Fibromyalgia is a chronic disease characterized by pain, stiffness, and tenderness in muscles, tendons, and joints. Fibromyalgia is also characterized by sleep disturbances, feelings of chronic fatigue, depression, anxiety, and bowel dysfunction. Fibromyalgia is sometimes called fibromyalgia syndrome or fibrositis.
Although fibromyalgia is one of the most common diseases affecting the muscles, the cause is still unknown. The tissues that are the source of pain are not accompanied by inflammation of this tissue. And therefore, pain, which causes a lot of inconvenience for the patient, does not lead to irreversible changes and tissue destruction. In addition, there is no damage to internal organs. In this regard, fibromyalgia differs from rheumatological diseases such as rheumatoid arthritis, SLE or polymyositis. With these diseases, tissue inflammation occurs - this is the main cause of pain, stiffness, soreness in joints, tendons and muscles, and, in addition, damage to both tissues and internal organs occurs.
Description
The prevalence of fibromyalgia in the population is from 1% to 8%; women are mainly affected by this syndrome. Fibromyalgia can be idiopathic, when it is not combined with another pathology, and secondary, if it is diagnosed together with any clinical pathology (most often, a chronic disease). Since 1984, the term central sensitivity syndrome has been proposed as a pathological concept that includes various processes with similar characteristics, including fibromyalgia, chronic fatigue syndrome and others.
Picture 1
Or “everything hurts and nothing helps”!
It is with this phrase that a patient with fibromyalgia most often enters the doctor’s office: this is how this disease can be characterized.
As a rule, he already:
- visited many doctors (according to statistics - at least four),
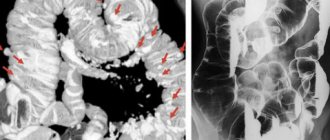
- he underwent a huge number of studies (on average, at least three instrumental studies only - MRI, CT, fibrocolonoscopy, etc.),
- a large number of “standard diagnoses” have been made, each of which is “nothing special” in the doctor’s opinion, several groups of drugs are being tried in treatment,
- and still the pain remains at the same level.
This process of going through examinations and consulting doctors takes an average of two years until one of them begins to think about fibromyalgia.
Symptoms
Fibromyalgia manifests itself as generalized chronic musculoskeletal pain (pain in the muscles and/or bones) , along with stiffness and other symptoms that affect the organs and systems of the body. The most common symptoms are: intestinal pain, headaches, tachycardia, menstrual irregularities, shortness of breath, insomnia, anxiety, depression and bad mood, problems with cognitive memory, attention and concentration . There is also severe fatigue and easy fatigability
standard treatment
The main treatment for fibromyalgia is medication and is aimed at relieving individual symptoms. It is carried out mainly to relieve pain and muscle spasms using painkillers and anti-inflammatory drugs. To reduce irritability, sleep disorders and symptoms of depression, low doses of antidepressants and antiepileptic drugs are prescribed.
Non-drug treatment methods include physiotherapy, acupuncture, light massage, physical therapy, spa treatment, and psychotherapy.
Causes
There are currently no generally accepted causes of fibromyalgia. There are several theories:
- Current research supports the theory that many of the signs and symptoms of fibromyalgia may be related to dysfunction of the central nervous system, which contributes to impaired sensory stimulation.
- Also, modern research recognizes a strong connection between fibromyalgia and diseases of the central nervous system.
- In particular, there is evidence of neuroendocrine and autonomic impairment in fibromyalgia, with symptoms very similar to those described by patients with filum terminale disease. This has led other authors to propose that, at least in a certain percentage of patients, fibromyalgia may be an epiphenomenon of filum terminale disease.
-According to the Filum System® method:
In some cases of fibromyalgia, it is observed that this syndrome is associated with asynchronous growth of the spinal cord (and with it the central nervous system) and the spine during the embryonic development phase. This provokes the appearance of abnormal tension in the spinal cord, which is transmitted by a tense and short filum terminale from the coccyx to the skull. In this case, it is believed that abnormal tension of the filum terminale may be a cause of predisposition to the development of fibromyalgia syndrome.
