Features of the use of indirect anticoagulants
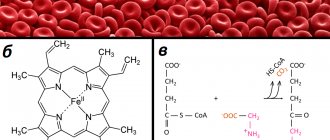
Indirect anticoagulants disrupt the synthesis of coagulation factors in the liver (prothrombin and proconvertin). Their effect appears 8-12 hours after administration and lasts from several days to two weeks. The most important advantage of these drugs is that they have a cumulative effect. Vitamin K antagonists (the second name for indirect anticoagulants) have been used for primary and secondary prevention of thromboembolism for more than 50 years. Vitamin K is an integral part of the coagulation process.
Vitamin K antagonists are called indirect anticoagulants.
Warfarin and other coumarin derivatives are the most commonly used indirect anticoagulants. VKAs (short name for vitamin K antagonists) have many limitations, so you should not start taking them on your own. Only a qualified doctor can select the correct dose based on test results. Regular monitoring of blood counts is of great importance for timely dosage adjustment. Therefore, you need to keep in mind that if your doctor has prescribed you to take warfarin 2 times a day, then you are prohibited from reducing or increasing the dose on your own.
It is also not recommended to resume taking the drug at the same dosage after a long break. Warfarin has a half-life of 40 hours and takes at least 7 days to take effect. The drug is metabolized in the liver and excreted from the body in the urine. Currently, warfarin remains the optimal treatment option for patients with ischemic stroke.
The future of OAC in the prevention and treatment of arterial and venous thrombosis
After nearly 60 years of use of OACs whose mechanism of action is mediated by vitamin K antagonism, two new OACs with different mechanisms of action were approved for use in 2008 in Canada, Europe (including Russia) and Australia for the prevention of thromboembolism in patients who have undergone hip or knee replacement surgery. Both drugs are currently being studied in large clinical trials in patients with cardiovascular disease. Particular emphasis is placed on the prevention of systemic thromboembolism in patients with atrial fibrillation. In addition, OACs are being tested in patients with acute coronary syndrome and for the prevention of VTE.
Compared with warfarin and its analogues, direct thrombin and factor Xa inhibitors have a more favorable pharmacological profile. They have a direct effect that is independent of the level of plasma antithrombin III, are small molecules with predictable pharmacodynamics, which allows their use once or twice a day with fixed dosing regimens without the need (in most cases) for regular monitoring of anticoagulant effects. So far, official indications for their use are limited to orthopedic interventions (arthroplasty of the hip or knee joints). However, future clinical trials may significantly expand the scope of their use. The short half-life of the new OACs may help prevent the clinically significant bleeding that occurs in patients taking warfarin, as well as provide long-term antithrombotic protection in individuals who are refractory to coumarins, for example, in the absence of an INR response to a weekly warfarin dose greater than 70 mg.
Another issue that requires careful analysis is the interaction of new OACs with other drugs. For example, dabigatran interacts with amiodarone, verapamil and quinidine, which belong to the group of P-glycoprotein inhibitors. Rivaraxoban also has drug interactions. In particular, inhibitors of CYP3A4 (rifampicin) or P-glycoprotein (ketoconazole, erythromycin, clarithromycin, ritonavir) alter the plasma levels of rivaroxoban.
Another potential issue that needs to be addressed in the future is the choice of antidotes when using new OACs in clinical situations requiring immediate hemostasis, such as severe bleeding. There are currently no recommendations on this matter. However, the use of recombinant factor VIIa (eptacog alfa) or activated prothrombin complex concentrate may be effective, although there is insufficient data to recommend their use for this purpose [26]. Other approaches currently in preclinical studies involve obtaining factor Xa from plasma with further chemical modification to competitively bind its inhibitor [33]. In addition, antidotes are being developed based on specific anti-DNA or anti-RNA antibodies [34]. It has also been shown that the use of the biotin/avidin system provides rapid inactivation of these drugs [35, 36]. It is likely that the strategy of direct thrombin inhibition or direct factor Xa inhibition using oral agents will become an alternative to warfarin in the near future. In addition, we can assume the possibility of preferential use of new OACs in certain groups of patients (for example, with impaired liver or kidney function).
List of indirect anticoagulants and their mechanism of action
The list of indirect anticoagulants is headed by warfarin (another trade name “Coumadin”). It is one of the most popular medications prescribed to prevent blood clots. Less popular vitamin K antagonist drugs are syncumar, acenocoumarol and dicumarol. The mechanism of action of these drugs is identical: a decrease in the activity of vitamin K absorption, which leads to the depletion of vitamin K-dependent blood clotting factors.
Patients taking warfarin and synonymous anticoagulants should limit daily intake of vitamin K from food and dietary supplements. Sudden changes in vitamin K levels in the body can significantly increase or decrease the effect of anticoagulant therapy.
Disadvantages of Vitamin K Antagonists
Warfarin is a real “old-timer” of the pharmaceutical market
Until the end of 2010, a vitamin K antagonist (warfarin) was the only oral anticoagulant approved by the World Health Organization for the prevention of thromboembolic complications in patients with non-valvular atrial fibrillation and the treatment of venous thromboembolism. For half a century, pharmacists have studied in detail the effectiveness of the drug, and also clearly identified the disadvantages and side effects.
The most common include:
- narrow therapeutic window (for poisoning it is enough to take a minimum number of tablets);
- interaction with foods rich in vitamin K (taking the tablets in combination with daily consumption of green vegetables can lead to hyperkalemia);
- delayed anticoagulant effect (this means that several weeks must pass between the start of therapy and the first results). For the prevention of venous thrombosis, this period is too long;
- the need for frequent blood monitoring and dose adjustments;
- the possibility of bruising and bleeding.
Factor Xa inhibitors
According to its mechanism of action, rivaroxaban is an oral direct inhibitor of factor Xa that binds reversibly to it [22]. Rivaroxaban has high bioavailability (60–80%) and reaches peak plasma concentrations approximately 3 hours after administration [23]. There is evidence that rivaroxaban can bind not only to factor Xa, but also to Va (prothrombinase complex). This is one of the clinical advantages of the drug compared to heparin, which has a molecular weight that is too large to block factor Xa as part of the prothrombinase complex [22]. Unlike dabigatran, the absorption of this drug is not affected by the pH of the intestinal environment [24]. The half-life of rivaroxaban is approximately 5–9 hours in patients with normal renal and hepatic function [23, 25]. Higher levels of rivaroxaban may be determined in patients with impaired renal and hepatic function, since one third of the drug is excreted by the kidneys and about two thirds is metabolized in the liver, primarily through the cytochrome P450 system [26].
