What is astheno-neurotic syndrome? This is a set of vegetative, neurological and psycho-emotional manifestations that occur against the background of a violation of the body’s adaptation, doctors call astheno-neurotic syndrome (asthenoneurosis). Such a deviation is possible with any pathology, the influence of mental or physical stress. The problem is identified at different periods of life. It does not allow adults to adequately respond to reality, nor does it allow children to develop according to their age. Emotional instability in children inhibits the processes of proper formation of intracerebral neural connections, therefore intellectual abilities slow down and the development of new skills worsens.
The syndrome is especially often diagnosed in children who have a delicate, very vulnerable mental organization. It is difficult for them to firmly respond to failures and control their mood. Treatment of asthenoneurosis usually consists of light psychocorrection, which helps to establish social relationships and quickly overcome one’s emotions.
Pathology or fiction?
Russians usually consider children's behavioral problems to be tiredness or poor upbringing. But according to the ICD, asthenoneurosis is recognized as a disease, having a personal code of F48.0. In the same category there are other neurotic disorders that require medical attention. Therefore, you need to be prudent, feel responsible for the child and treat him in a timely manner.
What is asthenic syndrome, asthenia?
Asthenic syndrome is a syndrome characterized by a state of mental irritable weakness, rapid depletion of nervous processes, unstable mood, impatience, decreased performance for prolonged physical activity and mental stress, intolerance to bright light, loud sound, strong smell, emotional lability, and sleep disturbances. The term " asthenic syndrome " comes from the Greek word "astheneia", which means "weakness, impotence". Asthenic syndrome has synonyms - chronic fatigue syndrome (CFS, CFS), asthenia , asthenic reaction , asthenic condition , asthenia of the nervous system .
Autonomic dystonia syndrome: a modern view of diagnosis and therapy
The article presents the principles of positive diagnosis of autonomic dystonia syndrome. The criterion for a positive diagnosis is the identification of stressful somatic symptoms, in response to which feelings, inappropriate thoughts and behavior arise. Modern approaches to the treatment of autonomic dystonia syndrome are outlined. It is noted that priority in complex treatment is given to antidepressants and psychotherapy.
Introduction
Autonomic dystonia syndrome (VDS) is one of the most common diagnoses in the practice of neurologists. This syndrome is also often encountered in the practice of therapists who prefer to refer to it as “neurocirculatory dystonia.” Several paradoxical facts should be noted. First, for such a common condition, clinicians are encouraged to use G90.9 (other autonomic nervous system disorders) or G90.8 (unspecified autonomic nervous system disorders) as a statistical code in the International Classification of Diseases (ICD) 10th Revision [1 ]. In other words, the syndrome is recognized as a vegetative disorder, but its nature is unknown. Secondly, foreign colleagues do not use diagnoses such as “vegetative dystonia syndrome” or “vegetative-vascular dystonia”. They use either the general term “medically unexplained symptoms” [2, 3], or, depending on the underlying emotional disorders, “generalized anxiety disorder”, “somatoform disorder”, “panic disorder”, etc. However, more often specific diagnoses are given terms denoting the leading and dominant symptom, for example, “non-coronary pain”, “hyperventilation syndrome”, “chronic fatigue syndrome”, “chronic tension headaches”. At a neurological appointment, six of the 20 most common diagnoses are in this disorder category [4].
A significant transformation of ideas about SVD has occurred in the last 15–20 years, when, on the one hand, methods for diagnosing organic pathology have been improved, and on the other, ideas about the role of individual brain structures in cognitive processes affecting memory, perception and behavior have significantly expanded. It is no coincidence that the famous American neurologist and neurophysiologist M. Hallett says that neurology is in crisis [5]. These processes were reflected in changes in terminology in the fifth edition of the American Manual of Classification of Mental Disorders (Diagnostic and statistical manual of mental diseases), published in 2013 [6], and proposals for improving ICD-11, the development of which has been extended until 2021. Essence of these changes is that somatic and neurological disorders, for which no organic substrate is found and the pathophysiology of which is not clear to the doctor, are designated as functional somatic or functional neurological symptoms, and this class of disorders is called not somatoform disorders, but body distress syndrome (bodily distress syndrome) [7]. Moreover, it is planned to move this group of disorders from the category of mental diseases (category F4) to the categories related to neurological diseases.
