Synovitis of the knee joint, what is it and how to treat?
Synovitis is an inflammation of the synovial membranes that line the inside of one or more large joints. During illness, fluid accumulates in the synovial membranes.
In 65–70% of cases, the knee joint is affected; the shoulder, elbow, ankle, and hip joints are much less often affected. The disease is widespread, has many variants of its course, and occurs equally often in children and adults of all age groups.
Most cases of synovitis, apart from pain, swelling and temporary impairment of motor activity of the affected joint, do not threaten anything else. But there are also its variants that can cause a severe infectious-purulent process, sepsis (blood poisoning) and permanent disability.
Causes
Inflammation of the synovial membrane can be provoked by:
- Injuries that result in constant irritation of the inner lining of the joint by pieces of cartilage or damaged meniscus.
- Infections that penetrate into the joint cavity from the external environment (in case of injury) or from neighboring tissues (in the presence of phlegmon, abscesses, wounds, abrasions, boils, etc.). Pathogenic microorganisms can also enter the joint from distant foci of infection via lymph or blood flow.
- Congenital and acquired pathologies of the joint and periarticular tissues. They lead to the development of synovitis for various reasons. For example, with rheumatoid polyarthritis or rheumatism, the disease develops under the influence of antibodies that affect the synovial membrane, and with arthrosis - due to irritation of this membrane by cartilage, which has lost its smooth surface, or bone growths.
- Autoimmune diseases (lupus erythematosus, rheumatoid arthritis). The immune system perceives the inner lining of the joint as a foreign agent, and antibodies begin to gradually destroy it.
- Metabolic disease. This cause causes synovitis, because metabolic products accumulate in the joint cavity, irritating the membrane.
- Allergic reactions. When allergens penetrate into the joint capsule, they are perceived as dangerous antigens, and the immune system begins to produce antibodies, resulting in inflammation, accompanied by excessive formation of synovial fluid.
- Endocrine diseases. Hormonal disruptions lead to the fact that synovial fluid begins to be produced in large quantities. Because of this, inflammation of the inner lining of the joint develops.
- Hemophilia. With this disease, constant hemorrhages occur in the joint cavity, which causes inflammation.
- Diseases of the nervous system. This is caused by severe stress, pinched or damaged nerves due to scoliosis, neoplasms or fractures, as well as neuritis of peripheral nerves.
There are 2 stages observed during the course of the disease:
- Spicy. Symptoms progress progressively: swelling, pain, and redness intensify during the first few days.
- Chronic (recurrent). Observed in the absence of adequate and timely treatment of the disease; The main symptom of chronic synovitis is dropsy and periodic mild pain.
Causes and types of disease
Doctors distinguish two main types of synovitis: infectious, which occurs due to the penetration of pathogenic microbes into the joint, and aseptic. The latter also comes in several types:
- exudative, developing as a result of a blow or injury to the knee joint;
- post-traumatic, caused by damage or rupture of the meniscus, bone fractures;
- reactive - an allergic reaction to certain irritants. It can also occur against the background of arthrosis and arthritis;
- chronic synovitis occurs due to incomplete cure of other types. Rarely seen.
Acute symptoms
Acute synovitis of the knee joints can be accompanied by severe pain. Therefore, if you suspect an infectious form of the disease, it is extremely important to consult a doctor as soon as possible, who will identify the causative agent of the infection and prescribe the necessary therapy.
Symptoms that accompany the acute purulent form:
- the joint is increased in volume;
- increased body temperature;
- general condition is characterized by weakness and nausea;
- there is pain when flexing and extending the leg;
- there is redness in the knee area, which turns out to be hot on palpation.
The disease is especially acute with a pyogenic infection. Pathogenic bacteria often penetrate into the joint cavity along with the bloodstream or through open wounds. Accumulated blood, pus and joint fluid cause stretching of the joint capsule, which causes pain.
Types of synovitis
There are acute and chronic forms of the inflammatory process. Usually, after the first manifestation of synovitis, the patient experiences relapses in the future - the disease becomes chronic. Synovitis can affect any joint, so the following classification exists:
- Moderate inflammation of the elbow joint. The disease can manifest itself in severe form, but this happens infrequently. The disease is classified as an occupational disease of mechanics and people involved in sports. Patients experience serious discomfort up to intense pain, not only during the process of moving, but also in conditions of complete rest.
- Synovitis of the shoulder joint. Occurs due to carrying heavy objects and injury to the shoulder or forearm. Among the signs, only pain can be identified, since the swelling itself appears only during the acute course of the disease.
- Synovitis of the knee joint. One of the symptoms of the disease is joint instability. You can check everything in a couple of minutes - you need to straighten your knee in a sitting position and press on the kneecap, which should return to its place after displacement. Treatment of the acute phase is performed only in inpatient settings. Only in a hospital can you quickly restore the condition of the joint and avoid the acute phase.
- Inflammation of the hip joint is considered a rare pathology among adults. Typically, this form of the disease occurs in children between 4 and 8 years of age. It is worth highlighting that in childhood, synovitis can occur without an obvious reason. Sometimes, in addition to injury, the cause of the inflammatory process is a viral infection. Synovitis of the hip joint leads to pain when moving. The diseased joint swells, and there is also some stiffness in movement. Synovitis appears spontaneously, patients complain of pain in the legs. Further pain is localized near the hip joint. In childhood, this disease can lead to temporary lameness.