The primary outcome of the phase III clinical trials that led to the approval of rivaroxaban was a clinical trial program that evaluated the effectiveness of rivaroxaban compared with enoxaparin in 1000 patients undergoing knee surgery or total hip replacement. The drug was approved for use in Canada (September 2008), Europe (EMEA, October 2008), Australia (November 2008) and Russia (December 2008). In March 2009, a panel of experts from the FDA (Food and Drug Administration) recommended rivaroxaban for clinical use, albeit with adjustments to the need for more detailed information about the safety of the drug. The currently approved dosage of rivaroxaban for the prevention of VTE in patients undergoing hip or knee surgery is 10 mg as a single dose 6 to 10 hours after surgery, then daily for 5 weeks after hip surgery and two weeks after knee surgery.
Currently, approval for rivaroxaban dosage guidelines is based on doses used in the double-blind, randomized clinical trials RECORD-1, -2, -3, and -4 (Table 2). In particular, RECORD-1 [27] and RECORD-2 [28] studied rivaroxaban in patients undergoing hip replacement, and RECORD-3 [29] and RECORD-4 [30] studied patients after knee surgery. The RECORD-1 and RECORD-2 studies showed superiority of rivaroxaban compared with enoxaparin 40 mg administered as a single dose. Superiority over enoxaparin, including at dosages of 30 mg 2 times / day (North American doses of enoxaparin), is shown in RECORD-3 and RECORD-4. Rivaroxaban was overall superior to enoxaparin in all of these trials, despite a small, non-significant increase in bleeding.
In the cardiovascular clinic, rivaroxaban is still in phase III clinical trials - for the prevention of thromboembolic events in patients with non-valvular atrial fibrillation (ROCKET-AF), for secondary prevention of VTE (EINSTEIN), for primary prevention of VTE in patients with acute illness ( MAGELLAN) and for the secondary prevention of adverse cardiovascular events in patients with acute coronary syndrome (ATLAS ACS 2 TIMI 51).
In the MAGELLAN trial, rivaroxaban 10 mg was administered for 31–39 days, similar to the doses used in RECORD, compared with enoxaparin 40 mg as a single subcutaneous dose for 6–14 days in 8000 hospitalized patients (Identifier: NCT00571649). The ROCKET-AF trial is examining rivaroxoban 20 mg/day versus warfarin with a target INR range of 2–3 for thromboembolic prophylaxis in 14,000 patients with nonvalvular atrial fibrillation (ID: NCT00403767). Rivaroxaban was found to have an additive effect compared with standard treatment with acetylsalicylic acid or the combination of acetylsalicylic acid with clopidogrel for the prevention of adverse cardiovascular events in patients with recent acute coronary syndrome - ATLAS ACS 2 TIMI 51 phase III clinical trial (Identifier: NCT00809965). This drug is taken 2.5 or 5.0 mg 2 times a day. This dose is regulated by the phase IIb clinical trial ATLAS ACS TIMI 46, which showed not only a trend towards a reduction in the risk of adverse cardiovascular events, but also a dose-dependent increase in clinically significant bleeding [31].
The EINSTEIN-DVT study analyzed the effects of rivaroxaban at a dose of 15 mg twice daily for 3 weeks, then 20 mg once daily for up to 12 months. The study included 2900 patients with acute DVT but without PE; the effects of rivaroxaban were compared with those of warfarin (www.clinicaltrials. identifier: NCT00440193).
The EINSTEIN-PE study, identical in design to EINSTEINDVT, included 3300 patients with PE (identifier: NCT00439777). Final results from both EINSTEIN-DVT and EINSTEIN-PE have not been reported (as of June 2010), but results from the preliminary EINSTEIN-EXTENSION trial (ID: NCT00439725), in which patients received rivaroxaban 20 mg/day compared with placebo were presented in 2009 at the annual meeting of the American Society of Hematology [32]. According to the results of a study of 1197 patients with an average treatment duration of 190 days, recurrent VTE was recorded in 7.1% of cases in the placebo group and in 1.3% of patients receiving rivaroxaban (p < 0.001) [32]. There was no significant difference in the incidence of major bleeding, while clinically significant minor bleeding was observed in 1.2% of cases in the placebo group in 5.4% of patients receiving thromboprophylaxis with rivaroxaban [32].
Advantages and disadvantages of direct anticoagulant drugs
Over the past 6 years, new direct anticoagulants have appeared on the pharmaceutical market. They are an alternative to vitamin K antagonists for the treatment of thromboembolism and the prevention of thrombosis. Direct oral anticoagulants (DOAs) are a more effective and safer analogue of vitamin K antagonists.
Direct anticoagulants are the only alternative to vitamin K antagonists
The popularity of PPA among cardiologists and patients is not surprising, because the advantages include:
- rapid onset of action;
- relatively short half-life;
- the presence of specific antidote agents (may be useful in the treatment of acute ischemic strokes, as well as for eliminating post-stroke negative symptoms);
- fixed dosage;
- no direct effect of dietary supplements on the daily dose of the drug;
- no need to undergo regular laboratory blood monitoring.
The most common side effect that occurs after taking DOACs is an increased risk of bleeding. But the perceived threat of severe bleeding is quite small compared to the benefits provided by direct anticoagulants.
Possible complications of anticoagulant therapy
The main side effect of oral anticoagulant therapy is bleeding, which can manifest itself in the form of prolonged bleeding from wounds and cuts, nosebleeds, bruising on the body, changes in the color of urine (pink or red) and stool (black, bloody), etc. These complications are rare but can be very dangerous.
The risk of complications increases significantly if the INR goes beyond the individual “corridor”. Thus, your efforts should be aimed at maintaining blood clotting within the boundaries of your “corridor”.
