Bronchiectasis is an expansion of a separate section of the bronchi with changes in structure and function. Bronchiectasis is not an independent disease, but occurs as a result of many other diseases and conditions.
Bronchiectasis increases the patient's susceptibility to respiratory tract infections, which leads to frequent exacerbations and progression of the disease. Thus, bronchiectasis is a chronic progressive bronchopulmonary disease that requires constant medical supervision and supportive treatment, the volume of which increases with exacerbations.
Symptoms of bronchiectasis
Symptoms of bronchiectasis vary: from repeated episodes of respiratory tract infections, between which all symptoms of the disease completely disappear, to daily cough with sputum, the nature of which can vary from mucous (colorless) to mucopurulent (light yellow) and purulent (dark yellow, green or grey-green). Patients with bronchiectasis are characterized by a large volume of sputum - up to 100-200 ml per day, but sometimes the sputum is more scanty. From time to time, bloody streaks or clots may appear in the sputum, which is associated with trauma to the thinned bronchial wall during a hacking cough.
In rare cases, bronchiectasis is complicated by severe pulmonary hemorrhage requiring surgical intervention. When inflammation passes from the bronchial wall to the lung tissue, pneumonia can develop, and to the pleura - pain in the chest when breathing and coughing. In later stages of the disease, respiratory failure may develop.
Exacerbations of the inflammatory process in bronchiectasis are often accompanied by weakness, prolonged episodes of temperature (usually no higher than 37.2-37.50C), and weight loss.
Main cause of bronchiectasis
The immediate cause of stretching of the bronchial wall is repeated purulent inflammation. It is this that causes tissue destruction, loss of strength and elasticity. Factors causing inflammation may be:
- biological (infectious pathogens, for example, cocci, Koch's bacillus, aspergillus, etc.);
- chemical (toxic impurities in the air, tobacco smoke, hydrochloric acid - when stomach contents enter the respiratory tract);
- physical (compression by a tumor).
Immunodeficiency conditions (for example, AIDS) are also predisposing factors to the appearance of bronchiectasis.
If the dilation of the bronchi is congenital or manifests itself independently in childhood, it is customary to talk about the so-called. bronchiectasis. In these cases, bronchiectasis is accompanied by such pathological conditions as:
- hereditary diseases (Duncan, Kartagener, Williams-Campbell, Shwachman-Diamond syndromes, cystic fibrosis);
- intrauterine infection with the Epstein-Barr virus.
Diagnosis of bronchiectasis
Bronchiectasis is detected by high-resolution computed tomography (CT) of the lungs. Conventional radiography, and especially fluorography, are not sensitive enough to diagnose this disease. According to CT scans of the lungs, it is sometimes possible to determine the cause - in congenital malformations of the lungs, tracheobronchomegaly, emphysema, tuberculosis, etc.
As a rule, to establish the cause, additional studies are required, the range of which can be quite wide, determined by the doctor during a conversation with the patient (collection of complaints and anamnesis), as well as based on the results of a CT scan of the lungs. Thus, if genetic diseases are suspected, a genetic analysis is carried out; if a fungal infection of the lungs is suspected, immunological studies (determination of antibodies to fungi) and special sputum cultures for fungal flora are performed.
What other studies are used in diagnosis?
Mandatory studies in patients with bronchiectasis are bacteriological analysis of sputum and a study of respiratory function (spirography, respiratory function or body plethysmography).
Bacteriological analysis of sputum (sputum culture)
Bronchiectasis creates ideal conditions for the colonization of various microorganisms - the constant presence of bacteria on the surface of the bronchial mucosa in bronchiectasis. Long-term colonization of bacteria can cause inflammation even in the absence of other provoking factors (hypothermia, ARVI, etc.). This inflammation is manifested by frequent or persistent bronchitis with fever, weakness, sweating, and weight loss.
If the bacteria are not or cannot be removed from the bronchial tree, the inflammation becomes chronic with constant production of purulent sputum and lung damage. That is why it is important to regularly conduct bacteriological examination of sputum in order to control the composition and number of microorganisms present in the bronchi.
