Medicinal and herbal diuretics.
September 23, 2021
25077
4.6
1
Content
- How to choose a diuretic
- What are the types of diuretics?
- Classes of diuretics and indications for their use
- The best diuretics
- Hydrochlorothiazide
- Furosemide
- Indapamide
- Veroshpiron
- Torasemide
- Triampur compositum
- Diuver
- Dog-rose fruit
- Diuretic collection
- Juniper fruits
The doctor prescribes diuretics for various edema, hypertension, for the prevention of kidney stones, etc. It is no secret that some women even try to lose weight with the help of diuretics, but this is dangerous to health. The fact is that diuretics, together with liquid, remove potassium from the body - muscle contraction (including the heart muscle) is disrupted. That is why such drugs should be prescribed exclusively by a doctor, taking into account the underlying disease, possible contraindications and side effects.
Read also How to treat dehydration: 5 solutions for rehydration What drugs for dehydration are most often prescribed by doctors?
Contraindications of drugs
The use of diuretics is not always advisable. There are certain conditions that prohibit the use of this type of medicine. These include:
- Low potassium levels in the blood.
- Individual intolerance to sulfonamide substances.
- Severe form of respiratory failure.
- Acute kidney diseases.
- Any type of diabetes.
An implicit contraindication to taking diuretics is ventricular arrhythmia. This clinical condition requires adjustment of the therapeutic dose and strict medical supervision.
How to choose a diuretic
There are specific factors to consider if you choose a diuretic.
- Speed of action.
There are diuretics for emergency use: if you need to quickly lower high blood pressure (used in combination with other drugs), remove morning puffiness under the eyes. You should not take such medications often because they are addictive. Long-acting diuretics are prescribed to treat hypertension and edema associated with poor heart and liver function. - Pregnancy and breastfeeding.
Any diuretic medications are prohibited for pregnant and lactating women. And only in cases where a pregnant or lactating woman has a threat to her health and life, is it possible to use them. Usually this phrase sounds like “the benefit to the mother outweighs the risk to the fetus.” The exception is practically harmless herbal diuretics, but a woman should talk to her doctor before using them. - Tendency to allergies.
People with allergies may experience an undesirable reaction to both the active ingredient of the diuretic drug and its minor components. If you are allergic, consult your doctor before treatment.
In addition to diuretic medications, mild herbal remedies are often used. They are usually prescribed in the complex treatment of cystitis, urethritis, etc. Herbal diuretics not only remove excess water, but also relieve inflammation.
Drinking diuretics for weight loss is dangerous - the heart muscle suffers
Photos from open sources
What are the types of diuretics?
All diuretic drugs are divided into several categories: according to their spectrum of use and mechanism of action.
- Loop diuretics.
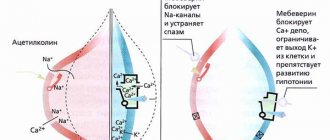
These drugs have the strongest effect (they begin to act literally a few minutes after administration), but the effect ends just as quickly. Such drugs are well suited for the treatment of hypertension and heart failure. But loop diuretics have a significant disadvantage - along with water, they remove potassium from the body, which is fraught with the development of arrhythmia. - Thiazide diuretics.
Another effective diuretic drug. They not only get rid of excess fluid, but also dilate peripheral vessels. Thiazide diuretics also reduce the response of blood vessels to adrenaline, so they spasm less. Such diuretics are also prescribed for the treatment of urolithiasis. Among the “side effects” are the excretion of potassium and an increase in uric acid, which can then accumulate in the joints and cause gout. - Potassium-sparing diuretics.
Such diuretics do not remove potassium from the body, protecting the patient from various heart complications. But these drugs are not as potent as the previous ones. - Osmotic diuretics.
This group of drugs reduces blood plasma pressure - excess water is quickly removed from the tissues, swelling goes away. The pressure in the tissues and in the plasma becomes the same. Typically, osmotic diuretics are prescribed to relieve swelling of the brain, lungs, and high intraocular or intracranial pressure.
When does a doctor prescribe diuretics?
List of indications for use:
- Arterial hypertension not complicated by renal failure
. A decrease in systolic pressure occurs due to a decrease in blood volume in the vascular system. There is no sharp drop in pressure; its levels decrease moderately, without the development of hypotension. The hypotensive effect is achieved by increasing the potassium content and decreasing sodium. After 1-2 months, diastolic pressure normalizes while maintaining cardiac output. Diuretics are not addictive and do not affect potency or libido.
- Chronic circulatory failure due to edema and arterial hypertension
. To correct this condition, strong diuretics of short and medium duration are used. Indications for emergency treatment: pulmonary edema, cerebral edema, barbiturate poisoning.
- Prevention of hypokalemia and secondary hyperaldosteronism
against the background of hypertension and chronic renal failure.
- Diabetes insipidus.
- Glaucoma.
