Traumatologist-orthopedist
Shelepov
Alexander Sergeevich
12 years of experience
Doctor
Make an appointment
A less common genetic pathology characterized by changes in connective tissue is Marfan syndrome. People with classic signs of this disease are easy to recognize by their characteristic appearance. Almost all of them are characterized by abnormally high growth and asthenic physique, elongated limbs and fingers, and excessively mobile joints. The disease is characterized by various pathological changes in the structure of the skeleton, heart muscle and blood vessels, and organs of vision. The incidence of Marfan syndrome is low and amounts to one per 10-20 thousand newborns, and this indicator is not influenced by gender or race.
Features and causes of the disease
The initial signs of Marfan syndrome appear in the prenatal period of development. They are caused by disorders of the development of connective tissues, which are caused by a mutation of the gene that regulates the production of one of the main proteins - fibrillin. Due to structural changes and fibrillin deficiency, tissues become less dense and elastic and do not tolerate loads well. The joints and ligaments, the walls of blood vessels and the eye apparatus, in which the tissue of the ligament of zinn is weakened, suffer most severely because of this.
The main cause of Marfan syndrome is the autosomal dominant inheritance of the mutation, i.e. the disease is transmitted from one parent to the child. In addition, in some cases, changes in the gene structure appear due to the impact on a woman of external unfavorable factors, which include radiation, ionized radiation, as well as radiation therapy to which the mother was exposed during the treatment of cancer.
Doctors distinguish erased and pronounced forms of the disease. In an erased form, changes are present in one or two systems, and they are quite minor. In a severe form of the disease, changes are present in at least three systems, regardless of the degree of their severity, or in one or two, but are quite pronounced. The patient's condition may remain stable for many years, or the pathology may progress, covering new areas of the body, systems and organs.
Marfan syndrome
Marfan syndrome. Synonyms: arachnodactyly, hyperchondroplasia. This is one of the most common hereditary connective tissue diseases with multiple visceral abnormalities, among which the most important are lesions of the histological structures of the heart, large vessels, musculoskeletal system and eyes.
The disease is caused by a mutation in the fibrillin gene on chromosome 15; has an autosomal dominant type of inheritance with high penetrance of the mutant gene. As a result, the synthesis of collagen and elastin is disrupted, and the accumulation of an increased amount of abnormal (immature) collagen leads to the formation of characteristic phenotypic manifestations of the disease.
The frequency of diagnosed clinical forms of Marfan syndrome (SM) in the population is 1 per 10-15 thousand people and does not depend on geographic or ethnic factors. However, there is no doubt that there are many more unidentified cases of SM and so-called mild forms of the disease. Signs of SM are detected in one of the patient’s parents in 60-70% of cases; in the remaining patients, a new mutation of the F1BN1 gene is detected. The pronounced expressiveness of the dominant gene gives rise to a wide range of clinical manifestations of the disease - from extremely severe to difficult to diagnose erased forms of the disease. This can happen within the same family.
The full clinical picture of SM is rare, but there is a clear age-related dynamics in the most persistent symptoms of the disease. In the neonatal period, only signs of arachnodactyly can be noted. An asthenic constitution is formed by the 3rd year, and a characteristic appearance appears by 3-4 years. Pronounced skeletal changes become obvious only by the age of 16.
Patients complain of aching pain in the back and bones. Children with SM begin to walk late, and they often experience joint dislocations. Patients with typical SM are tall and have disproportionately long limbs. Changes in tubular bones are the most typical. The fingers are thin and long - “spider fingers”, “Madonna fingers”.
Weakness of the intercostal muscles is often noted, which contributes to the development of chest deformities. They are of a peculiar nature: retraction at the level of the sternum (funnel chest), protrusion of the sternum (keeled chest), asymmetry of the chest, “wing-shaped” shoulder blades.
Often there are a high palate, a cleft palate, hypodontia, and a symptom of “running” of teeth. Scoliosis and kyphoscoliosis are typical. Pronounced changes in the chest can cause disability.
In the presence of joint hypermobility, its degree is small (unlike Ehlers-Danlos syndrome). Fingers and toes may be crooked. Exostoses of the calcaneal bones, flat feet, transverse and longitudinal are typical. Occasionally, subluxations and dislocations of the fingers and toes are observed: this is explained by the weakness of the ligamentous apparatus. In addition to deformities of the lower extremities, congenital arthrosis of the hip, ankylosis of the fingers, and manifestations of osteoarthritis of other joints can be found in some patients with SM.