- Synovitis of the ankle joint is in many ways similar to other types of disease. The ankle swells, the skin over its surface becomes hot to the touch and becomes covered with red spots. Pain can occur not only when moving, but also at rest. This is due to the fact that the synovial membrane is considered sensitive. Also, with minimal load on the ankle, rapid fatigue occurs. Usually the cause of inflammation of the ankle joint is injury. A subluxation or direct blow to the ankle usually leads to microtrauma of the synovium and the development of synovitis.
- Synovitis of the foot joints. Basically, the inflammatory process of the synovial membrane begins in the metatarsophalangeal joint of the big toe (it is this joint that is most susceptible to deformation). Sometimes the inflammation also spreads to the long extensor tendon of the toes (tendinitis). Often this localization of synovitis indicates serious stress on the feet. Dancers, gymnasts and ballerinas are at risk. This type of synovitis is characterized by an increase in the size of the joint, redness of the skin around it, and pain when moving. If symptoms of the disease reappear, in some cases degenerative changes in the diseased joint (arthrosis) are possible. Most often, within three weeks the inflammation goes away, and the functionality of the joint is completely restored.
There is also villonodular and suprapatellar synovitis, but these types are rarely observed in patients, they do not have characteristic symptoms and can only be diagnosed by specialists. Diagnosis of any type of synovitis is carried out using a comprehensive examination.
Signs of a non-infectious form of the disease
The main symptoms of an aseptic type of disease are an increase in the volume of the knee joint and the absence of pain. This phenomenon is caused by the fact that the synovial fluid, located in the joint capsule when the synovial membrane is irritated, sharply increases in quantity in just a few hours. The resulting swelling in the knee joint prevents free movement.
Symptoms of the aseptic type have the following form:
- an increase in volume occurs from several hours to 1-2 days;
- the affected area does not have a high temperature;
- when pressing on the patella bone, it sinks into the joint, after which it floats up again;
- general weakness.
Why is synovitis dangerous?
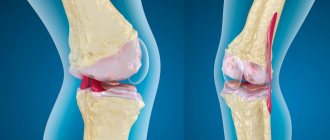
The synovial membrane performs an important function in the joint - it ensures the separation of hard tissues. Due to this, the joint moves with minimal bending of the components. The membrane is capable of changing shape, thereby adapting to supporting surfaces and providing shock absorption. The quality and quantity of synovial fluid in the joint depends on its condition, the same fluid whose deficiency develops coxarthrosis or gonarthrosis.
The connective tissue that forms this membrane can become inflamed. Swelling forms in the joint, during movement the person feels pain, and bleeding is possible. If the disease is not treated, the synovial membrane thickens and new blood vessels appear in it. In the future, this will lead to frequent joint bleeding.
Synovitis without treatment can lead to joint dysfunction
Signs of chronic form
Chronic synovitis is the result of undertreatment of the acute form of the pathology and is characterized by dull symptoms. Painful manifestations cause minor concern to the patient. The knee has slight swelling, no redness, and mild pain when bending and walking.
The chronic form of synovitis can be recognized by the following signs:
- The joint often crunches, and regular microdislocations are observed.
- Long walks are impossible, as there is increased fatigue in the legs.
- The joint has limited mobility.
In the chronic form, there are no symptoms such as fever or fever. Untreated rheumatism, allergic reactions, and gout can lead to inflammation.
Every year, the accumulation of effusion inside the knee joint gradually accelerates the development of the inflammatory process. The patient develops signs of hydrarthrosis (dropsy) and pathological changes are observed in the ligamentous apparatus itself.
Diagnosis and treatment
During the initial examination, the doctor checks the condition of the joint visually: notes the presence of pain, changes in skin color, difficulties with movement, and an increase in local temperature. MRI or ultrasound can help determine the amount of accumulated fluid. If there is tissue damage in the joint, an x-ray will show it.
To determine the root cause of the inflammatory process, the following is prescribed:
- a blood test to determine the bacterial infection that triggered the inflammation;
- analysis of synovial fluid.
Self-medication of synovitis, especially warm compresses, can lead to dangerous complications
Diagnostics
The program for diagnosing synovitis of the knee joint is accompanied by:
- Carrying out CT, MRI, ultrasound of the knee joint, radiography.
- Puncture and biopsy - in severe cases.
- Careful collection of medical history data, on the basis of which it is possible to confirm or refute a number of diseases.
- Professional examination by a specialist - palpation, general examination, accompanied by tests.
- Conducting studies, OBC and urine, examination of synovial fluid.
Making a diagnosis - synovitis of the knee joint, with proper treatment, in principle, we will win. However, you need to know that complete recovery can only occur with serous and allergic synovitis. After suffering from other types of synovitis, as a rule, stiffness of the joints remains; with purulent formations, unfortunately, sepsis develops.
Diagnostic measures
In order to obtain the most accurate diagnosis, when the first signs of an inflammatory process appear, it is recommended to immediately seek professional medical help.
The key diagnostic method is puncture (extraction of a small amount of joint fluid for the purpose of research). The most informative is bacteriological or bacterioscopic analysis of the extracted material.
The type of pathogenic microflora present is determined. It is mandatory to analyze the resistance of identified bacteria to antibacterial agents.
In addition, at the diagnostic stage, instrumental methods are also important, which include:
- arthroscopy;
- arthropneumography;
- CT/MRI.
If there are symptoms suggesting benign or malignant neoplasms, patients are prescribed a biopsy of the affected membrane.
Based on the results obtained, the severity of a particular clinical case is determined, which helps to outline ways to resolve it.
General principles of treatment of synovitis
Treatment of the knee joint is prescribed after a complete examination and diagnosis. The method of therapy depends on the type of inflammation, the stage of development of synovitis of the knee joint and the individual characteristics of the body.