Pulmonary function test (PRF)
With chronic inflammation, the lumen of the bronchi narrows due to swelling of the bronchial mucosa, accumulation of mucus in the lumen of the bronchi, and sometimes bronchospasm (contraction of the muscles of the bronchial wall) can develop.
All these processes narrow the lumen of the bronchi and can cause shortness of breath. To diagnose these conditions, various methods of studying the function of external respiration are used. The simplest and most accessible method is spirometry, but more complex research methods are often required - measuring lung volumes (body plethysmography) and assessing the diffusion capacity of the lungs (the ability to pass oxygen from inhaled air into the blood). The results of these studies are important for prescribing treatment for a patient with bronchiectasis.
Bronchiectasis - symptoms and treatment
The treatment of bronchiectasis is based on the principle of timely anti-inflammatory and drainage therapy , which is aimed at evacuating secretions from the dilated bronchi. The minimal invasiveness of the procedures is also important, since each episode of penetration of foreign objects (including endoscopic tubes) into the lungs increases the risk of additional infection of damaged areas of the bronchi.
Drug treatment
Currently, the safest and most effective is the inhalation form of delivering medicinal solutions to the lungs. For this purpose, nebulizers are used - devices that spray drug solutions throughout the tracheobronchial tree [10].
With their help, both at home and in medical institutions, mucolytics are inhaled - drugs that dilute sputum and stimulate the work of the ciliated epithelium that lines the lumens of the bronchi (for example, ambroxol solution). For anti-inflammatory purposes, inhalation of budesonide suspension is used to treat bronchiectasis; a compressor nebulizer is suitable for it. This drug is inhaled in courses, especially in the presence of bronchial obstruction (narrowing of the lumen of the bronchi) and associated shortness of breath with difficulty exhaling [10].
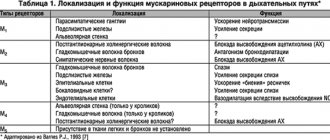
Expansion of the bronchial lumens is also achieved by inhalation of beta-2-agonists and M-anticholinergics and their combinations (salbutamol, ipratropium bromide, fenoterol) [10].
There are other inhaled drugs that do not require the use of a nebulizer: tiotropium bromide, umeclidinium bromide, formoterol, salmeterol, indacaterol, vilanterol. They are used in the form of powder, liquid inhalers, and aerosols. An important aspect is strict adherence to the inhalation technique, therefore, it is necessary to bring the device prescribed for treatment to each doctor’s appointment, which will allow you to check the process and promptly correct errors [10].
During exacerbations of bronchiectasis, the use of antibacterial drugs is indicated. Their use depends on the results of sputum cultures, as well as the timing and drugs of previous antibiotic therapy. Typically, beta-lactams (protected semi-synthetic penicillins, cephalosporins), drugs with antipseudomonal activity (fluoroquinolones, 3-4 generation cephalosporins, aminoglycosides) are used to treat bronchiectasis [11].
Instrumental methods
In the case of a severe form of the disease with frequent exacerbations, it is sometimes justified to conduct a series of sanitation bronchoscopy performed under local anesthesia. This will make it possible to cope with exacerbations more quickly [12]. The procedure must be performed in a hospital setting, less often on an outpatient basis.
Surgery
Surgical treatment methods are indicated for local processes in the following cases:
- the local process is accompanied by pulmonary hemorrhages;
- within two to three years it is not possible to achieve stable remission;
- development of local cirrhosis;
- pulmonary bleeding more than 200 ml/day cannot be treated with drugs.
Surgery is possible at any age. Surgeries for bilateral resection (removal of part of the lung) are usually performed at intervals of 6-8 months [7][8][9].
Maintaining proper nutrition
In the treatment of patients with bronchiectasis, along with other methods, therapeutic nutrition is of great importance. The diet should contain an increased amount of protein (up to 160 g), moderate amounts of fat and carbohydrates. It is necessary to include vitamins A, B1, B2 and C in the diet. Vitamin A helps improve the regeneration of the mucous membrane of the respiratory tract, vitamins B1, B2 and C improve oxidative processes and protein metabolism. Salt content is limited. Meals should be at least five times a day. Diet No. 5 with a high content of protein and vitamins is recommended.