Classes of diuretics and indications for their use
Main indications for the use of diuretics of various classes
| Diuretic class | Indications |
| Osmotic | Edema of the brain, lungs, acute attack of glaucoma, barbiturate poisoning |
| Carbonic anhydrase inhibitors | Edema due to pulmonary heart failure, glaucoma, epilepsy |
| Loop | Hypertensive crisis, cerebral edema, chronic renal failure, poisoning with water-soluble poisons |
| Thiazides and thiazide-like diuretics | Hypertension, cardiovascular failure, liver cirrhosis, nephrosis, pregnancy nephropathy, glaucoma |
| Potassium-sparing | Hypertension, heart failure, liver cirrhosis, hypokalemia during treatment with diuretics of other groups |
| Vegetable | Renal edema, whistitis, chronic renal failure |
| Xanthine derivatives | Hypertension, heart failure (in complex therapy) |
Hydrochlorothiazide
One of the most effective means for removing excess fluid and sodium salts from the body. Hydrochlorothiazide is prescribed for diseases of the kidneys, heart, lungs, to reduce blood pressure and reduce swelling. The drug does not form metabolites and is excreted unchanged by the kidneys. The maximum effect of the diuretic is achieved 4 hours after administration, and it lasts for 12 hours. Patients about it has a pronounced diuretic effect, any swelling quickly goes away, it is inexpensive. Among the disadvantages is a large list of “side effects” and the removal of important microelements from the body (including potassium and magnesium).
Hydrochlorothiazide
OZON, Russia; Pranapharm LLC, Russia; PJSC "Biokhimik", Russia; OJSC Borisov Plant of Medical Preparations (Borimed), Belarus; PJSC Valenta Pharm, Russia
A diuretic drug that is used for: Arterial hypertension, edema syndrome of various origins (chronic heart failure, nephrotic syndrome, renal failure, fluid retention in obesity), diabetes insipidus, glaucoma (subcompensated forms).
from 34
5.0 1 review
1271
- Like
- Write a review
"Hurry slowly." Long-acting diuretics for long-term therapy of outpatients
The main classes of drugs widely used today came into therapeutic practice in the form of short-acting drugs. This applies to beta blockers (BBs), angiotensin-converting enzyme inhibitors (ACEIs), and dihydropyridine calcium channel blockers (CCBs). Second half of the 20th century was marked by a significant breakthrough in the treatment of arterial hypertension (AH) due to the introduction of propranolol [1], and later nifedipine [2] and captopril [3]. Further clinical experience with the use of these drugs has made significant adjustments to the tactics of their prescription. It turned out to be extremely difficult to ensure regular 3-4 times a day medication intake for patients not undergoing hospital treatment. Attempts to prescribe propranolol once a day instead of three times were not very successful - even with a comparable antihypertensive effect, stable suppression of neurohumoral systems was achieved only with three doses [4]. The enthusiastic tone of the first publications concerning nifedipine also soon gave way to a more cautious one [5]. It was shown that the rapid and potent effect of this antihypertensive agent was accompanied by significant activation of the renin-angiotensin-aldosterone (RAAS) and sympathoadrenal systems (SAS) [6], which could have a negative impact on long-term prognosis. The solution to most of these problems came with the creation of drugs that have a long period of action. Suppression of neurohumoral systems during the day prevented their “rebound” activation, ensured stable control of blood pressure and significantly improved the quality of life of patients and their adherence to treatment [7–10]. Currently, no one doubts that in the outpatient management of patients, preference should be given to long-acting BBs, CCBs and ACEIs, and short-acting drugs of these classes retain their positions mainly in emergency situations.
The history of diuretics, one of the oldest classes of drugs used in the treatment of cardiovascular diseases, has not been so straightforward. At the end of the 1950s. Chlorothiazide, hydrochlorothiazide (HCTZ), and chlorthalidone (CT) were reported almost simultaneously. These drugs, having a similar chemical structure, differ significantly in pharmacokinetics. If thiazides can be classified as short-acting drugs, the half-life of CT, a thiazide-like diuretic, can reach 40–60 hours.
Data on a positive effect on the prognosis for patients with hypertension were obtained for both HCTZ and chemotherapy. At the end of the 1960s. placebo-controlled studies have been conducted showing the ability of diuretics to reduce cardiovascular mortality [11, 12]. The data obtained indicated the need to treat only 2.7 patients to prevent one cardiovascular complication (CVD). And currently, diuretic therapy has the lowest price/effectiveness ratio of all methods of primary prevention, second only to a diet that limits salt intake [13].