Fibromyalgia pain points and local pain syndromes
Typical pain points for fibromyalgia are where the muscles intertwine with the bones, i.e. enthesis. In fibromyalgia, the immune system attacks the enthesis, causing inflammation and pain. The picture of inflammation can be seen with MRI and ultrasound of the entheses, although structural changes in the entheses are not very noticeable due to their anatomical structure.
Local pain syndrome is a form of fibromyalgia in which pain is more severe in one region of the body. At the same time, other typical pain points are also active.
Fibromyalgia: typical pain points
Typical local pain syndromes in fibromyalgia:
- Headache;
- Atypical facial pain;
- Chronic pelvic pain (including tendinitis of the lumbar muscles, trochanteritis);
- Coccygeal pain – coccydynia;
- Humeral periarthritis of non-traumatic nature.
Practice shows that successful treatment of fibromyalgia and local pain syndromes is possible if 3 issues are resolved: a full night’s sleep is restored with the phases of slow-wave sleep and REM sleep present, infections that trigger inflammation are treated (they are usually visible in test results), normal work is restored immunity. Read more about treatment below on this page.
Diagnostics
Symptoms of fibromyalgia may come and go in cycles. This fact, coupled with the lack of established tests to make a diagnosis, hampers the diagnostic process, resulting in a delay in the implementation of existing treatments. The American College of Rheumatology proposed criteria for diagnosing fibromyalgia syndrome in 1990, which are still in effect today. In 2010, new criteria were proposed, which are still at the approval stage. The Filum System® method, in light of the fact that several cases of fibromyalgia have coincided with the diagnosis of Filum Terminale Disease, suggests an MRI of the brain and spine to check for the presence of signs of spinal cord tension.
start of treatment
Treatment of fibromyalgia in our center begins with an appointment with a vertebroneurologist. The initial appointment is conducted by the candidate of medical sciences, chief medical doctor Lyudmila Ivanovna Mazheiko.
Approaches to the treatment of fibromyalgia are strictly individual. At the appointment, the vertebroneurologist will conduct a clinical assessment of the main symptoms: the severity of the pain syndrome and the localization of trigger zones, identify signs of autoimmune aggression on muscle fibers and disturbances in metabolic processes.
Based on the examination, the doctor will develop an individual treatment plan.
Appointments with a vertebroneurologist are carried out by appointment. To begin treatment, make an appointment.
Factors influencing the development of fibromyalgia
Major risk/susceptibility factors for fibromyalgia:
- Female gender: This disease is most common in women (female/male ratio 6/1).
- Age: Fibromyalgia can appear at any age, but its incidence increases over the years.
- Genetic factor/Family predisposition: The development of fibromyalgia occurs more often if one of the relatives suffers from this syndrome. In addition, the tension on the spinal cord caused by an over-tight filum terminale (filum terminale disease) is a congenital condition and can be inherited.
- Stress: It has been proven that physical or psychological stress can trigger the onset of fibromyalgia.
- Other Factors: There have been a few cases of bacterial or viral infections, injuries, and other diseases (such as rheumatoid arthritis or lupus) that were not the cause of fibromyalgia but did cause symptoms typical of fibromyalgia.
Electromyography of nerves and muscles in fibromyalgia / ENMG in fibromyalgia
Our clinic can offer you specialists who are well acquainted with the topic of fibromyalgia and ENMG diagnostics using modern equipment. The main tasks of electromyography in fibromyalgia:
- Rule out poliomyositis of an autoimmune nature, myopathy, amyotrophic lateral sclerosis;
- Differential diagnosis of fibromyalgia and radicular pain caused by compression of the spinal cord roots;
- Diagnosis of polytunnel syndrome, which often accompanies fibromyalgia (pinching of the nerves of the arms and legs by thickened entheses).
How to Prepare for Electromyography for Fibromyalgia
- Before the examination, you should not treat the skin in the examination area (arms and legs) with greasy creams.
- We recommend that you do not take tranquilizers and centrally acting painkillers the day before and on the day of the study (this must be agreed with your doctor).