Diagnostics
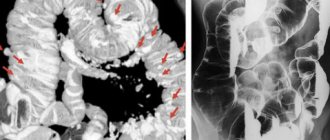
Traditionally, the diagnosis of SVD was based primarily on negative diagnosis, that is, the exclusion of organic disease. Modern diagnostic and classification manuals place emphasis on the criteria for a positive diagnosis. It states that in a number of cases “organic disease cannot explain the symptoms presented by patients,” which means it is important to determine the proportion of organic disease in patients’ complaints. This addition is significant, since functional disorders often appear in patients with organic diseases after they have been cured or in the stage of remission (compensation). Examples include hyperventilation syndrome in bronchial asthma, irritable bowel syndrome in Crohn's disease after achieving remission, postural phobic vertigo syndrome after an attack of benign postural positional vertigo, panic attacks with increased blood pressure in hypertension, pseudocardial pain after a myocardial infarction or myocarditis . In such cases, we are talking about the so-called overlap syndromes, in which treatment should be aimed not at the organic disease, but at those functional syndromes that mainly maladapt the patient and disrupt the quality of life.
The criteria for a positive diagnosis are currently formulated as follows: it is necessary to establish “stressful somatic symptoms in response to which feelings, inappropriate thoughts and behavior arise.” The determination of these parameters constitutes today a positive diagnosis of SVD. Let's look at each of them.
Stressful symptom
Any somatic symptom of both a subjective and objective nature can act as a stressful symptom: various pains (for example, headaches, pelvic pain, abdominal pain, chest pain), a feeling of lack of air, shortness of breath, dizziness, tachycardia, rises in blood pressure, stool disorders etc. Features of somatic symptoms are their polysystemic nature and tendency to paroxysmal course. The structure is determined by the leading complaint, relevant at the time of visiting the doctor, and accompanying symptoms (associated or comorbid), including in the medical history, which can be identified through active questioning. Active questioning can also reveal violations of biological motivations, which patients usually do not focus on the doctor's attention. Among them are disturbances of appetite, sleep, sexual function and activity, asthenia (weakness, fatigue). The proposed latest criteria emphasize the almost obligate nature of pain and asthenic disorders [7].
The stressogenicity of a symptom can be determined by its impact on areas of the patient’s life (visits to doctors, numerous examinations, cessation or difficulty in professional activity, problems in personal life). In addition, the stressogenicity of a symptom depends on the degree of its anxiogenicity (level of anxiety), which is determined by the following parameters:
- suddenness and unexpectedness of appearance;
- the inexplicability of the symptom;
- vital nature of dysfunction (heart, breathing, consciousness);
- the degree of maladjustment at the time of symptom onset and in the future.
It is natural that lipothymia and stool disorders differ significantly in their anxiogenicity. Highly anxiogenic disorders include dizziness, a feeling of instability, lightheadedness, suffocation, increases in blood pressure, increased heart rate and pulse, and convulsions.
Feelings, or emotional-affective component
Most patients with VDS present exclusively somatic complaints and even deny psychogenic factors at the onset and emotional disorders that would bother them. Nevertheless, the emotional-affective component is of fundamental importance as a diagnostic criterion. To verify it, emotions are analyzed during a paroxysm (panic attack) and the interictal period. Typical emotional syndromes include:
- anxiety, internal tension;
- anxiety;
- fear (of death, stroke, heart attack, falling, loss of control, etc.);
- aggression;
- irritability;
- depressed mood;
- lack of interest;
- apathy;
- tearfulness.
One of the characteristic misconceptions is the obligatory feeling of fear during a panic attack. Today it has been established that fear is more characteristic of the first, most severe and extensive panic attacks. With the passage of time and their successful resolution, fear passes and becomes de-actualized. Moreover, some attacks initially occur without fear - the so-called panic without panic, or “non-fear” panic attacks. In some panic attacks, other emotions may arise: irritation, aggression, apathy, depression, guilt, shame. Sometimes patients note that in the absence of any emotions during an attack, “for some reason, tears flow at this moment.” All these manifestations indicate an emotional-affective component in their suffering. Thus, the active detection of emotional syndromes in the clinical picture of VDS makes it possible to specify one of the positive criteria of the disease.
Inappropriate thoughts
A patient with VDS expects from a doctor not only help, but also a qualification of his disorder. That is why patients often ask the question: “So what is my diagnosis?” However, in accordance with the internal picture of the world that any person has, each patient has his own opinion about what is happening to him, about the cause of the symptoms of the disease and their consequences. The internal picture of the disease is formed by past experience (including past illnesses), previously seen from loved ones, acquaintances, read on the Internet, heard, in particular, from previous doctors and emergency doctors, etc. The patient's idea of the disease underlies an unconscious anxious expectation of change and increased attention to the processes occurring in the body. These processes, in turn, cause the formation of a stable pathological physiological pattern. An example is hyperventilation syndrome, in which the feeling of lack of air, typical of an anxious state, leads to an excessively long inhalation, which causes respiratory alkalosis, hypocapnia and sensations of lipothymia. With SVD, this breathing pattern is fixed, becomes habitual and persists even during sleep. In a situation of anxious waiting (for example, in the subway, where, according to the patient, there is “not enough air” and quick medical help is not available), this pattern is activated and leads to even greater hyperventilation and corresponding sensations. The same patterns, only concerning changes in postural reactions, can be traced in patients with postural phobic dizziness, asthenia and other functional syndromes.
