- home
- Gynecology
- Adhesions in the pelvis
Interview with Prof. Puchkov on Medical Channel 1 on the topic: “Adhesive disease and infertility”
Adhesions in the pelvis are adhesions of connective tissue that appear on the surface of the pelvic organs. As a result, their mobility is limited and function may be impaired. When these organs are displaced, the adhesions become tense, which leads to pain.
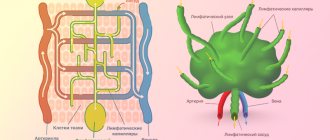
The formation of adhesions refers to a protective reaction of the body aimed at delimiting a pathological focus from healthy tissues that appears due to various reasons: trauma, inflammation, exposure to air, circulatory disorders, etc. With any damage, the body strives to grow a new one on the unprotected area of the mesothelium, and substances are released , synthesizing fibrin. As a result, nearby organs are “glued together” with fibrin fibers.
Most often this occurs during surgical interventions, for example, after myomectomy, and adhesions in the pelvis after cesarean section are not uncommon. They also appear in urgent conditions associated with bleeding (for example, during ectopic pregnancy, ovarian apoplexy, abscesses, etc.), and adhesions in the pelvis in women are formed due to various diseases, for example, endometriosis, salpingitis, oophoritis, fibroids. The likelihood of the formation of adhesions depends on a number of factors: the properties of connective tissue determined genetically, weakened immunity and the individual predisposition of tissues to adhesions.
Symptoms of adhesions in the pelvis
At the initial stage, there are no complaints, adhesions are detected by chance. Over time, pain appears - with adhesions in the pelvis, they can be constant or occur during physical activity, sexual intercourse, and even when changing position. Nausea and vomiting may occur. In severe cases, intestinal obstruction develops due to compression of the intestinal lumen and circulatory disorders.
One of the serious consequences of adhesive disease is infertility. There are three stages of the process:
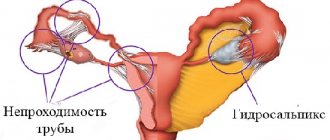
- I - the appearance of single adhesions near the ovary, tube, uterus is typical; nothing prevents the advancement of the egg;
- II - the ovary and tube are connected by dense adhesions, but half of the surface of the ovary is free; adhesions prevent the fimbriae from capturing the egg;
- III - the ovary is almost entirely covered with dense adhesions, the fallopian tubes are deformed and impassable, the lumen is blocked.
If pregnancy does occur, there is a risk of ectopic development due to an obstruction to the movement of the egg. At later stages, blood flow in the uterus may be disrupted, leading to miscarriage.
Symptoms
Symptoms in the presence of adhesions in a woman are very different, however, several common signs can be identified:
- Chronic pelvic pain syndrome is a constant, sometimes almost imperceptible, dull pain in the area of adhesion formation. It occurs due to tension and deformation of organs. In some cases, it can radiate to surrounding organs, the lower back and legs. The pain may intensify during sexual intercourse, physical exercise and prolonged exercise, hypothermia, and when the bladder is full.
- Impaired organ function - reduction or disappearance of menstruation, lack of ovulation, inability to become pregnant.
- In cases of formation of adhesions with intestinal loops - constipation, feeling of bloating, intestinal obstruction.
It is also worth noting that if a woman has adhesions, it is quite possible for her to experience increased pain during menstruation and ovulation. But it is worth considering that in half of the cases, adhesions do not cause any symptoms and are detected only during an ultrasound of the pelvic organs or a visual examination.
Diagnostics
The disease can be suspected if there are relevant patient complaints and medical history. To confirm the diagnosis, a number of examinations are carried out, which include:
- Ultrasound - adhesions in the pelvis are detected in the form of heterogeneous echo signals;
- Hysterosalpingography and hysterosalpingoscopy - performed to assess tubal involvement;
- MRI of the pelvic organs;
- Diagnostic laparoscopy is effective for visualizing adhesions between organs.
