What is bursitis?
Bursitis is an inflammatory disease of the synovial bursa.
The term bursa refers to a sac-like cavity filled with fluid.
Wherever we have bones, tendons, or ligaments, there are sacs called bursa. They are needed so that these places do not rub against each other so much. To prevent friction, the contact points are softened with special bursa bags. These bags are lined with special cells called synovial cells. With the help of bags, the joints work normally and perform the range of movements we need.
There are 160 similar bags with synovial fluid in the human body, and any of them can become inflamed.
The pathology has pronounced symptoms and requires treatment. It occurs due to the fact that the body protects itself in this way, protecting the lining of the bag from further injury and destruction. Sometimes, for the disease to subside and go away, all you need is rest, since in a state of rest the tissues heal, are restored and the inflammation recedes.
Causes
In most cases, bursitis is caused by injury, excessive stress on the joints, or infection. As a result of these factors, metabolic crystals begin to form in the bag, which provoke the disease.
Bursitis can also be caused by:
- minor soft tissue injury in the joint area (cuts, abrasions, bruises, sprains);
- inflammation that occurs near the joint capsule;
- chronic infection that occurs anywhere (caries, tonsillitis, genitourinary tract infection, intestinal pathology);
- crystallization in the bursa (for example, such crystals are provoked by uric acid, which occurs with gout);
- The work is monotonous and also hard. physical exercise;
- sports activities for wear and tear;
- obesity;
- unfavorable working conditions;
- chronic pathologies;
Additional causes of joint bursitis include autoimmune diseases, treatment with hormonal drugs, and changes that occur due to age (menopause). Overheating or, conversely, hypothermia of a certain part of the body, allergies, acute intoxication.
People at risk of getting a disease such as bursitis are:
- athletes (sports that involve regular movement, cycling, golf, gymnastics);
- people experiencing high physical stress associated with work;
- people have chronic infections;
- allergy sufferers;
- people with weakened immune systems;
- aged people;
These categories of the population need to carefully monitor their health and, if initial symptoms occur, visit a specialist.
Pathological anatomy of the disease
The cause of exacerbation of the symptomatic picture and the need for a therapeutic complex is inflammation of the bursa.
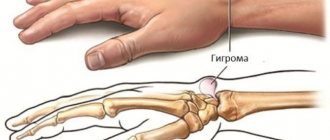
A bursa is a slit-type formation located relatively close to protruding bony areas, within which there is a relatively small amount of fluid.
The key function of the bursa is to cushion and protect the periarticular tissues from excessive pressure or excessive friction.
With systematic microtraumas, as well as increased pressure inside the joint, aseptic inflammation may occur, which will result in the active release of fluid from the bursa membrane. Depending on the amount of fluid produced, local swelling appears, caused by protrusion of the filled cavity.
Symptoms
If bursitis is not associated with injury, then the disease progresses from several days to several weeks.
Symptoms of bursitis are:
- swelling;
- increased temperature in the area of inflammation;
- pain and discomfort in the joint and area around the joint;
- pain on palpation;
- limited movement;
- skin redness;
If a joint is affected by bursitis, this area will be hot to the touch and discomfort will be felt upon palpation. In addition, a person will not be able to normally bend or straighten an arm, leg or other part of the body affected by the disease. In the morning, there may be limited movement and stiffness.
The inflamed bursa can increase significantly in size.
The entire range of symptoms will depend on the root cause that caused the disease, as well as the degree of the disease, the place where the bursa became inflamed.
If the bursa is located close to the skin, then common symptoms will be: swelling, redness and fever. For example, the outside of the heel, the elbow bursa at the very tip of that elbow.
With a deeply located bursa, swelling and hyperemia of the tissues will no longer be so pronounced; moreover, symptoms may be absent for some time at all. For example, vertebral bursa of the thigh, subacromial bursa of the shoulder.
Swelling may be less noticeable in people who are overweight.