Trophic skin disorders are very characteristic: marbling, cyanosis of the fingers, hyperhidrosis or dry skin, brittle nails.
Particularly important in the diagnosis of SM are lesions of the heart and blood vessels: the prognosis for the life of these patients depends on their severity. Anomalies of the cardiovascular system are observed in 50-90% of patients with SM. Changes in the elastic framework of all vessels are generalized. But the most significant changes are the aortic wall: most often the initial part is affected, i.e. valve ring and sinuses of Valsalva. As a result, aortic insufficiency, cardiomegaly, and left ventricular failure develop. As the changes progress, an aortic aneurysm occurs. For this reason, patients, especially those involved in physical work and sports, may suddenly die from rupture or dissection of the aorta. Arterial hypertension also contributes to this. Up to 60% of patients with SM die from aortic rupture at a young age.
Other complications of SM are also dangerous (infective endocarditis, aneurysm of the interatrial septum). Mitral valve prolapse is also a typical manifestation of SM, since the heart valves are thin and easily distensible. The heart may take on a “droplet” appearance.
Patients with SM with damage to the cardiovascular system complain of shortness of breath during physical activity, pain in the heart (long lasting, up to several hours), and interruptions in the heart.
With a shallow examination, they are mistakenly diagnosed with congenital or rheumatic heart defects, usually mitral insufficiency, syphilitic aortitis. Symptoms from the cardiovascular system are variable: from functional noise, presystolic click, lability of pulse and blood pressure, to rough systole-diastolic murmurs over the aorta and pulmonary artery. But variants of aortic damage have been noted when, without the progression of an aneurysm or heart disease, these changes remain unnoticed throughout the life of the patients.
Changes in the organ of vision may also be typical: dislocation (subluxation) of the lens, which leads to myopia, accommodation spasms, less common are aphakia, secondary glaucoma, retinal detachment, myopic astigmatism, macular degeneration, so-called blue sclera, etc. Eye manifestations usually detected after 18 years of age, with the exception of early detected lens subluxation.
Within the framework of SM, dyshistogenetic abnormalities of the lungs are detected: bullous pulmonary emphysema, spontaneous pneumothorax, severe fibrosis, compaction of the roots of the lungs.
Important congenital anomalies of the central nervous system include dilatation of the dura mater, hydrocephalus, dilation of the cisterna magna, and anisocoria. From childhood, attention deficits, learning lags, infantilism are noticeable, and in girls - menstrual irregularities. Asymmetry of reflexes, pyramidal symptoms, and nystagmus are also noted.
When the gastrointestinal tract is affected, long-term intestinal paresis is typical. If SM is accompanied by soft tissue anomalies, then hypoplasia of muscles and adipose tissue, hyperextensibility of tendons and joints are noticeable.
The most important, which cannot go unnoticed, are anomalies in the external appearance of patients with SM: a large nose, a pronounced chin, which gives the face a “bird-like” expression, dysplasia of the ear lobes, anti-Mongoloid eye shape, an senile appearance in children.
It is important to note that a complete set of even cardinal signs of SM in specific patients is practically not found, and the progression of the disease and transformation of the leading symptoms of SM can continue throughout the patient’s life. Differential diagnosis of SM is carried out with similar connective tissue anomalies - S. Ehlers-Danlos, MASS syndrome, Marfan-like familial phenotype, etc.
Diagnosis of SM is practically based on identifying the clinical manifestations of the disease. The diagnosis is confirmed by pedigree analysis and examination of family members by a clinical geneticist.
Diagnostics.
The diagnosis of SM is confirmed by increased levels and excretion of hydroxyproline, but with a stable form of the disease there may be a complete absence of changes in the concentration of hydroxyproline, or this is evidence of the presence of a similar but different disease. Renal excretion of glycosaminoglycans was doubled.
