Who, if not pharmacists and pharmacists, should know that ethanol is a typical representative of monohydric alcohols, capable of entering into various chemical reactions. It interacts with alkali metals, magnesium, aluminum, carboxylic, inorganic acids and many other substances, including medicinal ones. According to some data, up to 25% of visits to the emergency room are associated with various adverse reactions between alcohol and drugs [1]. And it is quite natural that such widespread unfavorable events have become fertile ground for various speculations. On the eve of a series of holidays, it’s time to find answers to the most controversial questions about interactions between drugs and alcohol, as well as dispel the myths associated with it.
Thesis No. 1: Alcohol is incompatible with any antibiotics
Status: Myth
Indeed, a number of antimicrobial agents block acetaldehydrogenase, delaying the enzymatic biotransformation of ethanol at the stage of extremely toxic acetaldehyde. Its accumulation in the body contributes to the development of intoxication, which is accompanied by severe sensations. In fact, these drugs work in the same way as the famous disulfiram, used to treat alcohol addiction, which simply causes poisoning of the body. Its typical symptoms are difficulty breathing, tachycardia, nausea and vomiting, low blood pressure, fever or chills.
However, only a few antimicrobial drugs act in this way, in particular: cefamandole, cefoperazone, chloramphenicol, griseofulvin, isoniazid, metronidazole, ornidazole, nitrofurantoin and sulfamethoxazole.
All other antimicrobials do not have strict restrictions when combined with ethanol, but this does not mean that their combination helps to effectively fight infection.
Comparison of the effectiveness of Acyclovir and Valvir
The effectiveness of Acyclovir is quite similar to Valvir - this means that the ability of the drug substance to provide the maximum possible effect is similar.
For example, if the therapeutic effect of Acyclovir is more pronounced, then using Valvir even in large doses will not achieve this effect.
Also, the speed of therapy - an indicator of the speed of therapeutic action - is approximately the same for Acyclovir and Valvir. And bioavailability, that is, the amount of a drug reaching its site of action in the body, is similar. The higher the bioavailability, the less it will be lost during absorption and use by the body.
Thesis No. 2: Alcohol and non-steroidal anti-inflammatory drugs are incompatible
Status: True
NSAIDs are one of the most popular painkillers. In the United States alone, this group accounts for 70 million prescriptions and 30 billion over-the-counter sales per year [2]. They are also used to relieve headaches due to alcohol intoxication. At the same time, most NSAIDs contribute to the development of gastropathy and increase the risk of gastrointestinal bleeding. Alcohol increases the severity of GI side effects of NSAIDs, increasing the risk of bleeding, which has been proven in clinical studies [3].
In addition, when acetylsalicylic acid, ibuprofen and indomethacin are taken simultaneously with ethanol, the duration of bleeding increases - an indicator that reflects the elasticity of blood vessels and their ability to contract during injury [3]. This feature further increases the risk of bleeding. Therefore, when dispensing oral and parenteral NSAIDs during the New Year holidays, it would be a good idea to remind visitors about possible drug interactions with alcohol.
Modern approaches to the diagnosis and treatment of herpesvirus infections
Herpesvirus infection is one of the most socially significant diseases, which is due to the high human susceptibility to herpes viruses and the annual increase in the number of patients with herpesvirus infections both abroad and in Russia, outpacing the natural population growth [1, 4, 16]. According to serological survey data, about 90% of the entire world population is infected with one or more serotypes of the herpes simplex virus (HSV). Over the past 5 years, the increase in registered cases of certain forms of herpesvirus infection is 90%, and the increase in infection is typical in the group of people aged 20–40 years. Recurrent forms of the disease affect 25 to 30% of infected people; in 30%, the infection is found in a subclinical and latent form. Features of the modern course of herpesvirus infection are the long-term recurrent nature of the disease, often an atypical clinical picture, and the emergence of pathogen strains resistant to standard drugs [2, 12].