If bursitis is of an acute type, then the pathology may develop unexpectedly, accompanied by acute pain, stabbing pain. At night, a person is tormented by shooting pains. When you feel the joint, you feel a seal, it is not hard, it is filled with liquid. It feels like a balloon filled with water. Movements are limited. There is heat in the area of inflammation, the joint area is hot.
Stages of development
Bursitis can be acute or chronic.
Acute occurs abruptly and has pronounced signs of the disease. In the chronic course of the pathology, the symptoms are blurred, and attacks occur from time to time. In this case, the patient sometimes does not have swelling and redness, and there is no increase in temperature.
Classification of bursitis
- Bursitis is divided into affected areas: hip, knee, shoulder, elbow, etc.
- Bursitis is divided into acute, acute, and chronic.
- Considering the causative agent of the pathology: specific or nonspecific.
- Considering the nature of the fluid: serous, purulent bursitis, hemorrhagic, fibrinous.
Bursitis of the knee joint
The knee joint is the most complex joint in the human body. There are a large number of synovial bursae in the knee. Causes of knee bursitis include trauma, sprains, microcrystalline arthropathy, inflammatory arthritis, and infections caused by bacteria.
The symptoms of knee bursitis are as follows:
- swelling in the knee area;
- skin redness;
- increased temperature in the diseased area;
- pain on palpation and movement;
Headache, general fatigue, and nausea may occur if bursitis is accompanied by an infection caused by pathogenic microbes. Bursitis can be superficial or deep.
Risk factors causing bursitis of the knee joint will be: untimely treatment, incomplete therapy, diabetes mellitus, gout, rheumatoid arthritis. Weakened immune system.
Elbow bursitis
Inflammation forms in the joint capsule located near the joint. The nature of the pathology is acute, subacute or chronic.
Symptoms of elbow bursitis are as follows:
- the presence of edema and hyperemia;
- pain when bending and straightening the arm;
- increased temperature in the affected area;
- pain on palpation;
If the disease is not treated, it becomes chronic. Here the symptoms are blurred, the skin acquires a normal shade, and the redness goes away. The pain subsides. However, as the load on the sore arm increases, discomfort begins to bother the person again.
The causes of elbow bursitis are constantly received microtraumas. The disease may appear as a result of infection (wound, cut). Leaning on something for a long time, for example, on a table. This may cause swelling in the elbow. The presence of chronic pathologies in the body.
Bursitis of the shoulder joint
Shoulder bursitis occurs in the bursa of the shoulder joint. Divided into infectious or aseptic. The nature of the disease is acute, sub-acute or chronic.
The symptoms of shoulder bursitis are as follows:
- pain syndrome;
- the presence of swelling and redness in the affected area;
- pain on palpation;
- rarely increased temperature (low-grade fever);
Acute bursitis is either cured or becomes chronic. With a chronic course, the symptoms become less pronounced. The patient may experience pain when moving, limited movement, increased fatigue, and rarely numbness.
Causes of shoulder bursitis: intense physical activity, hard work, injuries, sprains, bruises. If bursitis is of an infectious type, then it occurs as a result of the penetration of pathogenic bacteria into the body, more specifically into the synovial bursa. This happens in the case of: a wound, a cut, an abscess, abrasions.
Bursitis of the hip joint
Hip bursitis occurs more often in the female half of the population, also in older people.
Symptoms of hip bursitis are as follows:
- pain in the hip area that gets worse with movement;
- the presence of swelling on the inner or outer side of the thigh;
- increased body temperature;
These signs more often appear in the acute course of the disease; in a situation with a chronic stage, the signs are dulled and do not have a pronounced character.
However, the person still experiences difficulties when moving; for example, he cannot fully lift his leg.
The causes of hip bursitis are as follows: injuries, excess weight, scoliosis, flat feet, body asymmetry, diseases of bones and joints, old age. Also a sedentary lifestyle, salt deposition in the joints, gout, arthrosis.
Bursitis of the heel or foot
Occurs as a result of inflammation in the synovial bursa of the foot. It can be acute or chronic.
Symptoms of heel or foot bursitis:
- tissue hyperemia;
- edema;
- increased temperature in the area of inflammation;
- pain when palpating and stepping on the leg;
In the chronic course of the pathology, the above symptoms are blurred.