Additional evidence of the presence of arachnodactyly is the assessment of the metacarpal index (the ratio of the length to width of 2-5 metacarpal bones on an x-ray of the right hand; normally it is 6.4-7.9, increasing with SM to 8-11). Wrist tests are also indicative (when the fingers of the stretched hand of one hand are wrapped around the wrist of the other, in the presence of arachnodactyly, the first and fifth fingers are easily connected to each other) and a positive symptom of the thumb, when the extended first finger is brought to the hand and protrudes beyond the soft tissues.
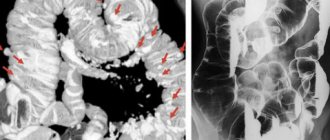
The nature of the CVS lesion and its severity are assessed by echocardiographic examination (aneurysms of various parts of the aorta, enlargement of the cavities of the atria and left ventricle) and Doppler data. If necessary, ultrasound of the abdominal organs and CT examination are performed.
Treatment.
In children with incomplete osteogenesis, so-called collagen-normalizing therapy (beta-blockers, riboflavin, vitamins C and pyridoxine) is performed. Adults undergo so-called situational therapy with beta blockers, potassium supplements, cardiac glycosides, and diuretics. Foci of infection are sanitized.
Main signs of pathology
Often, external symptoms of Marfan syndrome appear already in the first days after the birth of a child and then only intensify. Among the external signs by which pathology can be suspected, it should be noted, first of all:
- increased length of limbs and fingers (dolichostenomelia and arachnodactyly);
- insufficient weight with increased physical development of the child;
- elongated skull shape and elongated face;
- weak, poorly developed muscle tissue, lack of fatty tissue;
- abnormally high joint flexibility;
- awkwardness and clumsiness of movements.
Marfan syndrome in children over four years of age leads to changes in the shape of the chest, curvature of the spine, and the development of flat feet.
Among the ophthalmological symptoms, the most common are myopia, ectopic lens, changes in the shape of the cornea, strabismus, hypoplasia of the iris and retina. Changes often appear already in the first years of life and are bilateral in nature, steadily progressing over time.
The most dangerous are pathological changes in the cardiovascular system, which, in the absence of medical care, lead the patient to death at an early age. This includes changes in the vascular walls, various defects in the structure of the heart and coronary vessels. In the most unfavorable form of the disease, the child develops progressive heart failure already in the first year of life.
In addition, symptoms of Marfan syndrome may manifest themselves in the functioning of other systems and organs. The disease can affect nervous tissues, bronchi and lungs, skin, urinary and reproductive systems.
Are you experiencing symptoms of Marfan syndrome?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Medical history
In 1876, symptoms of an unknown pathology were noted by Dr. Williams, but clinical observations were carried out much later - in 1896 by a pediatrician from France A. Marfan. For 5 years, the doctor assessed the condition of a girl with previously unstudied anomalies, consisting in the progression of skeletal and muscle tissue dystrophy.
By the mid-20th century, there were many described cases in which patients exhibited symptoms close to Marfan's pathology, and all of them were hereditary diseases. Among such cases are aortic dissection, heart defects, ectopia of the lens, accompanied by bone deformation (chest, spine) and external deviations from the norm (tall stature, thinness, long limbs). American geneticist McKusick conducted a detailed study of chromosome mutations and discovered a new group of connective tissue diseases.
How to accurately determine pathology in a child?
Currently, the diagnosis of Marfan syndrome is based on compliance of the clinical picture with the Ghent criteria, developed in 1995 and refined in 2010. They describe a number of signs of pathology for the skeletal system, organs of vision, heart and blood vessels, as well as for other systems and organs. To determine the degree of compliance, the doctor collects anamnesis (including family history), conducts a thorough examination of the patient with phenotypic tests, prescribes laboratory tests and instrumental studies, which include:
- urine test to determine glycosaminoglycans;
- identification of DNA genotype;
- conducting ECG and EchoECG to identify pathologies of the heart and blood vessels;
- performing ultrasound of the heart;
- chest X-ray to document deformities of the skeleton, heart and lungs;
- computed and magnetic resonance imaging.
If necessary, other tests and studies may be prescribed.
Historical reference
The first mention of an unusual disease can be found in the works of the American ophthalmologist E. Williams, who in 1875 described signs of identical displacement of the lenses of the eyes of his siblings. In addition to ophthalmological problems, these children had increased joint mobility and high growth.