Thus, inadequate ideas about the disease and anxious anticipation of catastrophic consequences rivet patients’ attention to bodily functions and each time activate ingrained (fixed) pathological functional patterns.
Behavior
Stressful symptoms, emotional disorders, and inappropriate thoughts affect the patient’s behavior. Identifying changes in behavior reveals another of the proposed criteria for a positive diagnosis of VDS. The patient needs to “What are you doing?” in order to find out about his behavior both in the paroxysmal state and in the interictal period. It turns out that the patient always calls an ambulance or, in case of any “unpleasant sensations,” immediately measures blood pressure (the frequency of such measurements can reach up to 30 times a day), if he has a headache in the morning, he takes painkillers “prophylactically”; side of the gastrointestinal tract, he follows a strict diet, although “the doctors find nothing,” etc. Upon further questioning, it is discovered that the patient has not used the metro for a long time, is not left alone at home, cannot move around the city independently, does not work, often undergoes examinations that briefly alleviate the condition, etc. Thus, the patient develops agoraphobic syndrome, which can have varying degrees of severity:
- mild degree - the patient is afraid of any situations, but can overcome fear;
- medium degree - some situations are an insurmountable obstacle for the patient (for example, the subway);
- severe degree - the patient cannot move independently outside the home and is alone at home.
You can get an idea of the patient’s troubling thoughts, threats, and associated emotions by purposefully asking the patient the following questions:
- how you feel when the symptom appears;
- What do you think about it;
- what consequences do you expect as a result of these symptoms;
- how do you behave at this moment;
- in what situation the symptom usually appears;
- how the symptom affects your physical and social functioning;
- What actions are you taking to avoid the expected “consequences of the disease”?
Thus, identifying all components of the disease allows the doctor to substantiate the diagnosis and outline a treatment strategy and tactics.
Treatment
Treatment of patients with VDS largely depends on the clinical manifestations (leading syndrome), underlying emotional disorders, severity of symptoms, duration of the disease and concomitant endocrine dysfunction or somatic diseases (overlap syndromes). The main goals of VDS therapy include:
- relief of the leading symptom or syndrome;
- impact on cognitive, emotional and behavioral disorders (inappropriate thoughts, anxiety and fears and agoraphobia);
- prevention of relapses and further progression of the disease.
Symptomatic, pathogenetic and preventive therapy is used. Sometimes an explanatory conversation with a doctor about the essence of the disease, possibly in combination with placebo therapy, is sufficient.
Today, so-called educational programs play a significant role in understanding the causes of the disease. We can recommend turning to the non-profit website www.neurosimptomy.moonfruit.com, developed specifically for patients. There, in an accessible form, answers are given to the patient’s questions about functional and dissociative neurological symptoms: is the diagnosis correct, how do such symptoms arise, how dangerous are they, what role does the “nervous soil” play, how can one get rid of this suffering? From the information presented on the site, the patient will be able to understand what is causing his dizziness or shortness of breath, why he gets tired so quickly, what his “vegetative attacks” are, etc. It is extremely important to explain to the patient that this disorder, despite the frightening and “severe” symptoms, does not lead to catastrophic consequences, that is, to strokes, heart attacks, etc.
Symptomatic therapy
The goal of symptomatic therapy is rapid relief of the leading symptom. Prompt relief of the condition has a psychotherapeutic effect, as it removes the fear of a threatened and incurable disease. In addition, relief of the leading symptom prevents the process from becoming chronic. Thus, quick and early relief of acute back pain prevents the development of persistent muscle spasm - an important pathogenetic mechanism for the formation of chronic back pain. Early and successful relief of a panic attack prevents the development of agoraphobic syndrome and restrictive behavior as the main factors of social disability in patients with panic disorders.
Symptomatic therapy includes a variety of techniques. Thus, to relieve hyperventilation disorders, it is advisable to teach the patient breathing exercises, which he can also use to relieve panic attacks and correct respiratory disorders outside of an attack.
For most functional symptoms, pharmacological drugs are used as symptomatic therapy - the so-called on-demand treatment: to reduce tachycardia - beta-blockers, relieve nausea - prokinetics (metoclopramide), relieve pain - non-steroidal anti-inflammatory drugs and muscle relaxants, for functional dizziness - betahistines and other vestibulolytic drugs, gastrointestinal disorders (dyspepsia, pain, abnormal stool frequency) - H2 receptor blockers, enveloping and/or antidiarrheal drugs. The doctor must remember and explain to the patient that this treatment operates on the “here and now” principle, is prescribed for a short period of time and will be canceled as the main pathogenetic therapy begins to take effect.