Heel bursitis is caused by the following factors: injuries, bruises, standing work, uncomfortable shoes, physical activity in athletes, heavy physical work associated with lifting and moving heavy objects. Abnormal development of the feet at birth or already acquired.
Minimally invasive surgeries of the shoulder joint for inflammation of the periarticular bursa
Only in cases where drug treatment for shoulder bursitis, as well as physical therapy, have been unsuccessful and a person continues to feel tingling in the shoulder, does there become a need for surgical treatment of subacromial bursitis. We draw your attention to the fact that treatment of bursitis of the shoulder joint is carried out using arthroscopic minimally invasive techniques. This operation, during which the surgeon completely removes the inflamed joint capsule, is performed through the so-called “keyhole”.
Shoulder arthroscopy is a minimally invasive surgery for shoulder pain, for which the surgeon uses microscopic instruments with a diameter of 0.5 - 1 cm. An arthroscopic camera helps the doctor obtain a limited but accurate image of the surgical site. This intervention consists of aspiration (suction) of the contents from the joint capsule. In addition, in parallel, the surgeon can treat diseases that cause bursitis, such as impingement syndrome or calcification of the forearm. © bilderzwerg / fotolia
Additional operations when removing a bursa (bursectomy)
Additional interventions
- Removing calcium from the supraspinatus tendon
- Acromioplasty
- Suture placement of the supraspinatus tendon
In addition to the operation, the specialist examines and, if necessary, begins treatment of all structures of the shoulder joint. Thus, if bursitis is suspected, calcium deposits from the supraspinatus tendon, as well as bone spurs under the acromion, can be removed during arthroscopy.
Shoulder arthroscopy: Postoperative treatment and prognosis
After surgical removal of the periarticular bursa of the shoulder (bursectomy), a new bursa is formed in the same place within a short time, performing the functions of the removed tissue in full.
Motor functions of the shoulder are restored a few days after the operation. The pain syndrome disappears immediately.
Almost immediately, the patient can move the shoulder as before and return to previous activities. The stitches are removed after about 10 days.
Make an appointment
Complications
Any form of bursitis leads to severe complications. Untreated acute bursitis can provoke the development of an acute purulent process when the surrounding tissues are affected by pathogenic bacteria. Arthritis develops, which limits a person’s movements and does not allow him to fully engage in sports. When the acute phase becomes chronic, further discomfort and constant pain force a person to leave sports and stop engaging in his favorite profession.
If you start self-medicating and do not consult a doctor in time, you can bring the process to a sad state.
Why self-medication is dangerous
Self-medication is no less dangerous. A doctor at an appointment can recognize bursitis even by minimal signs. To confirm the diagnosis, he will prescribe an ultrasound, x-ray, MRI and will know exactly where the inflammatory process is located. After this, the doctor prescribes treatment for acute bursitis, which may include:
- non-steroidal anti-inflammatory drugs (NSAIDs) – Ibuprofen, Dexalgin, etc.; these drugs also have an analgesic effect;
- in case of a purulent process, the doctor pierces the bursa, removes the pus and rinses the cavity with antiseptics and administers antibiotics;
- in case of severe inflammation, hormonal drugs are injected into the bag;
- prescribes physiotherapeutic procedures.
If all this is not done and treatment is carried out at home with folk remedies, then the risk of developing complications increases sharply, the treatment of which is problematic even for a specialist.
Acute bursitis rarely develops without chronic joint injury. Joint pain requires immediate medical attention. If this is not done, the consequences may last a lifetime.
Sign up for a free initial appointment
Diagnostics
The diagnosis is made by a surgeon, traumatologist, or orthopedist. Additional consultation with an infectious disease specialist may be necessary.
At your appointment, your doctor will easily identify bursitis. Initially, the specialist will conduct a visual examination and collect the patient’s complaints.
The diagnosis is made based on the collection of all signs of pathology and diagnosis.