Factors that may increase the risk of bleeding:
- Concomitant illnesses (even the common cold)
- Use of other drugs that affect blood clotting
- Inaccurate adherence to instructions for use
Symptoms that should be reported to your doctor immediately:
- Black coloring of the chair
- Pink or red urine
- Vomit that resembles “coffee grounds”
- Easily occurring bruises and swelling on the body for no apparent reason
- Nosebleeds
- Excessive bleeding from the gums (especially noticeable when brushing teeth)
- Prolonged bleeding from minor wounds and cuts
And:
- The appearance of shortness of breath, palpitations, chest pain
- Dizziness, difficulty speaking
- Visual impairment
- Numbness or impaired movement of one or more limbs
- Cold snap, pain in limbs
- Stomach ache
- A sharp increase in body weight
- Edema of the lower extremities
Trade names of direct anticoagulants and their mechanism of action
The classification of direct-acting drugs is a little more extensive. Dabigatran etexilate (trade name Pradaxa) is a direct thrombin inhibitor. This drug was the first direct oral anticoagulant approved by the medical community. Literally within a few years, rivaroxaban inhibitors (xalerto and edoxaban) were added to the list of direct anticoagulants. Long-term clinical trials have shown the high effectiveness of the above drugs in the prevention of stroke and treatment of thrombosis. DOACs have clear advantages over warfarin, and most importantly, the drugs can be administered without regular monitoring of blood counts.
Pradaxa is the most studied direct-acting anticoagulant
The mechanism of action of DOACs differs significantly from the mechanism of vitamin K antagonists. Each direct anticoagulant contains small molecules that selectively bind to the catalytic site of thrombin. Because thrombin promotes coagulation by converting fibrinogen into fibrin filaments, dabigatran has the effect of blocking these fibrin filaments.
Additional effective mechanisms of direct anticoagulants include platelet deactivation and reduction of blood clotting activity. The half-life of this group of drugs is 7-14 hours, the time for the onset of the therapeutic effect ranges from one to four hours. Direct anticoagulants accumulate in the liver with the formation of active metabolites and are excreted from the body in the urine.
Also, two types of heparins are used as anticoagulants - unfractionated (UFH) and low molecular weight (LMWH). Low-fraction heparin has been used for the prevention and treatment of mild thrombosis for several decades. The disadvantages of UFH are that it has a variable anticoagulant effect, as well as limited bioavailability. Low molecular weight heparin is obtained from low-fraction heparin by depolymerization.
Low molecular weight heparin has a specific molecular weight distribution, which determines its anticoagulant activity and duration of action. The advantage of LMWH is that you can easily calculate the required dosage and not have to worry about severe side effects. For these reasons, it is the low molecular weight heparin that is used in most hospitals around the world.
Heparin solution is used as an anticoagulant.
Consistency and regularity are essential for effective treatment with direct anticoagulants. Because this type of drug has a short half-life, patients who miss doses intentionally or accidentally are at risk for thrombosis or inadequate coagulation. Considering that the positive effect of taking PPA quickly disappears when the drug stops entering the body, it is extremely important to follow the dosage schedule prescribed by your doctor.
Principles of antithrombotic therapy in children
According to the literature, thrombosis of vessels of various locations has been diagnosed in children more and more often in recent years, while thrombotic and thromboembolic complications are increasingly among the causes of disability and mortality in patients. Thus, the prevalence of venous thrombosis in children in Denmark and the Netherlands is 1.4 cases [33], in Canada and Hong Kong - 0.70–0.74 cases per 100,000 children per year, respectively [15, 19]. The incidence of strokes in children aged 1 to 18 years ranges from 1.29–13.0 per 100,000 children per year, and in newborns reaches 25.0 per 100,000 per year, while in half of the cases the stroke is ischemic nature [34]. Clinically manifest signs of various thrombotic complications are observed in 5.3 patients per 10,000 children hospitalized during the year [21].
Certain types of thrombosis are observed in children of different ages, but, summing up the data from a number of publications, we can conclude that the highest risk of their development is observed in children of the first year of life and in adolescents, especially girls. In most children, thrombotic events occur against the background of various diseases - congenital heart defects, rheumatic, infectious and oncological pathologies, after surgical interventions, trauma, etc. [22, 26].
Thrombophilia, characterized by activation of blood coagulation, can be caused by both genetically determined and acquired changes in the hemostatic system, determining an increased risk of developing thrombosis of vessels of various sizes in the patient. Among genetically determined changes, the most frequently diagnosed in children are thrombophilias associated with a deficiency of natural anticoagulants - antithrombin III (AT III), proteins C and S, resistance to activated protein C caused by a mutation in the factor V gene, and a mutation of the G20210A allele in the prothrombin gene. Thrombophilia can also be determined by other genetically determined disorders of hemostasis: high levels of plasminogen activator inhibitor 1, plasminogen deficiency, heparin cofactor II deficiency, etc. Homozygous forms of some of these mutations are associated with the possibility of developing thrombosis in children already in the newborn period (fulminant purpura of newborns) . It has been shown that thrombosis in children with genetically determined thrombophilias in most cases occurs when exposed to additional risk factors. But patients with heterozygous forms of mutations also require preventive antithrombotic therapy if they are expected to be exposed to certain previously known risk factors, for example, surgery.
Among acquired changes, thrombophilias caused by immune factors are most often observed in children. Specialists pay great attention to the study of a specific syndrome that occurs in the body when antibodies appear that have the ability to interact with antigenic determinants of membrane phospholipids and associated glycoproteins [11]. A clinical and laboratory symptom complex, pathogenetically associated with the synthesis of antiphospholipid antibodies (aPL) and characterized by venous and/or arterial thrombosis, in adult women, fetal loss syndrome (more than two cases of fetal loss) and often moderate thrombocytopenia, is called antiphospholipid syndrome (APS) [2, 6]. The cause of the development of thrombotic complications in children of different ages, including newborns, can be aPL. APS can be primary or secondary, developing against the background of various diseases. More often, thrombosis within the framework of APS is diagnosed in children against the background of rheumatic pathology, primarily with systemic lupus erythematosus, cancer and infectious diseases. In addition, thrombosis in children can be caused by metabolic (hyperhomocysteinemia, diabetes), medication and iatrogenic (bypass surgery, prosthetics) factors, etc.