The disease gained fame later, 20 years later, when the French pediatrician Antoine Marfan presented his observations of a 5-year-old patient. The little patient was distinguished by unusual skeletal abnormalities and rapid progression of the disease. The syndrome was named after the French doctor, although it later became known that the girl he observed suffered from another hereditary pathology - congenital contractural arachnodactyly.
You can find many examples of the syndrome being detected in talented, famous people. It is believed that violinist Niccolo Paganini, American President Abraham Lincoln, Russian composer Sergei Rachmaninov and other famous personalities suffered from this disease. Some researchers believe that the unusual nature of people with Marfan syndrome is explained by the increased concentration of adrenaline in the blood. This hormone causes an increase in activity and the development of extraordinary abilities.
How are they treated?
Since the disease is genetic in nature, and today medicine does not have the tools to correct gene mutations, treatment of Marfan syndrome is aimed at improving the patient’s condition, stopping the progression of the disease and eliminating clinical manifestations. This is a complex process in which different specialists take part, depending on the nature of the most pronounced symptoms - an orthopedist, a cardiologist, an ophthalmologist, a therapist, and doctors of other specialties.
Clinical recommendations for Marfan syndrome include limiting physical activity to the minimum acceptable level to avoid the development of pathologies of the heart and blood vessels, pneumothorax and other dangerous conditions. Treatment efforts include:
- taking medications;
- if necessary, surgical interventions to correct the most damaged areas of the heart and circulatory system;
- orthopedic correction;
- sanatorium treatment, physiotherapy, physical therapy.
If medical recommendations are followed, the prognosis is almost always favorable: through the efforts of doctors, the course of the disease is significantly improved, they get the opportunity to live a long life without serious health complications.
Why does the genetic syndrome appear?
The cause of the development of the disease is considered to be a mutation in the FBN1 gene, which is located on chromosome 15 and is responsible for the normal production of fibrillin 1. This protein of connective tissue is one of the main components that gives it elasticity and ability to contract.
The first to be affected by the genetic syndrome are the structures containing the largest amount of important protein - the walls of blood vessels, the ligamentous apparatus, and the ligament of cinnamon of the eye. The altered connective tissue is not able to perform its function or withstand physical stress due to loss of strength and elasticity, and the child develops symptoms of the disease.
The disease is genetic and is transmitted from parents in an autosomal dominant manner. The risk of having a baby with a hereditary syndrome is very high if mom or dad has signs of the disease. In 75% of cases of disease, the appearance of the disease in each generation of the family can be traced. In 25% of patients, a new, spontaneous mutation is detected; there is no clear connection with inheritance.
Connective tissue does not form a separate organ in the human body. But its cells are located throughout the body. By means of these structures, supporting, protective and trophic functions are performed, a kind of framework and integument of all organs are formed. Types of connective tissue include cartilage, bone, muscle, adipose tissue, blood and lymph. Therefore, systemic diseases associated with tissue pathology have a wide variety of manifestations.
Treatment methods
Marfan syndrome is incurable. There is no etiotropic therapy for the disease, because it is impossible to replace the genes of a child. Patients are given symptomatic therapy, the purpose of which is to alleviate the general condition, eliminate symptoms and prevent severe complications.
Drug treatment:
- β-blockers – “Propranolol”, “Atenolol”;
- calcium channel blockers - Nifedipine, Verapamil;
- ACE inhibitors - Captopril, Lisinopril;
- collagen normalizing therapy – “Alflutop”, “Rumalon”, “Structum”;
- Metabolics – “Riboxin”, “Mildronate”;
- multivitamin complexes;
- antibiotics for the prevention of infective endocarditis;
- anticoagulants for the prevention of thrombosis;
- antioxidants and antihypoxants – “Coenzyme Q10”, “Elkar”;
- nootropic drugs - Piracetam, Vinpocetine.
When visual acuity decreases, patients with ophthalmological diseases are prescribed glasses for constant wear or contact lenses.
Surgery:
- surgical intervention on the heart and aorta - prosthetics of the aorta and heart valves, reconstructive and plastic surgeries,
- eye surgeries - laser correction of myopia, lens replacement, elimination of glaucoma,
- surgical correction of the skeleton - plasty of the chest with its funnel-shaped deformity, stabilization of the spine, prosthetics of large joints.
People with the erased marfanoid phenotype are indicated for physical therapy and exercise therapy.