Most often, an integrated approach is used, which implies:
- puncture;
- immobilization of the damaged joint;
- taking medications;
- physiotherapy;
- use of traditional medicine.
If conservative methods of treating synovitis of the knee joint do not bring the desired result, surgical intervention is used.
Diagnostic methods
To identify the cause of the pathology and make an accurate diagnosis, it is necessary to conduct a comprehensive diagnosis. After collecting anamnesis and systematizing the data obtained about the patient’s complaints and previous diseases, a visual examination is carried out. In this case, the injured knee is palpated, the gait and the patient’s ability to straighten the joint are analyzed. The patient is asked to do:
- Puncture.
In this case, the surgeon numbs the pain, and then pierces the joint cavity with a thin needle, collecting the synovium. In laboratory analysis, attention is paid to the color, transparency and viscosity of the liquid. Next, it is subjected to microscopic and cytological examination to determine the cause of inflammation. The results obtained make it possible to choose the right treatment tactics. - MRI.
Using this method, you can see the structure of the synovial membrane. If there is liquid, the device allows you to estimate its quantity. Thanks to MRI, the specialist will receive a detailed description of the functionality of the joint, as well as information about the condition of the surrounding tissues, blood vessels, and nerve fibers. - Ultrasound.
Used to visualize changes in the thickness of the inflamed synovium. This is one of the signs of synovitis activity. At the same time, it is possible to examine in detail the structure of soft tissues and detect the pathological process at an early stage. - Arthroscopy.
This therapeutic and diagnostic procedure makes it possible to examine the affected joint, differentiate the nature of the lesion, and also study the relief of the synovial membrane along its entire length.
Based on these data, the specialist determines the diagnosis, clarifies the form and degree of development of the disease, and prescribes treatment.
Treatment of acute traumatic synovitis
The treatment regimen for this form of synovitis can be divided into the following points:
1) Treatment of injury - if it is an open fracture, the surgeon restores the normal position of the bones inside the joint, sutures the damaged ligaments and areas of the capsule (if there are damages) and sutures the skin over the wound.
2) For open and closed intra-articular fractures, the patient is subjected to “skeletal traction” - wires are pulled through the bones that form the joint and a weight is suspended to avoid their re-displacement. Typically, the patient should remain in this condition for up to 3 weeks, unless surgery has been previously scheduled.
3) If symptoms of synovitis occur at any time, the patient is prescribed:
- Non-hormonal anti-inflammatory drugs (NSAIDs) intramuscularly or in tablet form. Most often used: Diclofenac, Ketorolac (Ketoprofen, Ketorol), Ibuprofen, Nimesulide (Nise).
- To eliminate side effects in the form of stomach and duodenal ulcers, “proton pump inhibitors” are prescribed - Rabeprazole, Omerpazole, etc.
- If there is significant swelling in the knee area or examination methods reveal a large amount of fluid inside the joint, the patient is punctured and the excess volume is removed.
- During the period of “skeletal traction,” the patient is sent to undergo physiotherapeutic procedures (photo- or magnetic therapy), which promote tissue healing. They also produce an anti-inflammatory effect, which reduces the severity of synovitis.
4) After removing the pins, the damaged leg is cast for at least 6-8 weeks. During this period, synovitis is quite rare. And even if it occurs, it can only be detected by removing the plaster cast. Treat according to the above scheme.
Prevention of synovitis
To prevent a relapse, you must not forget about preventive measures. Prevention is a set of rules and measures that will help maintain the health of your lower extremities.
When playing sports, do not forget to be careful, this will help protect your knee from injury. Also, special attention should be paid to the choice of shoes, not only those in which you train, but also everyday ones. Having the right shoe collection will protect you from future injuries. Professional athletes should fix the articular surfaces with special pads or bandages. Contact us if you have severe or moderate synovitis, we will help. We employ qualified specialists. Prices can be found in the price list on the website or by calling +7,).
Treatment of acute infectious synovitis
In this form, inside the joint, in addition to excess fluid, there is pus and bacteria, which gradually destroy cartilage, ligaments and capsule. Therefore, it is important to perform a puncture of the knee joint in a timely manner with the introduction of disinfecting solutions.
After puncture, antibacterial drugs and NSAIDs are prescribed. Anti-inflammatory therapy is carried out similarly to that for acute traumatic synovitis. Antibiotics are prescribed penicillin or macrolides. They have the best effect with minimal side effects. The following drugs are indicated:
Macrolides:
- Erythromycin;
- Azithromycin;
- Josamycin (recommended for children or pregnant women).
Penicillins:
- Amoxicillin;
- Ampicillin;
- Amoxiclav (if the above medications are ineffective or the patient has recently taken antibiotics).
Physiotherapeutic procedures are contraindicated in infectious processes, because they contribute to an increase in the number of bacteria. Therefore, this treatment method is not used for infectious synovitis.
Symptoms
The signs of the disease, regardless of its origin, are the same. True, they can appear at different time intervals. Symptoms characteristic of synovitis are:
- increased fatigue under loads that a person could previously easily cope with;
- feeling of discomfort in the problem area;
- pain localized in the ankle area, which can affect surrounding tissues with severe swelling;
- redness and swelling of the area involved in the pathological process;
- an increase in temperature and the appearance of symptoms of general intoxication (with an infectious form) are possible.
The severity of symptoms depends on the stage of the disease. The first alarm bell is always pain, which initially appears only when performing rotational movements. Gradually, the pain increases so much that it accompanies the patient even at rest, disrupting sleep and normal functioning in general.