To date, there has been an understanding of thrombosis in children as a multifactorial pathology, which determines its importance as a multidisciplinary problem that attracts the attention of specialists in various fields: pediatricians, neonatologists, pediatric rheumatologists, oncologists, infectious disease specialists, doctors in intensive care units, etc.
Anticoagulant therapy is necessary for the treatment and prevention of thrombotic complications, however, determining the tactics for its implementation in children is often difficult, due to a number of reasons. It has been established that the epidemiology of thrombosis and their localization in children and adults have significant differences. The principles of antithrombotic therapy in children were extrapolated from the recommendations of general practitioners; At the same time, it is obvious that when treating this population, important ontogenetic features of hemostasis should be taken into account, which relate to both the pathophysiology of the thrombotic process and the response to treatment. Indeed, the development of thrombosis and embolism in children occurs against the background of the emerging hemostasis system, which determines the characteristics of their pathogenesis, as well as the response of the child’s body to the pharmacological action of antithrombotic drugs. It has been established, in particular, that the distribution, binding and clearance of antithrombotic drugs have differences associated with age. There is no doubt that the frequency and range of intercurrent diseases, as well as their treatment, change significantly with the age of patients, while the effect of antithrombotic drugs depends significantly on the use of a large number of other drugs. It should be noted that antithrombotic drugs are not available in dosages or forms suitable for use in children, such as suspensions or liquids, and low molecular weight heparins (LMWHs) are typically packaged in standard adult dosage syringes. The nutritional characteristics of children of different ages, in particular the feeding of infants, determine significant differences in their supply of vitamin K, which determines the difficulties in developing standard recommendations for the use of oral anticoagulants in children of different ages. Finally, long-term anticoagulant therapy can be difficult due to the negative attitude of the child, which is most typical for adolescents or their parents, i.e., depends on social factors [20].
All of the above explains the fact that, despite the presence of fairly clear recommendations for the diagnosis, treatment and prevention of thrombotic complications in adults in pediatric practice, this problem has still not been solved. Recommendations for the treatment and prevention of thrombosis in children remain insufficiently substantiated and require further development.
As is known, pharmacological agents that affect the blood coagulation system are divided into three large groups: direct-acting anticoagulants, indirect-acting anticoagulants (ANDA) and antiplatelet agents. To correctly select the right drug, it is necessary to take into account the differences in thrombus formation in the arterial and venous beds: in arterial thrombosis, the leading factors are damage and dysfunction of the vascular wall and platelet activation, as well as vascular stenosis or vasoconstriction; with venous - systemic hypercoagulation, slowing and disruption of blood flow.
Antithrombotic drugs and their combinations are selected in accordance with the pathogenetic mechanisms.
Direct anticoagulants
Direct anticoagulants play an important role in the prevention and treatment of thrombotic complications. The most widely used in clinical practice around the world are heparins, which are glycosaminoglycans of varying molecular weight, consisting of sulfated residues of D-glucosamine and D-glucuronic acid. The mechanism of the anticoagulant action of heparins is due to the fact that they form a complex with antithrombin III, increasing the ability of the latter to inhibit thrombin, Hageman factor, factors IX, X, XI, etc.
Unfractionated heparin (UFH) is the main drug in this group, widely used to treat both adults and children. The tactics of using UFH in children should be based on monitoring the activated partial thromboplastin time (aPTT) in order to maintain it at a level 1.5–2.5 times higher than normal. Difficulties associated with monitoring UFH therapy are observed in children with APS in the presence of a lupus anticoagulant (a special group of aPL), which determines the prolongation of the aPTT.
UFH has a number of undesirable side properties that limit its use in clinical practice. Due to the heterogeneity of its structure, UFH has relatively low bioavailability (30%). In addition, UFH is influenced by the antiheparin platelet factor (factor IV), forming a heparin-factor complex. When antibodies to this complex appear, heparin immune thrombocytopenia may develop, which is associated with potentially the most dangerous form of thrombosis, which determines the need to control the number of platelets in the blood. One of the undesirable effects of UFH is the depletion of antithrombin III with long-term use of the drug in large doses, which can again lead to hypercoagulability and thrombosis. Treatment with heparins, including UFH, is associated with the risk of developing a number of complications, primarily bleeding. Other side effects of UFH include osteoporosis, alopecia, and possible hypersensitivity reactions.
Low molecular weight heparins (LMWH), produced by depolymerization of UFH, have a lower molecular weight. A change in the structure of the heparin molecule, i.e., a decrease in molecular weight by almost 3 times, entailed changes in its pharmacodynamics and pharmacokinetics. LMWHs have a higher bioavailability (about 98%) than UFH and a longer half-life. LMWHs bind less to various proteins and cells, i.e. their effect is more predictable. Unlike UFH, the renal clearance of LMWH significantly prevails over cellular clearance (which is important to consider in patients with renal failure). LMWHs, to a much lesser extent than UFH, bind to endothelial cells, which ensures their long-term circulation in the plasma (2–4 times longer). The antithrombotic effect of LMWHs mainly depends on their effect on factor Xa; LMWHs do not have antithrombin properties and, therefore, do not cause hypocoagulation. In addition, LMWHs promote the activation of fibrinolysis by releasing tissue plasminogen activator from the endothelium. Monitoring of LMWH treatment is based on the assessment of anti-Xa activity and is not required in most patients. Monitoring LMWH treatment is necessary in children, especially young children, in patients with impaired renal function (filtration less than 30 ml/min), in patients with cancer pathology and in the presence of a high risk of bleeding.
In general, LMWHs should be classified as the drugs of choice for the prevention and treatment of thrombotic complications, since they have a more predictable anticoagulant effect, have a long-lasting effect, which makes them possible to administer 1-2 times a day, and in most cases do not require regular laboratory monitoring. LMWHs are resistant to the action of antiheparin platelet factor, therefore they are approximately 10 times less likely than UFH to cause heparin-induced thrombocytopenia. LMWH contribute to the development of osteoporosis to a lesser extent than UFH [4, 23, 24, 32].
