What is gonarthrosis?
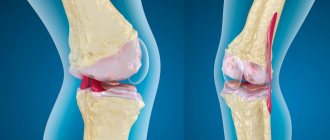
Gonarthrosis (syn. arthrosis deformans, osteoarthrosis, osteoarthritis, degenerative arthritis of the knee joint) is a polyetiological degenerative-dystrophic disease accompanied by joint deformation, destruction of hyaline cartilage, the appearance and growth of osteophytes, and loss of limb mobility. It leads in number among all arthrosis in the musculoskeletal system. The knee is a very important place of articulation of bones, because the possibility of free movement depends on it.
Fact!
Pathology of one department can deform another. For example, gonarthrosis worsens the condition of the spine.
The cause of primary damage to large joints is explained by the heavy daily load placed on them. Women suffer from arthrosis 10 times more often (due to hormonal characteristics). In 75% of cases, the part that articulates the femur and tibia is affected. The patellofemoral side is affected less frequently, but more often leads to disability. In practice, bilateral gonarthrosis occurs predominantly.
Briefly about the disease
The disease is classified as degenerative-dystrophic and affects women more often than men. Although if a man has problems with being overweight, regularly gets cold, or often injures his knees while doing active sports, then he too is at risk.
According to WHO forecasts, in the coming decades, gonarthrosis will become the fourth cause of disability in women and the eighth cause in men. Thus, the problem of effective treatment of gonarthrosis acquires not only medical and social, but also economic significance. (Kosareva et al.)
As a rule, the pathology is chronic and progressive. The fact that the disease is developing is indicated by inflammatory processes that are not observed at the beginning. Late stages of gonarthrosis do not respond well to conservative treatment and, as a rule, lead to joint replacement.
Causes of the disease
Physiological aging is an inevitable process for living beings. Changes occur in all tissues, including bones, muscles, cartilage, etc. Against this background, joints weaken, become worn out, and lose flexibility and elasticity. This begins at the 40-year mark.
If for some reason the wear and tear of biological tissues accelerates, joint damage progresses faster, that is, with arthrosis, the process of destruction begins to predominate. Hormonal imbalance plays a special role in this - failure of the thyroid gland, menopause, taking hormones.
Cartilage loses its natural elasticity and density. It can no longer absorb movement and is gradually replaced by bone tissue, which grows in the form of spines - osteophytes. The functionality of the joint is lost.
The development of gonarthrosis is preceded by predisposing factors: mechanical, biological, physiological, etc.
The main reasons may be:
- Congenital anomalies of the knee joint - hypermobility, congenital dislocation of the patella, articular dysplasia, valgus and varus deformity;
- Past injuries - menisci with displacements/ruptures, joints, local dislocations, sprains, bone diaphyseal fractures, knee surgeries.
- Metabolic disorders - obesity, hemochromatosis, gout, Wilson's disease.
- Endocrinopathies - thyroid disorders, diabetes mellitus, acromegaly.
- Changes in joints of a neurodystrophic nature.
- Inflammatory processes in the knee joint.
According to the etiology, gonarthrosis can be primary or secondary. In the first case, it is often hereditary or idiopathic in nature and occurs without external causes. Secondary gonarthrosis of the knee joint develops against the background of aging and various previous diseases.
Provoking factors include old age, female gender in menopause, obesity, physical inactivity, constant stress on the joints, professional activity with constant squatting or kneeling, previous injuries, inflammation, heredity (pathology of the type II collagen gene).
The disease can be provoked even by starting to exercise too actively after a long break. This is often done by retirees who decide to start leading a healthy lifestyle. Unprepared knee joints are easily injured and micro-tears occur in them. Even minimal damage ends in gonarthrosis, not to mention more serious injuries.
Pathogenesis
The pathology develops over a fairly long period of time. The whole process can be defined in the following sequence:
- The emergence of causes of disruption of natural metabolic processes provokes the destruction of cartilage tissue.
- Destructive processes destroy the structure of the fibers responsible for the shock-absorbing effect. Not only the elasticity of the tissues gradually decreases, but also the stability of the joint.
- Due to the constant increased load on the joint membrane, an inflammatory process occurs, causing a decrease in mobility.