The above does not apply to tranquilizers, the use of which in the “on demand” mode only worsens the condition, leading to more frequent episodes of poor health and chronicity of the disease. In most cases, the prescription of tranquilizers at the beginning of therapy is determined by the severity of symptoms, but not only the severity of emotional disorders. As a rule, the patient does not feel emotional disorders, and if he does, he explains them with fears for his health due to “severe” somatic disorders: high blood pressure, lightheadedness, dizziness, etc. In such cases, taking tranquilizers on a regular basis, firstly, reduces anxiety, and secondly, relieves vegetative symptoms. In addition, tranquilizers have additional properties, in particular muscle relaxant, antiparoxysmal, anticonvulsant, and hypnotic effects. The use of tranquilizers stabilizes the patient’s condition during the period of delayed action of the antidepressant, eliminates possible undesirable effects of the initial stage of antidepressant therapy and, finally, increases confidence in the doctor and the therapy he has chosen. Already at the first appointment, it is necessary to discuss the prejudice that patients have against taking tranquilizers. The patient should know that tranquilizers affect not only emotions, but also vegetative symptoms; the drugs are prescribed for a short period of time (no more than one month) and then gradually withdrawn, so there is no danger that addiction will develop to them. You can use herbal preparations (valerian, motherwort, Persen, Novo-Passit) and derivatives of various chemical groups: benzodiazepine and non-benzodiazepine (Phenibut, Atarax, Stresam, Buspirone). Since the emotional-affective component, namely anxiety and fear, plays a key role in both the formation and persistence of VDS symptoms, treatment with tranquilizers is appropriate and justified. Tranquilizers have undoubted advantages: they immediately have an anti-anxiety and vegetative-stabilizing effect and thereby prevent the fixation and chronicity of the disease.
Tranquilizers are effective not only in situations of exclusively SVD, but also when the syndrome is combined with ongoing organic diseases (overlap syndromes). The use of psychotropic drugs, in particular tranquilizers from the group of benzodiazepines (seduxen, phenazepam, clonazepam, alprazolam, etc.), is fraught with the development of dependence upon further use (including after discharge), cognitive impairment (especially in old age), and in the case of rapid withdrawal – exacerbation of symptoms.
In connection with the above circumstances, it seems relevant to search for a drug that effectively relieves psychovegetative disorders, but does not have the disadvantages inherent in typical benzodiazepines. Such a drug can be the benzodiazepine tranquilizer tofisopam (Grandaxin). Like all benzodiazepine tranquilizers, it uses the nonspecific inhibitory neurotransmitter, GABA, as its main active ingredient. This is what causes a wide range of inhibitory effects both on the emotional sphere (reducing anxiety, fear, tension) and on the autonomic functions of the body (vegetative stabilizing effect) [8].
Not being a typical tranquilizer, tofisopam has the following unique properties:
- does not cause the development of physical dependence;
- does not have sedative or muscle relaxant effects;
- does not potentiate the effect of alcohol;
- does not impair cognitive functions (in particular, does not reduce concentration);
- does not have a cardiotoxic effect (on the contrary, it has a beneficial effect on coronary blood flow and myocardial oxygen demand);
- is characterized by a moderate stimulating effect and therefore belongs to the group of daytime tranquilizers [9].
In 2007–2008 A multicenter controlled study of the effectiveness of treatment of SVD was conducted using the tranquilizer Grandaxin along with standard nonspecific therapy [10]. The study involved 220 patients with VDS. In addition to VDS, 35% of patients had other diseases (dyscirculatory encephalopathy, vertebrobasilar insufficiency, migraine without aura, cervicalgia and lumbodynia), and in 65% only VDS was diagnosed. 140 patients used Grandaxin along with standard therapy for 28 days, and in the control group, 80 people with the same disorders received only nonspecific therapy. The data obtained allowed the researchers to draw such conclusions.
- Nonspecific therapy of psychovegetative syndrome with the inclusion of vascular, metabolic and nootropic drugs for four weeks significantly improved both indicators of emotional status (anxiety and depression) and symptoms of autonomic dysfunction.
- The use of Grandaxin along with nonspecific therapy made it possible to significantly improve the condition of patients faster and to a much greater extent, normalize psycho-vegetative imbalance and improve the quality of sleep.
- The addition of Grandaxin to therapy had a positive effect not only on subjective sensations, but also on objective indicators according to the Vegetative Questionnaire [11].