In recent years, LMWHs have become more accessible and are increasingly used as alternative drugs to heparin for both the treatment and prevention of thrombosis in children. According to the literature, LMWH in children is as effective and well tolerated as UFH, and is easier to use. The costs of purchasing LMWH are offset by simpler laboratory monitoring and a reduction in the length of stay of patients in the hospital.
Indications for the use of UFH and LMWH include all cases involving the need for emergency and intensive hypocoagulation: acute thrombosis requiring emergency medical intervention (deep venous thrombosis, thromboembolism of the pulmonary arteries and cerebral vessels, acute myocardial infarction and resulting thromboembolic complications), heart surgery and blood vessels, disseminated intravascular coagulation syndrome (DIC syndrome), etc.
Direct anticoagulants are used when carrying out extracorporeal methods (hemosorption, hemodialysis, peritoneal dialysis) in the presence of thrombinemia, which is diagnosed taking into account the indicators of fibrinopeptide A, D-dimer, prothrombin fragments 1+2, thrombin-antithrombin III complex, soluble fibrin-monomer complexes (RFMC) ), fibrinogen. Thrombinemia is an important predictor of thrombotic risk, and dynamic monitoring of its severity is an effective method for assessing treatment. A significant increase in the level of D-dimer, thrombin-antithrombin III complex and prothrombin fragments 1+2 are observed in thrombosis, pulmonary embolism, and already in the initial stages of DIC syndrome, which determines the diagnostic significance of these markers. However, it should be noted that the study of D-dimer is of limited value for diagnosing thrombosis in newborns, since significant fluctuations in its level at this age are also observed in healthy children [10].
UFH is preferable in difficult cases where there is a high risk of bleeding and the need for rapid cessation of heparin therapy. UFG is used for extracorporeal circulation in cardiac surgery, and control is based on assessment of blood coagulation directly at the patient's bedside.
LMWH are widely used for the prevention of thrombosis in heart defects, for the prevention and treatment of venous thromboembolism in adults. Meta-analysis data suggest that LMWHs are more effective as initial therapy for venous thromboembolism in adults than UFH, as they provide a significantly lower incidence of major bleeding at the beginning of treatment and higher rates of overall survival [31]. The benefits of LMWH have also been noted in children with severe venous thrombosis [9]. It should be emphasized that the optimal duration of anticoagulant therapy after an episode of venous thrombosis should be determined individually, taking into account an assessment of the risk of recurrent thrombosis upon cessation of treatment and the risk of bleeding during further treatment; in particular, the longest therapy is indicated for children in the presence of aPL and malignant neoplasms [12] .
Contraindications for the use of direct anticoagulants are hypocoagulation of various origins (hemophilia, etc.), bleeding, peptic ulcer of the stomach or duodenum, ulcerative colitis in the acute stage with the risk of bleeding, a history of heparin-induced thrombocytopenia for UFH, severe dysfunction of the liver and kidneys .
Indirect anticoagulants
AEDs are the drugs of choice for long-term prevention of thrombotic complications. According to the recommendations, adult patients with venous thromboembolism receive intravenous UFH or subcutaneous LMWH for at least 5–7 days, then switch to treatment with vitamin K antagonists for 3 or more months [30]. Currently, warfarin is recognized as the “gold standard” of drugs in this group due to its lower toxicity, rapid action and short (about 2 days) aftereffect. Warfarin is a coumarin derivative. The main mechanism of its action is the blockade of the final stage of synthesis (γ-carboxylation) in liver cells of vitamin K-dependent blood coagulation factors - factors VII, X, IX and II (prothrombin), as well as to a lesser extent of two anticoagulants - proteins C and S Under the influence of AED, inactive protein molecules of factors VII, X, IX and II are formed that are not involved in the blood coagulation process, resulting in hypocoagulation, which prevents the formation of thrombin, the development and progression of thromboembolism. The rate at which the activity of the above factors decreases is not the same. The activity of factor VII decreases first, and prothrombin decreases last (about 4 days after starting the drug). In recent studies, it has been established that in order to achieve a more pronounced antithrombotic effect, it is the reduction in plasma prothrombin levels that is of paramount importance [18], therefore, when transferring a patient from treatment with UFH or LMWH to maintenance therapy or prophylaxis with warfarin, it is important to prescribe the latter within 4–5 days before discontinuation of heparins to select the optimal dose of the drug.
The therapeutic and prophylactic use of warfarin should be accompanied by systematic laboratory monitoring. The goal of laboratory monitoring in the treatment of AEDs is the need to achieve and maintain the hypocoagulative effect of these drugs at the desired level with a minimal risk of developing hemorrhagic complications. In 1937, AJ Quick et al proposed using prothrombin time to assess the degree of hypocoagulation [27]. Nowadays, the results of a prothrombin test are usually assessed using an indicator - the International Normalized Ratio (INR) (INR - International Normalized Ratio). INR allows for a mathematical correction that standardizes the prothrombin time of various thromboplastins that have different sensitivities. Oral anticoagulants are increasingly used in pediatric practice, so it is necessary to expand the capabilities of laboratory monitoring of children in the community and their self-control.
Individual sensitivity to warfarin is primarily due to the polymorphism of cytochrome P450СYP2C9, which is a key enzyme in the oxidation and clearance of warfarin [6]. The pharmacokinetic properties of warfarin depend on the structural polymorphism of the cytochrome CYP2C9 gene, which metabolizes warfarin. The catalytic activity of CYP2C9 is a decisive factor in determining the concentration of warfarin in blood plasma. To date, six variants of structural polymorphism have been identified. These allelic variants of the gene are called СYP2C9*1 (“wild” allele), СYP2C9*2 (Arg144Cys) and СYP2C9*3 (Ile 359Leu). The catalytic activity of the enzyme encoded by the СYP2C9*2 and СYP2C9*3 alleles is reduced relative to СYP2C9*1. It has been shown that the required daily dose of warfarin in carriers of the mutant alleles CYP2C9*2 and CYP2C9*3 is significantly lower than in individuals with the “wild” genotype [17], and the risk of developing hemorrhagic complications is higher. Patients with APS often exhibit resistance to warfarin, which is genetic in nature (mutation of coagulation factors V and II). In such situations, it is necessary to prescribe a dose of warfarin several times higher than usual. Determination of allelic variants CYP2C9*2 and CYP2C9*3 in patients is necessary to optimize the timing of selection of the required dose of warfarin and prevent the development of hemorrhagic complications. Thus, when examining 24 children with systemic lupus erythematosus in our clinic, allelic variants of CYP2C9*1, CYP2C9*2 and CYP2C9*3 were identified in 62.5, 25.0 and 12.5% of patients, respectively, which is comparable to the frequencies of allelic variants the CYP2C9 gene in the population in a study by O. V. Sirotkina and co-authors [3]. Warfarin therapy in these children required a strictly individual approach.