- If possible, take with you the results of previously performed studies, including tests, images, consultation data, this may be useful for choosing the most appropriate ENMG technique.
- Come to us 15-20 minutes before the test to calmly fill out your medical card.
Complications
- Impaired quality of life: Symptoms of general pain and chronic fatigue in fibromyalgia may wax and wane. Symptoms that affect cognitive abilities may be associated with chronic pain, which can trigger the development of depression and/or anxiety. All this affects the deterioration of the quality of life of patients who are limited in their activity and experience frustration due to a lack of understanding of the causes of their condition, which can lead to the growth and development of symptoms
- Chronic pain: Muscle and bone pain, headaches, abdominal pain and general pain may become frequent or constant, complicating the patient's condition.
our treatment
Our treatment of fibromyalgia differs from the standard in understanding the causes of the origin of this disease and the impact on them.
With fibromyalgia, painful lumps form in the muscles - triggers. They are formed as a result of a combination of the following disorders in muscle fibers: metabolic processes, microcirculation, autoimmune reaction. In such conditions, the muscles do not receive sufficient nutrition, become denser and the person experiences pain.
Painful points (triggers) for fibromyalgia are detected in many muscles, but most often in the occipital region, in the neck, shoulders, shoulder blades, in the area of the elbow and knee joints, in the sacrum and pelvic region.
We have developed a special method for treating fibromyalgia - an integrated approach that combines special therapy to resolve triggers, selection of natural drugs to normalize metabolic processes and the immune response, as well as movement therapy to improve microcirculation in muscle fibers.
At the first stage, restorative treatment is carried out for dystrophic muscles and ligaments, eliminating triggers using microinjections of vitamin preparations. Thus, the sensations of tightness, stiffness in the muscles, numbness and “goosebumps” disappear.
At the second stage, metabolic processes in muscle fibers improve, muscle pain disappears, a feeling of freedom of movement appears, a surge of strength and an improvement in the emotional state.
At the end of the course, the effect is consolidated by osteopathic, massage and special movement techniques, which allows you to completely get rid of any unpleasant sensations in the muscles, leading to an improved quality of life and increased performance.
Fibromyalgia Treatment
There is no specific treatment for this disease. Today, treatment is carried out to reduce pain and other symptoms to improve the patient's quality of life. Currently, the following specialties are involved in the treatment of fibromyalgia syndrome: general and clinical medicine, rheumatology, rehabilitation medicine, physiotherapy, psychology, dietetics, etc. In our specialty, neurosurgery, since the publication of a study conducted by Dr. Mantia and his colleagues in 2015, which looked at the use of the Filum System® method and concluded that patients who have undergone surgery show better results using physical therapy, provided that Since the presence of filum terminale disease is confirmed, we believe that some patients with fibromyalgia syndrome may be caused by filum terminale disease. Since 1993, with the publication of the doctoral dissertation of Dr. Royo Salvador, who linked the tension of the entire nervous system with the filum terminale as the cause of several diseases, a new treatment method that is etiological, that is, acting on the cause of the development of the disease. With surgical cutting of the filum terminale using the Filum System® method, the tension force responsible for this pathological mechanism is eliminated. Our dissection technique is minimally invasive, indicated in all cases of filum terminale disease and is recommended to be used as early as possible because it stops further development of the disease with minimal risks.
Fibromyalgia
Fibromyalgia
Fibromyalgia is a disease that comes to the attention of not only rheumatologists, neurologists, pain specialists, but also general practitioners.