An analysis of the annual incidence in Russia showed that genital herpes, according to state dermatovenerological institutions, is detected in 20% of the adult population. For the period 2000–2004. the incidence rate of genital herpes in Moscow increased 6 times, in the Moscow region - 2 times [4]. Genital herpes occurs in all population groups, the highest incidence is recorded in the age group of 20–29 years, but there is a second peak at the age of 35–40 years. Individuals who begin early sexual activity are at increased risk of developing the disease. Young people aged 15–19 years often develop genital herpes, which may be due to lack of awareness about urogenital infections and their prevention [11].
We believe that one of the reasons for the epidemic of the disease is poor diagnosis of subclinical or atypical forms of herpesvirus infection. In such cases, reactivation of the virus is observed less frequently than in recurrent disease with clinical manifestations. It has been established that after primary infection, the herpes virus migrates from the site of inoculation along the peripheral nerves to the spinal and cerebral ganglia, where it remains “dormant” and invulnerable to antiviral drugs. Under the influence of provoking factors, the virus is reactivated and migrates further along the peripheral nerves. In this case, irritation of the nerve endings occurs, leading to prodromal sensations in the form of tingling, burning or itching, the so-called precursors of vesicular rashes. However, asymptomatic production of the virus on the mucous membranes is possible, which is associated with insufficient local immune defense mechanisms. Consequently, the herpes virus can be transmitted during the period of clinical remission of a recurrent herpes virus infection. Such chronic viral shedding can cause infection of a sexual partner, newborns, and the development of neonatal herpesvirus infection [7].
The clinical picture of herpesvirus infection is diverse and depends on several factors [12]:
- characteristics of the HSV virus: type, antigenicity and virulence;
- gender, age and degree of immunocompetence of the patient;
- stages and phases of the disease (exacerbation or remission);
- severity and duration of the infectious process;
- the presence of concomitant diseases that affect the course of the infection;
- the presence of previously conducted therapeutic measures.
The primary episode of the disease is characterized by extensive vesicular and erosive-ulcerative rashes, severe general clinical symptoms and prolonged viral replication. In 80% of patients, typical manifestations of primary infection are preceded by local prodromal symptoms in the form of paresthesia, itching, pain, burning, regional lymphadenitis, as well as deterioration of the general condition (headache, fever, chills, myalgia, weakness, sleep disturbances) [7] . Then rashes appear on the mucous membrane and skin in the form of individual or grouped vesicular elements 2–3 mm in size on an erythematous background. Usually the rash is profuse, the blisters quickly burst, leaving behind erosions with irregular outlines or an ulcerative surface. As a rule, rashes tend to reappear in the same place.
The duration of the acute period of the disease ranges from 8–10 to 18–22 days. Clinical manifestations increase during the first week. Over the next 2 weeks, asymptomatic desquamation of the epithelium damaged by the virus occurs. Typical herpes simplex rashes during the primary episode are localized perioral in the area of the red border of the lips, wings of the nose, genitals, and gluteal region. Also, quite often, the primary episode of herpes virus infection can occur with damage to the oropharyngeal mucosa in the form of gingivitis, glossitis, stomatitis, and herpetic sore throat [4]. In immunocompromised patients (oncological diseases, HIV infection, taking glucocorticosteroids, cytostatics, radiation therapy), complications such as sacral radiculopathy, severe aseptic meningitis or disseminated infection requiring hospitalization are possible.
The clinical manifestations of relapse are shorter compared to the primary episode of herpesvirus infection; the duration of complete epithelization is only 5–7 days. With increasing duration of the disease and under the influence of therapy, the clinical picture of herpes simplex often changes.