The effect of chemotherapy-based therapy on the incidence of stroke and other CV events in 4736 patients with isolated systolic hypertension was studied in the SHEP study. Compared with placebo, chemotherapy reduced the incidence of stroke by 36%, myocardial infarction by 27%, chronic heart failure (CHF) by 54%, and the total number of cardiovascular events by approximately 32% [14]. The ALLHAT trial [15, 16] randomized more than 42,000 patients with hypertension and either known cardiovascular disease or risk factors for its development. In this study, chemotherapy was not inferior to such powerful competitors as the ACE inhibitor lisinopril and the CCB amlodipine, either in its effect on the combined primary endpoint or on mortality.
It should be noted that other data have been published, according to which diuretics showed less effectiveness than other classes of antihypertensive drugs. In the ACCOMPLISH study [17], 11,506 hypertensive patients at high risk for CV events received either benazepril with amlodipine or benazepril with HCTZ for 36 months. The reduction in the relative risk of developing cardiovascular events was 20% greater in the group of patients receiving a combination of amlodipine and benazepril, despite a similar decrease in office blood pressure (BP). The failure of HCTZ may have been due to the fact that the drug was used in this study at lower doses (12.5–25 mg) than those used in the placebo-controlled trials. Moreover, in the SHEP study, chemotherapy at a dose of more than 12.5–25.0 mg controlled blood pressure in 50% of patients for several years without significant adverse effects [14]. In vitro, CT is 2 times more effective than HCTZ [18]. However, an analysis of clinical studies showed that an equivalent antihypertensive effect is achieved with 3 times higher doses of HCTZ [19]. As the main reason for this superiority of CT MA, Peterzan et al. They call differences in the pharmacokinetics of drugs - a significant difference in the duration of their action.
Loop diuretics (LDs) are traditionally used in the treatment of patients with uncomplicated hypertension to a lesser extent than thiazide-type diuretics. This circumstance is probably explained not only by the lack of studies indicating the influence of PD on prognosis, but also by existing stereotypes. For example, low doses of HCTZ are widely prescribed by physicians and cardiologists to lower blood pressure, while no data have been obtained confirming their positive effect on the risk of developing CV events in patients with hypertension. PD is generally preferred when a patient develops cardiac or renal failure. The situation changed somewhat with the advent of the late 1980s. torasemide, a PD with a long half-life. A number of studies have been conducted to examine its antihypertensive effect and tolerability. Torsemide was used in doses that did not lead to a significant diuretic effect (2.5–5 mg/day) in monotherapy or in combination with other antihypertensive drugs. Diastolic pressure has been demonstrated to decrease to target values after 8–12 weeks of treatment in 70–80% of patients. At doses of 10 mg/day, diastolic pressure normalized in more than 90% of patients [20]. Treatment with torasemide was started in most cases with low doses. In cases where it was not possible to achieve optimal blood pressure control, the dose was increased. In light of the discussion on the importance of the duration of action of a diuretic drug, the work of I. Achhammer et al. is of interest. [21], which demonstrated comparable antihypertensive effects of torsemide and chlorthalidone (Fig. 1).
It is known that prolonging the circulation period of a diuretic in the blood can reduce peak natriuresis, thereby preventing “rebound” sodium reuptake and hyperactivation of the RAAS and SAS [22, 23]. This effect can be achieved either by prolonging the half-life or by creating sustained-release dosage forms. Torsemide itself has a longer half-life compared to Furosemide - 180–240 minutes versus 90 minutes [24], but, in addition, its new form with a slow release of the drug (Britomar) has appeared relatively recently [25]. The matrix tablet allows you to further increase the time to reach the maximum concentration of torasemide in the blood [26], thereby minimizing the activation of neurohumoral systems (Fig. 2).
In clinical practice, such differences in the pharmacokinetics of immediate- and sustained-release torasemide are realized in a more pronounced effect on the blood pressure of the latter [27] (Fig. 3).
There is no doubt that randomized trials are required to evaluate the impact of both PD and low-dose HCTZ on prognosis. However, the advent of sustained-release torasemide has significantly expanded the possibilities of using PDs as antihypertensive drugs. In the USA, torasemide in small doses has been recommended since the 6th (1993) report of the Expert Committee of the US National Heart, Lung and Blood Institute for long-term treatment of hypertension [28].
Nevertheless, the main area of application of PD in cardiology has been and remains heart failure. In Russian recommendations on CHF [29], the place of diuretics is defined as the place of drugs “used in certain clinical situations.” First of all, we mean patients who have signs of fluid retention: edema, shortness of breath, moist rales in the lungs, etc. However, the need to prescribe PD to patients without clinical manifestations of congestion, but with signs of increased left ventricular filling pressure, is currently being discussed [30 ].