Oxygen therapy
In the presence of chronic respiratory failure with a decrease in blood saturation to 89% or less, long-term oxygen therapy at home using oxygen concentrators is recommended. Also, situational oxygen therapy is carried out in a hospital setting at the stage of treatment of exacerbations of the disease, accompanied by a decrease in saturation to 95% or less.
Physiotherapy
During the period of exacerbation of the process, electrophoresis and UHF therapy are used on the chest - a low-thermal dose lasting 10-15 minutes. During the period of remission, general UV irradiation and inhalation of mucolytic agents are carried out. To improve the functional state of the lungs and the drainage function of the bronchi, chest massage is used. Vibration massage is carried out using a special vest or with direct percussion on the chest in a lying position in the direction from bottom to top. It is better to carry it out after the inhalation procedure in order to increase the rate of disintegration (breakdown) of sputum and its removal from the airways.
In case of illness, evacuation of bronchial secretions is important. To do this, static and dynamic postural drainage is used - adopting a body position in which coughing up sputum is most effective.
Exercise therapy
Therapeutic exercise should be carried out by a patient with bronchiectasis constantly. Exercises are used to increase the movement of the diaphragm and intercostal muscles in combination with postural drainage of the bronchi (body position for better sputum discharge depends on the location of bronchiectasis). Breathing exercises increase the pressure created in the lumen of the bronchi, promote their cleansing and more uniform filling with air during inhalation. Gymnastics can be done independently or with the connection of portable exercise machines, some of which can create additional vibration.
Contraindications for physical therapy: pulmonary hemorrhage; stage III cardiovascular failure; an increase in temperature to 38-39 ° C, not due to the accumulation of sputum. If there is sputum, therapeutic exercises begin with exercises that promote the removal of sputum: postural drainage is used; drainage exercises and their combination. When a large amount of sputum is produced, exercises that drain the bronchi are performed up to 8-10 times a day: in the morning before breakfast for 20-25 minutes, 2 hours after breakfast, lunch, every hour before dinner and an hour before bedtime.
Is it possible to cure the disease?
Bronchiectasis is a chronic progressive disease in which the quality of life of patients depends on the extent of lung damage, the degree of impairment of pulmonary function, the severity and frequency of exacerbations. There is no cure for this disease. But we are able to influence the rate at which the disease worsens. The rate of progression is largely determined by the nature of the chronic bronchial infection.
Thus, it is possible to slow down the progression of the disease and improve the patient’s quality of life with early diagnosis, identification and treatment of their cause, adequate treatment of chronic bronchial infections, prevention of exacerbations and regular medical supervision of the patient.
Are there surveillance programs for patients with bronchiectasis? Yes, they exist. Follow-up examinations with a doctor should be scheduled every 1 to 6 months, depending on the severity of the disease. Even if the patient’s condition is stable (in the remission phase), a general sputum analysis and bacteriological examination of sputum should be performed to assess the activity of inflammation in the bronchi. During the examination, the doctor should assess the severity of shortness of breath, the presence or absence of hemoptysis, general symptoms of inflammation (weakness, sweating, weight loss, temperature), listen to the lungs and, in case of severe impairment of pulmonary function, conduct a stress test (6-minute walk test).
Annual examination of a patient with bronchiectasis should include spirometry with a bronchodilator to assess the rate of decline in pulmonary function, a complete blood count with C-reactive protein (CRP) and immunoglobulin (Ig) A to assess the overall inflammatory response of the body.
At each visit to the doctor, it is advisable to measure saturation (oxygen saturation in the blood) using a pulse oximeter. If saturation decreases below 93%, it is recommended to perform a complete study of the gas composition of arterial blood to decide on the prescription of oxygen therapy.
For patients at high risk of disease progression, it is recommended to repeat CT scans of the lungs routinely once every 2 years. In addition, an X-ray of the lungs is performed annually, as well as if severe or life-threatening complications (pneumonia, pneumothorax) are suspected.
Rehabilitation, prevention, possible risks
An important component of complex rehabilitation for bronchiectasis is lifestyle correction. The patient needs to walk in the fresh air, quit smoking and avoid second-hand smoke, eat a balanced diet, exercise, and do breathing exercises regularly.