Fibromyalgia is a fairly common disease, affecting about 20 million people worldwide (about 4% of the population), mostly middle-aged women. However, despite its prevalence, the diagnosis of fibromyalgia in the world, particularly in Russia, is extremely rare. This is due to unusual manifestations of the disease, insufficient awareness of doctors and the lack of clear diagnostic criteria. Fibromyalgia is understood as a syndrome of non-articular widespread symmetrical musculoskeletal pain, which is chronic in nature and accompanied by depression, sleep disturbances and the presence of specific tender points. In neurological practice, this is also a fairly common pathology. Nevertheless, there is a paradoxical situation in which the actual diagnosis of fibromyalgia, even syndromic, is, in principle, absent in the daily practice of medical specialists. The reason for this, on the one hand, most likely lies in the variety of clinical manifestations of fibromyalgia. Neurologists most often evaluate such patients in accordance with the leading comorbid manifestations (“panic attacks”, tension headaches, widespread osteochondrosis, myofascial syndrome, osteoarthritis, etc.). On the other hand, the reason lies in the underestimation of the significance of mental disorders and stress for these patients and the lack of generally established ideas and views on this symptom complex as a single suffering. Undoubtedly, such patients are also encountered in the practice of psychiatrists, who, however, do not diagnose patients with FM, since they do not subject the patient’s somatic state to a detailed analysis and do not examine their sensitive points.
Story
Although the term “fibromyalgia” was coined relatively recently, this condition has long been described in the scientific literature. In 1904, William Gowers coined the term fibrositis. The modern concept of fibromyalgia was created by Smythe and Moldofsky in the mid-1970s. They coined a new term, fibromyalgia. The authors identified the presence of local hypersensitivity, so-called “tender points,” as a characteristic symptom of fibromyalgia. They also found that patients with fibromyalgia often experience sleep disturbances. The next stage in fibromyalgia research was the development of the American College of Rheumatology (ACR) diagnostic criteria for fibromyalgia, which were published in 1990. Significant progress in the study of fibromyalgia has been made after researchers concluded that the condition is not caused by damage or inflammation of peripheral tissues. Therefore, all efforts were aimed at studying the central mechanisms of pathogenesis.
Etiology and pathogenesis
One of the most important mechanisms for the formation of chronic pain in fibromyalgia is the phenomenon of central sensitization (CS). It is characterized by the fact that after prolonged peripheral nociceptive stimulation, a certain level of excitation remains in the central sensory neurons of the dorsal horn, which maintains pain even in the absence of further peripheral pathology. However, numerous studies have demonstrated that CS can develop in the presence of disorders in the central nervous system without peripheral damage. Fibromyalgia is such an example. Often, patients with fibromyalgia who do not show peripheral changes are considered by doctors as malingerers or patients with hysteria. Some doctors, in situations where they cannot find an organic cause of pain, prefer to use diagnostic labels such as psychosomatic and somatoform disorders. However, today it has been convincingly shown that central sesitization, as well as impaired descending (noradrenergic and serotonergic) inhibitory control of pain, occur in fibromyalgia not as a result of peripheral changes in muscles, fascia, ligaments or connective tissue, but as a result of neurodynamic disorders in the central nervous system in individuals with a genetic predisposition under the influence of a large number of stressful (physical and mental) events. Research into fibromyalgia over the past two decades has shown that the pain threshold depends on the degree of distress. Many psychological factors, such as hypervigilance, suspiciousness, catastrophizing, and external locus of pain control, may play an important role in the severity of fibromyalgia symptoms. Special studies have shown that patients with fibromyalgia have reduced serotonergic and noradrenergic activity. It has also been found that patients with fibromyalgia have decreased levels of serum serotonin and its precursor L-tryptophan. This evidence is supported by the fact that drugs that simultaneously increase serotonin and norepinephrine levels (tricyclic antidepressants, duloxetine, milnacipram and tramadol) are effective in treating fibromyalgia.
The main symptoms of fibromyalgia are pain (100%), stiffness (77%) and fatigue (81.4%). The onset of fibromyalgia in most patients is gradual. The onset of the disease is often associated with emotional factors, stress, changes in the family, injuries, surgical interventions, etc. The most common symptoms of fibromyalgia are pain, which worsens in a state of fatigue, tension, excessive physical activity, immobility and cold. The pain is usually bilateral and symmetrical. Pain and stiffness in the head and neck area are typical in the morning. Complaints of calf muscle cramps, paresthesia and sensations of fullness in the upper and lower extremities are quite common. Fatigue is one of the most common complaints. Often the patient wakes up more tired than before going to bed.