Noteworthy is the fact that in the recommendations for CHF treatment with diuretics, evidence class IC is assigned. This means that “this method is useful and effective.” However, the “C” label assumes that “the recommendation is based on expert consensus and/or the results of small studies, retrospective studies, registries.” Indeed, it is unlikely that a doctor who had to treat a patient with CHF in a state of decompensation would have doubts about the need to use diuretics. On the other hand, randomized placebo-controlled trials with diuretics in CHF have not been conducted and most likely will not be conducted. The largest published comparative study with the TORIC PD examined the effect of torasemide versus furosemide (or other diuretics) on the clinical course and mortality of patients with CHF [31]. It included 1350 patients with FC II–IV CHF, the observation period was 12 months, the average dose of Furosemide was 40 mg (it was used in more than 85% of patients), torsemide 10 mg. Torasemide was superior to Furosemide both in its effect on the frequency of hospitalizations and on the clinical condition of patients. But the most striking differences were in the effects on total, cardiovascular and sudden mortality (Fig. 4).
In many studies in patients with CHF, diuretics with a short half-life - Furosemide and thiazides - were prescribed twice a day to achieve better effect [32]. However, an attempt to attribute the benefits of torasemide only to the duration of its action would look tendentious. This drug has a number of pleiotropic effects. Its antialdosterone activity prevents the development of fibrosis and excess potassium excretion [33, 34]. It is impossible to single out the predominant influence of different mechanisms of action of a drug on the prognosis, but when talking about ensuring the quality of life of patients, the duration of action of the drug takes on independent significance. In a number of comparative studies, patients with CHF reported more comfortable excretion of excess fluid on torsemide than on Furosemide [24, 35, 36]. A “pure” experiment can be considered a comparison of immediate-release torasemide with a drug in which the same torasemide molecule is packaged in a hydrophilic matrix, ensuring its consistent absorption in the intestine. The sustained-release form (Britomar) was significantly less restrictive in daily activities in patients with more severe natriuresis [37].
Conclusion
The requirements for long-term diuretic therapy are not original - high efficiency, maximum safety, good tolerability. Modern diuretics largely provide the required diuretic response. However, achieving the last two criteria in real practice is often difficult due to limited laboratory monitoring of electrolyte levels and low patient adherence to treatment associated with disruption of the usual lifestyle when taking diuretics. In the conditions of outpatient management of patients, it is possible to approach this level only by prescribing diuretics with a long period of action. “Festina lente” - hurry up slowly.
Literature
- Richards F. Propranolol in hypertension // Am J Cardiol. 1966 Sep; 18(3):384–386.
- Olivari M., Polese A., Fiorentini C. et al. Nifedipine, a new antihypertensive with rapid action // Clin Pharmacol Ther. 1977; 22 (5 Pt 1): 528–532.
- Rubin B., Antonaccio M., Horovitz Z. Captopril (SQ 14,225) (D-3-mercapto-2-methylpropranoyl-L-proline): a novel orally active inhibitor of angiotensin-converting enzyme and antihypertensive agent // Prog Cardiovasc Dis . 1978; 21 (3): 183–194.
- Van den Brink G., Boer P., van Asten P. et al. One and three doses of propranolol a day in hypertension // Clin Pharmacol Ther. 1980; 27 (1): 9–15.
- Stone P., Antman E., Muller J. et al. Calcium channel blocking agents in the treatment of cardiovascular disorders. Part II: Hemodynamic effects and clinical applications // Ann Intern Med. 1980; 93(6):886–904.
- Corea L., Miele N., Bentivoglio M. et al. Acute and chronic effects of nifedipine on plasma renin activity and plasma adrenaline and noradrenaline in controls and hypertensive patients // Clin Sci (Lond). 1979; 57 Suppl 5: 115 s-117 s.
- Calcium antagonists in cardiovascular disease: rationale for 24-hour action. Proceedings of an official satellite symposium and papers on amlodipine presented at the 25th Anniversary International Symposium on Calcium Antagonists in Hypertension. Basel, Switzerland, February 11–12, 1988 // J Cardiovasc Pharmacol. 1988; 12 Suppl 7:S1–114.
- Buhler F., Burkart F., Lutold B. et al. Antihypertensive beta blocking action as related to renin and age: a pharmacologic tool to identify pathogenetic mechanisms in essential hypertension // Am J Cardiol. 1975; 36(5):653–669.
- Van den Broek S., de Graeff P., van Veldhuisen D. et al. Clinical and neurohumoral differences between spirapril and captopril in mild to moderate chronic congestive heart failure // J Card Fail. 1997; 3 (3): 165–171.
- Ruszty L., Hidas I., Ivanyi J. et al. Evaluation of captopril-enalapril replacement therapy in hypertensive patients under ambulatory blood pressure monitoring // Orv Hetil. 1996; 137(51):2851–2854.
- Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressure averaging 115 through 129 mm Hg. Veterans Administration Cooperative Study Group on Antihypertensive Agents // JAMA. 1967; 202:1028–1034.
- Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. Veterans Administration Cooperative Study Group on Antihypertensive Agents // JAMA. 1970; 213:1143–1152.
- Cobiac L., Magnus A., Lim S. et al. Which interventions offer best value for money in primary prevention of cardiovascular disease? // PLoS One. 2012; 7(7):e41842.