Clinical recommendations from specialists to their patients:
- maintaining a healthy lifestyle,
- limitation of hard work and physical overexertion,
- refusal of high-activity sports games,
- regular visits to specialists in the field of cardiology, ophthalmology, orthopedics, neurology,
- keeping patients under constant supervision and control of doctors,
- periodic diagnostic examinations.
Famous people
Despite the fact that this pathology is very rare, many famous people have had this syndrome. Known representatives who had the anomaly:
- Flo Hyman;
- John Tavener;
- Joey Ramone;
- Leslie Hornby.
Historical figures have also been affected by Marfan syndrome. Despite the fact that many died before the pathology was fully studied, it was still possible to find out from photographs and paintings that they had it. The pathology was discovered in the following famous people:
- Niccolo Paganini. He had the standard deformity of the fingers for this disease and was excessively thin. The man was tall, had a sunken chest, and his legs and arms were disproportionately developed.
- Hans Christian Andersen. The writer's body was characterized by an angular face, long arms and poor eyesight.
- Abraham Lincoln. The President of America had not only external manifestations of pathology, but also pain of rheumatic origin, looseness not only in large but also small joints.
- Korney Chukovsky had a strangely shaped nose and long limbs, but even these anomalies did not prevent him from becoming a doctor in philology and one of the finest writers.
Share:
Niccolo Paganini
The famous composer and violinist fell victim to a genetic disease. Long, unusually mobile and flexible fingers allowed the musician to achieve success in his chosen profession.
The appearance of Niccolo Paganini, according to the descriptions of his contemporaries, looked strange and frightening: excessive thinness and pallor, tall stature, incorrect posture, deformed chest, legs of unequal length and disproportion. In addition, at his concerts and performances, the brilliant musician amazed the audience with his unusual manner of performance and the feverish movements that made Paganini a legend.
View this post on Instagram
A post shared by Drunk Grandma (@babushkaalkashka) on Jul 30, 2020 at 8:42pm PDT
Prognosis and life expectancy
The prognosis largely depends on the degree of cardiovascular and skeletal changes, as well as visual impairment. If you ignore treatment, the life expectancy rarely exceeds 30-45 years, and he faces sudden death, but with timely help, the prognosis is more comforting. Modern medicine has ensured that patients live to an advanced age (up to 70), while leading a moderate lifestyle. However, mortality is still high (the probability of not living to age 50 is 90-95%). There is a high risk of complications. Disability is given for decreased vision.
The main cause of death is heart failure, caused by an aneurysm, subsequent rupture of the aorta and regurgitation (backflow of blood) of the heart valves. These events occur during physical activity. This is where all the danger lies.
Since people with this syndrome have an asthenic physique, especially long arms, this allows them to go into sports due to their wide arm span, but precisely such loads carry a mortal danger.
Consequences and complications
As the syndrome progresses, the likelihood of complications occurring is quite high. The most common complications are:
- cataract (clouding of the lens);
- glaucoma (periodic increase in intraocular pressure);
- complete blindness;
- postural disorders (latest degrees of kyphosis, scoliosis);
- mitral valve prolapse (sagging of its valves when the left ventricle of the heart contracts);
- congestive heart failure caused by impaired contractility of the heart muscle;
- dissecting aneurysm;
- spontaneous pneumothorax;
- pneumonia;
- stroke;
- thrombosis.
The most serious complication is rupture of the aneurysm, which leads to death.
The most common complication of the syndrome, which ends in death
Pathogenesis
More than half of human weight is represented by connective tissue. It consists of the skeleton, skin, and vascular walls.
If we look in more detail at the mechanism of the disease, we need to start with the fact that each cell of the body that has a nucleus contains 23 pairs of chromosomes. Absolutely each of the chromosomes was formed from 1 molecule of deoxyribonucleic acid (or DNA). DNA contains a large number of genes. Thus, each chromosome contains from 429 to 3511 genes.
One of the genes, fibrillin-1, is located on the long arm of chromosome 15 and is designated FBN1. It is responsible for encoding a large structural protein, which is part of microfibrils (organelles of muscle fibers) and is responsible for creating tissue elasticity and the formation of a strong cytoskeleton (the “skeleton” of cellular structures). Defects in fibrillin-1 lead to mutation.