American College of Rheumatology criteria for fibromyalgia (N. Smyth, M. Yunus, 1990):
- The presence of generalized symmetrical pain (spreading to the right and left, upper and lower halves of the body, or axial), lasting for at least the last 3 months.
- Pain on palpation of at least 11 out of 18 (9 pairs) specific tender points.
The following points are used:
- occipital region - place of attachment of m. suboccipitalis;
- neck region - anterior sections of the space between the transverse processes CV - CVII;
- trapezius muscle - middle of the upper edge;
- supraspinatus muscle at its insertion;
- the zone of articulation of the second rib with the sternum along its upper edge;
- a point located 2 cm distal to the lateral epicondyle of the humerus;
- in the gluteal region - the upper outer quadrant of the buttock along the anterior edge of the muscle;
- greater trochanter of the femur;
- in the area of the knee joint there is a medial fat pad.
The pressure applied at these points should be 4 kg/cm, the pressure at which the examiner's nail beds turn white. When palpating 18 painful points, it is recommended to apply even pressure on paired points and, with the same force, palpate other areas of the body to compare sensitivity. Patients with fibromyalgia experience increased sensitivity in tender spots compared to other areas of the body. Painful points reflect areas of increased sensitivity to painful stimuli, and are not a consequence of local inflammation or tissue damage. In addition, it is necessary to determine pain sensitivity at control points (in the frontal, above the head of the fibula).
The presence of a positive reaction in more than 11 of 18 painful points was determined by the diagnostic criterion based on the analysis of statistical data from large populations of patients. However, not all patients with fibromyalgia will have increased sensitivity in more than 11 points. Once again, we note that the ACR criteria for fibromyalgia are intended for research purposes and not for making diagnoses for specific patients. However, examination of tender points is considered an important part of studying the functioning of the musculoskeletal system in patients with generalized pain syndrome. Palpation of soft tissues and joints allows you to identify areas of increased sensitivity. This examination allows you to exclude synovitis or myositis and is very important in the diagnosis of fibromyalgia. Along with the described most characteristic complaints of pain, fatigue and stiffness, patients with fibromyalgia have a whole symptom complex of psychovegetative, psychosomatic and various algic disorders, which occur in FM several times more often than in the population. The high association with FM allows us to consider them as comorbid. The most common among them are the following: “panic attacks”, hyperventilation syndrome, tension headaches, migraines, lipothymic conditions, irritable bowel syndrome, cardialgia, abdominalgia, Raynaud’s syndrome. It should be emphasized that in one patient, as a rule, one can detect a whole symptom complex of the mentioned disorders, the dominance of which in the clinical picture often makes it difficult to identify “fibromyalgic phenomena proper,” which is reflected in the interpretation of these patients and, as a consequence, in the leading diagnosis (tension headaches). , chronic myofascial syndrome, etc.). Recently, the FiRST (Fibromyalgia Rapid Screening Tool) questionnaire has been proposed to screen for fibromyalgia (Table 3). The advantages of the questionnaire are its brevity and ease of completion. It should be emphasized its high sensitivity (90.5%) and specificity (85.7%). It is important to note that the questionnaire is intended for screening and a diagnosis cannot be made using it alone. Patients who score 5 or more on the FiRST questionnaire should be carefully evaluated to make a definitive diagnosis of fibromyalgia.