- SHEP cooperative research group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the systolic hypertension in the elderly program (SHEP) // JAMA. 1991; 265:3255–3264.
- Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) // JAMA. 2002; 288:2981–2997.
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Diuretic versus alpha-blocker as first-step antihypertensive therapy. Final results from the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) // Hypertension. 2003; 42: 239–246.
- Jamerson K., Weber M., Bakris G. et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients // N Engl J Med. 2008; 359:2417–2428.
- Beaumont K., Vaughn D., Fanestil D. Thiazide diuretic drug receptors in rat kidney: identification with metolazone // Proc Natl Acad Sci USA. 1988; 85:2311–2314.
- Peterzan M., Hardy R., Chaturvedi N. et al. Meta-analysis of dose-response relationships for hydrochlorothiazide, chlorthalidone, and bendroflumethiazide on blood pressure, serum potassium, and urate // Hypertension. 2012; 59(6):1104–1109.
- Brater D. Benefits and risks of torasemide in congestive heart failure and essential hypertension // Drug Saf. 1996; 14: 104–120.
- Achhammer I., Metz P. Low dose loop diuretics in essential hypertension. Experience with torasemide // Drugs. 1991; 41(Suppl. 3): 80–91.
- Reyes A. Effects of diuretics on renal excretory function // Eur Heart J. 1992; 13 Suppl G: 15–21.
- Arutyunov G.P., Oganezova L.G., Dragunov D.O. Relationship between the half-life of a loop diuretic, the severity of natriuresis and central hemodynamic parameters in patients with CHF (pilot study) // Heart failure. 2012; 13 (4): 222–227.
- Vargo D., Kramer W., Black P. et al. Bioavailability, pharmacokinetics, and pharmacodynamics of torsemide and furosemide in patients with congestive heart failure // Clin. Pharm. Ther. 1995; 57:601–609.
- Lyseng-Williamson K. Torasemide Prolonged Release // Drugs. 2009; 69(10):1363–1372.
- Barbanoj M., Ballester M., Antonijoan R. et al. Comparison of repeated-dose pharmacokinetics of prolonged-release and immediate-release torasemide formulations in healthy young volunteers // Fundamental & Clinical Pharmacology. 2009; 23: 115–125.
- Roca-Cusachs A., Aracil-Vilar J., Calvo-Gomez C. et al. Clinical effects of torasemide extended release in mild-to-moderate hypertension: A randomized noninferiority trial versus torasemide immediate release // Cardiovasc Ther. 2008; 26:91–100.
- Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI) // Arch Intern Med. 1997; 157:2413–2446.
- National recommendations of VNOK and OSSN for the diagnosis and treatment of CHF (III revision) // Heart failure. 2010; 11, No. 1 (57).
- Azizova A. G., Ovchinnikov A. G., Ageev F. T. Comparative effect of torasemide and furosemide on the clinical status and diastolic function of the left ventricle in patients with compensated heart failure and high filling pressure of the left ventricle // Heart failure. 2011; 6:326–332.
- Cosyn J., Dyez J. Torasemide in chronic heart failure; results of the TORIC study // The European Journal of Heart Failure. 2002; 4:507–513.
- Jentzer J., DeWald T., Hernandez A. Combination of Loop Diuretics With Thiazide-Type Diuretics in Heart Failure // Journal of the American College of Cardiology. 2010; 56(19):1527–1534.
- Lopez B., Querejeta R., Gonzalez A. et al. Effects of loop diuretics on myocardial fibrosis and collagen type I turnover in chronic heart failure // J Am Coll Cardiol. 2004; 43:2028–2035.
- Reyes A., Leary W. Response of serum potassium concentration to the diuretic torasemide: formal assessment // AHJ. 2002; 15 (4): 38 A.
- Muller K., Gamba G., Jaquet F. et al. Torasemide vs. furosemide in primary care patients with chronic heart failure NYHA II to IV - efficacy and quality of life // Eur J Heart Fail. 2003; 5(6):793–801.
- Noe L., Vreeland M., Pezzella S. et al. A pharmaco-nomical assessment of torasemide and furosemide in the treatment of patients with congestive heart failure // Clin Ther. 1999; 21(5):854–856.
- Barbanoj M., Ballester M., Antonijoan R. et al. Comparison of repeated-dose pharmacokinetics of prolonged-release and immediate-release torasemide formulations in healthy young volunteers // Fundamental & Clinical Pharmacology. 2009; 23: 115–125.
Y. A. Orlova, Doctor of Medical Sciences, Professor
Medical Research and Educational Center of the State Budgetary Educational Institution of Higher Professional Education, Moscow State University named after. M. V. Lomonosova, Moscow
Contact Information
Furosemide
This diuretic is one of the most popular and frequently prescribed, and is a strong diuretic. Furosemide removes excess water and sodium salts from the body well and quickly, and relieves swelling. The drug is indicated for hypertension, poor functioning of the heart, kidneys and liver. Diuretic tablets begin to act 20-30 minutes after administration. Furosemide is usually used in emergency cases. You cannot take the drug without medical supervision, because self-medication can lead to dehydration. Furosemide is inexpensive, acts quickly, but has many side effects, including the removal of potassium and magnesium.