In a typical course, the clinical picture of herpesvirus infection in most cases allows a correct diagnosis to be made without the use of additional laboratory and instrumental methods. Difficulties in differential diagnosis may arise with atypical forms of herpes simplex or other diseases characterized by similar skin rashes. Sometimes it is necessary to differentiate between herpes virus infection and scabies, traumatic lesions of the skin and mucous membranes, contact dermatitis, Dühring's dermatitis herpetiformis, streptococcal impetigo, pemphigus, bullous pemphigoid, fungal infections of the skin and mucous membranes, fixed toxicerma, Darier's, Behçet's, and Crohn's diseases.
With an atypical course, herpes simplex rashes in the affected area may bypass certain stages of development. Only erosion, papular elements and edematous spots against the background of erythema are preserved. With this form of herpesvirus infection, characteristic lesions on the mucous membranes and skin may be absent, only hyperemia and diffuse swelling are noted, and recurrent painful cracks occasionally appear on the mucous membrane. A recurrent form has also been described for genital herpes, which is characterized only by itching, and in some cases there are no subjective sensations [13].
Atypical herpes in the genital area can masquerade as some sexually transmitted diseases, such as syphilis. Differential diagnostic signs of herpetic eruptions in this case are: polycyclic outlines of lesions, less pronounced reaction of regional lymph nodes, absence of infiltrate at the base. Herpetic rashes in the genital area are differentiated from herpetiform chancre in primary syphilis, syphilides in secondary syphilis. When examining the discharge, there is no treponema pallidum.
The atypical form of genital herpes is often masked by a concomitant urogenital infection and is not always diagnosed by doctors. A frequent combination of genital herpesvirus infection with Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma genitalium, Gardnerella vaginalis, Candida albicans, human papillomavirus types 16, 18, and cytomegalovirus has been noted. In addition, the accompanying urogenital microflora is a favorable background for recurrence of the disease [7].
Particular difficulties in differential diagnosis may arise when a herpes virus infection is combined with the above diseases. In such cases, a history of the disease and diagnostic tests (studies to identify virus antigens and antibodies to it) help make the correct diagnosis. The purpose of laboratory diagnostics is to determine the etiological factor (detection of the virion, genome or antigen of viruses) and dynamic monitoring of the course of the pathological process (dynamics of specific antibodies). Laboratory diagnostic data are often used to confirm the diagnosis of herpesvirus infection.
Modern methods for identifying HSV include detecting the virus by classical virus isolation on sensitive cell cultures using the immunofluorescent method (determination of ELISA antibodies) and the method of identifying fragments of viral nucleic acids (polymerase chain reaction - PCR) [4]. We believe that among the many laboratory tests for verifying HSV on the skin and mucous membranes, PCR is the most informative - detection of viruses and virions. The advantages of the method are direct determination of the pathogen (detection of specific DNA sections), high specificity (95–100%) and sensitivity (95–98%) - from 10 to 1000 genomic copies in the sample, high speed of obtaining analysis results.
To assess the activity of the viral process and the adequacy of the antiviral immune response, the most accessible test for widespread clinical practice is a test for determining the level of specific IgM and IgG for HSV types 1 and 2. There are peculiarities in the interpretation of this test. In a number of patients without clinical manifestations of genital herpes, only specific IgG to HSV increases. There is an opinion among medical practitioners that this is evidence of viral replication, and antiviral and immunomodulatory therapy is carried out to reduce the activity of the infectious process. This tactic is not entirely correct. In these cases, to verify the viral antigen itself, an additional PCR test is necessary. Negative PCR for HSV types 1 and 2 with an increase in specific IgG in patients without clinical manifestations of herpes virus infection indicates virus carriage and does not require additional examination and treatment. We insist on this provision, since often the first stage of laboratory diagnosis is the determination of specific antibodies to HSV types 1 and 2. With this analysis, many practitioners replace the identification of the herpes virus itself and justify the prescription of antiviral therapy by the detection of high titers of specific antibodies to HSV types 1 and 2. It is worth noting that today there are no clinically significant titers of specific IgG to HSV, and the level of their excess is also clinically uninformative. We believe that antiviral therapy is indicated only for patients with clinical manifestations of genital herpesvirus infection, and in their absence, only if replication of the herpes virus is detected by PCR.
