Chronic obstructive pulmonary disease ranks 4th in the list of causes of death on our planet (data from the World Health Organization).
Unfortunately, it remains incurable today. However, modern medicine can slow the progression of the disease, reduce symptoms and improve quality of life.
In this article you will learn about modern scientifically proven methods of prolonging the life of patients, which are today recommended by leading pulmonologists in our country and around the world.
Fragment of the TV show “Live Healthy.” COPD The rights to the video belong to
OJSC “Channel One”. The full version of the TV show is available at this link.
Chronic obstructive pulmonary disease (COPD) is a multicomponent disease, which is based on chronic inflammation and narrowing of the small airways (bronchi) with the destruction of lung tissue (alveoli), the formation of its “overinflation”, which leads to cough, progressive shortness of breath and fatigue. . COPD is a serious disease that progresses over many years, accompanied by a lack of oxygen in the body. In the absence of necessary treatment, the consequences of COPD are disability and death.
Why might I develop COPD?
The most common cause of the development of this disease is smoking (cigarettes, hookah and other smoking mixtures). The smoke you inhale when smoking damages the bronchi and lung tissue (alveoli). Moreover, the damage is irreversible! The longer you smoke, the more pronounced changes occur in the respiratory system. It is very important to understand that passive smoking leads to the same consequences as active smoking.
Other reasons may be:
- work in hazardous production conditions (miners, welders, metallurgical and chemical industry workers);
- prolonged inhalation of smoke generated by the combustion of biofuels (wood, coal for stove heating);
- living in environmentally unfavorable conditions.
Symptoms of COPD.
It is very important to understand that in the initial stages of development, chronic obstructive pulmonary disease may not manifest itself in any way. Clinical manifestations usually occur with prolonged smoking. In some patients, symptoms appear earlier, in others later. Much depends on the hereditary predisposition to the development of this disease. You can easily remember people who smoked 1-2 packs of cigarettes a day for 50 years and did not have shortness of breath. Such exceptions only confirm the general rule. COPD is most likely to occur after 10 years of smoking 20 cigarettes a day.
The main symptoms of COPD are:
- cough (dry or with sputum), often in the morning;
- shortness of breath (difficulty breathing initially during physical activity, and as the disease progresses, shortness of breath will occur at rest);
- wheezing in the chest when breathing (appears in later stages of the disease).
Patients with COPD are also at high risk of:
- frequent exacerbations of chronic bronchitis (inflammation of the bronchi) and the occurrence of pneumonia (pneumonia);
- lung cancer;
- heart problems (myocardial infarction, heart rhythm disturbances);
Diagnosis of the disease
For diagnosis, you first need to consult a therapist. The specialist will conduct an examination and, if necessary, refer you to a pulmonologist. As a rule, the doctor prescribes several examinations:
- urine and blood tests - general;
- sputum analysis - cytological and bacteriological research;
- performing spirography;
- fluorographic examination (to exclude other pathologies);
- fibrobronchoscopy.
During diagnosis, doctors determine the volume of exhalation in a normal state and at an accelerated rate (within a second), and measure the maximum volume of the lungs (vital capacity). If the respiratory failure syndrome is clearly expressed, a blood test is additionally done to check for the presence of gases and determine their composition.
COPD classification:
- I – light;
- II – moderate;
- III – heavy;
- IV – extremely severe.
Chronic obstructive pulmonary disease is a progressive disease! Most patients consult a doctor at stages III and IV, when severe shortness of breath appears. In stages I and II, as a rule, there is no shortness of breath, and only a rare cough in the morning is bothersome, so the patient does not see a doctor. This is the insidiousness of the disease. Most patients present late, and valuable time for treatment is partially lost.
At each stage (I-IV) you can feel satisfactorily (as usual) - this is the phase of remission or imaginary recovery, when the manifestations of the disease are minimal. But with hypothermia or for no apparent reason, an exacerbation may occur.
Our specialists
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
Nikitina Natalia Vladimirovna
Deputy chief physician, pulmonologist, allergist of the highest category. Full member of the European Academy of Allergy and Immunology.
Experience 15 years
Why do people with COPD suffer from cough, shortness of breath and fatigue?
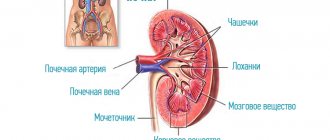
Harmful substances that a potential patient inhales for a long time act on the respiratory system in the following way: when they enter the small airways (bronchi), they maintain constant inflammation. This, in turn, leads to a gradual narrowing of the bronchi and the accumulation of mucus in them. The patient coughs up excess mucus (phlegm), most often in the morning. Narrowing of the bronchi and excessive accumulation of mucus (phlegm) makes it difficult for air to penetrate into the lung tissue (alveoli).
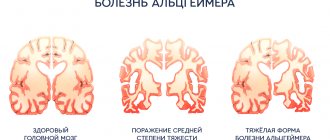
Lung tissue is a very fine sponge. If you expand each cell of this sponge, then in a healthy person the lung area will be comparable to a football field in a stadium. It is this huge area that makes it possible to effectively extract oxygen from the air. In a sick person, due to the action of harmful substances from tobacco smoke, the structure of the lungs is destroyed. The small sponge becomes coarse. If you expand each cell of such a sponge, then the total area of the lungs of a patient with COPD will be 5-10 times smaller than a football field. Therefore, the lungs of a patient with Chronic Obstructive Pulmonary Disease can no longer extract oxygen from the air as efficiently. A constant lack of oxygen in the body causes a painful feeling of shortness of breath (lack of air) and rapid fatigue, because muscles cannot work well in conditions of lack of oxygen.