- The addition of Grandaxin to the treatment regimen had a positive effect on sleep quality, which makes it possible to recommend it to patients suffering from VDS and insomnia.
- Good tolerability of the drug and reduction of possible adverse events during treatment make it possible to prescribe Grandaxin at a dose of 150 mg/day both to patients suffering only from SVD and to patients with somatic and neurological pathologies along with SVD.
Pathogenetic therapy
Pathogenetic therapy is aimed at preventing repeated paroxysmal manifestations, regression of chronic pain syndrome and abuse factor, relief of anticipation anxiety, agoraphobic syndrome and restrictive behavior, secondary depression, asthenia, aggression and dyssomnia, eating disorders and other chronic manifestations of VDS.
Numerous multicenter placebo-controlled studies have shown that antidepressants are the basic drugs in the treatment of functional disorders. It has been established that antidepressants can be effective in chronic pain syndromes of various localizations [12], panic disorders [13, 14], asthenia [15] and appetite disorders [16], functional dizziness [17] and other manifestations of VDS. Moreover, antidepressants are effective regardless of whether these syndromes are combined with depression or not, and the doses used to treat VDS are significantly lower than for the treatment of major depression. The benefits of antidepressants include:
- wide spectrum of action (
emotions, aggression, chronic pain, vegetative symptoms, eating behavior, sleep disorders, etc.); - lack of addiction and dependence;
- no effect on cognitive functions;
- good tolerance;
- safety (therefore can be used in elderly and somatically burdened patients), compatibility with somatotropic drugs;
- effectiveness in small doses (usually one to one and a half tablets is enough);
- convenient method of administration (once a day).
Among the disadvantages of antidepressants, one should note the delayed effect of action and the need for long-term course therapy.
It must be emphasized that the pronounced side effects of a number of antidepressants, in particular tricyclics, significantly reduce the possibility of their use, especially in outpatient practice. Therefore, the drugs of first choice are currently antidepressants from the group of selective serotonin reuptake inhibitors (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram and escitalopram) and serotonin and norepinephrine reuptake inhibitors (venlafaxine, duloxetine, milnacipran) [18].
When determining the tactics of antidepressant therapy, it is necessary to resolve two main issues: choosing a drug and determining its dose. The choice is determined mainly by the clinical picture of the disease and the characteristics of the drug. Each of the antidepressants has features that can be useful in treating patients with certain syndromes. Thus, drugs from the group of selective serotonin and norepinephrine reuptake inhibitors (duloxetine, venlafaxine, milnacipran) have a proven analgesic effect. It has been shown that the analgesic effect of tricyclic antidepressants is due to a combined serotonergic and noradrenergic effect and does not depend on their antidepressant effect. Numerous international studies show that venlafaxine, having a dual effect, increases the concentration of serotonin and norepinephrine in the synapses of brain structures. Possessing high selectivity for these neurotransmitters, the drug does not affect muscarinic and H1 receptors, which suggests little side effects of treatment, as well as unwanted drug interactions with other drugs. According to international studies, venlafaxine is not inferior in effectiveness to tricyclic antidepressants (amitriptyline) and is superior to selective serotonin reuptake inhibitors. A number of studies have shown the effectiveness of venlafaxine in chronic migraine and tension-type headache [19, 20].
We conducted a study of the effectiveness of venlafaxine (Velaxin, long-acting capsules) in patients with chronic tension-type headaches and psychogenic headaches. The course of treatment (venlafaxine 75 mg/day for two months) had a positive effect on the well-being of patients in both groups. The intensity and frequency of headaches decreased significantly, the amount of painkillers taken decreased, the symptoms associated with headache decreased, and the function of antinociceptive systems normalized [21].
The following guidelines may be helpful when prescribing antidepressants.
- Considering the individual sensitivity and alarming sensitivity of this category of patients, it is advisable to start therapy with small doses (1/2–1/4 of the planned dose) with a gradual increase in dose over three to five days.
- The criterion for limiting the dose may be the severity of side effects that do not disappear within three to five days.
- A daily distribution of the drug is recommended depending on the hypnogenic effect.
- There may be a delay in the effect of therapy, since for most, the antidepressant effect manifests itself with a latent period (14–21 days) from the start of their use.
- Abrupt withdrawal of drugs at any stage of treatment can lead to exacerbation of the disease, therefore, at the end of treatment, the drug is discontinued gradually.
- The course of treatment should be long, sometimes a year or more.
In recent years, a drug has appeared on the Russian market that has the properties of both a tranquilizer and an antidepressant. This is a drug from the pharmacological company EGIS Spitamin (buspirone). Buspirone is a non-benzodiazepine anxiolytic and at the same time an antidepressant that acts on serotonergic and dopaminergic receptors.