How to treat rheumatoid and psoriatic synovitis
This synovitis develops against the background of rheumatoid arthritis. Therefore, in order to eliminate its symptoms, it is necessary to treat the underlying disease. Therapy should be carried out comprehensively and include the following elements:
- Chondroprotective agents are used to preserve the tissues of the knee joint. An effective and inexpensive drug in this group is Chondroitin.
- Anti-inflammatory treatment - if there is a good effect from NSAIDs, you can limit yourself to regular use of these drugs in combination with Omeprazole. If it is ineffective, the doctor prescribes hormones (Prednisolone, Hydrocortisone, etc.), calculating the dose individually.
- Reducing the load on the affected joint also reduces pain. The knee joint can be unloaded by recommending that the patient use a cane when walking.
- Physiotherapy is pain-relieving procedures aimed at the affected area. The use of any techniques is allowed: UHF therapy, photo and magnetic therapy, galvanization.
Treatment should be carried out by a rheumatologist. It is not recommended to independently treat this form of synovitis.
Causes
Damage to the synovial membrane by the inflammatory process is a problem that not all people face during their lives. Doctors identify a number of factors that contribute to the development of the disease.
Injuries
Among the main reasons for the development of the disease are traumatization. Most often, synovitis is caused by sprains and ruptures of ligaments, and fractures in the ankle joint.
Birth defects
Often in the practice of an orthopedic traumatologist there are congenital defects that contribute to the development of the disease. This could be, for example, hallux valgus or flat feet. In this case, the load is distributed incorrectly, which leads to inflammation.
Diseases
Osteochondropathy of the talus. As a result, the articular surfaces are deformed, and a free osteochondral articular fragment may form. The above factors cause synovitis.
Shoes
Incorrectly chosen shoes can contribute to the development of symptoms of synovitis. For this reason, the disease affects women who are forced to wear high-heeled shoes, due to which the load on the ankle joint is very high.
High physical activity
Another important factor is intense physical activity. The joint does not have an infinite reserve of strength, and sooner or later its functionality begins to decline, which leads to the appearance of unpleasant symptoms.
Treatment of gouty synovitis
With gout, synovitis very often occurs due to the deposition of uric acid salts into the joint cavity, irritation of the capsule and inflammation of the synovial membrane. The most effective treatment method is to follow a diet that includes:
- limit tea, coffee;
- exclude legumes, mushrooms, beets and “greens” (onions, parsley, sorrel, lettuce, etc.);
- exclude meat and fish products;
- exclude alcohol;
- include mineral waters (Narzan, Yesentuki) in the diet.
Drug therapy includes:
- NSAIDs during periods of exacerbations, if they are ineffective, take hormones (Hydrocortisone or Prednisolone).
- Colchicine is a drug intended to relieve seizures.
- Constant use of medications that remove uric acid from the body - Allopurinol or Benzbromanone.
It should be noted that the use of medications without diet is useless in the treatment of gouty synovitis.
Causes of synovitis
Synovitis is divided into two groups - aseptic and infectious. Aseptic factors include traumatic, neurogenic, allergic factors and endocrine disorders. Infectious synovitis can be caused by pathogenic microorganisms that cause specific (pathogens - tuberculous mycobacteria) and nonspecific (pathogens - staphylococci, streptococci, pneumococci) inflammatory processes in the area of the synovial membrane. Pathogens can enter it from the environment through the wound surface by contact, as well as by lymphogenous or hematogenous routes from the source of infection inside the body.
Therapy for villous nodular synovitis
This form of synovitis is, by its nature, a benign tumor. The most effective treatment option is removal of the formation. For this purpose, arthroscopic operations are currently performed:
- make two small incisions of 1-2 cm each;
- they are used to remove the tumor;
- After the procedure, the incisions are sutured;
- instruments are inserted into the joint. One of them is a camera with a flashlight, and the second is an electric knife or tweezers.
Complications after such manipulations occur very rarely. They do not require long hospitalization - on average, the patient stays in the hospital for 4-7 days.
Chronic synovitis in rheumatology. Assessment of activity and treatment tactics
About the article
62184
0
Regular issues of "RMZh" No. 8 dated April 29, 2005 p. 548
Category: General articles
Author: Olyunin Yu.A. 1 1 FGBNU NIIR im. V.A. Nasonova, Moscow, Russia
For quotation:
Olyunin Yu.A. Chronic synovitis in rheumatology. Assessment of activity and treatment tactics. RMJ. 2005;8:548.
Among the various manifestations of chronic joint diseases, synovitis occupies a leading place. The inflammatory process developing in the synovium determines the main features of the clinical picture and is the driving force behind the progression of the disease. It is the body’s response to a pathogenic stimulus, which is realized through the transformation of the synovium into a kind of immune defense organ. In this case, functionally active cells of inflammatory infiltrates are formed not due to the local proliferation of the initially present cellular elements, but as a result of the migration of the corresponding cells from the circulation.
