Diabetes insipidus
, otherwise referred to as diabetes, is a pathological process characterized by a violation of the reabsorption of fluid in the kidneys, as a result of which urine is not sufficiently concentrated and is therefore excreted in very large quantities in a diluted form. Against this background, patients develop a constant feeling of thirst, indicating significant loss of fluid in the body. If the loss of fluid by the body is not sufficiently compensated from the outside, then dehydration develops.
Diabetes insipidus develops as a result of a defect in the production of vasopressin, an antidiuretic hormone produced by the hypothalamus, or a decrease in the sensitivity of kidney tissue to its effects. Diabetes insipidus belongs to the group of rare endocrine pathologies, which in 20% of cases develops as a complication after brain surgery. According to medical statistics, the development of the disease is not related to the gender and age of patients, but is more often recorded in people 20-40 years old.
Classification of diabetes insipidus
Depending on the level at which the disorders occur, two types of diabetes insipidus are distinguished:
1. Central or hypothalamic diabetes insipidus
– occurs as a result of a violation of the formation or release of antidiuretic hormone.
It, in turn, is divided into idiopathic diabetes insipidus
, which is based on a hereditary pathology characterized by low production of antidiuretic hormone, and
symptomatic diabetes insipidus
, which can occur against the background of other diseases, for example, with injuries and tumor processes of the brain, infectious inflammation of the meninges and so on.
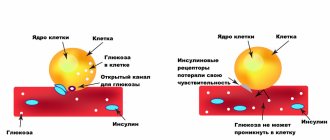
2. Nephrogenic or renal diabetes insipidus
– occurs due to impaired sensitivity of renal tissue to the effects of vasopressin. This type of diabetes insipidus is much less common. In this case, either an inferior structure of the nephrons or vasopressin resistance of the receptors of the renal tissue is noted. This type of diabetes insipidus can be congenital, or it can occur due to drug-induced damage to kidney cells.
A number of authors also highlight gestagenic diabetes insipidus in pregnant women
, the development of which is associated with increased activity of a special placental enzyme that destroys vasopressin.
Young children may develop functional diabetes insipidus
, which is associated with immaturity of the urine concentrating mechanism in the kidneys.
In addition, during the use of drugs from the group of diuretics, the development of iatrogenic diabetes insipidus
.
Endocrinologists also distinguish primary polydipsia
as one of the forms of diabetes insipidus, which manifests itself in the form of a pathological feeling of thirst (with damage or tumor processes of the thirst center in the hypothalamus) or a compulsive desire to drink (with neuroses, psychoses and schizophrenia). At the same time, due to increased fluid intake, the physiological production of vasopressin is suppressed and the clinical picture of diabetes insipidus develops.
Based on the clinical picture, diabetes insipidus is also classified according to severity without correction with medications:
— mild degree
the disease is characterized by daily urine output in the range of 6-8 liters;
- with average degree
pathology, the amount of urine excreted per day is 8-14 liters;
- for severe
The typical daily volume of urine excreted is more than 14 liters.
During the period when the disease is subject to correction with medications, three stages are distinguished in its course:
1. compensation stage
, which is characterized by the absence of symptoms of thirst and an increase in the volume of urine excreted;
2. subcompensatory stage
– with periodic occurrence of thirst and the presence of polyuria.
3. stage of decompensation
, which is characterized by a constant feeling of thirst and polyuria even during treatment.
Our doctors
Kolodko Inna Mikhailovna
Doctor - endocrinologist, doctor of the highest category
Experience 26 years
Make an appointment
Slovesnova Tatyana Alekseevna
Endocrinologist, Candidate of Medical Sciences, doctor of the highest category
Experience 48 years
Make an appointment
Mikhailova Elena Vladimirovna
Endocrinologist, diabetologist, candidate of medical sciences
Experience 46 years
Make an appointment
Diabetes insipidus - causes and mechanism of development
Central type diabetes insipidus
can develop as a result of congenital genetic defects and brain pathologies.
Acquired diabetes insipidus of the central type develops due to tumor processes in the brain, as well as metastases resulting from tumor damage to other organs, after injuries and infectious diseases affecting the brain. In addition, the disease can develop during ischemia and hypoxia of brain tissue as a result of vascular disorders. Idiopathic diabetes insipidus
occurs with the spontaneous appearance of antibodies to cells that produce antidiuretic hormone, while organic damage to the hypothalamus is not detected.