The anti-anxiety effect of buspirone is not associated with an effect on GABA-benzodiazepine receptors. However, in terms of anxiolytic activity, buspirone is comparable to both typical (diazepam) and atypical benzodiazepines (lorazepam or alprazolam). Unlike them, it does not cause drug dependence, cognitive and psychomotor impairments, and does not have a pronounced sedative or muscle relaxant effect [22].
Among the main indications for the use of buspirone (Spitomina) are generalized anxiety disorder, panic disorder, VDS, alcohol withdrawal syndrome (as an adjuvant therapy), depressive disorders (as an adjuvant therapy, but not for monotherapy of depression). Buspirone is included in recommendations for the treatment of generalized anxiety disorder, which many foreign colleagues consider as equivalent to SVD.
The therapeutic (anxiolytic) effect develops gradually, manifests itself after 7–14 days and reaches a maximum after four weeks. Due to the delayed development of the drug's action and to enhance its effect, buspirone can be combined with tofisopam (Grandaxin), sedatives and hypnotics (for insomnia). Buspirone is especially often used in combination with drugs from the group of selective serotonin reuptake inhibitors when patients have insufficient response to these antidepressants or to level out their side effects [23].
The advantages of the drug include safety, absence of dependence and withdrawal syndrome, weight gain and sexual dysfunction. Moreover, buspirone can have a positive effect on sexual disorders caused by both generalized anxiety and serotonergic antidepressants.
Buspirone is well tolerated. Side effects (dizziness, headache, weakness, sleep disturbance, decreased attention), if observed at the beginning of the course of treatment, subsequently disappear despite continuing to take the drug. Side effects can be prevented by gradually increasing the dose by 5 mg every two to three days from an initial dose of 5 mg to 20–30 mg.
In addition to pharmacotherapy, psychotherapy, both cognitive-behavioral and psychodynamic, is recommended for patients with SVD. The first corrects distortions or errors in thinking and forms more adaptive behavioral patterns. The second works on unconscious interpersonal conflicts both in the past and in the present.
Conclusion
Currently, a large group of patient complaints and physical symptoms are united on the basis of the absence of organic pathology and common pathophysiological mechanisms in their origin. Comprehensive treatment, which prioritizes antidepressants and psychotherapy, can successfully manage such a common and socially disabling suffering as VDS.
Asthenic syndrome in children: symptoms
What is the clinic for asthenia in children? Asthenic syndrome in children has characteristic symptoms : tearfulness, moodiness, increased drowsiness, fatigue, fatigue, excitability, overexcitability, poor sleep, motor disinhibition, dizziness.
At school, gymnasium, and lyceum, children remain productive only in the first lessons and in the first half of the school hour. Children with asthenia or asthenic syndrome have poor attention, they are often distracted in class, attention is depleted, immunity decreases, and childhood diseases occur. Children often make mistakes, miss letters, underwrite letters, swap letters, double letters, underwrite words, forget to put commas or periods, and make incorrect indentations. With asthenia, with asthenic syndrome, autonomic reactions and autonomic disorders are often observed: acrocyanosis, hyperhidrosis (excessive sweating), poor appetite, discomfort, pain, unpleasant sensations in the heart (in the heart area).
Treatment with folk remedies
Folk remedies are used as an auxiliary method of treating neurasthenia. Herbal sedatives can be used to help reduce irritability and other symptoms. However, it is important to remember that any folk remedies may have certain contraindications. Therefore, it is better to consult your doctor first.
- Herbal teas . They can be prepared from chamomile, peppermint, and lemon balm. You can drink them separately or prepare a collection. To prepare tea, take 1 tbsp. l. mixture in 250 ml of boiling water, leave for 10 minutes. You need to drink this tea 2-3 times a day, 150 ml. You can also add rose hips and oregano to this tea. It is recommended to drink herbal tea with honey.
- Motherwort . Helps reduce the severity of symptoms of neurasthenia. To prepare the product you need 2 tsp. pour 200 ml of boiling water over the raw material and leave for 8 hours. Strain and drink throughout the day. Similarly, you can prepare an infusion of St. John's wort.
- Hawthorn . 3 tbsp. l of hawthorn fruit, pour 250 g of boiling water and leave for half an hour. Drink 150 ml half an hour before meals three times a day.
- Celery greens. It is recommended to add it to salads and soups. You can also prepare an infusion, pour 3 tbsp. l. celery 250 g boiling water. Fresh dill is similarly useful for neurasthenia.
- Beetroot juice . Fresh beet juice is mixed with natural honey in a 1:1 ratio. You need to drink 100 g 3 times a day for a month.
- Valerian root . 1 tbsp. l of the product, pour 250 ml of boiling water into a thermos and leave overnight. Drink 70 g three times a day for 1-2 months.