Furosemide
Sopharma, Bulgaria; PJSC "Biosintez", Russia; Binnopharm, Russia; JSC Avexima, Russia; Update, Russia; JSC Pharmstandard-TomskKhimPharm, Russia; "Moskhimfarmpreparaty" named after. N. A. Semashko, Russia; Ozon LLC, Russia; OJSC Borisov Plant of Medical Preparations (Borimed), Belarus; JSC Dalkhimfarm, Russia
Edema syndrome of various origins (with chronic heart failure, cirrhosis of the liver (portal hypertension syndrome); edematous syndrome of renal origin (with nephrotic syndrome, treatment of the underlying disease is in the foreground), acute heart failure, especially with pulmonary edema (used in combination with other therapeutic agents) measures); cerebral edema; severe forms of arterial hypertension; hypertensive crisis; forced diuresis in case of poisoning with chemical compounds excreted unchanged by the kidneys.
from 17
2.0 1 review
1317
- Like
- Write a review
Distinguishing the cause of edema
Of course, this material is not addressed to doctors, but a specialist should understand the causes of edema. But the modern Russian healthcare system is designed in such a way that it is extremely difficult to immediately get free access to a specialist; you must first visit a therapist as a “divorce”. Therefore, many turn to a paid doctor, and the main thing is to choose exactly who to turn to for edema: a cardiologist, a vascular surgeon who deals with the problems of varicose veins, or, for example, a nephrologist.
In order to figure this out right away and not spend extra money, we can tell you general but important information about edema:
- You should visit a cardiologist if swelling occurs in the legs; it is symmetrical and painless, intensifies in the evening, and leaves a pit of doughy consistency after pressing. Additional symptoms include shortness of breath; the patient often has long-term chronic heart damage, for example, valvular defects, previous myocardial infarction or arrhythmia;
- if swelling also occurs in the legs, but together with a feeling of heaviness in the calves, aching pain, night cramps, and appears after prolonged standing or long walking, and decreases overnight, then this is due to varicose veins of the lower extremities . This is especially true if, after a long period of such edema, spider veins, peeling of the skin, or the phenomenon of varicose dermatitis occur. We need a phlebologist or vascular surgeon;
- if in this case the swelling of the leg is asymmetrical, on the one hand, the leg is hotter than the other, then, most likely, we are talking about thrombosis of the venous vessels, and here you need to contact a vascular surgeon;
- if the patient has a long-term chronic pathology of the kidneys, swelling appears on the face, on the eyelids, does not change its location depending on changes in the state of the body in space, is not accompanied by shortness of breath, and in matcha tests a high protein is determined, more than 3 g per day, then speech It's about nephrotic syndrome. If the patient has high blood pressure and a small amount of urine, then it is necessary to urgently visit a nephrologist or kidney disease specialists;
- if a person had jaundice, active hepatitis, cirrhosis was diagnosed, the amount of protein in the blood plasma was reduced, the level of bilirubin and transaminases was high, and his stomach swells like a drum, his navel protrudes, then everything is clear. We are talking about the development of ascites, or the accumulation of fluid in the abdominal cavity and portal hypertension, and here it is necessary to visit either a hepatologist for liver diseases, or an infectious disease specialist in the case of chronic viral hepatitis, or a surgeon.
Finally, if lymphatic edema associated with lymphostasis occurs, then at first the edema may be asymmetrical, on the one hand. But even if they become double-sided, they may also not be the same. At first these are soft swellings, like dough, they can intensify in hot weather, the skin over them easily moves. If they exist for a long time, then the skin over them thickens and becomes denser, the hole no longer remains, and in the later stages complete tissue fibrosis develops. The skin becomes lumpy and separated by deep folds. This happens when lymph nodes and lymphatic vessels are compressed, and in our country this most often occurs in advanced forms of cancer pathology. An urgent consultation is needed, first of all, with an oncologist.
Treatment of edema should always be comprehensive, and treatment should begin with attempts to eliminate the cause. So, if the cause is chronic heart failure, then it is necessary to enhance the work of the heart, for example, by using cardiac glycosides. In the presence of glomerulonephritis, it is necessary to use hormones and cytostatics; in the presence of hypothyroidism and myxedema, thyroid hormones must be prescribed, and so on.
However, in addition to etiotropic treatment aimed at the direct cause of edema, it is necessary to limit the intake of fluid, and for generalized edema it is necessary to limit salt intake, and one of the most important methods of pathogenetic treatment of edema syndrome is the prescription of modern diuretics, or diuretics. How are diuretics used, and what are diuretics? What caution should patients and physicians take when using them?