Symptoms of gonarthrosis of the knee joint
The most important symptom of damage is pain. It does not appear immediately, so early diagnosis is delayed, because as long as it doesn’t hurt, no one worries. A person does not think, for example, when climbing stairs, about the complexity of the biomechanics of movements in the knee joint. But when the pain comes, he begins to realize that he overcomes a huge number of steps a day and this is hard work.
So, among the initial signs of gonarthrosis are morning stiffness and minor discomfort (not even pain), which quickly disappear with movement. After the joint warms up, they disappear. This is characterized by the so-called “starting pain”. It manifests itself not only at the beginning of walking, but also when changing position, for example, getting up from a chair. As soon as the patient “diverges”, it will disappear, but after the load it will appear again.
There may be slight swelling of the joint, but without visible external changes. From time to time, when walking, clicking, creaking, weakness, and tingling sensations occur in the legs. All this is short-term in nature. The pain symptom is not very disturbing and the person comes to his senses already at stage II.
Gonarthrosis of the knee joint of the 2nd degree manifests itself with a more intense pain syndrome, which is localized along the anterior-inner surface of the joint. Pain occurs even with minor exertion and intensifies during intense walking. You can't confuse it with fatigue. After a long rest, it goes away for a while, but then resumes again.
Painful sensations in this phase already occur much more often and are more intense. With gonarthrosis, the flexion function is impaired, resulting in a limp. To help such a patient, doctors often resort to surgery even at this stage.
Crunching and creaking when walking are already obvious, movements become more limited, and when you try to bend your leg, sharp pain occurs. The joint becomes swollen and changes its configuration.
The third stage is characterized by permanent pain, including at rest and at night. The pain is constant, lameness progresses, and muscle atrophy begins. The patient needs supportive devices. At this stage, varus curvature of the legs is provoked, when the limbs acquire an O-shape, as they say, “legs like a wheel.”
Every movement provokes friction between the articular surfaces, which causes pain and disturbs sleep. The leg cannot bend or straighten. The gait becomes duck-like and a cane or crutches are required.
At this stage, the osteophytes are already massive; they often break off into the cavity of the joint capsule, which makes the pain even more unbearable. At this time, knee replacement surgery becomes vital and urgent. Otherwise, you will face excruciating suffering and life in a wheelchair.
The fourth stage is the end point. All functional articular structures have already been lost - the hyaline cartilage has been erased, there is no joint space left, the epiphyses of the bones are deformed, and the osteophytes have become large. Pain is not relieved by analgesics. A persistent flexion-extension contracture sets in - maximum loss of support, coordination and ability to move. The person finds himself confined to a wheelchair; at best, he moves with the help of a walker.
Important!
The consequence of gonarthrosis is often an increase in body weight and an increased risk of heart disease due to decreased physical activity.
The degree of self-care decreases sharply: not only walking is difficult, but also turning in bed, getting up, and sitting down. The patient constantly remembers, fears and expects pain. Usually, one of the joints suffers from irreversible changes to a greater extent than the second.
Diet
Diet for gonarthrosis of the knee joint
- Efficacy: healing effect
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
One of the most important factors slowing down the development of degenerative-dystrophic processes in the cartilaginous tissue of the joints is therapeutic nutrition, which, in combination with drug treatment, physiotherapy, exercise therapy, orthopedic regimen, therapeutic massage and spa treatment, can improve the patient’s quality of life. The diet for gonarthrosis is aimed primarily at correcting metabolic processes, regulating body weight/fighting obesity , preventing pathological changes in the hyaline cartilage of the knee joints, stopping the inflammatory process and normalizing articular connective tissue structures. Medical nutrition is based on the following principles:
- Physiological completeness and balance of the diet with a high content of minerals/vitamins. For patients with normal body weight, the energy value of the diet should not exceed the average daily energy expenditure.
- Any fish/meat broths containing extractives, refractory fats, fatty meats, smoked meats (ham/bacon), semi-finished meat/fish products or canned food containing various kinds of food additives in the form of preservatives, flavor enhancers and dyes should be excluded from the diet. , salo.
- Limit to 5-8 g/day salt and salty foods.
- Introduction of 1-2 fasting days/week in the form of a curd fasting day (350-400 g of cottage cheese and 500 grams of milk for 3-4 doses); fruit and vegetable fasting day (1.5 kg of fruits/vegetables with rosehip decoction); kefir fasting day (1.5-2 liters of kefir).