The following diagnostic methods are needed to exclude other diseases:
- X-ray;
- mri;
- puncture and analysis of synovial fluid;
- blood analysis;
X-rays are performed to see the condition of the patient’s joints, whether there are osteophytes or arthritis.
Magnetic resonance imaging is necessary to visually see the overall picture of the disease.
Fluid puncture is done to exclude infection. With knee or elbow bursitis, the synovial fluid is most often infected.
A clinical blood test is needed to see whether the patient has diabetes or rheumatoid arthritis.
Only a comprehensive examination allows you to accurately diagnose and select effective treatment for bursitis.
Preventive measures
The best method of treating diseases is their timely prevention. To avoid having to experience the effectiveness of modern treatment methods, it is best to take preventive measures. Let's try to figure out what these include.
Disease Prevention
A number of simple recommendations will help prevent elbow bursitis, compliance with which will ensure the ability to maintain healthy joints and the overall level of quality of life:
- Preventing injuries, ensuring skin protection.
- Providing high-quality first aid for injuries to the skin or joint.
- Timely seeking medical help.
- Maintaining a healthy lifestyle.
- Quitting bad habits (smoking, drinking alcohol, overeating).
- Attending preventive medical examinations.
- Preventive use of a course of chondroprotectors like Artracam.
Treatment
Treatment of joint bursitis is aimed at quickly relieving pain and further eliminating the disease. Therapy lasts 14 days or 1.5 months. Surgical intervention is necessary in advanced cases.
Treatment for bursitis includes:
- taking medications;
- physiotherapy;
- aspiration;
It is important to provide rest to the diseased part of the body and avoid further traumatization. If you endure pain, move or work through discomfort, then bursitis will develop into a chronic stage.
The doctor prescribes compresses and ointments to treat bursitis. Cold compresses can be applied to the sore spot for no more than 15 minutes; if kept longer, there is a risk of frostbite.
Non-steroidal medications are prescribed. These include: Ibuprofen, Dexalgin. Antibiotics if infection is present.
If liquid has accumulated, it is removed. This is done after the inflammation in the bursa has decreased, but the fluid remains. Using a syringe, the specialist pumps out 5 to 20 milliliters of liquid, then injects cortisone. Apply a pressure bandage to prevent fluid from accumulating. It is important to carry out such manipulations only in sterile conditions, minimizing the risk of infection and infection.
Injections into the sore joint help a lot. Injections for bursitis are prescribed with Diprospan. Glucocortisone, Prednisolone, Methylprednisolone, Dexamethasone, Triamcinolone are also prescribed.
Physiotherapeutic methods are used such as: ultrasound or diathermy. Physiotherapy helps relieve inflammation, relieve pain, and increase the effect of medications. At the same time, physiotherapy often has no contraindications. Perfectly complements the complex treatment of bursitis.
Other physiotherapy methods:
- balneotherapy;
- magnet therapy;
- electrophoresis;
- shock wave therapy;
A massage may be prescribed, but only during the period when the illness subsides.
Surgery is needed when there is a very large lump, and the treatment will be long and lengthy. Then the specialist can perform a puncture or drainage of fluid in the bursa.
Surgery for bursitis is performed in case of accumulation of purulent contents in the bursa. Sometimes a specialist performs tissue excision or bursectomy. This is done when the previous treatment did not have the desired effect.
Advantages of Dr. Elshansky I.V.
Our clinic, located in the center of Moscow, traditionally deals with bursitis of various types and locations.
Main competitive advantages:
- Doctor with extensive (over 25 years) experience, Ph.D.
- The ability to perform all necessary manipulations immediately, on the day of treatment, incl. ultrasound guided punctures
- If necessary, an ultrasound scan is performed immediately during the appointment and is included in the cost.
- We do not prescribe unnecessary tests and examinations, and if there is still a need for them, we do not require them to be done exclusively in our clinic
- Qualified, polite staff
- No queues - we plan the time and accept appointments strictly by appointment
- Convenient transport accessibility - 5 minutes walk from Turgenevskaya metro station, Chisty Prudy, Sretensky Boulevard