Treatment of thrombotic complications in children with oral anticoagulants has been the subject of active study and discussion over the past decade, but recommendations for the use of AEDs in children of different ages are still under development. Thus, the authors of prospective studies conducted in Canada and Argentina, emphasizing the difficulties of using warfarin in children, noted that patients under the age of 12 months require relatively large doses to achieve and maintain the INR in the required therapeutic interval, faster adjustment of therapy when the INR changes in In order to avoid drug overdose, more frequent laboratory monitoring when selecting a dose, and then less frequent monitoring when maintaining it [5].
In 2000, the VI Consensus Conference on Antithrombotic Therapy of the American College of Chest Physicians revised the range of therapeutic INR values and indications for the use of AEDs [25], in particular, establishing recommended INR values in patients with APS within 2.0–3.0 [ 25]. Data from prospective studies indicate that in patients with significant secondary and primary APS, when treated with high doses of warfarin, which allows maintaining a hypocoagulation state at the level of 3.0–4.0 according to INR, there is a significant decrease in the frequency of recurrent thrombosis [8], associated however, with the development of hemorrhagic complications. Meanwhile, researchers have recently found that treatment with a relatively low dose of warfarin (INR range 1.5–2.5) is as effective in preventing recurrent venous thrombosis in APS as the use of higher doses of the drug [1].
If it is impossible to use warfarin, long-term prophylaxis of thrombosis can be carried out with LMWH. LMWH treatment is safer than vitamin K antagonist therapy and is therefore preferable for some patients who live in remote locations, are unwilling to undergo regular laboratory monitoring, or have contraindications to the use of vitamin K antagonists. Meta-analysis data suggest that LMWH are as effective as and warfarin in preventing recurrence of venous thrombosis, but are more expensive [16, 30].
Antiplatelet agents are drugs that reduce the functional activity of platelets and are used to prevent and relieve thrombosis in the arterial and microcirculatory beds. Antiplatelet agents used in clinical practice include three main groups of drugs: acetylsalicylic acid (ASA), thienopyridines, and platelet glycoprotein IIb/IIIa receptor blockers. The effectiveness of treatment with antiplatelet drugs is judged on the basis of a study of the adhesive-aggregation activity of platelets over time. The criteria for the effectiveness of ASA therapy, according to the aggregogram, are a decrease in collagen and adenosine diphosphate (ADP)-induced platelet aggregation by up to 20%; for thienopyridines - a decrease in ADP-induced platelet aggregation.
Antiplatelet agents can be used alone or as an addition to anticoagulants. ASA is the most widely used antiplatelet agent; for adults the recommended dose of the drug is 75–150 mg/day, for children - 1.5 mg/kg/day [14]. The results of a prospective multicenter study demonstrated similar effectiveness of ASA and LMWH in preventing recurrent thrombosis in children with ischemic stroke [29]. At the same time, there are reports about the possibility of combination therapy with AED and low doses of ASA when warfarin monotherapy is insufficiently effective [28]. One of the problems forcing the search for new antiplatelet drugs is resistance to ASA, characterized by the inability of the drug to prevent the development of thrombotic complications by adequately suppressing the production of thromboxane A2. Resistance to ASA is detected in 5–45% of patients, both among various groups of patients and in healthy individuals. Among the reasons for resistance to ASA are considered: polymorphism and/or mutation of the cyclooxygenase-1 gene; the possibility of thromboxane A2 formation in macrophages and endothelial cells via cyclooxygenase-2; polymorphism of platelet IIb/IIIa receptors; activation of platelets through other pathways that are not blocked by ASA.
Thienopyridines (ticlopidine, clopidogrel) inhibit the ADP-dependent pathway of platelet aggregation, their effect occurs more slowly than ASA, so loading doses of drugs are used at the beginning of therapy. Undesirable side effects of thienopyridines include the possibility of thrombocytopenic purpura and neutropenia at the beginning of treatment with subsequent relapses, which are less common during treatment with clopidogrel. Clopidogrel is used as an alternative drug to ASA when it is impossible to use the latter, for example, in cardiac surgery.
Different mechanisms of antiplatelet action of thienopyridines and ASA provide the possibility of combined use of these drugs. Thus, the results of various international multicenter randomized studies confirmed the advantages of combination therapy with clopidogrel in combination with ASA compared with monotherapy with ASA or ASA and placebo in adult patients with cardiovascular diseases and showed good tolerability of the drug [13]. Difficulties in the use of thienopyridines in pediatric practice are associated with the lack of developed doses for children. However, an analysis of the experience of using clopidogrel in 15 children with heart defects at a children's hospital in Toronto [7] in doses of 1–6 mg/kg/day for 1–6 months demonstrated the promise of using the drug for the prevention of recurrent thrombosis with a relatively low incidence of complications . The authors cite 1 mg/kg/day as the starting dose of clopidogrel for children.
Among the new and promising drugs, blockers of glycoprotein IIb/IIIa receptors are considered, which prevent the formation of platelet bonds with fibrinogen and fibronectin, affecting the main mechanism of platelet aggregation. Studies have shown the high effectiveness of these drugs in adult cardiac patients, but there is practically no information on the use of such drugs in children. In the available literature, we came across only one report on the successful use of abciximab in the complex treatment of children with Kawasaki disease. The authors noted that the addition of the drug to standard therapy was accompanied by a large regression in the diameter of coronary artery aneurysms in the early stages of the disease [20].
Thus, the treatment and prevention of thrombotic complications represent one of the most pressing multidisciplinary problems of modern pediatrics, which has not yet been resolved. The need to improve medical care for children requires attracting the attention of pediatricians to the search for the most optimal anticoagulant therapy regimens for children of different ages.