FiRST questionnaire for screening for fibromyalgia
| Yes | No |
| I have pain all over my body | |
| Pain combined with a constant feeling of exhaustion | |
| The pain is like a burning sensation, electric shock, or cramping | |
| The pain is combined with other unusual sensations throughout the body such as pins and needles, tingling, and numbness. | |
| The pain is combined with other disorders (problems with digestion, urination, headaches, sleep disorders, depression) | |
| The pain greatly affects my life, especially my sleep and ability to concentrate, I’m kind of slow |
Fibromyalgia Treatment
The presence of pronounced psychological disorders dictates the need to include antidepressants in the treatment of fibromyalgia. The most commonly used are amitriptyline and melipramine at a dose of 10-25 mg 1 time per night. The course of treatment is 4-6 weeks. Fluoxetine is prescribed 20 mg 1 time in the morning. Non-steroidal anti-inflammatory drugs have found widespread use in the treatment of fibromyalgia. Long-term oral administration of non-steroidal anti-inflammatory drugs is undesirable due to possible side effects. Recently, preference has been given to local therapy in the form of ointments, gels, as well as local injections in combination with painkillers, in particular lidocaine. In a recent RCT of patients with fibromyalgia, lidocaine 50 mg was injected into a painful point in the trapezius muscle. As a result, not only a local reduction in pain at the injection site was noticed, but also a general analgesic effect. This study demonstrated the important role of peripheral tissues in the development of hyperalgesia in fibromyalgia and demonstrated the clinical utility of local anesthetic injections for the management of pain in fibromyalgia. It is considered appropriate to include so-called local muscle relaxants: baclofen at a dose of 15-30 mg per day or dantrolene at a dose of 25-75 mg per day help reduce muscle tone and have an analgesic effect. There are reports of the effectiveness of antioxidants (ascorbic acid, alpha-tocopherol) in the treatment of fibromyalgia. Among non-drug treatments, various physiotherapeutic procedures are widely used, in particular massage, balneotherapy, and cryotherapy. In recent years, much attention has been paid to physical exercise, namely aerobics, as an effective way to eliminate chronic muscle pain and fatigue. Importance is also attached to methods of psychological rehabilitation of patients with fibromyalgia - psychotherapy and autogenic training.
Dissection of the filum terminale using the Filum Sistem method
Advantages
1. The tension on the spinal cord caused by a too short or tight filum terminale is eliminated.
2. Using the minimally invasive surgical technique of the Chiari Institute of Barcelona, the surgical time is 45 minutes. Stay in the hospital for about a day. The post-operative period is short and without serious restrictions. No admission to the intensive care unit. No blood transfusion.
3. Its use reduces the risk of mortality to zero. No serious complications.
4. Improves symptoms and stops the development of pathologies associated with filum terminale disease.
Diagnosis of the disease
Fibromyalgia can be difficult to diagnose because many diseases have similar symptoms. For example, hypothyroidism, vitamin D deficiency, hypercalcemia, polymyositis (muscle disease), Paget's disease (bone disease), as well as oncology and infectious diseases (hepatitis, AIDS, etc.). Therefore, studies and extensive tests are carried out, first of all, to exclude these pathologies. There are no specific methods for establishing the diagnosis of fibromyalgia; it can be suspected based on the patient’s complaints and his physical examination. Experts identify 18 tender points at the tendon attachment points, which can cause pain when pressed. If 11 or more points react, fibromyalgia is suspected.
Bibliography:
- Cazzola M, Sarzi Puttini P, Stisi S, Di Franco M, Bazzichi L, Carignola R, Gracely RH, Salaffi F, Marinangeli F, Torta R, Giamberardino MA, Buskila D, Spath M, Biasi G, Cassisi G, Casale R, Altomonte L, Arioli G, Alciati A, Marsico A, Ceccherelli F, Leardini G, Gorla R, Atzeni F, Italian Fibromyalgia Network (2008) Fibromyalgia syndrome: definition and diagnostic aspects. Reumatismo 60(Suppl.1):3-14.
- Claw DJ (2009) Fibromyalgia: an overview. Am. J Med 122:S3–S13.
- Crofford LJ (1998) Neuroendocrine abnormalities in fibromyalgia and related disorders. Am J Med Sci 315:359–366
- Demitrack M, Crofford L (1998) Evidence for and pathophyiologic implication of hypothalamic-pituitary-adrenal axis dysregulation in fibromyalgia and chronic fatigue syndrome. Ann NY Acad Sci 840:684–697
- Forseth KO, Gran JT, Husby G (1997) A population study of the incidence of fibromyalgia among women aged 26-55 yr. Brit J Rheumatol 36:1318–1323.
- Goldenberg DL (2009) Diagnosis and differential diagnosis of Fybromialgia. Am J Med 122:S14–21.