Asthenic syndrome in adults: symptoms, signs, manifestations of asthenia
What is the clinic for asthenic syndrome in adults, men and women? Asthenic syndrome in adults (men, women), in adolescents (boys, girls) has typical symptoms : irritability, restlessness, sleep disturbance, intolerance to loud sound, fatigue, mood swings, bad mood (low, depressed mood), poor mental tolerance and physical activity, fatigue, decreased self-control, intolerance to bright light, impatience, inappropriate behavior, intolerance to strong odors, poor willpower, irritability, excitability, melancholy, apathy. The person feels tired, but often continues to do something. Lethargy can occur without exercise and does not go away even after rest. Sometimes in old age there is a decrease in memory, headache, fatigue from life, mentism (involuntary flow of thoughts), tearfulness, increased tearfulness, hyperesthesia, tearfulness (unreasonable crying for any minor reason), whims (moody). They are also characterized by “harassing”, “harassing” relatives, dissatisfaction with work, life, financial condition, and people around them.
Causes
Neurasthenia develops in people against the background of mental and physical overload, which, in turn, provokes overwork of the body. The reason for the development of this condition can be internal conflicts, a weak psyche, long-term adherence to a very strict diet, etc.
The occurrence of neurasthenia is influenced by predisposing and provoking factors. Predisposing ones include:
- increased anxiety;
- tendency towards perfectionism;
- period of recovery after somatic illnesses.
Provoking include :
- severe stress;
- conflict situations in the family and at work;
- lack of normal rest for a long time;
- previous traumas, including birth injuries;
- previous surgical interventions;
- infectious diseases;
- poor nutrition and, as a result, deficiency of vitamins and other important substances;
- alcohol abuse, smoking;
- lack of physical activity;
- lack of sleep;
- intoxication;
- endocrinological disorders;
- unfavorable psychosocial conditions;
- severe weather conditions, etc.
Asthenic syndrome, causes of asthenia
Asthenia and asthenic syndrome have certain causes of development. What are the main reasons for the development of asthenia and asthenic syndrome?
- Adynamia, physical inactivity.
- Great physical or mental stress, overload.
- Exposure to an electromagnetic field (EMF) is electromagnetic radiation.
- Excitement, stress, worry, conflicts.
- Hypertension, hypertension, hypertension, high, high blood pressure.
- Depression, depressive state.
- Working on a computer for a long time, watching TV, talking on a cell phone, using devices such as microwave ovens (microwave ovens), tablets, tablets, smartphones.
- Alcohol abuse, alcoholism.
- Intoxication.
- Infectious diseases, STIs.
- Coronary heart disease (CHD), angina pectoris, myocardial infarction.
- Constitutional characteristics of a person.
- Weather sensitivity, intolerance to changes in atmospheric pressure, intolerance to magnetic drills, increased solar activity (solar flares).
- Hereditary predisposition.
- Neurosis, neuroses.
- Improper organization of work, overtime at work, irregular work schedule.
- Nervous diseases, diseases of the nervous system.
- Organic diseases of the brain, central nervous system, central nervous system.
- Obesity.
- Human psychotype (psychological type of the nervous system).
- Overload of the nervous system in educational institutions (institute, university, academy, school, gymnasium, lyceum, technical school, college, kindergarten, courses).
- Poor emotional atmosphere at work.
- Poor nutrition, anorexia.
- Post-traumatic arachnoiditis.
- Mental illnesses.
- Psychosis, psychoses, psychopathy.
- Somatic diseases.
- Chronic diseases.
- Traumatic brain injury, traumatic brain injury, concussion, brain contusion, brain compression.
- Schizophrenia, initial stage.
Treatment of astheno-neurotic syndrome
The need to visit a neurologist arises in situations where the child is too irritable and capricious, his school grades have deteriorated, or nervous breakdowns occur in which he raises his voice at adults. All such signs can indicate not character problems, but nervous disorders. Attempts to independently pacify a teenager by shouting (or punishing) only aggravate the problem.
The first step is to visit a pediatric neurologist. An experienced specialist will quickly find out what is really happening: is it asthenoneurosis or is the child simply manipulating his parents due to hormonal changes in his body. Most often, a child’s nervous system can be easily corrected with corrective and developmental exercises, after which everything is restored, returning to normal. Good treatment results are provided by:
- consultations with a psychologist, changing the style of everyday life;
- sand therapy;
- sensory integration.
When astheno-neurotic syndrome is provoked by organic damage to the central nervous system and brain, correction must be supplemented with rehabilitation measures.
In such a situation, doctors prescribe the following procedures:
- TANK;
- Audiotherapy according to the A. Tomatis method;
- TCM;
- Biofeedback trainings.