In addition, during serological examination in some patients with the onset of clinical manifestations of herpesvirus infection, false negative results are possible. We studied a unique group of patients newly infected with HSV with initial clinical manifestations in the form of genital herpes. On the first day of the disease, we noted the formation of a primary early humoral response in 86% of patients in the form of the synthesis of specific IgM. On days 7–14, 26–47% of patients showed an increase in the level of specific IgG against the background of a decrease in specific IgM. However, by the 28th day of the disease, 38% of patients did not show seroconversion, i.e., the level of specific IgM and IgG did not increase. In 86% of these patients, a late humoral immune response was formed only after 2 months. The results obtained show that during the period of conversion of the early humoral response to the late one (by the 28th day), a “seronegative” zone is formed in 38% of patients. It is during this period that false-negative results of a study of specific humoral immunity are possible, which should not be regarded as the absence of HSV infection.
Thus, the diagnosis of herpesvirus infection and treatment tactics are based on anamnestic, clinical data and laboratory examination results.
Treatment of patients with herpes virus infection presents certain difficulties due to the lack of antiviral drugs that can completely eliminate HSV from the body, as well as due to the formation of disorders in the immune system with a high frequency of relapses. In addition, the reasons for the ineffectiveness of treatment are often the insufficiency of the therapeutic doses of drugs used by doctors to control the severity of the disease, a lack of understanding of the mechanisms of action of acyclic nucleosides, as well as the lack of personal contact between the patient and the attending physician.
Currently, all methods of drug therapy and prevention of herpesvirus infection can be combined into three main groups: chemotherapy (acyclic nucleosides), immunotherapy and combination therapy, including chemo- and immunomodulatory drugs.
In 1981, the drug acyclovir (Zovirax) was created and introduced into clinical practice. The mechanism of action of acyclovir is based on its high specificity for viral thymidine kinase, which phosphorylates acyclovir. The viral DNA polymerase mistakenly includes phosphorylated acyclovir instead of natural deoxyguanosine triphosphate into the terminal sections of new viral DNA, thereby interrupting the process of viral replication at any stage, and new generations of viruses are not formed. Currently, it is the most frequently prescribed antiherpetic drug and has already been used by more than 50 million patients [15]. In addition, new antiviral drugs of the same group have recently been synthesized and widely used: valacyclovir (Valtrex) and famciclovir (Famvir) [5]. According to studies, the bioavailability of antiherpetic drugs from the group of acyclic nucleosides increases as follows: acyclovir - 20%, valacyclovir - 54% and famciclovir - 77% [10].
There are two main ways to use antiviral chemotherapy drugs:
- episodic administration (as needed during exacerbations of herpesvirus infection);
- prolonged or preventive therapy.
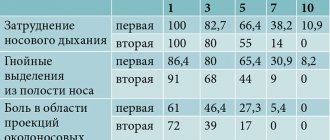
In the first case, the drug is prescribed in a short course for 7–10 days. In the second, patients take the drug daily for several months or years, not only to stop a given relapse, but also to prevent subsequent relapses. We have studied various regimens for the use of acyclic nucleosides in patients with genital herpesvirus infection with a high frequency of relapses (table).
Clear advantages of high-dose therapy were evident when assessing the duration of relapse of genital herpes during treatment. Valtrex and Famvir in high doses reduced the time of relapse by more than 2 times compared to standard therapy (from 3.9 to 1.7 days). The effectiveness of acyclovir was slightly lower. Nevertheless, all of these drugs significantly reduced the time of clinical manifestations of relapse compared to the standard treatment regimen. Our studies have revealed the undeniable advantages of a high-dose therapy regimen, when against its background, already on the 3rd day, the intensity of itching, burning, swelling and hyperemia in the area of the rash significantly decreased.