It is important to be registered with a pulmonologist, attend preventive appointments as often as prescribed by your doctor, and, if necessary, undergo physical therapy courses. Comprehensive prevention includes timely treatment of respiratory diseases and hardening.
Without adequate treatment of bronchiectasis, chronic bronchitis, pulmonary and heart failure, cor pulmonale, and bronchial asthma develop. Patients' performance decreases and their quality of life deteriorates. It is extremely important to consult a doctor in a timely manner in order to achieve long-term, sustainable remission.
Pulmonary rehabilitation for bronchiectasis
Our pulmonology department has developed a “Pulmonary Rehabilitation Program for Patients with Bronchiectasis.”
A course of complex therapy can replace bronchoscopic sanitation in patients with bronchiectasis.
- sputum becomes easily coughed up, coughing occurs naturally, medications are poured into the smallest bronchi, including antimicrobial agents.
- the introduction of drugs into the bronchus and removal of sputum is not invasive and traumatic.
- Due to the positive effect of drainage techniques and special exercises included in the course, lymphatic drainage of the bronchi and their blood supply improve. As a result, the protective properties of the mucous membrane of damaged bronchi and surrounding lung tissue are enhanced.
- There are no risks inherent in bronchoscopy: the risk of bleeding, damage and allergic reaction to anesthesia.
Bronchiectasis. Complications
The altered walls of the bronchi, which have lost their elasticity and strength, and have lost their natural defense mechanisms, are suitable soil for the rooting and growth of pathogens (both those present in the body and those coming from outside). As a result of repeated inflammations and subsequent destruction of bronchial tissue, the situation worsens and can lead to:
- bleeding;
- recurring bronchitis and pneumonia;
- emphysema;
- secondary amyloidosis.
And ultimately - to the progression of heart and pulmonary failure.
Treatment of bronchiectasis
Treatment of a patient with bronchiectasis is aimed at improving the condition, preventing exacerbations, and, consequently, progression of the disease.
If the cause of bronchiectasis is known, then treatment should be aimed at eliminating it.
The main components of success in treatment:
- adequate antibiotic therapy;
- powerful mucolytic (sputum thinning) therapy;
- bronchodilators;
- breathing exercises, breathing simulators;
- complete nutrition.
In some cases, mainly with a limited prevalence of bronchiectasis, surgical treatment (removal of the affected area of the lung) is possible in a thoracic department or surgical hospital. For this, a consultation with a thoracic surgeon will be necessary.
All patients with bronchiectasis should receive an influenza vaccine annually in the fall, and once every 5 years - the Pneumo-23 anti-pneumococcal vaccine. Of course, vaccination, like any method of treatment, has its contraindications, but modern vaccines reduce them to a minimum and make it possible to safely vaccinate the vast majority of patients, including patients with bronchial asthma and other allergic diseases.
How to treat pulmonary bronchiectasis
What is the purpose of therapy: healing or improving quality of life? It all depends on the duration, severity and nature of the process. If bronchiectasis is a complication of other diseases, then their timely treatment and activation of internal reserves can lead to partial or complete restoration of bronchial tissue. After all, our body sometimes demonstrates an amazing ability to regenerate.
In other cases, with periodic maintenance therapy, it is possible to compensate for existing disorders and improve the quality of life. Most often in modern medicine we mean drug treatment (immunomodulators, antibacterial agents, proteolytic enzymes and mucolytic agents, bronchoscopy, drainage of the trachea and bronchi). In severe cases, surgical treatment is required. There are effective ways to help yourself:
- breathing exercises;
- physical exercise;
- massage and self-massage;
- diet.
All of the above methods can be combined with traditional medicine methods - acupuncture, herbal medicine, homeopathy, osteopathy. The latter can also be used as an independent treatment for bronchiectasis, their causes and consequences.
Make an appointment
Our specialists
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
Nikitina Natalia Vladimirovna
Deputy chief physician, pulmonologist, allergist of the highest category. Full member of the European Academy of Allergy and Immunology.
Experience 15 years