To identify the causes of adhesions, laboratory tests may be prescribed: determination of flora, STIs, PCR diagnostics, etc.
Prevention
The cellular and molecular mechanisms of adhesion formation are now quite well understood. Therefore, the process of adhesions after surgical operations, including after laparoscopy, can be sharply slowed down using so-called adjuvant (auxiliary) therapy. This therapy should begin as early as possible after the operation (in the first days and hours) and continue for several weeks. Treatment is aimed at suppressing the inflammatory reaction, suppressing fibrin deposition in the abdominal cavity, and activating fibrin dissolution.
Adjuvant therapy includes the use of the following drugs:
- Fibrinolytic agents are substances that dissolve fibrin, around which adhesions are formed: FIBRINOLYSIN, STREPTOKINASE, UROCINASE, HYALURONIDASE, CHEMOTRYPSIN, TRYPSIN, TISSUE ACTIVATORS OF PLASMINOGEN.
- Anticoagulants - drugs that prevent blood clotting: drugs HEPARIN, OXALATES, CITRATES.
- Antibiotics : TETRACYCLINES, CEPHALOSPORINS, SULPHANAMIDES.
- Anti-inflammatory drugs : corticosteroids, antihistamines, non-steroidal anti-inflammatory drugs, progesterone, calcium channel blockers.
The choice of drugs and treatment regimens depends on each specific case and can only be made by the attending physician.
Treatment of adhesions in the pelvis in women
Conservative therapy is recommended to prevent complications; if the disease appears as a result of an infection, antibacterial drugs may be prescribed; for endometriosis, hormone therapy; for pain relief, as well as for the inflammatory process, anti-inflammatory drugs may be recommended; fibrinolytics are prescribed for resorption.
The goal of surgical treatment is to cut the adhesions and free the organs. Indications for surgery are:
- severe pain syndrome;
- risk of developing intestinal obstruction;
- female infertility.
Postoperative adhesions
During surgical interventions, adhesions are formed due to:
- tissue hypoxia or ischemia - insufficient supply of tissues with blood and oxygen;
- drying tissue during surgery;
- rough manipulation of fabric;
- presence of foreign bodies;
- presence of blood;
- separation of former adhesions.
Foreign bodies that cause adhesions often include talc particles from doctor's gloves, small cotton fibers from gauze or tampons, and suture material. Adhesions also form with endometriosis. During menstruation, a small amount of menstrual blood containing living cells from the lining of the uterus (endometrium) may enter the abdominal cavity through the fallopian tubes. Normally, these cells are removed by the body's own immune system, but if there are any problems, they take root and form functioning endometrial islands that menstruate into the abdominal cavity. Adhesions form around these foci.
Laparoscopy for adhesions in the pelvis
Video from the operating room. Laparoscopic cystadnexectomy for severe adhesions
The gold standard for the surgical treatment of adhesions is laparoscopy, during which all adhesions are sequentially intersected. At the same time, I select the choice of instruments taking into account the area of intervention; when dissecting adhesions between the peritoneal wall and the omentum or intestine, I use the Liga Sure device, which allows for bloodless manipulations while simultaneously sealing the vessels. Between intestinal loops, I always use a cold method for dissection, without electrosurgery, to avoid damage to the intestinal wall with subsequent perforation.
To prevent adhesions and fusion of organs, I use special anti-adhesion barriers, which dissolve without a trace after 7-10 days. These drugs are effective in the presence of exudate and blood, are safe, encapsulation is excluded, and do not require fastening with sutures.
The advantage of laparoscopy is the absence of extensive damage; there is no drying out of the operation area, since carbon dioxide is introduced instead of air (in open surgery), which dries out the peritoneum. When washing, solutions are used, which, unlike napkins, does not injure the mesothelium. Also among the advantages of laparoscopy are the absence of blood loss and high precision of manipulation due to the possibility of visualization. To prevent adhesions and fusion of organs, I use special membranes that dissolve without a trace after 7-10 days.