Nephrogenic diabetes insipidus
can also be congenital and acquired. Congenital forms of this type of diabetes insipidus develop with Wolfram syndrome and genetic defects in receptors that respond to vasopressin. Acquired forms of renal diabetes insipidus can develop with chronic renal failure, renal amyloidosis, disturbances in the metabolic processes of calcium and potassium in the body, and poisoning with drugs containing lithium.
Symptoms of diabetes insipidus
The two most telling symptoms of diabetes insipidus are polyuria
(excretion of urine exceeding the daily norm) and
polydipsia
(drinking large quantities of fluid). The volume of urine excreted per day in patients with diabetes insipidus can vary in the range of 4-30 liters, depending on the severity of the disease. At the same time, urine is practically colorless, has low density and practically does not contain salt and other components. Due to an irresistible feeling of thirst, patients suffering from diabetes insipidus consume a lot of liquid. The amount of fluid consumed by patients can range from 3 to 18 liters per day. Both one and the second signs entail sleep disturbances, neuroses, increased fatigue, and emotional imbalance.
Diabetes insipidus in children
It is most often manifested by bedwetting, which is subsequently accompanied by delayed growth and puberty. Over time, structural changes occur in the organs of the urinary system, manifested in the form of expansion of the renal pelvis, ureters and bladder. Due to the consumption of significant volumes of liquid, the stomach also suffers, since its walls, as well as surrounding tissues, are overstretched, which leads to prolapse of the stomach, dysfunction of the biliary tract and chronic irritable bowel syndrome.
When examining patients with diabetes insipidus, excessive dryness of the skin and mucous membranes is revealed. Patients complain of poor appetite, sudden weight loss, headaches, vomiting, and hypotension. One of the symptoms of diabetes insipidus in women is menstrual irregularity. Diabetes insipidus in men is characterized by decreased sexual function.
The danger of diabetes insipidus is the possibility of developing dehydration, which can result in permanent neurological disorders. A similar complication occurs if the liquid. lost in urine is not adequately replenished from the outside.
Treatment of central nervous system disorder
All patients diagnosed with CDI are prescribed desmopressin, a synthetic analogue of vasopressin [9]. The drug lacks vasoconstrictor activity and has a more pronounced and long-lasting antidiuretic effect [16]. Currently, 2 forms of desmopressin are used in Russia: a tablet form (Minirin) and an intranasal spray (Presaynex). For CND, the average therapeutic doses of tableted desmopressin vary from 0.1 mg to 1.6 mg/day, the frequency of administration is 2–3 times a day. When administered intranasally, the dose ranges from 10 to 40 mcg per day, which is due to individual sensitivity to the drug; frequency of administration – 2 times a day [7, 13].
When taking the tablet form, the antidiuretic effect is observed after 1–2 hours. Intranasal administration provides a faster onset of action after 15–30 minutes, since the administration of the drug is not associated with food intake, which ensures greater bioavailability. For colds or allergic diseases, it is possible to administer the drug sublingually in doses 1.5–2.0 times higher than the dose for intranasal administration [15].
Based on what criteria is the diagnosis of diabetes insipidus made?
Making a diagnosis in the typical course of diabetes insipidus is quite simple. It is based on a history of unquenchable thirst and an increased volume of daily urine, exceeding 3 liters per day. In laboratory tests, important criteria are hyperosmolarity of blood plasma and increased levels of sodium and calcium with a reduced level of potassium. When examining urine, its hyperosmolarity and low density are also revealed.
The first stage of diagnosing diabetes insipidus is aimed at confirming the very fact of the presence of polyuria (increased amount of urine) with low density. Typically, with diabetes insipidus, urine output exceeds 40 ml per kilogram of body weight with a relative density of urine less than 1005 g/l. If such urine output is established, the second stage of diagnosis is carried out, which consists of performing a test with dry eating. The dry-eating test in the classic version according to Robertson involves a refusal to take liquids (complete) and (preferably) a refusal to eat in the first 8 hours of the test. Before starting fluid and food restriction, the patient's blood and urine osmolality, blood sodium levels, urine output, body weight, and blood pressure levels are determined. After stopping the patient's food and water supply, this set of tests must be repeated every 1-2 hours, depending on how the patient feels. The test is completed if during the test the patient has lost more than 3-5% of his weight, the patient’s condition worsens, the level of sodium and blood osmolality increases, and urine with an osmolality of more than 300 mOsm/L is received. In patients with a stable condition, such a test can be carried out on an outpatient basis, and the patient must not drink for as long as he can withstand according to his health. If, during fluid restriction, a urine sample is obtained that has an osmolality of 650 mOsm/L, the diagnosis of diabetes insipidus can be excluded.