The basis of nutrition for gonarthrosis should be a diet enriched with vitamins/microelements - low-fat varieties of sea/river fish, seafood, dietary meat, low-fat cottage cheese, offal, chicken eggs, butter, cereals, vegetables/fruits, unsalted cheese, whole grain varieties bread, nuts, low-fat dairy products, virgin vegetable oils.
To maintain the cartilage tissue of the joints, it is necessary to include in the diet foods containing mucopolysaccharides, which are by their nature natural chondroprotectors (red fish, cartilage, chicken/pork legs, chicken meat, hard cheeses, gelatin) from which it is recommended to prepare jellied fish, jellies, fruit jellies/jelly. These products, when taken frequently/long-term, normalize the structure of cartilage tissue, help accelerate the processes of its synthesis, slow down degenerative processes and normalize joint function.
In case of obesity/body weight exceeding the norm, the calorie content of the diet should be reduced within 500-600 kcal and not exceed an average of 1800-2000 kcal/day, which allows for a gradual reduction in body weight. First of all, simple carbohydrates up to 250-300 g and refractory animal fats up to 60 g are subject to restrictions, and the protein content must correspond to the physiological norm.
Limit the consumption of white bread, pastries, sugar, confectionery, sweets, cream-containing products, honey, chocolate, fast food, fatty meats, mayonnaise, high-fat dairy products (cream/sour cream), duck/goose meat, smoked meats, animals/ cooking fats. It is prohibited to consume salty foods (canned food, pickles, preserves), starchy foods, cocoa, strong black tea, coffee, seasonings/spices that increase appetite - ketchup, vinegar, garlic, ground black pepper, horseradish, mustard, onions. All fried foods are also excluded. Meals are fractional. Sweet carbonated/alcohol-containing drinks are subject to restrictions.
Diagnostics
An appointment with a doctor begins with listening to the patient’s complaints, which are of a specific nature. Next, a physical examination is carried out, which helps to detect the presence of joint deformation, smoothness of its contours, fluctuation, pain on palpation, and curvature of the limb.
To the preliminary diagnosis, the doctor adds instrumental examination methods, and sometimes laboratory ones. The first step or the simplest method is to x-ray the joint. It will show the degree of narrowing of the joint space, changes in the contours of the adjacent bones, and osteophytes.
X-ray signs of hoarthrosis by degree:
- Gonarthrosis of the knee joint 1st degree - the joint space is narrowed slightly; in some cases, unexpressed subchondral osteosclerosis is observed.
- Gonarthrosis of the knee joint 2nd degree - narrowing of the joint space exceeds the physiological norm by 2 times. Subchondral sclerosis is more pronounced; small bone growths are detected along the edges of the joint space/in the area of the intercondylar eminence.
- Gonarthrosis of the 3rd degree - the joint space is practically absent, there are zones of osteoporosis, the articular surfaces are deformed, subchondral sclerosis is replaced by necrosis, extensive osteophytes are characteristic.
The early stage is characterized by scarcity of tissue changes, so x-rays may be ineffective.
An ultrasound of the joint is performed, but it often does not provide a clear image and does not allow changes to be assessed. For such cases, a CT scan (if bone pathology is suspected) or MRI (if soft tissue damage is suspected) is prescribed. Change detection is 85-90% accurate. This study helps to detect even small osteophytes and cartilaginous growths.
Laboratory diagnosis of gonarthrosis serves only as an addition. With gonarthrosis, the composition of the synovial fluid changes: the level of calcium and phosphorus increases, which confirms the diagnosis.
medi products
Orthoses that correct the position of the knee joint can be an effective alternative to endoprosthetics and pain medications.
Knee braces and orthoses: Genumedi, Collamed OA, M.3s OA and M.4s OA can be used to treat gonarthrosis at different stages.
Conservative treatment of gonarthrosis of the knee joint
Such therapy will be effective in the early stages of the disease. The complexity of conservative treatment involves not only pharmaceuticals, but also non-medicinal methods, for example, physiotherapy, exercise therapy, exercises, wearing orthoses, etc. In any case, all treatment regimens and drug dosages are prescribed only by a doctor!
Early manifestations are quite effectively treated with the use of locally irritating ointments. During periods of exacerbation of pathology, nonsteroids, glucocorticosteroids, and analgesics are used.
PRP or plasma therapy can also help - intra-articular injection of your own plasma enriched with platelets. The result will be a reduction in inflammation and the launch of regeneration processes. After the acute process subsides, they switch to physical therapy, exercise therapy, massages, etc.