This process leads to the formation of highly specialized cellular aggregates, the components of which actively interact with each other and produce aggressive products that cause tissue damage. The formation of inflammatory cell infiltrates is accompanied by proliferation of stromal elements and blood vessels of the synovium. Over time, the thin shell of the joint turns into a fairly powerful tissue mass. The structure and functional activity of such tissue varies in different diseases, in different patients suffering from the same disease, in different joints of the same patient, and even within the same joint. The most common types of chronic synovitis are primary inflammation of the synovium in chronic arthritis and secondary synovitis in patients with osteoarthritis (OA). According to modern concepts, the key link in the development of chronic arthritis is the recognition of an unknown pathogenic factor by the antigen-presenting cell [4]. The cell that recognizes the antigen processes it and presents it to the T lymphocyte, triggering the synthesis of proinflammatory cytokines that induce the migration of inflammatory cells into the joint and the proliferation of synovial vessels. The development of secondary synovitis in OA is associated with the accumulation of cartilage degradation products (fragments of proteoglycan and collagen molecules, chondrocyte membranes, etc.) in the joint [6]. Normally, cells of the immune system do not come into contact with these antigens and therefore recognize them as foreign material. This leads to the development of an immune response, accompanied by chronic inflammation of the synovium. The morphological picture of secondary synovitis as a whole is not fundamentally different from those changes that are observed in chronic arthritis. Active synovitis in patients with chronic arthritis is accompanied by the production of proteolytic enzymes that mediate joint destruction. Chronic synovitis in OA is itself the result of a destructive process. However, it, in turn, can aggravate joint destruction [1]. Therefore, suppression of the chronic inflammatory process, apparently, can slow down the progression of the disease not only in chronic inflammatory joint diseases, but also in OA. The basis for the treatment of inflammatory changes in the joints is systemic drug therapy. However, often systemic treatment does not adequately suppress local inflammatory activity and synovitis occurs as a relatively autonomous process, which is supported mainly by local mechanisms. In such cases, a favorable result can be achieved with the help of therapeutic measures aimed directly at the source of inflammation. At the same time, the tactics of therapeutic measures are largely determined by the activity of the inflammatory process. The main clinical signs of the activity of chronic inflammation of the synovial membrane are arthralgia and swelling of the affected joint. These symptoms are equally characteristic of both primary and secondary synovitis. The formation of pain syndrome in inflammatory and degenerative joint diseases can be associated with various mechanisms. But the main role among them is probably played by irritation of the nerve endings located in the joint under the influence of inflammatory mediators produced here. Joint pain is the leading symptom of the disease, and the functional limitations that develop in the patient are primarily associated with it. Currently, there are two main ways to record the intensity of pain. The simpler of them is the assessment of arthralgia in points, which usually provides 5 degrees of severity of the symptom (0 - no pain, 1 - mild, 2 - moderate, 3 - severe and 4 - very severe pain). It is somewhat more difficult to assess pain using a visual analogue scale (VAS), but this method provides more accurate results. VAS is a straight line 100 mm long. The zero point of the scale located on its left edge means no pain. The far right point corresponds to unbearable pain. Between these extreme positions, the patient must indicate the level corresponding to his pain sensations. It should be borne in mind that pain is a dynamic indicator, the severity of which varies depending on the time of day and the physical activity of the patient. Therefore, it is not the intensity of pain at the time of examination that should be recorded, but its maximum level over the past week. The exudative component of inflammation is not as noticeable for the patient as pain, but is of exceptional importance as an objective indicator of the activity of synovitis. The presence of exudate in the cavity of the affected joint is necessarily taken into account when determining treatment tactics and assessing the effectiveness of the therapy. When examining a patient, as a rule, one can quite reliably judge the presence or absence of exudate in those joints that are sufficiently accessible for visual and palpation examination (knees, wrist elbow joints, small joints of the hands and feet). It is quite difficult to detect moderate accumulation of exudate in the ankle and shoulder joints. It is not possible to detect fluid in the hip joints without the help of instrumental research methods. In order to reliably estimate the amount of exudate, it must be evacuated from the joint cavity. You can roughly assess the severity of the exudative component of arthritis by measuring the circumference of the inflamed joint. For short periods of observation, the dynamics of this indicator can be taken into account when assessing the effectiveness of treatment. However, in cases where the result is assessed at a sufficiently long term, a decrease in the circumference of the joint can occur due to atrophy of the muscles located in this area. Therefore, when examining a patient, qualitative registration of the presence or absence of exudate provides more reliable data than an attempt to quantify it. Additional information about the nature of changes in the affected joint can be obtained using instrumental research methods. The most common of these is radiography. However, a standard x-ray examination allows us to evaluate not the features of the development of synovitis, but its consequences. It makes it possible to determine, first of all, the degree of destruction of the joints, to record the presence of subluxation, aseptic necrosis of the bone or ankylosis of the joint. Ultrasound can be used to visualize the inflamed synovium itself. It allows you to obtain an image of a section of the joint under study, made in a certain plane. Using such a section, you can accurately measure the thickness of the synovial membrane, as well as approximately estimate the amount of synovial fluid in a given part of the joint. Ultrasound provides the ability to semiquantitatively assess exudative changes. The degree of accumulation of exudate in a certain part of the joint can be expressed in points and then the dynamics of this indicator can be monitored against the background of the treatment. The thickness of the synovial membrane, which can be recorded by ultrasound, is also one of the signs of synovitis activity. Its value is largely determined by inflammatory edema and decreases significantly as inflammation subsides. The use of arthroscopy (AS) allows direct visual examination of the inflamed synovium of the affected joint. Unlike ultrasound, AS does not allow one to accurately measure the thickness