The study showed that the duration of remission in patients with various forms of genital herpesvirus infection depends on the treatment regimen. With standard and high-dose treatment regimens with Acyclovir, Valtrex and Famvir, in the typical course of the disease the period of remission ranged from 0.8 to 1.6 months, in the atypical form - from 0.7 to 1.7 months. There were no statistically significant differences in the duration of remission with these treatment regimens. At the same time, the prolonged treatment regimen contributed to a significant increase in the relapse-free course of herpesvirus infection. Thus, in the typical form of the disease after treatment with Acyclovir, the period of remission reached 4.1 months, with Valtrex - 10.5 months, Famvir - 9.2 months, in the atypical form - 3.3 months, 7.1 months and 6.8 months, respectively. . Thus, the maximum relapse-free period was obtained with prolonged use of Valtrex and Famvir.
Currently, practicing physicians mainly use standard treatment regimens with antiviral drugs. Prolonged and high-dose treatment regimens are practically not used for the relief and prevention of repeated relapses of herpesvirus infection. Perhaps a barrier to such therapy is the lack of information about its effectiveness. In addition, prolonged therapy helps prevent relapses of genital herpes and thereby has a positive psychological effect on the patient. Unfortunately, poorly informed patients often refuse prolonged and high-dose therapy, expressing concerns about the safety of its use and the development of drug resistance.
High-dose and prolonged treatment regimens improve the quality of life of patients who, at a certain stage of treatment, begin to take a direct part in controlling the disease. Such therapy should be prescribed to patients with a high frequency of relapses, since repeated manifestations of the disease are stressful for them, which, in turn, provokes immunosuppression and contributes to the development of subsequent relapse.
It has been shown that asymptomatic viral shedding usually occurs in the first years after primary infection [15]. Therefore, during the first episode of herpesvirus infection, it is advisable to carry out high-dose therapy, which reduces the risk of transmission of the virus. As practice shows, at this time patients prefer quick and effective treatment. In addition, during this period, patients especially need specialist consultation and psychological support [9].
The patient’s lifestyle determines the choice of treatment tactics for genital herpes. For example, during periods of long trips with climate change, exams, and stressful situations, it is preferable to prescribe prolonged therapy to patients, which in this case is preventive and prevents the possible development of a relapse. An integral part of the treatment and prevention of the spread of HSV is an educational program. The doctor must inform the patient about the danger of spreading the infection, the prospects for treatment and the need for cooperation.
In patients with a high frequency of relapses, a so-called secondary immunodeficiency is formed with a violation of the humoral and cellular components of immunity, a decrease in the number and inhibition of the functional activity of natural killer cells and cells of the monocyte-macrophage series, and a violation of the production of interferon [14]. Such patients are advised to include immunocorrective drugs in the treatment regimen. At present, sufficient experience has already been accumulated in the successful use of interferons (Reaferon, Viferon, etc.), interferon inducers (Cycloferon, Amiksin, Kagocel, Ridostin, etc.), immunomodulators of various spectrums of action (Polyoxidonium, Galavit, Immunomax, Likopid, etc.) for treatment of recurrent herpesvirus infection [3, 6, 8]. However, the prescription of drugs aimed at correcting disturbances in the interferon system, stimulating cellular antiviral defense and strengthening specific antiherpetic immunity should be carried out taking into account the data of an immunological examination of a particular patient.
In conclusion, we will discuss four possible options for medical tactics depending on the results of examining patients for herpesvirus infection.
Option 1. An increase in the level of specific IgG, a negative result of a PCR test for HSV types 1 and 2 in a patient without clinical manifestations of herpes virus infection indicate a virus carrier and do not require additional examination and treatment. The patient is monitored dynamically and a course of antioxidant vitamins is prescribed.