- Yunus MB (2008) Central Sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Reum 37:339–352.
- Kwiatek R, Barnden L, Tedman R, Jarrett R, Chew J, Rowe C, Pile K (2000) Regional cerebral blood flow in fibromyalgia: single-photon-emission computed tomography evidence of reduction in the pontine tegmentum and thalami. Arthritis Rheum 43:2823–2233.
- Mantia R., Di Gesù M., Vetro A., Mantia F., Palma S., Iovane A. Shortness of filum terminale represents an anatomical specific feature in fibromyalgia: a nuclear magnetic resonance and clinical study. Muscles Ligaments Tendons J. 2015 Mar 27;5(1):33-7.
- Mountz JM, Bradley LA, Modell JG, Alexander RW, Triana-Alexander M, Aaron LA, Stewart KE, Alarcón GS, Mountz JD (1995) Fibromyalgia in women. Abnormalities in regional cerebral blood flow in the thalamus and caudate nucleus are associated with low pain thresholds. Arthritis Rheum 38:926.
- Murga I et al. Cambios en la resonancia cerebral asociados al syndrome de fibromialgia. Med Clin (Barc). 2021.
- Royo Salvador MB (1996), Siringomielia, escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF).REV NEUROL (Barc); 24 (132): 937-959.
- Royo Salvador MB (1996), Platibasia, impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia, escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia , la escoliosis , la malformación de Arnold-Chiari , el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia , scoliosis and Chiari malformation .” (PDF). Acta Neurochir (Wien) 147:515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve.”
- Staud R (2008) Autonomic dysfunction in fibromyalgia syndrome: postural orthostatic tachycardia. Curr Rheumatol Rep 10:463–466.
- Tanriverdi F, Karaca Z, Unluhizarci K, Kelestimur F (2007) The hypothalamo-pituitary-adrenal axis in chronic fatigue syndrome and fibromyalgia syndrome. Stress 10:13–25.
- Winfield JB (2007) Fibromyalgia and related central sensitivity syndromes: twenty-five years of progress. Semin Arthritis Rheum 36:335–338.
- Wolfe F, Smythe HA, Yunus MB, Bennet RM, Bombardier C, Goldenberg DL et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Arthritis Rheum. 1990;33:160-72.
Treatment options
Treatment of the disease consists of an integrated approach and requires the participation of several specialists (neurologist, psychotherapist, psychiatrist).
Drug therapy is used when diagnosed with fibromyalgia to relieve muscle spasms, pain, sleep disturbances and symptoms of depression. The list of such drugs includes local anesthetics, antidepressants, tranquilizers, anticonvulsants, and sedatives.
But drugs for fibromyalgia are not the only important ones. Numerous studies have shown that relief from illness can be achieved through exercise. Moreover, they can be of a different nature - swimming, yoga, Pilates, cycling and walking. And although patients are often afraid of increased pain from playing sports, the doctor’s task is to destroy this stereotype. It is physical activity that helps increase the production of endorphins, the lack of which the patient usually suffers from.
Another effective way is cognitive behavioral therapy; to put it simply, working with a psychologist who can help fight stress and cope with difficult life situations, teach you to look at the world differently.
Balneological procedures, light massages and even meditation are also used as a cure for fibromyalgia.
Today there are no uniform recommendations for the management of such patients. Therefore, therapy in each case is individual and takes into account the characteristics of clinical manifestations and response to treatment measures.
FAQ
How to treat fibromyalgia?
The disease is treated comprehensively using various methods. These include drug therapy, work with a psychologist and physical exercise. But the most important thing for the patient is to be aware of the problem and want to cope with it.
How does fibromyalgia manifest?
When diagnosed with fibromyalgia, pain may be felt in the back, neck, chest, hips, and knee joints. It also manifests itself as sleep disturbances, anxiety, and somatic problems.
Can fibromyalgia be cured?
If the diagnosis is made correctly and treatment is started, most often this disease can be overcome, and in other cases the condition can be significantly alleviated.