of the inflamed synovium and assess the severity of exudative changes in a given part of the joint. These two methods do not replace, but complement each other. Arthroscopic examination of the joint makes it possible to study the relief of the synovium along its entire length. Depending on the duration of synovitis and the characteristics of its development in a given joint, changes in the synovial membrane can vary within a very wide range. Normal synovium in the form of a thin transparent film covers the joint capsule. The development of the inflammatory process is accompanied by its thickening, the appearance of hyperemia, proliferation of villi, and the formation of fibrin clots on its surface. AS allows for a differentiated assessment of the nature of joint damage in patients with a similar clinical picture of the disease. To record observed changes, several methods for their semi-quantitative assessment have been proposed. Zschabitz A. et al. assessed the morphological changes in the synovium identified in AS using an index, which was calculated according to 4 indicators: vascularization, hyperemia, swelling of the synovium and villi formation [10]. The severity of each indicator was determined in points from 0 to 3. This scheme allows you to record the severity of changes, but does not take into account their prevalence, so it is difficult to characterize the damage to the joint as a whole. Paus AC et al. tried to overcome this drawback [9]. They divided the joint into 5 regions (posterior, intercondylar, medial, lateral, suprapatellar). In each zone, the severity of the lesion was assessed in 4 degrees: 1 - no signs of synovitis, 2 - moderate hyperemia without villi formation, 3 - moderate hyperemia with moderate villi formation, 4 - moderate or severe hyperemia with massive villi formation. The overall index was the arithmetic average of the scores of the 5 specified areas. The American College of Rheumatology has proposed assessing the severity of hyperemia, thickening, and villous proliferation of the synovium using a visual analogue scale and simultaneously recording the extent of the lesion as a percentage of the total area of the synovium. It should be noted that one of the most significant parameters characterizing the development of chronic synovitis may be the degree of increase in the volume of the affected synovium, an indicator of which is the severity of its villous proliferation. As it progresses, the size of the inflammatory focus increases, which, on the one hand, leads to a change in the ratio between the amount of drug injected into the joint and the mass of the affected tissue, and on the other hand, it impairs the circulation of fluid in the joint and makes it difficult for the drug to enter the inflammatory zone. There are 4 degrees of proliferative changes in the synovial membrane of the knee joint. The first is thickening of the synovium without significant villous proliferation. The second can be defined as the appearance of focal accumulations of villi against the background of a thickened synovium. In the third degree, the villi cover most of the synovium of the lateral parts of the joint, leaving the upper part free. The fourth degree is characterized by diffuse villous proliferation, which covers all parts of the joint. Arthroscopic control could be of some interest for assessing the results of treatment of chronic arthritis. Judging by the data from publications that assessed the effectiveness of intra-articular injections of drugs (in particular, methotrexate and rifampicin), the most dynamic indicator is synovial hyperemia [8]. It clearly decreases with a decrease in clinical signs of inflammation. At the same time, the structure of the synovia is generally quite stable. When examining patients before and after radiosynovectomy, we also observed the disappearance of hyperemia with favorable clinical results. In addition, in some cases, areas of synovial sclerosis and fatty degeneration of synovial villi appeared. While clinical signs of active inflammation persisted, hyperemia of the synovial membrane persisted in all cases. The tactics of local treatment of chronic synovitis is determined by the activity of the local pathological process and the effectiveness of previous therapy. In the presence of pain syndrome that is not accompanied by significant exudative changes, both in chronic inflammatory diseases of the joints and in OA, in addition to systemic drug therapy, medications in the form of ointments or gels are usually prescribed. In many cases, a beneficial effect can be achieved by prescribing locally irritating drugs that reduce the severity of pain due to a distracting effect. For this purpose, preparations based on menthol, turpentine, and camphor are used. The use of ointment and gel products containing nonsteroidal anti-inflammatory drugs (NSAIDs) ensures that these medications are delivered through the skin directly to the site of inflammation. For this purpose, medications containing such powerful agents as indomethacin, diclofenac, ibuprofen, and piroxicam are widely used. They are usually used 3-4 times a day, squeezing 4-8 cm out of the tube, depending on the size of the affected joint. Often, the optimal effect can be achieved using combination drugs containing ingredients with different mechanisms of action. One such successful combination is Dicloran Plus. It contains three anti-inflammatory components (diclofenac, methyl salicylate, linseed oil) and menthol, which has a local irritant effect. Menthol has a so-called “cooling” effect - due to irritation of cold receptors. A number of drug studies have shown that “cooling” gels containing menthol have significant analgesic activity and help to shorten the period of swelling and dysfunction when compared with placebo. Diclofenac and methyl salicylate are among the classic NSAIDs that achieve their effect by inhibiting the activity of cyclooxygenases, leading to a decrease in the synthesis of prostaglandins, which reduces swelling and infiltration of inflamed tissues. At the moment, according to FDA (USA) experts, only drugs containing methyl salicylate, menthol and capsaicin can be considered undeniably effective as analgesics. A-linolenic acid, which is part of flaxseed oil, binds activated cyclooxygenases at the site of inflammation. In the presence of significant exudative manifestations of the inflammatory process, the method of choice is intra-articular injection of GC. It is also practiced for both inflammatory and degenerative joint changes. It should be noted, however, that secondary synovitis is generally more resistant to the action of hormones and clinical improvement is often not long-lasting. For injection into joints, microcrystalline suspensions of poorly soluble hormonal drugs are used, which can be deposited in the affected joint for up to 3 weeks. As a result of the gradual dissolution of hormonal compounds deposited in the joint, a constant supply of a sufficient amount of medicine directly to the site of inflammation is ensured. The effect of GCs introduced into the joint cavity is mediated by interaction with the corresponding receptors of cells infiltrating the synovium and participating in the development of synovitis. The effect of HA on joint tissue largely depends on the dose and frequency of administration. Frequent injections of high doses of hormones in the experiment