Chronical bronchitis
| Long-term inflammation of the airways is characterized by excessive mucus production and a persistent cough. Damage to the bronchial tubes causes chronic bronchitis. Bronchitis occurs when the bronchi become irritated and swollen. This causes coughing and shortness of breath. If phlegm appears when you cough, and the cough continues for at least three months for two years in a row, bronchitis is called chronic. There are hair-like fibers lining the bronchi. These tiny hairs are called cilia. The cilia help move mucus down the bronchi so it can be coughed up. With chronic bronchitis, eyelashes lose their mobility. This makes it more difficult to cough up mucus from the lungs, causing a more severe cough. Mucus may accumulate in the lungs. Smoking interferes with the normal functioning of eyelashes. |
Are there accurate methods for diagnosing COPD?
Yes. The main diagnostic method is spirometry (respiratory function test). The essence of spirometry is that you will need to inhale as deeply as possible and then exhale into a special tube (spirometer) as powerfully and sharply as you can. A computer connected to a spirometer will measure and analyze how much air you exhaled and at what speed. If your spirometry readings are abnormal, the doctor or nurse will suggest you inhale the medicine through an inhaler. After about 15-30 minutes. spirometry will be repeated. This will help your doctor determine whether your symptoms (shortness of breath and cough) are due to COPD or another disease, such as asthma.
Causes of obstructive disease
The main cause of the development of pathology is chronic smoking. There are a number of other factors that can trigger the onset of COPD:
- abundance of exhaust gases, smoke, dust;
- air pollution from industrial waste;
- work in hazardous conditions (coal mine, hot shop, chemical industry);
- climatic features (dampness, constantly high humidity);
- infectious microorganisms (influenza virus, pneumococcus, mycoplasma bacteria and others);
- development of concomitant pathologies of the bronchi and lungs, especially bronchial asthma (including inherited).
Treatment of COPD. How to slow down the progress of the disease?
Quitting smoking is the only proven method that can slow the decline in lung function. Other treatment methods reduce the number of exacerbations and shortness of breath, but have a much worse effect on the progression of the disease. In people with chronic obstructive pulmonary disease who continue to smoke, the effectiveness of complex therapy is significantly less than in patients who quit this bad habit.
It is imperative to stop smoking. It doesn't matter how long or how much you smoke. Doctors who recommend you not to quit smoking, because... “You’ve been smoking for a very long time and you can’t quit, it’s dangerous,” deliberately (or because of your lack of education) worsen the prognosis for your illness. Quitting smoking will slow the progression of the disease, make you feel better, and greatly increase the effectiveness of other treatments.
Global Alliance to Fight Chronic Respiratory Diseases
The Global Alliance Against Chronic Respiratory Diseases (GARD) promotes WHO's work to prevent and control chronic respiratory diseases. GARD is a broad voluntary alliance of national and international organizations and institutions working towards the common goal of reducing the global burden of chronic respiratory diseases.
Bibliography
1. WHO Global Health Estimates
2. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2021 global survey. Geneva: World Health Organization; 2021. License: CC BY-NC-SA 3.0 IGO
Prevention of influenza and pneumococcal pneumonia
Because pulmonary infection is common in patients with COPD and can lead to deterioration of lung function and respiratory failure, annual influenza vaccination is recommended for patients who are not allergic to egg whites. Its effectiveness reaches 60-80%. Unvaccinated patients at high risk of influenza A and at an early stage are prescribed amantadine. For patients over 50 years of age, a single immunization with the pneumococcal vaccine is also recommended. Revaccination is now carried out after five or more years, if at the time of vaccination the patient’s age did not exceed 65 years.
Physiotherapy
Removing mucus from the respiratory tract can significantly improve the patient’s well-being, especially with the bronchitis type of COPD. There are many ways to clear mucus from your airways and prevent it from accumulating. Cough in patients with COPD, as a rule, does not remove sputum and is only exhausting. Such patients can be advised to use a simple and effective method of coughing up sputum, which, unfortunately, is often neglected. Its essence is as follows: after a couple of slow deep breaths, you need to hold your breath for 5-10 seconds to increase intrathoracic pressure and then, as you exhale, cough with an open glottis.
Postural drainage, vibration and percussion massage
facilitate the removal of mucus from the lower parts of the lungs due to the action of gravity and the oscillatory movements of the chest imparted to it during percussion or using a vibrator. Upon completion of the procedure, the patient should cough well, as described above.
All of the described methods facilitate the removal of sputum in one way or another, but only coughing with an open glottis can still move sputum into the trachea and large bronchi, from where it can be removed by coughing or by aspiration.
Treatment
There is currently no cure for COPD, but treatments are available to relieve symptoms and slow the progression of the disease.
The main goals of COPD treatment are:
- Symptom relief
- Slowing the progression of the disease
- Prevention and treatment of exacerbations
- Optimizing lung function
- Reducing mortality
Recommended treatments may include:
- To give up smoking.
If you smoke, the most important thing in preventing further progression of COPD is to quit smoking. - Medications.
These include a variety of inhalers, steroids, and antibiotics (as needed) to help manage symptoms and reduce the frequency and severity of flare-ups. - Pulmonary rehabilitation.
A specialized program that combines exercises with education about your condition will help you manage your symptoms and illness. - Changes in diet.
Some people with COPD find that changing their diet makes them feel better. - Oxygen therapy.
Patients with insufficient oxygen saturation in the blood (a condition known as hypoxia) may benefit from oxygen therapy using an oxygen concentrator. - Non-invasive ventilation.
Adding noninvasive ventilation to conventional therapy can reduce dyspnea, improve respiratory rate and gas exchange, and improve quality of life.
Your doctor will discuss various treatment options with you.