Indapamide
This is a moderate-acting drug that is usually prescribed for edema associated with heart failure. "Indapamide" is quickly absorbed into the gastrointestinal tract. Diuretic tablets reduce the load on the heart and peripheral vessels and stabilize blood pressure. The effect occurs an hour after taking the drug and lasts 12-18 hours. You can buy Indapamide with a prescription, it is inexpensive, but it is a generic (not the original drug). Be sure to check the possible side effects.
Indapamide
OZON, Russia
Arterial hypertension;
sodium and water retention in chronic heart failure. from 8
885
- Like
- Write a review
Veroshpiron
This is a potassium-sparing diuretic, which is prescribed for edema due to chronic heart failure and hormonal problems. And although Veroshpiron has a weak diuretic effect, the drug does not remove potassium and does not upset the acid-base balance in the body. The maximum effect of the diuretic occurs after 2-3 days and lasts a long time. You can buy Veroshpiron with a prescription; it is important to take into account the impressive list of contraindications.
Veroshpiron
Gedeon Richter, Hungary
The drug Veroshpiron is a potassium-sparing diuretic.
from 64
917
- Like
- Write a review
Read also Diet pills: effective drugs for weight loss List of the most effective weight loss pills.
Loop diuretics
Loop diuretics have the following properties:
- Act quickly (within 15-30 minutes);
- The effect of the drug lasts for 2-6 hours;
- When administered intravenously, hemodynamic parameters are changed: end-diastolic pressure and end-diastolic volume are reduced in case of left ventricular failure and pulmonary hypertension);
- Reduce the volume of extracellular fluid and the intensity of shortness of breath.
Loop diuretics, due to their advantages, are often used in emergency complex relief of symptoms of cardiovascular and renal failure.
Video about the effect of various diuretics on the human body:
Representatives of loop diuretics:
- Furosemide (Lasix).
The drug for rapid action is taken on an empty stomach, it acts after 30-50 minutes, when administered intravenously - after 5 minutes. When administered orally, after 4-6 hours, most of the active substance is excreted in the urine; when administered intravenously, after 2 hours.
- Torasemide
. It has a longer duration of action and removes less potassium than Furosemide. In the treatment of heart and kidney failure, Lasix is more effective.
- Bumetanide
(Burinex, Yurinex).
It is quickly absorbed, after 30 minutes it has a diuretic effect, and is used for swelling of the face and limbs, and for hypertension against the background of severe renal failure. - Piretanide
. It has a significant effect, much greater than that of Furosemide. It is used as an effective antihypertensive agent, calcium channel blocker, for edema, heart and kidney failure.
- Ethacrynic
acid (Uregit
). The diuretic effect is pronounced, the effect lasts from 2 to 6 hours. Used for swelling, has contraindications: anuria, oliguria, hepatic coma.
All representatives of diuretics remove potassium and other trace elements in an increased volume: magnesium, sodium, calcium, chlorine.
To compensate for the loss of valuable substances, Panagin, Asparkam, and potassium orotate are simultaneously prescribed.
Torasemide
This diuretic drug is one of the most effective today. "Torasemide" is prescribed for acute and chronic heart failure, as well as renal failure. The product can also be taken to prevent edema. The drug effectively reduces high blood pressure by quickly removing excess fluid and sodium salts. The effect occurs an hour after administration and lasts 12-18 hours. Patients note that the diuretic effect does not occur immediately, so in the first hour after taking the drug you do not have to limit your activity. "Torasemide" is inexpensive and works well to relieve swelling of the face. You can buy diuretic tablets with a prescription; there are some side effects.
Torasemide
Berezovsky Pharmaceutical Plant, Russia
Edema syndrome of various origins, incl.
for chronic heart failure, diseases of the liver, kidneys and lungs; - arterial hypertension. from 81
594
- Like
- Write a review
pharmachologic effect
Diuretics increase the volume of urine excreted by reducing the reabsorption (reabsorption) of water in the tubules or by increasing the filtration of primary urine in the capillaries of the nephron glomeruli - the structural and functional units of the kidneys.
In addition, diuretic drugs have a decongestant effect and also reduce blood pressure, intracranial pressure, and intraocular pressure.
Diuretics of plant origin additionally have anti-inflammatory and antimicrobial effects.
Triampur compositum
This diuretic does not have a very pronounced effect and does not remove potassium from the body, only water, salts and toxins. That is why Triampur compositum is considered the safest diuretic drug, which is prescribed for edema due to chronic heart failure and liver problems. Triampur begins to act 15 minutes after administration, and the effect lasts about 12 hours. Doctors say that this diuretic is safe for relieving facial swelling, is quickly absorbed into the gastrointestinal tract, and has a gentle effect.