contributed to the development of degenerative changes in articular cartilage. At the same time, sporadic intra-articular injections of these drugs may have a chondroprotective effect. Therefore, in clinical practice, the injection of HA into the same joint is allowed no more than 3–4 times a year. The number of injections into different joints is not particularly regulated. However, they should not be performed too often and regularly. Otherwise, local therapy will actually become an analogue of systemic hormonal treatment, since the drug is constantly absorbed from the joint cavity into the bloodstream and provides, in addition to local, a noticeable systemic effect. The anti-inflammatory effect of GCs introduced into the joint is usually quite pronounced. The duration of the improvement achieved can vary within very wide limits. It depends both on the properties of the drug and on the characteristics of the course of inflammation in each specific case. The effectiveness of the drug directly depends on the solubility of the microcrystalline suspension. Reduced solubility increases duration of action and increases effectiveness. Currently, triamcinolone compounds (hexacetonide and acetonide) have the most long-lasting effects [3]. The lack of effectiveness of intra-articular injections in many cases may be associated with relative resistance to the action of GCs due to the production of a large number of pro-inflammatory cytokines at the site of inflammation. To avoid the unwanted effects of inflammatory stimulants that accumulate in the joints during chronic synovitis, the exudate is removed before administering the drug. However, proliferative changes forming in the joint and fibrin clots often prevent the full evacuation of the synovial fluid. Therefore, in a number of cases, it is not possible to completely remove it with a joint puncture and the pro -inflammatory factors remaining in the joint cavity impede the effect of the drug. The almost complete removal of inflammatory exudate can be achieved when the joint washes with a large amount of fluid during the AC. This method provides sufficient fluid intake into all parts of the joint and free evacuation of the contents of the joint cavity. In most patients with chronic arthritis, the joint washing with AS already in itself ensures a significant decrease in inflammatory changes. However, this effect is usually unstable. Introduction after washing the Civil Code gives significantly more favorable results. The clinical improvement achieved with intra -articular administration of the Civil Code after the AC is longer in most patients than with traditional local steroid therapy. We evaluated the effect of pre -washing the joints with AC on 55 knee joints of patients with RA. In 27 of them, the Civil Code was introduced in the traditional way after removing the exudate. 28 Before the introduction of the Civil Code were washed at the AC. 3 and 6 months after treatment, the decrease in arthralgia in these patients was significantly more significant than in the control group. A significant decrease in pain in the knee joints is observed after AS and in patients of OA [5]. Moreover, in contrast to chronic arthritis, the introduction into the joint of the Civil Code after AS in patients of the OA is not required. This phenomenon was noted even more than 50 years ago and is due, apparently, by a decrease in inflammatory changes characteristic of this disease. Rinsing the knee joints with AS allows you to remove the bulk of cartilage detritus and crystals from them. The elimination of these stimulants of inflammation can lead to a decrease in synovitis activity and a decrease in the severity of pain. It is also possible that such treatment can reduce the production of enzymes involved in the development of joint cartilage destruction, thereby slowing down the progression of the disease. The clinical effect of the AC largely depends on the technical features of its implementation. Thus, the authors who studied the results of the AC when using various volumes of fluid for its conduct, note that washing the knee joints with 3 liters of liquid gave a more favorable effect than 250 ml. The amount of detrit, removed during the procedure, also correlates with the degree of reduction in the severity of pain syndrome [7]. The favorable effect observed in patients with the joints after washing the joints at the AC prompted some researchers to use a simplified rinse procedure using puncture needles for the treatment of this disease. The results of such treatment are evaluated ambiguously. According to some authors, this procedure is no less effective than washing the joints with AS and gives a longer clinical improvement than the intra -articular introduction of the Civil Code. Others believe that it does not differ significantly from placebo [2]. Probably, in patients of the OA, as in chronic arthritis, the effect of washing largely depends on its technical characteristics. AS allows you to achieve significantly more complete removal of cartilaginous detritus and crystals from the cavity of the affected joint than washing through puncture needles. Therefore, despite the greater technical complexity, this procedure seems more promising than a simplified washing option. Literature 1. Panasyuk E.Yu., Tsvetkova E.S., Olyunin Yu.A., Smirnov A.V. Arthroscopy in the diagnosis of gonarthrosis. Scientific and practical rheumatology 2000, No. 2, p. 12–17. 2. Bradyy JD, Heilman DK, Katz BP, GSELL P, WALLICK JE, Brandt KD. Tidal Irrigation As Treatment for Knee Osteoarthritis: A Sham - Controlled, Randomized, Double - Blinded Evaluation. Arthritis Rheum. 2002 Jan; 46 (1): 100–8. 3. Centeno LM, Moore Me Preferred Intraarticolar Corticosteroids and Associated Practice: A Survey of Members of the American College of Rheumatology 4. Choyi Ehs, Panayi Gs Cytokin E PathWays and Joint InflamMatio in Rheumatoid Arthritis. New England Journal of Medicine, 2001, 344, 12, 907–916 5. Edelson R, Burks RT, BloEbaum RD, Short - Term Effects of Knee Washout for OsteartHritis. Am J Sports Med 1995, 23 (3), 345–9 6. Ghosh P, Smith M. Osteoarthritis, Genetic and Molecular Mechanisms. Biogerontology, 2002, 3, 85–88 7. Kalunian KC, Moreland LW, Klashman DJ, Brion PH, Concoff Al, Myers S, Singh Rw, Seeger LL, Rich E, Skovron Ml. Visually - Guuided Irrigation in Patience with Early Knee Osteoarthritis: A Multicenter Randomized, Controlled Trial. Osteoarthritis Cartilage. 2000 nov; 8 (6): 412–8. 8. Lindblad S., Hedfors E., Malmborg As Rifamycin SV in Local Treatment of Synovitis - A Clinical, Arthroscopic and Pharmacolagical Evaluation. J. RHEUMATOL. 1985, 12, 5, 900–903 9. Paus Ac, Pahle Ja Arthroscopic EvalUration of the Synovial Lining Before and Inter Open Synovence of the Knee Joint In Patys with Chronic INFLAMATORY JOIN T Disease. Scand J. Rheumatol. 1990, V. 19, p. 193–201. 10. Zscchabitz A., Neurath M., Grevenstein J. et al. Correlative Histologic and Arthroscopic Evalving in Rheumatoid Knee Joints. SURG ENDOSC. 1992, V. 6, p. 277–282.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Treatment with folk remedies
This disorder can also be treated with folk remedies. But this should be done only after an accurate diagnosis has been made and the main course of treatment has been prescribed. Traditional methods of getting rid of this type of illness help well at the initial stage of the disease.