Symptoms of asthenoneurosis do not seriously threaten children's health, but prolonged asthenia significantly worsens the quality of life and delays intellectual and physical development. Treating the problem is a complex task; it requires the involvement of a professional team, a combination of various healing methods.
Asthenia, asthenic syndrome, types of asthenia in men and women
Neurologist, neuropathologist, reflexologist, reflexologist distinguish types of asthenia , types of asthenic syndrome : morning (morning), daytime (day), evening (evening), nocturnal (at night) asthenia (neurotics), neurocirculatory asthenia, functional or organic asthenia, mental asthenia ( psychological), psychogenic and physiogenic, cerebral asthenia, infectious (post-infectious), post-viral (post-viral, post-viral asthenia syndrome), alcoholic (post-alcoholic), sexual (post-sexual), tonic, hypersthenic, hyposthenic, somatogenic (somatic), neurocirculatory, agastric, skin , traumatic (post-traumatic), neurasthenia . Reflexotherapists, neurologists, neuropathologists distinguish various variants of asthenic syndrome: astheno-vegetative syndrome, astheno-subdepressive syndrome, astheno-hypochondriacal syndrome.
Astheno-vegetative syndrome is characterized by both manifestations of asthenia and severe autonomic disorders.
Astheno-subdepressive syndrome is a non-psychotic pathological condition characterized by mild melancholy with a feeling of loss of vitality and activity. Physical and mental fatigue, weakness, exhaustion, mental and emotional hyperesthesia, emotional lability, absent-mindedness and distractibility of attention are observed.
Astheno-hypochondriacal syndrome is characterized by a combination of asthenia with exaggerated concern for one’s health.
VSD (vegetative vascular, vegetative vascular dystonia) of mixed, hypotonic, hypertonic type.
Symptoms of the disease
Typically, the symptoms of asthenovegetative syndrome are characterized by a gradual increase, in very rare cases they can be expressed quickly and vividly. Since asthenia is translated from Greek as impotence, the very first clinical sign is considered to be fatigue. Then:
- performance decreases;
- absent-mindedness and lapses in short-term memory appear;
- it becomes difficult to concentrate on one object and formulate your thoughts;
- restlessness, anxiety, irritability appear;
- Possible disturbances in the functioning of the genital organs (sexual dysfunction).
In addition to this, patients may develop hypochondria, which results in constant worry about their health. And this is understandable, since they may also be bothered by: tachycardia, shortness of breath, severe headaches, digestive disorders, loss of appetite, severe sweating, cold feet. Later, tinnitus and urination problems may appear. But this is hardly worth allowing; it is better to consult a doctor much earlier.
Prevention of asthenia
Sarklinik has developed an effective program “ Prevention of asthenia ”, which allows you to avoid future exhaustion of the nervous system. A healthy nervous system is a reality today. The peculiarity of the disease is that the symptoms slowly, gradually, but clearly increase, and the condition worsens sharply. Do not expect dangerous complications of asthenia, asthenic syndrome; contact Sarclinic for timely treatment.
Sign up for a consultation. They have contraindications. Specialist consultation is required.
Photo: (©) Bds | Dreamstime.com \ Dreamstock.ru The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Hypothalamic syndrome, treatment of hypothalamic syndrome, how to treat
Brain stroke: ischemic, hemorrhagic, treatment, rehabilitation, consequences
Asthenia, asthenic syndrome, treatment, symptoms, causes, how to treat in children, adults
Insomnia, treatment of insomnia in Saratov, what to do for insomnia
Vegetative vascular dystonia: treatment of VSD, how to treat VSD, symptoms, signs
Comments ()
Tests and diagnostics
The specialist carries out diagnostics, assessing the clinical picture, as well as the complaints of the patient and his loved ones. In the process of establishing a diagnosis, it is imperative to visit a therapist and carry out the examinations that he prescribes in order to exclude other diseases.
Since neurasthenia can be a sign of brain diseases. Therefore, it is important to conduct a CT scan or magnetic resonance imaging to rule out such diseases. The doctor may also prescribe rheoencephalography to assess blood circulation in the brain.
You can take a test for neurasthenia on a variety of online resources. However, such a test cannot be considered an analogue of diagnosis - it can only be used to confirm or refute the presence of a predisposition to such a disease.
Prevention of autonomic dystonia syndrome
Strengthening health and restorative measures is the most important stage in the prevention of SVD. It is important not only to monitor the child and his lifestyle, but also to maintain a good microclimate in the family (reduce stress, prevent conflicts, and so on). Proper nutrition should be combined with adequate physical activity that is feasible for the child’s body. For preventive purposes, walks in the forest, drinking mineral waters, swimming in the sea, and clean mountain air are useful.