Triampur compositum
AVD.pharma, Croatia
-arterial hypertension;
—edematous syndrome of various origins (with chronic heart failure, nephrotic syndrome, liver cirrhosis). from 256
432
- Like
- Write a review
Diuretics in products
For those who need to take diuretics, there is the option of using natural diuretics. This is the use of diuretic herbal preparations, products that can remove excess fluid from the body, and the use of a diet with a minimum amount of table salt in the diet.
Such measures are applicable to the treatment of practically healthy people whose edema is associated with excessive consumption of salty foods, overwork, and poor diet.
Herbs with diuretic effect:
- Pharmaceutical camomile,
- Chicory,
- Birch buds and leaves,
- Dill greens,
- Horsetail,
- Bird's knotweed,
- Juniper,
- Lingonberry leaf,
- Burdock leaves and roots,
- Rosehip roots and berries,
- Bearberry,
- Flax seed;
- Parsley root.
These plants can be used alone or as part of herbal teas.
Selection of diuretic plants depending on symptoms:
Products with a diuretic effect:
- Watermelon,
- Melon,
- A pineapple,
- cucumbers,
- Cranberry,
- Dill, parsley, celery.
A product such as baked potatoes has a dual effect: it is a source of potassium and has diuretic properties. To lose weight, use a three-day diet based on it, during which a kilogram of baked potatoes is consumed throughout the day, washed down with water. In 3 days you can get rid of 2.5-3 kg of excess weight and swelling.
Diuver
Modern diuretic tablets from the group of loop diuretics. The active ingredient of the drug, turasemide, copes well with edema of various natures. “Diuver” has the mildest, prolonged action; the effect after administration occurs within 3-4 hours. Although it is not a potassium-sparing diuretic, it removes much less potassium than other diuretics. Diuver is prescribed for diseases of the kidneys, liver, lungs and heart failure. You can buy Diuver with a prescription (by the way, it is not cheap), be sure to familiarize yourself with the contraindications and side effects.
Diuver
JSC "Biolek", Ukraine
- edematous syndrome of various origins, incl.
for chronic heart failure, diseases of the liver, kidneys and lungs; - arterial hypertension. from 236
677
- Like
- Write a review
Natural Diuretics
Photos from open sources
History of the origin of diuretics
Over the years, scientists have tried to discover organic and inorganic substances to treat edema. In the early 16th century, weak diuretics were used. Such as sea onion and calomel. In the 20s of the last century, people began to use mercury-containing substances to reduce swelling.
In 1950, the first taizide diuretics, chlorothiazide and hydrochlorothiazide, were synthesized. They are close in chemical structure to sulfonamides. In 1960, the structure of substances was modified. More effective loop diuretics, furosemide and ethacrynic acid, have been created. Diuretics with antikaliuretic activity have been synthesized. The drugs began to be widely used in medicine to treat diseases.
Dog-rose fruit
In addition to medicinal diuretics, herbal drugs have a mild diuretic effect. Firstly, it is rosehip. In addition to being a diuretic, it is famous for its general strengthening effect, helping the body resist various infections (also for urinary tract diseases). Rosehip improves the functioning of the digestive and cardiovascular systems. The value of rosehip is that it contains a lot of useful vitamins. Rose hips relieve swelling, reduce cholesterol levels, normalize blood clotting, and help cells recover faster.
Rosehip fruits
OJSC Krasnogorskleksredstva, Russia
For the prevention of hypovitaminosis C and R. In the complex therapy of acute and chronic infectious diseases, asthenic conditions, during the period of recovery after serious illnesses, surgical operations
from 28
418
- Like
- Write a review
Diuretic collection
Herbal infusions are very popular for the treatment of many diseases, including as a diuretic for edema. Diuretic collection in complex treatment helps cure urinary tract infections. Medicinal herbs in the diuretic collection act very gently, relieve spasms and inflammation. A diuretic preparation is often prescribed for cystitis; it is suitable for preventing relapses of this disease and is available in almost every pharmacy. Disadvantages include an unpleasant taste and green coloration of urine.
Diuretic collection
ST-Medipharm, Russia
Combined product of plant origin.
It has diuretic, anti-inflammatory, antiseptic, antispasmodic effects. from 76
5.0 1 review
485
- Like
- Write a review
Juniper fruits
Juniper helps with urinary tract infections by reducing inflammation and destroying germs. And thanks to the diuretic effect, pathogenic microflora is quickly eliminated from the body. Juniper fruits are also used as an appetite stimulant and to improve the functioning of the gastrointestinal tract. In addition, this herbal preparation stabilizes blood pressure and has a mild laxative effect. Contraindications include pregnancy, breastfeeding and childhood.
Juniper fruits
OJSC Krasnogorskleksredstva, Russia
In the complex treatment of edematous syndrome (with heart failure, insufficiency of kidney and/or liver function), cystitis
from 40
246
- Like
- Write a review