The following folk remedies are used to treat synovitis:
- lotions from herbal decoctions;
- rubbing the knee with tinctures;
- taking decoctions;
- ointments based on herbs and animal fats.
But you can begin to treat synovitis with folk remedies only as prescribed by a doctor. Even if all the symptoms indicate a disease, you should still not self-medicate. Such a disorder should only be treated by a specialist after a final diagnosis. Treatment will be most effective if you combine “grandmother’s” recipes with drug therapy.
Diagnosis of synovitis
Diagnosis of pathology should be based on the patient’s complaints, as well as on the research performed. To make a correct diagnosis, instrumental research methods are usually used. To confirm synovitis, the following diagnostic methods are prescribed:
- radiography of the joint;
- Ultrasound of the joint;
- joint puncture;
- arthroscopy;
- CT;
- MRI.
Surgery
If drug treatment is ineffective, arthroscopy is performed to obtain more complete information about the pathology - a surgical procedure with minimal intervention in the body. Using an arthroscope, the doctor clarifies the condition of the tissues of the joint capsule and specifies the diagnosis (excluding or confirming other diseases: gouty arthritis, arthrosis deformans and others). If necessary, a biopsy of the altered synovial tissue is performed.
Arthroscopy can also be used to treat synovitis: after treating the joint cavity with medications from the inside, the swelling decreases, and then it is possible to use conventional medications.
Chronic synovitis of the knee joint with frequent relapses and persistent symptoms, as well as pronounced changes in the synovial membrane (with tumor-like growths) are indications for synovectomy (complete or partial removal of the changed tissue). In the postoperative period, antibiotics and analgesics and physiotherapy are prescribed (from the first day). The joint is kept immobile for a week, but walking is allowed from the second day after surgery.
Stages of patient examination when diagnosing “synovitis of the knee joint”
| History taking | Systematization of information about the patient’s past illnesses, reactions to medications, allergies, habits, stress, complaints and symptoms |
| Visual inspection |
|
| Laboratory diagnostics |
|
| Tomographic, X-ray or ultrasound examination | It is prescribed to obtain additional information about the condition of the knee joint, including the degree of deformation. |
MRI image shows synovitis of the knee joint
Exercise therapy
After arthroscopy, joint surgery or conservative treatment, it is recommended to perform a set of exercises to quickly restore the functions of the limb (start exercises within the time frame indicated by the doctor):
- Lie on your back, then perform partial flexion and extension of the knee (10 times).
- While lying down, squeeze any flat object up to 10 cm thick under the knee (10 times).
- In any position, strain the muscles of the thigh and lower leg (5-6 times).
- Lie on your back, slowly lift your straight leg 40 cm from the floor and lower it (10 times).
- Lie on the side opposite the side of the affected leg, then move the affected leg up (5 times).
- Sit on a chair and slightly lift the sore leg above the floor surface with a 1-kilogram load attached (5 times).
- Standing on the affected leg, half-squat and perform rotational movements with the other leg (1 minute).
After stabilizing the condition, it is recommended to walk for a distance of up to 500-600 m several times a week at a slow speed, as well as exercise on an exercise bike.
Depending on the stage of the disease, we choose one or more treatment methods in Moscow:
Therapeutic massage, osteopathy, manual therapy
Helps bones and joints take the correct physiological position, relieves pain and spasms, relaxes muscles.
Acupuncture in Moscow
Work on biologically active points. It affects the affected area and the body as a whole. Eliminates the cause of the disease and removes the symptoms.
In addition, according to indications, the following are used: taping, pharmacopuncture, FormTotix insoles, exercise therapy with an instructor and other methods. The choice of procedures depends on the current condition; taken together, they act faster and give a more lasting result.
Complications and prognosis
The prognosis is serious for purulent and secondary septic synovitis. Complications may include purulent panarthritis, phlegmon with lesions of cartilage and bones. In the case of reactive synovitis, the prognosis is favorable.
Synovitis of the knee joint, the symptoms and treatment of which we have examined, is a relatively common disease. Often it is a secondary process, a complication of arthritis. Therefore, any pain, discomfort during movement or swelling should be controlled.
If symptoms do not go away within a few days, you should see a doctor.
What is tenosynovitis
Tenosynovitis is an inflammation of the tendon sheaths. The latter are tubular-shaped connective tissue filled with liquid lubricant. The sheaths surround the tendons, which are made of flexible fibrous collagen tissue. It is what attaches muscles to bones. If the outer covering of the tendons becomes inflamed, it is called tenosynovitis. Both inflammatory diseases are accompanied by pain when moving, so only a doctor can make an accurate diagnosis.
Tenosynovitis most often affects the hands, wrists and feet