Option 2. If HSV types 1 and 2 are detected during a PCR study in a patient without clinical manifestations of herpesvirus infection, the level of specific IgM and IgG should be assessed. A selective increase in specific IgM indicates primary infection. In these cases, standard antiviral therapy is carried out, after which control PCR is performed. Other immunological examinations are not appropriate. An increase in specific IgG and IgM indicates an enhanced immune response in reinfected patients. They also undergo standard antiviral therapy, after which a control PCR is performed. Dynamic monitoring is also carried out and antioxidant vitamins are used.
Option 3. An increase in the level of specific antibodies in a patient with clinical manifestations of herpesvirus infection and a low frequency of relapses (2-4 times a year) indicates an enhanced immune response and does not require further study of antiviral immunity. Standard antiviral therapy is recommended for such patients. For severe clinical manifestations, high-dose therapy is indicated. Dynamic observation and a course of antioxidant vitamins are carried out.
Option 4. In a patient with clinical manifestations of herpesvirus infection with a high frequency of relapses (more than 6 times a year) and elevated levels of specific IgM and IgG, an immunogram is performed. The subpopulation composition of cells, NK activity and the level of α- and γ-interferons are assessed. If violations in antiviral defense are detected, either prolonged therapy with acyclic nucleosides or standard antiviral treatment in combination with immunomodulatory drugs is carried out. It is necessary to exclude the provoking factor and prescribe a course of antioxidant vitamins. The presented options may not contain all possible situations for examining patients with herpes virus infection, however, they are a guide to action available to primary care practitioners.
Thus, an individual approach to therapy, taking into account the results of clinical and laboratory examination, provides adequate control of the course of herpesvirus infection and provides an advantage over standard treatment. For widespread implementation in clinical practice, it is necessary that such methods of examination and therapy are available to all segments of the population and correspond to the modern level of medical care.
For questions regarding literature, please contact the editor.
A. E. Shulzhenko , Doctor of Medical Sciences I. N. Zuikova Institute of Immunology, FMBF of Russia, Moscow
Thesis #3: Alcohol should be avoided during treatment with antidepressants.
Status: True
It is not recommended to combine alcohol with all antidepressants, although the mechanism of drug-ethanol-drug interaction and the severity of the consequences vary. Thus, in combination with tricyclic blood pressure medications (amitriptyline, maprotiline), ethanol can contribute to hypersedation. It disrupts the metabolism of drugs of this group in the liver, which leads to an increase in their concentration in the blood. If, in addition, the alcohol consumer has a history of alcoholic liver disease, the risks increase even more, since in this case the breakdown of antidepressants slows down and, accordingly, their level in the bloodstream increases. Increasing the dose of tricyclic antidepressants in the blood, in turn, causes cardiac arrhythmias, convulsions, hallucinations and other severe consequences, including coma [3].
The combination of selective serotonin reuptake inhibitors and alcohol is much less dangerous. Drugs in this group generally have a higher safety profile than tricyclic antidepressants and are less likely to enter into drug interactions. However, despite the absence of documented reactions between them and ethanol, their use in combination is still not recommended. This is largely due to the fact that combining SSRIs with alcohol can exacerbate the disease [4]. In addition, it has been proven that when venlafaxine is combined with ethanol, memory and cognitive abilities may decrease [4].
Comparison of ease of use of Acyclovir and Valvir
This includes dose selection taking into account various conditions and frequency of doses. At the same time, it is important not to forget about the release form of the drug; it is also important to take it into account when making an assessment.
The ease of use of Acyclovir is approximately the same as Valvir. However, they are not convenient enough to use.
The drug ratings were compiled by experienced pharmacists who studied international research. The report is generated automatically.