The drugs prescribed are chondroprotectors and drugs to improve microcirculation. This is already maintenance treatment.
During the period of remission, exercise therapy, massage of the muscles of the lower leg and thigh are indicated, which will help improve lymphatic drainage, relieve swelling, strengthen the muscular-ligamentous apparatus of the legs and slow down the progression of the pathology.
Physiotherapeutic procedures will also be effective: UHF, ultrasound, magnetic and laser therapy, electro- and phonophoresis with drugs, microwave therapy, ozokerite applications, inductothermy, sinusoidal modulated currents, etc.
It is impossible to completely eliminate arthrosis. Treatment stops or slows the progression of the disease, eliminates symptoms (pain, stiffness) and allows the patient to improve their quality of life. After a diagnosis of arthrosis is made, you have to monitor your joints and undergo preventive and symptomatic treatment for life.
Self-help is a way to improve your quality of life
Self-help has a huge impact on the outcome of gonarthrosis treatment. Be active in the fight against the disease: watch your weight, stay physically active and eat healthy foods.
Surgical treatment of gonarthrosis
Conservative treatment with its drugs and non-drug methods is effective only in the early stages of the disease. For advanced cases, the only option for salvation will be surgery. Direct indications for surgery are severe dysfunction of the joint, severe pain and loss of performance (full/partial).
Surgical treatment is essentially endoprosthetics, when a natural joint is replaced with a synthetic one. Endoprosthesis replacement is used for grade 3 and 4 gonarthrosis. It can be total or partial.
Another method of surgical treatment is arthroscopy. This is not only diagnostics, but also removal of disorders and defects inside the joint using the endoscopic method. The procedure is minimally invasive, that is, non-traumatic. It is used as a treatment for factors that provoke arthrosis - meniscus damage, ligament ruptures, etc.
Two more methods are corrective osteotomy and arthrodesis. In the first case, an artificial redistribution of the load on the joint is implied. In the second, surgical immobilization of the joint by connecting bone tissues together. This relieves pain, but the leg will only serve as a support.
The last two methods are rarely used. Only when endoprosthesis replacement is not possible.
Regardless of the type of operation (except arthroscopy), the patient undergoes rehabilitation for 3–4 months, and full recovery takes up to six months or more.
Endoprosthetics is the only method that, in advanced cases, relieves the patient of pain and disability caused by gonarthrosis. Modern knee replacement designs have been so improved that in most cases they serve patients for 20–25 years. But installing a prosthesis is an extreme method that should be used only after using all possible conservative methods, since preserving “your” joint is always better than installing an artificial one.
Fact!
At stage 4 of degenerative processes with bilateral damage, the pain syndrome is pronounced and “does not go away” either day or night, so “emergency” total bilateral endoprosthetics is performed.
Prevention
Prevention of gonarthrosis of the knee joint comes down to the following measures:
- Elimination/minimization of severe physical overload of the knee joint (sports, household, professional).
- Avoidance of knee joint injuries/permanent microtrauma.
- Body weight control and dietary nutrition in cases of exceeding the physiological norm.
- Physical stress on the joints that is adequate to the age/condition of the body.
- Wearing special shoes/low heels, to unload the joint - walking with a cane.
- Regular wearing (as prescribed by a doctor) of knee braces/orthoses.
List of sources
- Loginov S.I., Solodilov R.O. The influence of gonarthrosis on the kinematics of the knee joint. Bulletin of Siberian Medicine. 2016;15(3):70-78.
- Kashevarova NG, Alekseeva LI, Anikin SG, et al. Osteoarthritis of the knee joints: risk factors for the progression of joint disease in a five-year prospective disease. Materials of the III Eurasian Congress of Rheumatologists, (Minsk, Republic of Belarus, May 26-27, 2021). Issues of organization and informatization of healthcare. 2021.
- Kosareva M.A., Mikhailov I.N., Tishkov N.V. Modern principles and approaches to the treatment of gonarthrosis // Modern problems of science and education. – 2021. – No. 6.
- Bagirova G.G. Osteoarthrosis: epidemiology, clinic, diagnosis, treatment / Bagirova G.G., Meiko O.Yu. - M., 2005. - 224 p.
- Badokin V.V. Main symptom-modifying slow-acting drugs in the treatment of osteoarthritis // Breast Cancer. 2011. No. 12. pp. 72–79.