Carrying out a dry food test in patients suffering from diabetes insipidus does not lead to a significant increase in urine osmolality and the concentration of substances in it. During the test, patients with diabetes insipidus experience nausea and vomiting, convulsions, agitation, and headaches due to dehydration that develops due to loss of fluid. The temperature may rise.
When the diagnosis of diabetes insipidus is confirmed, a desmopressin test is performed - the administration of despopressin in patients with central diabetes insipidus causes a decrease in the amount of urine, but in patients with renal diabetes insipidus the volume of urine does not decrease.
For differential diagnosis with diabetes mellitus, the level of glucose in blood taken on an empty stomach is determined. To clarify the cause of the development of diabetes insipidus, an x-ray and an examination by an ophthalmologist and neuropsychiatrist are performed. If space-occupying lesions in the brain are suspected, magnetic resonance imaging is performed. The renal form of diabetes insipidus is diagnosed by ultrasound and computed tomography of the kidneys. If in doubt, consult a nephrologist and perform a kidney biopsy.
Diagnosis of the disease
Diagnosis begins with a study of the properties of urine: daily amount, relative density and osmolarity, which is used to judge the concentration function of the kidneys. Other necessary studies, without which a complete diagnosis is impossible:
- blood potassium and calcium levels;
- fasting blood glucose;
- blood ADH;
- Ultrasound and kidneys;
- kidney biopsy (if indicated);
- fundus examination;
- MRI of the brain.
Your doctor may order other tests if any organ failure is suspected. It is advisable to conduct a psychoneurological examination in children, since their congenital disorders are often combined with pathology in this area.
To clarify the diagnosis, dry eating may be prescribed for 10 or 12 hours. If a person is sick, then during this time body weight can decrease by 5% due to fluid loss.
How to treat diabetes insipidus?
After making a diagnosis and establishing the form of diabetes insipidus, treatment begins with eliminating the cause that caused it, i.e. remove tumors, eliminate the consequences of traumatic brain injuries, treat underlying diseases, etc.
For antidiuretic hormone replacement in all forms of diabetes insipidus
Its synthetic analogue, desmopressin, is prescribed, which is administered orally by instillation into the nose.
Central diabetes insipidus
involves the use of chlorpropamide, carbamazepine and other drugs that stimulate the production of vasopressin.
An integral part of therapy are measures to normalize the water-salt balance, which include the infusion of large volumes of saline solutions. To reduce urine output, hypothiazide is prescribed.
Diet for diabetes insipidus
involves reducing the load on the kidneys, therefore it includes foods containing a minimum of protein and a sufficient amount of fats and carbohydrates. For patients with diabetes insipidus, frequent split meals are recommended, including a lot of vegetables and fruits. To quench your thirst, it is preferable to use juices, compotes, and fruit drinks instead of water.
Idiopathic form of diabetes insipidus
does not pose a threat to life, but cases of complete recovery are extremely rare.
Gestational and iatrogenic diabetes insipidus
are more transient in nature and most often result in complete recovery.
Proper use of replacement therapy allows patients to maintain their ability to work. One of the most unfavorable prognostic forms of diabetes insipidus is renal diabetes insipidus in children
.
Experience in managing patients with CND
Patients with CND are under observation at the Endocrinological Dispensary of the Moscow Department of Health. 67 patients were transferred from the tablet form of desmopressin to the intranasal spray: 42 women and 26 men aged from 20 to 82 years.
During the translation, it was taken into account that taking 0.2 mg of the tablet form of desmopressin is equivalent to 10 μg of desmopressin administered intranasally.
In the vast majority of patients, the dose of oral desmopressin ranged from 0.2 to 0.6 mg/day (Fig. 1). When switching to intranasal spray, the average therapeutic doses of desmopressin ranged from 10 to 30 mcg/day. In patients receiving tableted desmopressin at a dose of 1.0 to 1.8 g per day, the dosage frequency was 8 times; when switching to the intranasal form of the drug, disease compensation was achieved at a dose of 60 to 80 mcg/day with a dosage frequency of 2 times in a day. The dosage range of intranasal desmopressin is presented in Fig. 2. No significant side effects were noted while taking the intranasal form of the drug.