Our patients are usually discharged on days 2-4; three days after discharge, we conduct a follow-up examination and make recommendations for further treatment. After laparoscopy, a woman can return to her usual lifestyle within two weeks.
I have been performing such interventions since 1993, and have performed more than 900 operations to remove adhesions. I also use modern technologies to prevent the appearance of adhesions during any surgical procedure. Thanks to the modern approach, the likelihood of developing adhesions during surgery in our clinic has been reduced tenfold.
Methods for eliminating synechiae
How to cure adhesions in the fallopian tubes and how to get pregnant? Various methods can be used aimed at restoring the normal functional and anatomical state of these organs. In unadvanced cases, it is possible to cope with the problem conservatively; in advanced cases, surgical intervention is performed. However, with the fourth degree of adhesive disease, its effectiveness does not exceed 15-20%.
The solution to this situation is IVF. In this case, the fallopian tubes are not involved in the process, and a 3-5-day embryo is immediately implanted into the site of its future implantation (uterine cavity). IVF for tubal infertility is the most successful, and the percentage of successful attempts is quite high.
Medication
Drug treatment can be effective during exacerbation of the chronic process, when fluid is detected in the fallopian tubes. Timely prescribed antimicrobial therapy helps stop inflammation, prevent excessive adhesions and restore patency of the fallopian tubes. For already formed synechiae, conservative treatment methods are ineffective.
Physiotherapy
Physiotherapy is used at the next stage of treatment of the inflammatory process, after it subsides. The method is also indicated in the early postoperative period to prevent the formation of adhesions. The most optimal method and dosage regimen is selected by a qualified physiotherapist who specializes in the gynecological field.
Laparoscopy
Is it possible to remove adhesions in the fallopian tubes? Yes, with the help of their dissection during laparoscopy. However, the risk of relapse is quite high. Therefore, such operations are performed on a limited number of women.
If IVF is planned, then laparoscopy can be a preparatory step. In this situation, surgery involves complete removal of the fallopian tubes. A tubectomy is performed when the tube is completely blocked and there is an increased risk of ectopic pregnancy.
Causes of adhesions in the abdominal cavity
The pathological condition in question can develop for a variety of reasons. There are three main groups of factors that can provoke the formation of adhesions:
- Mechanical injuries. These are injuries to the abdomen resulting from a fall from a height, a bullet or knife wound, or as a result of surgery.
- Inflammatory diseases of the abdominal organs. Thus, adhesive disease can develop as a result of current or after previous cholecystitis (inflammation of the gallbladder), enteritis (inflammation of the small intestine), adnexitis (inflammation of the ovaries) and so on.
- Chemical damage to the abdominal organs. Most often observed when bile or stomach contents leak (for example, when a perforated gastric ulcer occurs).
Often the adhesive process occurs in the pelvis. It can develop rapidly, with characteristic symptoms, or be asymptomatic. Thus, adhesions after a cesarean section often do not appear at all. They can be diagnosed when a woman consults a doctor about the inability to become pregnant again, since adhesions in the pelvis can provoke female infertility.
The occurrence of synechiae inside the uterine cavity
Intrauterine adhesions occur mainly due to injury to the mucous membrane during abortion, miscarriage, complicated childbirth, and infectious inflammation. This pathology in gynecology is called Asherman's Syndrome. This disease is characterized by a decrease in the internal volume of the uterus and a deterioration in the quality of endothermy. Asherman's syndrome reduces the ability to conceive and bear a child. The functions of the uterus in this case are hampered by adhesions. With the syndrome, the amount of menstrual flow decreases significantly and may disappear.
The presence of adhesions in the uterine cavity is detected using ultrasound, as well as hysteroscopy. Diagnostic hysteroscopy is considered the most effective, allowing to determine the type of adhesions, their development, and also examine the endometrium. Based on the diagnostic results, the doctor selects treatment methods, taking into account the individual characteristics of each patient.