Elastin fibrils are an integral part of large vessels and ligaments. Often, when these fibrils are disrupted, aneurysms appear.
The syndrome causes damage to transforming growth factor beta (TGF-β), which controls proliferation (proliferation of cellular elements) and cellular differentiation (distribution of functions). There is a disruption in the binding of the inactive form of TGF-β, which will entail an increase in the activity of the factor, which means that all the signs of the syndrome will appear.
Due to a genetic disorder, there is a loss of elasticity of the skin and other connective tissue, and a loss of their strength. Loose joints occur, and the skin can stretch greatly.
Due to changes in collagen fibers, normal hemostasis fails, which is designed to maintain the liquid state of the blood, dissolve blood clots, and stop bleeding through blood clotting. Defects lead to impaired aggregation (combination) of platelets (one of the elements of blood). Fibrils (cytoplasmic fibers) are involved in hemostasis. Along with slow blood flow inside the vessels, platelet adhesion to elastin occurs (their adherence) with the help of fibronectin. Fibronectin ensures the restoration of structures, creating the necessary components of connective tissue - fibroblasts. Individuals suffering from the syndrome have a deficiency of fibronectin.
Problems with the gastrointestinal tract are caused by an increased content of collagen in the digestive system. There is dysfunction of the biliary tract (bile tract, gall bladder), chronic gastroduodenitis, dolichosigma (abnormal lengthening of one of the sections of the colon), hiatal hernia.
Due to the above factors, characteristic signs of the syndrome arise.
Classification
Marfan syndrome occurs differently for everyone. Considering the severity, it happens:
- light;
- average
; - heavy.
Severe ones are very rare, 1 in 50,000.
Based on how many body structures are affected, Marfan syndrome is classified into 2 forms:
- erased
(there are mild deviations in 1 or 2 systems); - pronounced
(there are implicit deviations in 3 systems or expressed in 1; pronounced deviations in 2, 3 systems or more).
The nature of the course is progressive
(rapidly progressing signs, deterioration of the condition) and
stable
(unchanging signs of the syndrome over many years).
All cases of the disease are divided as follows:
- family
(inherited from generation to generation) – make up 75%; - random
or
sporadic
(disease occurring for the first time in the family) – account for 25%.
Diagnostic methods
manifestations of Marfan syndrome at a young age
Specialists in the field of genetics, cardiology, ophthalmology, neurology, and orthopedics are involved in identifying Marfan syndrome. Diagnosis of pathology includes collecting an anamnesis of life and illness, identifying typical clinical signs, analyzing an external examination and physical data, the results of a cardiographic and radiographic examination, visiting an ophthalmologist, and drawing up a pedigree from a geneticist.
Basic diagnostic techniques:
- general blood and urine analysis - typical signs of inflammation;
- a biochemical blood test allows you to identify dysfunction of a certain organ that has arisen as a result of the development of a pathological process, as well as determine the root cause of the disease and prescribe the correct treatment;
- electrocardiography displays electrical potentials formed in the beating heart;
- echocardiography – study of morphological and functional changes in the heart and its valve apparatus;
- X-ray and tomographic examination are informative diagnostic techniques that detect damage to bones, joints, internal organs and soft tissues;
- aortography - X-ray examination of the aorta using a contrast agent;
- Ultrasound of internal organs,
- biomicroscopy and ophthalmoscopy,
- molecular genetic analysis.
Prevention
No specific prevention has been developed, so there is no way to prevent the mutation, which in half of the cases will definitely be inherited, but for those already suffering from Marfan syndrome there are a number of restrictions that will prevent them from serious consequences.
Prohibited
:
- strong physical activity;
- participation in sports competitions, scuba diving, contact sports;
- work in hazardous industries;
- being in a place where background radiation is high.
If possible, it is better to change the hot climate to a temperate one.
Patients need to be seen regularly by a doctor (every six months). Light physical activity, race walking, ball games, and basic exercises (squats, turns, stretching) are allowed.
You should not ignore caries, the common cold or helminthic infestations, as they also significantly aggravate the course of the syndrome, since the immunity with such a diagnosis is much weaker than in healthy people.
To prevent Marfan disease, diagnosis should be carried out at the stage of conception in order to calculate all the risks, since the pathology is inherited with a high degree of probability.