Literature
- Alekberova Z. S., Reshetnyak T. M., Kosheleva N. M. et al. Antiphospholipid syndrome in systemic lupus erythematosus: assessment of diagnostic and classification criteria // Clinical Medicine. 1996. No. 6. pp. 39–42.
- Nasonov E. L., Ivanova M. M. Antimalarial (aminoquinoline) drugs: new pharmacological properties and prospects for clinical use // Clinical pharmacology. Therapy. 1998. No. 3. P. 65–68.
- Sirotkina O. V., Ulitina A. S., Taraskina A. E., Kadinskaya M. I., Vavilova T. V., Pchelina S. N., Shvarts E. I. Allelic variants СYP2C9*2 and СYP2C9*3 cytochrome gene CYP2C9 in the population of St. Petersburg and their clinical significance during anticoagulant therapy with warfarin // Russian Journal of Cardiology. 2004. No. 6. pp. 47–50.
- Shilova A. N., Khodorenko S. A., Vorobyov P. A. et al. Comparative study of the effectiveness of the prophylactic use of unfractionated and low molecular weight heparins in the surgical treatment of cancer patients // Clinical gerontology. 2002. T. 8. No. 4. P. 11–17.
- Bonduel MM Oral anticoagulation therapy in children//Thromb. Res. 2006: 118: 85–94.
- Crowther MA, Ginsberg JS, Julian J. et al. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome//New. Engl. J. Med. 2003; 349:1133–1138.
- Finkelstein Y., Nurmohamed L., Avner M. et al. Clopidogrel use in children//J. Pediatr. 2005; 147:657–661.
- Harrison L., Johnston M., Massicotte MP et al. Comparison of 5-mg and 10-mg loading doses in initiation of warfarin therapy//Ann. Intern. Med. 1997; 126:133–136.
- Jilma B., Kamath S., Lip GYH Antithrombotic therapy in special circumstances. II — In children thrombophilia, and miscellaneous conditions//BMJ. 2003; 326:37–40.
- John CM, Harkensee C. Thrombolytic agents for arterial and venous thromboses in neonates//The Cochrane Database of Systematic Reviews. 2005; 25: CD004342.
- Kandiah DA, Krilis SA Immunology of antiphospholipid antibodies and their interaction with plasma proteins//Lupus. 1996; 5: 153–155.
- Kearon C. Duration of anticoagulation for venous thromboembolism//J. Thrombosis. Thrombolysis. 2001; 12:59–65.
- Keller TT, Squizzato A., Weeda VB, Middeldorp S. Clopidogrel and aspirin versus aspirin for preventing cardiovascular disease in those at high risk//The Cochrane Database of Systematic Reviews 2005; 1:CD005158.
- Kutteh WH Antiphospholipid antibodies and reproduction//J. Reprod. Immunol. 1997; 35: 151–171.
- Lee ACW, Li CH, Szeto SC, Ma ESK Symptomatic venous thromboembolism in Hong Kong Chinese Children//Hong Kong Med. J. 2003; 9:259–262.
- Merkel N., Gunther G., Schobess R. Long-term treatment of thrombosis with enoxaparin in pediatric and adolescent patients//Acta. Haematol. 2006; 115:230–236.
- Miners JO, Birkett DJ Cytochrome P. 450 CYP2C9: an enzyme of major importance in human drug metabolism//Br. J. Clin. Pharmacol. 1998; 45:25–538.
- Mitchell L., Abshire T., Hanna K. et al. Supranormalizing antithrombin levels is safe in children with acute lymphoblastic leukemia treated with L-asparaginase: results of the PARKAA study [abstract]//Blood. 1999; 94 (suppl): 27.
- Monagle P., Adams M., Mahoney M. et al. Outcome of pediatric thromboembolic disease: a report from the Canadian Childhood Thrombophilia Registry//Pediatr. Res. 2000; 47: 763–766.
- Monagle P., Chan A., Massicotte P., Chalmers E., Michelson AD, Antithrombotic Therapy in Children: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy // Chest. 2004; 126:645–687.
- Nowak-Gottl U., Duering C., Kempf-Bielack B., Strater R. Thromboembolic diseases in neonates and children//Pathophysiol. Haemost. Thromb. 2003/2004; 33:269–274.
- Ogasawara M., Aoki K., Matsuura E., Kunimatsu M. Anticardiolipin antibodies in patients with pregnancy loss induse factor Xa production in the presence of beta 2-glycoprotein I//Amer. J. Reprod. Immunol. 1995; 34: 269–273.
- Perona A., Galligani L. The clinical syndrome associated with antiphospholipid antibodies. A diagnosis to be confirmed after a long follow-up//Minerva. Pediatr. 1995; 47:39–41.
- Petri M. Evidence-based management of thrombosis in the antiphospholipid antibody syndrome//Curr. Rheumatol. Report. 2003; 5:370–373.
- Severin T., Sutor A.H. Heparin-induced thrombocytopenia in pediatricsn//Semin. Thromb. Hemost. 2001; 27:293–299.
- Solymar L., Rao PS, Mardini M. et al. Prosthetic valves in children and adolescents//Am. Heart. J. 1991; 121:557–568.
- Stein PD, Alpert JS, Bussey HI, Dalen JE, Turpie AG Antithrombotic therapy in patients with mechanical and biological prosthetic heart valves//Chest. 2001; 119(Suppl): 220–227.
- Steward DJ, Haining RL, Henne KR et al. Genetic association between sensitivity to warfarin and expression of CYPC9*3//Pharmacogenetics. 1997; 7:361–367.
- Strater R., Kurnik K., Heller C. et al. Aspirin versus low-dose low-molecular-weight heparin: antithrombotic therapy in pediatric ischemic stroke patients: a prospective follow-up study//Stroke. 2001; 32:2554–2558.
- Van der Heijden JF, Hutten BA, Buller HR, Prins MH//Vitamin K antagonists or low-molecular-weight heparin for the long term treatment of symptomatic venous thromboembolism//The Cochrane Database of Systematic Reviews. 2001; 1:CD002001.