For Asherman's Syndrome, therapeutic hysteroscopy with excision of synechiae and the prescription of hormonal treatment gives good results. As a result of this operation, the uterus is restored, the endometrium improves to a normal state. The success of treatment largely depends on the degree of endometrial damage. A woman’s chances of becoming pregnant naturally or with the help of assisted reproductive technologies can be assessed already at the diagnostic stage.
Video on the topic
Classification
Intestinal adhesions are classified according to the degree of strength and some morphological characteristics. The scale for assessing the severity of the adhesive process is as follows:
- 0 points - no adhesions;
- 1 point - single fusion, membranous structure, without narrowing of the intestinal lumen (divided in a blunt manner);
- 2 points - two adhesions of a loose structure without blood vessels. The intestinal tube is moderately deformed, the lumen is not narrowed (divided in a blunt way, in rare cases sharp);
- 3 points - more than two adhesions. Dense, can grow blood vessels. The intestine is deformed, the lumen is narrowed to 50% (divided only by acute means);
- 4 points - conglomerate of adhesions. They are dense, permeated with blood vessels. The deformation of the intestinal tube is extensive, the lumen is narrowed by more than 50% (they are separated only by an acute method, it is difficult to avoid trauma to the fused organ).
Surgical treatment of adhesive disease
Treatment is a very difficult task - you can never be sure that a laparotomy performed for adhesive disease will be the last for the patient and will eliminate the process that caused the adhesive process. Therefore, it is always worth considering the feasibility of a particular operation and drawing up a clear plan based on a clinical examination. Only in emergency cases should this scheme be abandoned. The question of the soldering of small intestinal loops to the scar remains open. Therefore, during laparotomy, the old scar should not be excised - the incision is made 2-3 cm away from the scar.
When separating intestinal adhesions, it is advisable to use hydraulic preparation with novocaine. Deserosed areas of the intestinal walls must be carefully sutured. The soldered sections of the gland should be crossed between the applied ligatures. In cases where the intestinal loops form very adherent conglomerates, and it is not possible to separate them, it is necessary to apply a bypass anastomosis between the adductor and efferent intestines (as if to shunt), since the separation of this conglomerate will take a lot of time, and secondly, it will cause additional trauma to the peritoneum . Before deciding on planned surgical intervention, patients require a high-quality X-ray examination. During surgery, releasing intestinal loops from adhesions is a rather difficult task, which, according to Noble, takes about 90% of the operation time. In 1937, Noble proposed an operation, which was called Noble enteroplication of the intestine.
The essence of the operation is that after separation of the adhesions, the intestinal loops were laid horizontally or vertically and sutured together in the area of the mesenteric edge with a continuous thread. Thus, the intestinal loops were fixed in a certain position, and later they grew together. Recurrences of intestinal obstruction were observed after surgery - 12-15%, so this operation was treated with caution. In addition, stitching the intestinal loops takes a lot of time, then the loops begin to peristalt worse.
In 1960, this operating principle was modified by Chalds and Phillips, who proposed to perform enteroplication not by suturing intestinal loops, but by suturing the mesentery of the small intestine with a long needle. Surgery using this method provides better peristalsis and an easier postoperative period. In addition, less time is spent on this operation.
In 1956, White and in 1960, Deder proposed fixation of intestinal loops with an elastic tube inserted into the intestinal lumen by enterostomy. Dederer proposed performing a microgastrostomy, through which a long tube with many holes was inserted throughout the entire length of the small intestine. This method is not bad at all due to the fact that the tube was a frame for intestinal loops and the loops were fixed and fused in a functionally advantageous position. But opening the stomach cavity (Dederer) or intestine (White) was unfavorable with regard to infection of the abdominal cavity. However, during operations for intestinal obstruction, the tube is passed transnasally, bringing it almost to the ileocecal angle.
The tube is fixed to the wing of the nose; later, during the period of intestinal paresis, the contents of the intestine are drained through this tube; nutrients can be introduced into this tube. But basically it is removed a few days after surgery, after reliable restoration of peristalsis, since long-term removal of intestinal contents can cause electrolyte imbalances.
