapse of the uterus in women can provide important information about the state of health and choose the best ways to solve the problem.
- Endocrinologist. A woman with uterine prolapse is recommended to consult an endocrinologist - a doctor who regulates hormonal levels. Since the cause of uterine prolapse may be a lack of estrogen.
- Nephrologist and urologist. When the uterus prolapses, the urinary system is affected, so it is necessary to conduct an examination before treatment.
- Oncologist. Any changes in the pelvic organs in women require consultation with an oncologist-gynecologist. This will eliminate dangerous conditions that may not be visible to the naked eye.
- Surgeon. Treatment for uterine prolapse in women is usually done with surgery. A consultation with a surgeon is required first.
- Therapist. A general practitioner is able to adequately assess the lifestyle of a patient with uterine prolapse and give the necessary recommendations.
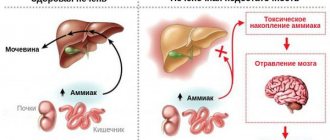
Pathogenesis
All pelvic organs in women are mobile relative to each other. They shift under the influence of external or internal factors, but normally they always return back. The root cause of uterine prolapse is considered to be connective tissue failure and hereditary predisposition. Under such conditions, a woman (even in the absence of other aggressive factors) will sooner or later begin to experience prolapse of the vagina and cervix. Other conditions that affect the function of the pelvic organs aggravate the problem and accelerate its occurrence. Uterine prolapse develops against the background of prolapse in the absence of therapy.
It is worth noting that uterine prolapse and prolapse can occur even in women who do not have a genetic predisposition for this. In such a situation, pathogenetic factors include difficult labor, intense physical activity and constant intra-abdominal pressure.
When choosing a method of pathogenetic therapy for uterine prolapse in women, it is important to determine what caused the intimate problem. For primary causes (heredity), treatment is performed, the purpose of which is to improve the patient’s quality of life. In case of secondary pathogenetic factors, it is necessary to eliminate the negative impact, and then carry out correction.
Conservative treatment
It is prescribed only if the healthy functioning of the genitourinary system organs is maintained. If the uterus has dropped to the genital slit, then surgery is recommended. For minor violations, the gynecologist prescribes the following treatment procedures:
- Gynecological massage.
- Hormone replacement therapy.
- Therapeutic exercises to strengthen the muscles of the genital organs.
- Local application of pastes and gels with female hormones and metabolites.
If surgery is unacceptable due to age, then dense tampons and pessaries (rubber rings with different diameters and thicknesses) are prescribed. Fixing the pessary in the vagina allows you to keep the cervix in the optimal position. The duration of treatment is prescribed by the attending physician. Wearing rubber rings for a long time is prohibited due to possible complications. Additionally, medicinal drugs and herbal mixtures for douching are prescribed. You can wear pessaries for a month, after which you rest for two weeks. At least once a month you need to visit a specialist for a gynecological examination.
Complications
Prolapse of the cervix and uterus is a condition that in itself is a complication. For a woman, the consequence of pelvic organ prolapse is their complete loss.
Since all organs in the human body are interconnected, displacement of the uterus and appendages leads to a change in position and disruption of the function of neighboring organs. Uterine prolapse greatly affects the functioning of the urinary system. A woman experiences urinary incontinence when laughing and exercising. When the uterus prolapses, recurrent cystitis occurs, which over time is complicated by pyelonephritis and can even lead to acute renal failure.
Uterine prolapse disrupts bowel function. Women experience constipation or fecal incontinence, and increased flatulence.
Prolapse and prolapse of the uterus are fraught with frequent inflammatory processes “female-like”. Due to friction against underwear during prolapse, trophic ulcers and cracks are formed on the mucous membrane, into which infection easily penetrates. As a rule, a woman with complete prolapse of the uterus develops infertility. Even after surgery, it is not always possible to restore fertility.
Advantages of the author's methodology
- The result of the operation is reliable fixation of the uterus (or the stump of the cervix or the dome of the vagina in previous operations to remove the body of the uterus and the uterus with the cervix) in the optimal direction in accordance with the natural vector of tension. If intra-abdominal pressure increases in the future, the likelihood of relapse is virtually eliminated.
- The risk of postoperative complications associated with implant installation (the appearance of erosions, infections, phlegmons, abscesses, etc.) does not exceed 0.1% (when using the Prolift, Elevate, etc. techniques, this figure reaches 30%).
- Thanks to the use of high-tech equipment, the risk of intraoperative complications is practically eliminated.
- After recovery, sexual activity can be carried out without restrictions (unlike other methods).
- It is possible to preserve the uterus (unless there are indications for its removal) and plan a pregnancy in the future.
- Due to the use of laparoscopic and vaginal access - low-traumatic techniques - recovery takes about two weeks, hospitalization does not exceed three days.
Thanks to the use of laparoscopic access, it is possible to perform simultaneous operations: eliminating several diseases at once that require surgical treatment, during one anesthesia. Thus, a woman who has, for example, fibroids, cysts, adenomyosis, hernia, etc., has the opportunity to also eliminate these diseases when treating genital prolapse, regardless of its degree.
Uterine prolapse does not occur suddenly; the onset of pathological changes can be detected during regular preventive examinations. In addition, the asymptomatic course at the initial stage is necessarily replaced by a bright clinical picture. Having contacted a specialist with the appearance of the first warning signs (this often happens after the first vaginal birth), you can get by with either conservative treatment or a low-traumatic operation with a quick recovery.
If you have any symptoms, please contact me in a way that is convenient for you. I select treatment for each patient taking into account the existing disorders, explaining in detail why I recommend this or that treatment method. In the absence of indications for surgical treatment, I prescribe conservative therapy. If surgery is unavoidable, I always give preference to low-traumatic methods. You should also know that removal of the uterus, even at a late stage, is not a prerequisite for recovery. I always strive to have breast-conserving surgery if possible. Most of my patients managed to save the organ. Some women who came to me after ineffective treatment in other clinics were finally able to forget about prolapse.
The technique I developed in 1997 was awarded a diploma from the Association of Coloproctologists of Russia as the best work in the treatment of pelvic organ prolapse. I have been treating patients for many years. The results of prolapse treatment are summarized in monographs and scientific publications, which are published in peer-reviewed professional publications: domestic and foreign.