Last update date: 2020-12-13 10:31:36
Thesis No. 4: If you have a headache from drinking alcohol, it is better to take paracetamol
Status: Myth
Paracetamol is metabolized by the CYP2E enzyme to form the hepatotoxic metabolite N-acetyl-p-benzoquinone imine. Normally, it is quickly inactivated by glutathione. When consuming alcoholic beverages, especially chronically, the activity of CYP2E1 increases, which leads to increased production of a toxic metabolite. In addition, during prolonged drinking, glutathione reserves are depleted, which is associated with the accumulation of a toxic metabolite in the blood and an increased risk of developing liver failure [5].
The likelihood of drug interactions between ethanol and paracetamol also increases when taking more than 4 grams of the drug per day. The American regulator FDA recommends that those who take more than 3 alcoholic units per day (remember, an alcoholic unit is 30 ml of 40% alcohol, 100 ml of wine or 250 ml of beer) consult a doctor before taking either paracetamol or over-the-counter analgesics [ 5]. During the New Year holidays, it is important for residents of the capital to draw the attention of consumers to the increased likelihood of hepatotoxic reactions when combining paracetamol and combination drugs containing it with alcohol.
Thesis No. 7: Alcohol should not be combined with certain antidiabetic drugs.
Status: True
In case of diabetes mellitus, drinking alcoholic beverages is generally extremely undesirable - this threatens a sharp drop in blood sugar levels and the development of hypoglycemia, which is associated with a violation of the release of carbohydrates stored in liver cells against the background of alcohol intoxication. The risks of hypoglycemia in diabetic patients who drink alcohol are further increased due to possible drug interactions between ethanol and some sulfonylureas, in particular glipizide [3].
Combining alcoholic beverages with the first-line drug for the treatment of type 2 diabetes mellitus, metformin, can lead to increased levels of lactic acid in the blood and the development of lactic acidosis. The likelihood of its occurrence increases with a low-calorie diet, poor nutrition and liver failure. Therefore, metformin is incompatible with alcohol in both alcoholic beverages and alcohol-containing medications [3].
Insulin also interacts with ethanol. Alcohol can enhance or weaken the hypoglycemic effect of the drug, which can lead to the development of hypo- or hyperglycemia and, accordingly, worsening disease control [7].
Thesis No. 8: If you have a hangover, you can take regular “cold powders”
Status: Myth
Anti-cold combination drugs contain several components, and at least two of them can interact with ethanol. Firstly, most drugs in this group contain paracetamol, sometimes in a dose of 1000 g. When it is combined with alcohol, the risk of hepatotoxic reactions increases. Secondly, many anti-cold combination drugs contain 1st generation antihistamine components. Alcohol can potentiate their depressant effect on the central nervous system, promoting the development of hypersedation and drowsiness [3]. Therefore, drugs from this group should not be recommended as remedies to relieve hangover symptoms.
Sources
- Alcohol-medication interactions. Alberta Health Services. – [Electronic resource] – URL: https://www.albertahealthservices.ca/assets/healthinfo/AddictionsSubstanceAbuse/hi-asa-beyond-abcs-a... (Access date 12/09/2019).
- Alcohol-medication interactions. Alberta Health Services. – [Electronic resource] – URL: https://www.albertahealthservices.ca/assets/healthinfo/AddictionsSubstanceAbuse/hi-asa-beyond-abcs-a... (Access date 12/09/2019).
- Green GA Understanding NSAIDs: from aspirin to COX-2 //Clinical cornerstone. 2001; 3 (5): 50–59.
- Weathermon R., Crabb DW Alcohol and medication interactions //Alcohol research. 1999; 23 (1): 40.
- Adams WL Interactions between alcohol and other drugs //International journal of the addictions. 1995; 30 (13–14): 1903–1923.
- Noureldin M. et al. Drug-alcohol interactions: a review of three therapeutic classes //US Pharm. 2010; 35 (11): 29–40.
- Moore AA, Whiteman EJ, Ward KT Risks of combined alcohol/medication use in older adults //The American journal of geriatric pharmacotherapy. 2007; 5 (1): 64–74.
- According to GRLS data as of December 12, 2019.