Laparoscopic adhesiolysis of the pelvis
Surgical intervention is widely used today to treat adhesions, but it is carried out mainly by laparoscopic method. Adhesiolysis is used - dissection of pelvic adhesions using special surgical instruments that are inserted through punctures in the abdominal cavity. The operation is performed in an operating room using anesthesia, but the intervention itself is not as traumatic as a full-fledged operation with incisions. Adhesions are dissected and removed in order to restore the functionality of the organs of the female reproductive system and eliminate intestinal problems. This is the safest and most effective method, after which a woman quickly recovers and can live a full life.
Causes of adhesive disease:
- Reasons leading to gluing of the peritoneal layers.
- Reasons leading to soldering of the omentum to areas of damaged peritoneum.
- Loss of fibrin, which, falling out on the peritoneum, gradually turns into connective tissue cords.
- Numerous adhesions.
All these reasons lead to the formation of planar or strand adhesions, which can cause the development of acute intestinal obstruction. All these reasons give rise to the development of adhesive disease, which sometimes occurs with the clinic of OKN. Some authors interpret adhesive disease as the obligatory presence of OKN, but this is not so. The main reason for the formation of adhesions is trauma to the peritoneum.
From the first minute, a serous-fibrinous exudate containing various cellular elements appears at the site of peritoneal damage. Fibrin will fall out of the exudate, and the damaged surface of the peritoneum will become covered with fibrin. At the end of the 2nd day, tender fibrous formations can be observed on the peritoneum. When damaged areas of the peritoneum come into contact, they bond together due to fibrin threads. However, in the future, with shallow damage to the peritoneum, such fibrin deposits may undergo resorption and the adhesive surfaces may separate under the influence of peristalsis. If the damage to the peritoneum was deeper, involving layers deeper than the limiting membrane, then healing of the peritoneum occurs according to the type of secondary intention.
In these cases, well-vascularized granulation tissue is formed on the surface of the peritoneal defect; collagen fibers appear between the fibrin threads, located according to the direction of tension. Numerous anastomoses of venous vessels and nerve fibers appear in the adhesions. The adhesions formed in this way do not undergo resorption. Particularly powerful adhesions are formed when the parietal and visceral layers of the peritoneum are damaged and the wound surfaces come into contact. After surgical trauma, serous surfaces with a damaged mesothelial layer in some cases may be adjacent to one another, and the resulting postoperative intestinal paresis maintains the direct contact of these surfaces, which makes it possible for the process of development of adhesions to develop quietly within 2-3 days. The peristaltic movements of the intestines that occur on the 3rd day are no longer able to separate the glued surfaces and the adhesions become persistent and strong.
Adhesions and adhesions in the abdominal cavity can also develop as a result of inflammatory processes in the abdominal cavity. One of the main reasons here is acute purulent peritonitis. Chronic inflammatory process - tuberculosis, can also cause adhesions. In acute purulent peritonitis, pus accumulates in the abdominal cavity, the parietal peritoneum (and especially the visceral) sharply swells and becomes edematous, so the peritoneal mesothelium, even under the influence of a minor injury, easily sloughs off, exposing the deeper layers of the peritoneum.
The presence of an inflammatory process in the abdominal cavity leads to the cessation of peristalsis, due to which sections of the intestinal loops can come into contact with each other for a long time and thereby create conditions for gluing. In addition, deposited fibrin can also cause adhesions. The greater omentum (the policeman of the abdominal cavity) is soldered to the inflamed peritoneum of the loops, further causing the formation of cord adhesions.
The omentum entangles the intestinal loops, which leads to the formation of conglomerates of intestinal loops. Most often, in acute peritonitis, adhesions form in the lower sections, since exudate accumulates there. In most cases, after diffuse purulent peritonitis, gluing of the loops of the small intestine to each other is observed.