- Van Dongen CJJ, van den Belt AGM, Prins MH, Lensing AWA Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism//The Cochrane Database of Systematic Reviews. 2004; 18: CD001100.
- Von Landenberg P., von Landenberg C., Scholmerich J., Lackner KJ Antiphospholipid syndrome. Pathogenesis, molecular basis and clinical aspects//Med. Clin. 2001; 96:331–342.
- Van Ommen CH, Heijboer H, Buller HR et al. Venous thromboembolism in childhood: a prospective two-year registry in the Netherlands//J. Pediatr. 2001; 139:676–681.
- Williams AN Childhood stroke: beyond re-inventing the wheel//Eur. J. Paediatr. Neurol. 2000; 4: 103–107.
N. S. Podchernyaeva , Doctor of Medical Sciences, Professor M. F. Mehrabyan N. D. Vashakmadze S. G. Nesterov MMA named after. I. M. Sechenova, Moscow
Is it possible to combine direct and indirect anticoagulants?
As has already become clear, anticoagulants are used for therapeutic and prophylactic purposes for heart attacks, angina pectoris, vascular embolism of various organs, thrombosis, and thrombophlebitis. In acute conditions, direct anticoagulants are usually prescribed, which provide an immediate effect and prevent blood clotting. After 3-4 days (subject to the success of primary treatment), therapy can be enhanced with indirect anticoagulants.
Combined anticoagulant therapy is also carried out before operations on the heart and blood vessels, during blood transfusions, and also for the prevention of thrombosis. Treatment with a combination of different types of anticoagulants should be carried out under the constant supervision of medical professionals. Due to the increased frequency of angina attacks and paroxysmal atrial fibrillation, when treated with two types of drugs simultaneously, the presence of sediment in the urine, the rate of blood clotting and the level of prothrombin in the blood are constantly monitored.
Combined anticoagulant therapy should occur under medical supervision
Treatment with a combination of different anticoagulants is contraindicated in:
- hemorrhagic diathesis;
- diseases accompanied by decreased blood clotting;
- during pregnancy;
- liver and kidney dysfunction;
- malignant neoplasms;
- peptic ulcer disease.
It is also necessary to urgently interrupt combination therapy if blood appears in the urine.
Prescription of medications, indications and contraindications
Medicines are manufactured in tablets, injection solutions, ointments, and gels. Anticoagulants are intended to treat and prevent the formation of blood clots. Active components affect the production of elements of the coagulation system, reduce the rate of formation of blood clots settling on the inner surface of blood vessels.
Anticoagulant medications are prescribed:
- for acute venous thrombosis;
- preventing the occurrence of thromboembolism - when replacing heart valves, supraventricular tachyarrhythmia;
- heart attacks, blockages of arterial vessels in the lungs;
- ischemic strokes;
- atherosclerotic vascular damage;
- injuries, shock, septic lesions;
- varicose veins;
- hemorrhoids with blood clots;
- formation of blood clots in the IVC.
Medications are not used:
- with lactose deficiency, impaired absorption of galactose, glucose;
- gastrointestinal ulcers, aneurysms;
- renal, liver pathologies;
- bleeding, thrombocytopenia.
The simultaneous use of anticoagulants with Aspirin, Penicillin, Dipyridamole, Cimetidine and other representatives of the NSAID group is prohibited.
During therapeutic procedures, adverse reactions may occur, which occur due to incorrectly selected doses of drugs or violation of the treatment regimen. General symptoms include attacks of nausea with vomiting, diarrhea, pain in the abdomen, allergies with nettle fever. Sometimes massive hair loss and necrosis begin.
How to determine the effectiveness of taking anticoagulants?
Indirect coagulants are easy to detect in the blood and even measure their effectiveness. For this purpose, a special indicator called “international normalized ratio” has been developed.
- A person not taking indirect anticoagulants will have an INR just below 1.
- A patient taking warfarin will have an INR between 2.0 and 3.0. Seeing such high numbers, doctors will be prepared for the possibility of sudden bleeding.
- An INR between 1 and 2 will indicate that the patient may be at risk of developing an ischemic stroke.
- With an INR of 4 or higher, there is the greatest risk of blood non-coagulation and the development of hemorrhagic stroke.
A blood test for INR is indicative of therapy with indirect anticoagulants
But a blood test for INR will not provide objective indicators if the patient is taking direct anticoagulants. The biggest problem with the newer direct anticoagulants is the lack of a reliable way to assess their effectiveness. Doctors can tell when bleeding stops, but there is no indicator that assesses the presence of anticoagulant effects. For example, this is very important when treating patients who are admitted to the emergency room in an unconscious state. If the medical record does not indicate any information about the patient taking direct-acting anticoagulants, it is quite difficult to quickly detect them in the blood.
What to do in case of overdose?
Despite all of the above benefits, doctors are still concerned about the lack of specific antidotes to use in the event of an overdose. To prevent such a serious condition, doctors adhere to the following rules:
- reduce the dose of epobaxan after 7 days of use;
- Xalerto requires a dose reduction after a course of 21 days.
Currently, when life-threatening bleeding occurs, including those caused by indirect anticoagulants, the patient is administered fresh frozen plasma, prothrombin complex concentrate, and Phytonadione.
Phytonadione is one of the few antidotes to anticoagulants
The pharmacology and mechanism of action of each antidote are different. Different anticoagulants will require different doses and strategies for administering antidotes. The duration of the course and dosage of antidotes is calculated depending on how the patient reacts to the drugs already administered (there are cases when some antidotes not only stop bleeding, but also activate platelet aggregation).
Mortality rates with DOACs and VKAs
Patients receiving direct anticoagulants to prevent complications of heart disease had a higher incidence of sudden bleeding, but at the same time lower mortality rates, compared with patients who received vitamin K antagonists. It should not be concluded that the presence of bleeding is what - thus helping to reduce mortality rates.
These conflicting results are due to the fact that most studies are conducted in hospital settings. All bleeding that occurs when the patient is in the hospital and receives direct anticoagulants through an IV is very quickly stopped by qualified medical personnel and does not lead to death. But the patient most often takes indirect anticoagulants without medical supervision, which leads to a higher mortality rate.