Chronic tuberculous peritonitis: strand and planar adhesions may occur, sometimes entire conglomerates of intestines are formed, which are difficult to separate. The omentum plays an important role in the formation of adhesions, which adheres to the tuberculous tubercles on the intestinal serosa; various types of conglomerates of intestinal loops that arise give rise to the development of OKN, and with tuberculous peritonitis, the surgeon is sometimes forced to perform surgical intervention for emergency reasons.
Presence of foreign bodies in the abdominal cavity. Even medicinal drugs increased the formation of adhesions. Of particular importance is the ingestion of tiny talc powder, which, if it gets on the peritoneum, leads to the formation of granulomas on the peritoneum. In this case, talc has not only a mechanical, but also a chemical effect - in these places an aseptic inflammatory process occurs, which has a chronic proliferative nature.
Experimental studies have shown that after introducing talc into the abdominal cavity, wide planar adhesions develop between the omentum and the parietal peritoneum, and flat adhesions between the loops of the small intestine.
Surgeons should always remember this, since in most surgical clinics, talc is widely used when putting on gloves: you should never wear gloves near the surgical field; you should change gloves when they tear.
When ligatures are applied to vessels, intestines, etc., suture material remains, which is also a foreign body. Catgut is especially undesirable in this regard; nylon and lavsan are used instead.
The introduction of drugs into the abdominal cavity causes an increase in the formation of adhesions. In the past, the technique of leaving a microirrigator in the abdominal cavity to administer antibiotics was widely used. However, now this is considered not entirely appropriate: after 1-2 days, the peritoneum sticks together and a canal forms around the microirrigator, and antibiotics do not enter the abdominal cavity. Moreover, the effect of antibiotics on an object is through its absorption into the blood, and then exposure. Local administration of antibiotics is controversial.
According to the majority of surgeons, adhesions that arise after a deep injury to the peritoneal integument most likely do not resolve, but undergo restructuring. Adhesions that arise against the background of an acute inflammatory process in any part of the abdominal cavity in a number of people undergo reverse development.
The possibility of resorption of inflammatory adhesions is indicated by the fact of resorption of the appendiceal infiltrate. If during the period of an acute inflammatory process the infiltrated omentum is fused over a large area with the appendix and adjacent intestinal loops, then after the infiltrate is reabsorbed, very small adhesions of the omentum and the appendix often remain, and all other adhesions are resolved.
From these observations it was concluded that in the immediate period after recovery from purulent peritonitis, it makes sense to use various physiotherapeutic procedures that cause the resorption of adhesions. The use of these procedures in a later period, when adhesions have already formed, will be poorly justified.
The adhesive process develops mainly after operations performed in the lower parts of the abdominal cavity and after appendectomies, which apparently should be explained by the greater frequency of this operation. Most often, the adhesive process after laparotomy develops in patients aged 20-30 years, so indications for surgical intervention at this age, especially in women, should be made very reasonably. In vain, an appendectomy performed at this age can lead to the development of adhesive disease. Therefore, prophylactic appendectomies are not justified.
The development of adhesive disease largely depends on the constitution of the body. In some cases, after one laparotomy, a significant number of adhesions develop, in other cases, after a number of laparotomies, no adhesions are formed.
The scale of the adhesive process can be different: from total to the formation of individual strands fixed at two points. As a rule, the adhesive process is more pronounced in the surgical area. Often, loops of intestines are soldered to the postoperative scar, or fixed to the walls of the postoperative hernial sac.
Therefore, when there is an operation for a ventral postoperative hernia, especially a strangulated one, it is very easy to damage the swollen loops of intestines when the hernial sac is opened.
Make an appointment
Contraindications for surgery
List of contraindications for laparoscopic dissection of adhesions:
- acute infections and diseases;
- exacerbation of chronic pathology;
- severe damage to the heart, blood vessels and respiratory tract (due to problems with anesthesia);
- severe damage to the kidneys, liver, digestion until the condition stabilizes;
- serious and uncorrectable metabolic problems;
- blood clotting disorders;
- pregnancy period.
After the examination, the doctor can determine other individual contraindications, for example, allergies or intolerance to anesthesia or medications, and then the issue of intervention is decided individually.